Abstract
Objectives
This study examined the relationship between the consumption of plant-based diet and frailty in older Chinese adults.
Design
Prospective cohort study
Setting
Community-based setting in 22 provinces of China.
Participants
The final sample included data from 3990 older adults from 2011–2014 from the Chinese Longitudinal Healthy Longevity Survey
Measurements
A plant-based diet index (PDI) was calculated based on a qualitative food frequency questionnaire. Frailty was defined using modified Fried criteria. A Generalized Estimating Equation was used to estimate risk ratios (RRs) and 95% confidence intervals (CIs) for frailty. We further performed subgroup analyses stratified by sex and lifestyle factors.
Results
557 cases of frailty were observed. After adjustment for covariates, the RR for frailty of a high PDI was 0.792 (95% CI: 0.644–0.973), relative to a low PDI. During follow-up, compared with respondents with a continually low PDI, the respondents with a continually high PDI had a significantly reduced risk of frailty (RR = 0.683, 95% CI: 0.514–0.908). In further subgroup analysis, a consistently high PDI over time resulted in a significantly reduced risk of frailty for male (RR = 0.591, 95% CI: 0.391–0.893); for never smokers (RR = 0.670, 95% CI: 0.458–0.979); for people who did never consume alcohol (RR = 0.654, 95% CI: 0.454–0.941); and for people with current or former exercise habits (RR = 0.488, 95% CI: 0.313–0.762).
Conclusion
Plant-based diet was associated with low risk of frailty in men and in older adults with healthy lifestyle. These findings stress that plant-based diet should be recommended as a dietary strategy to prevent and reduce frailty in older adults; in addition, more dietary interventions along with lifestyle modification should be adopted to promote successful ageing, especially for women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is one of the most severe global public health challenges (1). The number of older adults with frailty will increase rapidly with the older adult population (2). The prevalence of frailty in older adults (≥65 years) is estimated to range from 4.0% to 59.1% (3–5). Frailty is an age-related clinical syndrome of decreased resilience to internal and external stressors and is associated with a wide range of adverse outcomes, including fractures, hospitalization, disability, falls, and death (6). Frailty is dynamic (7), and individual frailty can increase or decrease over time (8). Strategies to prevent and slow the progression of frailty are therefore crucial (9).
Diet is a crucial lifestyle factor to frailty prevention (10). A meta-analysis of 13 studies revealed that high adherence to healthy dietary patterns is associated with a reduced risk of frailty (11). Plant-based diet has received more and more attention for their health benefits. Plant-based diet is defined as a dietary profile that emphasizes the intake of plant-based foods while limiting the intake of animal products (12–15). A plant-based diet index (PDI) can be used to assess compliance with plant-based diet and low consumption of animal products (16).
Previous two studies have reported an association between plant-based diets and frailty (17, 18), one conducted in an older Mediterranean population (17) and the other in American women (18). However, neither study focused on the association of changes in the dynamics of plant-based diets with frailty. In addition, there were no studies on Chinese older adults. This study is to explore the association between the adherence to plant-based diet and the development of frailty in Chinese older adults by using a nationally representative survey and is the first time to explore the lifestyle- and gender-specific differences in the relationship between plant-based diet and frailty, providing evidence to formulate targeted dietary strategies to prevent older adults’ frailty and its associated adverse outcomes.
Methods
Study population
The Chinese Longitudinal Healthy Longevity Survey (CLHLS) is an ongoing prospective cohort study investigating the determinants of the health and longevity of older adults in China (19). In brief, the CLHLS is a national survey covering 22 of 31 provinces in China and accounting for approximately 85% of China’s population. It began in 1998 and is administered every 2–3 years. After entering the cohort, all individuals are interviewed about potential health determinants, including their lifestyle habits, socio-economic characteristics, cognitive function, physical abilities, and psychological status.
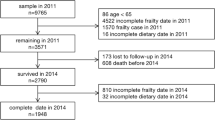
Longitudinal data from 2011 to 2014 were used in this study. The 2011 survey wave included 9765 participants, of which we excluded participants under 65 years of age, with missing dietary data and missing frailty data, having frailty in 2011, and participants who lost or died prior to the 2014 survey, and participants with missing dietary data and frailty data in 2014. Finally, a total of 3990 participants from 2011 to 2014 were included to determine the relationship between plant-based diet and frailty in this study. Figure 1 illustrates the sample selection process.
Frailty assessment
Frailty was defined using modified Fried criteria (6, 20–22). Exhaustion, low mobility, weakness, inactivity, and shrink were assessed using self-report data. Exhaustion was defined as an answer of “always,” “often,” or “sometimes” to whether a participant felt “useless with age” (21–24). Shrink was defined as a body mass index <18.5 kg/m2 (20, 21, 25). Weakness was defined as the participant failing to lift a 5-kg bag (20, 25). Low mobility was defined as the participant failing to walk a distance of 1 km (26). Inactivity was defined if the participant did the following activities 1 time per week or less: housework, outside activity, gardening, keeping a pet, livestock breeding, playing cards or mah-jongg, and social activity (23). A participant fulfilling at least three criteria (i.e., exhaustion, low mobility, weakness, shrink, or inactivity) was considered to exhibit frailty.
PDI calculation
Information on each participant’s diet in 2011 and 2014 was collected using a qualitative simplified food frequency questionnaire (FFQ). The reliability and validity of the questionnaire are well supported (27). The qualitative simplified FFQ included 16 food groups that Chinese people often consume, divided into two categories: plant-based foods (whole grains, nuts, tea, legumes, garlic, vegetable oils, fresh fruits, fresh vegetables, preserved vegetables, refined grains, and sugar [white granulated sugar or candy]) and animal-based foods (fish and seafood, meat, animal fat, eggs, and milk and dairy products) (15, 28). The qualitative simplified FFQ collects information about the participant’s diet at the time of the interview (e.g., “how often eat meat at present?” Response included almost everyday, ≥1 time/week, ≥1 time/month, occasionally and rarely or never).
A PDI was calculated on the basis of the frequency with which the participants consumed the 16 food groups as a reflection of their overall diets (15). Intake frequencies were scored between 1 and 5; the plant-based food groups received positive scores, whereas the animal-based food groups received negative scores. The theoretical range of the PDI was 16–80. The scoring criteria and intake frequencies are presented in Table A1 (Supplementary Materials). We divided the participants into a low PDI group and a high PDI group on the basis of the median PDI.
We further categorized the temporal PDI change from 2011 to 2014 based on the dichotomous PDI as a PDI decrease, PDI increase, consistently low PDI, or consistently high PDI. This information is presented in Table A2 (Supplementary Materials).
Covariate assessment
In our analysis, we adjusted for covariates that may influence frailty in older adults (29) which were collected in 2011, including sex (male vs. female), age group (65–79 vs. ≥80 years), education status (formal vs. informal education, according to whether the respondent had attended school), alcohol consumption (former or current drinker vs. never drinker), exercise status (former or current exercise habits vs. no history of regular exercise), smoking status (former or current smoker vs. never smoker), body mass index (BMI, underweight, vs. normal, vs. overweight, vs. obese), residential location (city vs. town or rural area), marital status (currently married and living with a spouse vs. other), insurance status (yes vs. no), financial support (dependent vs. independent), and history of chronic disease (yes vs. no). A participant was considered to have no history of chronic disease if they did not self-report hypertension, asthma, heart disease, emphysema, bronchitis, diabetes, or pneumonia; otherwise, they were considered to have a history of chronic disease. We dichotomized financial support into financial independence, which was defined as having employment or retirement wages, or financial dependence, which was defined as reliance on other family members for financial support.
Statistical analysis
Baseline characteristics were analyzed as numbers and percentages, and chi-square tests were used to identify differences. We used a Generalized Estimating Equation to estimate the association between PDI (including PDI for continuous variables, PDI for categorical variables, and changes in PDI) and frailty. We further stratified the sample by sex and lifestyle factors (smoking status, alcohol consumption, and exercise) to investigate whether these factors affect the benefits of high PDI diet. Statistical analysis was conducted in RStudio, version 4.1.2 (the R Foundation). Significance was indicated by P < 0.05.
Results
Table 1 provides the baseline characteristics of the study participants. Of the 3990 participants, 2076 (52.0%) were men, and the mean age was 79.57 ± 8.94 years. In total, 3355 (84.1%) participants were living in towns or rural areas, 2420 (60.9%) were never smokers, 2517 (63.6%) were never drinkers, 1891 (47.9%) never had regular exercise habits, 2100 (52.8%) had formal education, 2497 (62.7%) were financially dependent, 2309 (57.9%) had a normal BMI, 3638 (92.7%) had insurance and 1744 (45.4%) had a history of chronic illness. According to chi-square tests, all baseline characteristics differed between the high PDI and low PDI groups, except for insurance and history of chronic diseases.
The median PDI of the 3990 participants was 50. The participants who are male, aged 65–79, have a normal BMI, live in city area, have formal education, be financially independent, be currently married and living with spouse, have previous or current exercise habits and are former or current smokers and drinkers were more likely to have high PDI.
During the follow-up of 11134.5 person-years, 557 cases of frailty were observed: 363 participants with low PDIs and 194 participants with high PDIs. In an unadjusted analysis, the risk ratio (RR) of a high PDI (vs. a low PDI) for frailty was 0.654 (95% confidence interval [CI]: 0.538–0.794). After adjustment for sex, age, BMI, residential location, financial support, insurance, history of chronic diseases, alcohol consumption, smoking status, exercise status, marital status, and education status (the final model), the inverse association remained significant (RR = 0.792, 95% CI: 0.644–0.973; Table 2). With PDI as a continuous variable, this inverse association did not change (RR = 0.964, 95% CI: 0.949–0.978) in the crude model; RR = 0.982, 95% CI: 0.966–0.998 in the final model; Table 2).
Table 3 presents the associations between changes in PDI and frailty. After adjustment for all covariates, compared with participants whose PDI remained low, only those whose PDI remained high over time had a significantly reduced risk of frailty (RR = 0.683; 95% CI: 0.514–0.908).
We further evaluated the how the relationship between PDI changes and frailty changed with sex and lifestyle factors (smoking, alcohol consumption, and exercise). As presented in Table 3, compared with a consistently low PDI, a consistently high PDI resulted in a significantly reduced risk of frailty for male (RR = 0.591, 95% CI: 0.391–0.893) but not for female (RR = 0.762, 95% CI: 0.512–1,134); for never smokers (RR = 0.670, 95% CI: 0.458–0.979) but not for former or current smokers (RR = 0.711, 95% CI: 0.456–1.110); for never drinkers (RR = 0.654, 95% CI: 0.454–0.941) but not for former or current drinkers (RR = 0.720, 95% CI: 0.454–1.142); and for people with current or former exercise habits (RR = 0.488, 95% CI: 0.313–0.762) but not for people who never exercised regularly (RR = 0.924, 95% CI: 0.634–1.347).
Discussion
Using data from a large prospective study of the Chinese community and adjusting for baseline frailty risk factors and additional confounding variables, we observed that a high PDI, that is, greater intake of plant-based diet or greater adherence to plant-based diet, was significantly and inversely associated with the risk of frailty among older adults. However, there are gender and lifestyle specific differences in the protective effects of high PDI diet. This association appeared in men and participants with a healthy lifestyle and was not observed in women and participants with an unhealthy lifestyle.
Frailty may result from tissue damage caused by oxidative stress and inflammatory processes (30). A meta-analysis discovered that C-reactive protein and serum interleukin 6 levels were higher in individuals exhibiting prefrailty or frailty than they were in nonfrail individuals (31). Consumption of foods rich in antioxidants in daily diet can reduce the adverse effects of oxidative stress (32) and is negatively associated with the risk of frailty (33). Plant-based foods have high levels of various antioxidant micronutrients, including vitamins C and E and beta-carotene (34). These antioxidants reduce or prevent frailty by lower levels of reactive oxygen species, which can cause DNA, lipid, and protein damage and induce mitochondrial dysfunction and apoptosis (35). Plant-based diet rich in whole grains, fruits, nuts, and vegetables can regulate immune and inflammatory processes (36, 37). Tea is also common in Chinese plant-based diet, and tea polyphenols can reduce the levels of interleukin 1β, the proinflammatory cytokine tumor necrosis factor, and interleukin 6 to reduce inflammation and prevent frailty (38). A Japanese study showed that green tea consumption was inversely related to the prevalence of frailty (39). Plant-based diet is rich in dietary fiber, which has also been linked to lower levels of inflammatory markers (40). Adequate dietary protein intake has a positive impact on increasing muscle protein synthesis and improving body function, and another characteristic of frailty is the loss of muscle strength and quality (41). The protein in beans and nuts helps to prevent muscle loss (42). Although this diet maybe does not present higher amounts of protein, the vegetable protein (mainly from legumes) associated with antioxidant nutrients may collaborate for muscle maintenance. People with high PDI diet can prevent frailty by consuming more plant protein. Similar with other healthy dietary patterns, such as the Mediterranean diet, high PDI diet is rich in fruits, nuts, vegetables, and legumes, and is conductive to reduce the frailty (43, 44). It is noted that the Mediterranean diet also has moderate consumption of fish and poultry (45) which provide high quality protein, and it is associated with a reduced risk of frailty (46). However, the PDI was scored for animal foods reverse orientation, and high PDI diet is often low in animal foods, which may be associated with increased risk of frailty. Interestingly, the integration effect from high PDI diet finally reduced the risk of frailty in this study.
Plant-based diet is associated with reduced risks of cognitive impairment (28) and diabetes (47) improved insulin resistance (48) and weight loss (49), and lower total cholesterol (50). In addition, high intake of fruits, vegetables, and whole grains is associated with a reduced risk of depression (51) The aforementioned chronic diseases are risk factors for frailty (4, 52–54). Thus, the protective effect of plant-based diet against frailty risk may stem from their benefits in preventing chronic diseases. In the present study, older adults who reported a high PDI that remained consistent over time had a significantly lower risk of frailty during follow-up than those who reported a less PDI at any time. An individual’s eating behavior may change over time (55), and the prevalence of dysphagia increases with age (56) Older adults with dysphagia consume fewer vegetables than those without consume (57). Thus, only consistent consumption of high PDI may be beneficial in combating frailty, as suggested by our previous study in which long-term tea consumption was beneficial in reducing the risk of frailty in older adults (58).
It is noted that the frailty-lowering effect of long-term adherence to high PDI diet occurred only in men, but not in women in the sex-stratified analysis. This sex-difference may be related to the vulnerability of women in response to stress or diseases. Women are more likely to be frailty than men (59). Compared with men, women are more vulnerable to disability and chronic diseases (60), have greater loss of physiological reserves (61) and lower muscle mass index (62). In addition, women’s socio-economic and health status is often worse (63). In this situation, the benefit of high PDI diet in preventing frailty did not present in women. Our results also suggest that the benefits of high PDI diet are dependent on lifestyle factors. We found that long-term consumption of a high PDI had a significant preventive effect against frailty in older adults with healthy lifestyles (never smoking, never drinking, or exercising or having exercised). Smokers have demonstrated poor adherence to high PDI diet and often consume more meat and fewer cereals, fruits, and vegetables than nonsmokers do (64, 65). Additionally, smokers have significantly higher intake of cholesterol, saturated fat, and total fat and lower intake of beta-carotene, vitamin E, vitamin C, and fiber (66) as well as higher levels of inflammatory mediators (67), which can lead to frailty (6, 68). Smoking also increases the risk of frailty by reducing muscle protein synthesis, muscle strength, and physical function in older adults (69). Therefore, people who smoke are more likely to experience frailty (70), and the preventive effect of high PDI diet against frailty may be weakened in smokers. Increased alcohol consumption is associated with decreased diet quality, including increased meat and fat intake and reduced fruit intake (71, 72). In addition, older adults are at higher risks of the negative effects of alcohol consumption, such as malnutrition, fractures, falls, and cognitive decline (73). Physical exercise can increase muscle strength (74) and brain volume (75). Colcombe et al. showed that exercise increased the volume of white and gray matter primarily located in the temporal cortex and prefrontal cortex, which showed age-related deterioration (75). Physical exercise can also improve mobility and physical function in older people with mobility problems or physical disabilities (76). One of the reasons for performing physical exercise is a desire to maintain fitness. Such health consciousness is related to healthy diet choices (77). That is, older people who exercise may be more likely to choose high PDI diet. Thus, we observed that the association between high PDI diet and frailty varied with lifestyle factors. These findings provide guidance for older adults to prevent or delay frailty through lifestyle choices.
Strengths and limitations
To our knowledge, this study was the first to examine the association between plant-based diet and frailty among older Chinese adults by using nationally representative cohort data. An advantage is its exploration of the role of changes in the consumption of plant-based diet. However, our study has some limitations. First, although the frailty criteria have been widely used, frailty screening tools are heterogeneous. Second, the information used to classify frailty was self-reported by the participants and no physical tests were performed. Moreover, weight change or nutritional status is not assessed. Finally, we could not calculate and adjust for total energy intake, and dietary assessment based on the FFQ may have been subject to recall bias.
Conclusions
This study demonstrated a prospective association between adherence to high PDI diet and reduced risk of frailty in older adults. However, it should be noted that this association was heterogeneous with respect to gender and lifestyle. In particular, the association between high PDI diet and frailty was significant in men and in individuals with a healthy lifestyle. These findings stress that plant-based diet, especially with consistently high PDI diet, should be recommended as a dietary strategy to prevent and reduce frailty in older adults; in addition, more dietary interventions along with lifestyle modification should be adopted to promote successful ageing, especially for women.
References
Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394:1376–1386. doi:https://doi.org/10.1016/S0140-6736(19)31785-4
Yu R, Wong M, Chong KC, Chang B, Lum CM, Auyeung TW, Lee J, Lee R, Woo J. Trajectories of frailty among Chinese older people in Hong Kong between 2001 and 2012: an age-period-cohort analysis. Age Ageing. 2018;47:254–261. doi:https://doi.org/10.1016/S0140-6736(19)31785-4
Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64:675–681. doi:https://doi.org/10.1093/gerona/glp012
Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012 60:1487–1492. doi:https://doi.org/10.1111/j.1532-5415.2012.04054.x
Woo J, Yu R, Wong M, Yeung F, Wong M, Lum C. Frailty Screening in the Community Using the FRAIL Scale. J Am Med Dir Assoc. 2015;16:412–419. doi:https://doi.org/10.1016/j.jamda.2015.01.087
Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: https://doi.org/10.1093/gerona/56.3.m146.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people Lancet. 2013;381:752–762. doi:https://doi.org/10.1016/S0140-6736(12)62167-9
Junius-Walker U, Onder G, Soleymani D, et al. The essence of frailty: A systematic review and qualitative synthesis on frailty concepts and definitions. Eur J Intern Med. 2018;56:3–10. doi: https://doi.org/10.1016/j.ejim.2018.04.023
Puts MTE, Toubasi S, Andrew MK, et al. Interventions to prevent or reduce the level of frailty in community-dwelling older adults: a scoping review of the literature and international policies. Age Ageing. 2017;46:383–392. doi: https://doi.org/10.1093/ageing/afw247
Capurso C, Bellanti F, Lo Buglio A, Vendemiale G. The Mediterranean Diet Slows Down the Progression of Aging and Helps to Prevent the Onset of Frailty: A Narrative Review. Nutrients. 2019;12:35. doi:https://doi.org/10.3390/nu12010035
Rashidi Pour Fard N, Amirabdollahian F, Haghighatdoost F. Dietary patterns and frailty: a systematic review and meta-analysis. Nutr Rev. 2019;77:498–513. doi: https://doi.org/10.1093/nutrit/nuz007
Quek J, Lim G, Lim WH, et al. The Association of Plant-Based Diet With Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies. Front Cardiovasc Med. 2021; 8:756810. doi: https://doi.org/10.3389/fcvm.2021.756810
Ostfeld RJ. Definition of a plant-based diet and overview of this special issue. J Geriatr Cardiol. 2017;14:315. doi:https://doi.org/10.11909/j.issn.1671-5411.2017.05.008
Tuso PJ, Ismail MH, Ha BP, Bartolotto C. Nutritional update for physicians: plant-based diets. Perm J. 2013;17:61–66. doi: https://doi.org/10.7812/TPP/12-085
Joshi S, McMacken M, Kalantar-Zadeh K. Plant-Based Diets for Kidney Disease: A Guide for Clinicians. Am J Kidney Dis. 2021;77:287–296. doi: https://doi.org/10.1053/j.ajkd.2020.10.003
Satija A, Bhupathiraju SN, Rimm EB, et al. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLos Med. 2016;13:18. doi: https://doi.org/10.1371/journal.pmed.1002039.
Maroto-Rodriguez J, Delgado-Velandia M, Ortolá R, et al. Plant-based diets and risk of frailty in community-dwelling older adults: the Seniors-ENRICA-1 cohort. GeroScience. 2022;1-12. doi:https://doi.org/10.1007/s11357-022-00614-3
Sotos-Prieto M, Struijk EA, Fung TT, et al. Association between the quality of plant-based diets and risk of frailty. J Cachexia Sarcopenia Muscle. 2022. doi:https://doi.org/10.1002/jcsm.13077
Zeng Y, Poston DL, Jr. Introduction to the Chinese Longitudinal Healthy Longevity Survey (CLHLS) In: Zeng Y, Vlosky DA, Gu D, editors. Healthy longevity in China: demographic, socioeconomic, and psychological dimensions. Dordrecht: Springer Publisher; 2008. p. 23–38.
Herr M, Jeune B, Fors S, et al. Frailty and associated factors among centenarians in the 5-COOP countries. Gerontology. 2018;64:521–531. doi:https://doi.org/10.1159/000489955
Wu C, Smit E, Xue QL, Odden MC. Prevalence and correlates of frailty among community-dwelling chinese older adults: the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. 2017;73:102–108. doi:https://doi.org/10.1093/gerona/glx098
Wang HY, Lv X, Du J, Kong G, Zhang L. Age- and Gender-Specific Prevalence of Frailty and Its Outcomes in the Longevous Population: The Chinese Longitudinal Healthy Longevity Study. Front Med 2021;8:719806. doi:https://doi.org/10.3389/fmed.2021.719806
Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK Biobank participants. Lancet Public Health. 2018;3:e323–332. doi:https://doi.org/10.1016/S2468-2667(18)30091-4
Sha S, Xu Y, Chen L. Loneliness as a risk factor for frailty transition among older Chinese people BMC Geriatr. 2020;20:300. doi: https://doi.org/10.1186/s12877-020-01714-5
Singh S, Bailey KR, Noheria A, Kullo IJ. Frailty across the spectrum of ankle-brachial index. Angiology. 2012;63:229–236. doi:https://doi.org/10.1177/0003319711413457
Abellan van Kan G, Rolland YM, Morley JE, Vellas B. Frailty: toward a clinical definition. J Am Med Dir Assoc. 2008;9:71–72. doi:https://doi.org/10.1016/j.jamda.2007.11.005
Zhu A, Chen H, Shen J, Wang X, Li Z, Zhao A, Shi X, Yan L, Zeng Y, Yuan C, Ji JS. Interaction between plant-based dietary pattern and air pollution on cognitive function: a prospective cohort analysis of Chinese older adults. Lancet Reg Health West Pac. 2022 Jan 5;20:100372. doi:https://doi.org/10.1016/j.lanwpc.2021.100372
Liang F, Fu J, Turner-McGrievy G, et al. Association of Body Mass Index and Plant-Based Diet with Cognitive Impairment among Older Chinese Adults: A Prospective, Nationwide Cohort Study. Nutrients. 2022;14: 3132. doi:https://doi.org/10.3390/nu14153132
Sirven N, Dumontet M, Rapp T. The dynamics of frailty and change in socio-economic conditions: evidence for the 65+ in Europe. Eur J Public Health. 2020; 30:715–719. doi:https://doi.org/10.1093/eurpub/ckaa068
Lo YL, Hsieh YT, Hsu LL, et al. Dietary pattern associated with frailty: results from nutrition and health survey in Taiwan. J Am Geriatr Soc. 2017;65:2009–2015. doi:https://doi.org/10.1111/jgs.14972.
Soysal P, Stubbs B, Lucato P, et al. Inflammation and frailty in the elderly: A systematic review and meta-analysis. Ageing Res Rev. 2016;31:1–8. doi: https://doi.org/10.1016/j.arr.2016.08.006
Jiang S, Liu H, Li C. Dietary Regulation of Oxidative Stress in Chronic Metabolic Diseases. Foods. 2021;10:1854. 35. doi:https://doi.org/10.3390/foods10081854
Three-generation Three-generation Study of Women on Diets and Health Study Group, Kobayashi S, Suga H, Sasaki S. Diet with a combination of high protein and high total antioxidant capacity is strongly associated with low prevalence of frailty among old Japanese women: a multicenter cross-sectional study. Nutr J. 2017;16:29. doi:https://doi.org/10.1186/s12937-017-0250-9
Talegawkar SA, Bandinelli S, Bandeen-Roche K, et al. A higher adherence to a Mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J Nutr. 2012;142: 2161–2166. doi: https://doi.org/10.3945/jn.112.165498
Bonnefoy M, Berrut G, Lesourd B, et al. Frailty and nutrition: searching for evidence. J Nutr Health Aging. 2015;19:250–257. doi: https://doi.org/10.1007/s12603-014-0568-3
Menzel J, Biemann R, Longree A, et al. Associations of a vegan diet with inflammatory biomarkers. Sci Rep. 2020;10:1933. doi: https://doi.org/10.1038/s41598-020-58875-x
Jiang L, Zhang G, Li Y, Shi G, Li M. Potential Application of Plant-Based Functional Foods in the Development of Immune Boosters. Front Pharmacol. 2021; 12:637782. doi:https://doi.org/10.3389/fphar.2021.637782
Chen Y, Cheng S, Dai J, et al. Molecular mechanisms and applications of tea polyphenols: a narrative review. J Food Biochemist 2021; 45:e13910.
Nanri H, Yoshida T, Watanabe Y, et al. The Association between Habitual Green Tea Consumption and Comprehensive Frailty as Assessed by Kihon Checklist Indexes among an Older Japanese Population. Nutrients. 2021:13:4149. doi:https://doi.org/10.3390/nu13114149
Butcher JL, Beckstrand RL. Fiber’s impact on high-sensitivity C-reactive protein levels in cardiovascular disease. J Am Acad Nurse Pract. 2010;22:566–572. doi: https://doi.org/10.1111/j.1745-7599.2010.00555.x
Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61:1059–1064. doi: https://doi.org/10.1093/gerona/61.10.1059
Kojima G, Avgerinou C, Iliffe S, Jivraj S, Sekiguchi K, Walters K. Fruit and Vegetable Consumption and Frailty: A Systematic Review. J Nutr Health Aging. 2018;22:1010–1017. doi: https://doi.org/10.1007/s12603-018-1069-6
García-Esquinas E, Rahi B, Peres K, et al. Consumption of fruit and vegetables and risk of frailty: a dose-response analysis of 3 prospective cohorts of community-dwelling older adults. Am J Clin Nutr. 2016;104:132–142. doi:https://doi.org/10.3945/ajcn.115.125781
Wang R, Hannan MT, Wang M, Schwartz AW, Lopez-Garcia E, Grodstein F. Long-Term Consumption of Nuts (Including Peanuts, Peanut Butter, Walnuts, and Other Nuts) in Relation to Risk of Frailty in Older Women: Evidence from a Cohort Study. J Nutr. 2023;153:820–827. doi:https://doi.org/10.1016/j.tjnut.2023.01.003
Figueroa C, Echeverría G, Villarreal G, Martínez X, Ferreccio C, Rigotti A. Introducing Plant-Based Mediterranean Diet as a Lifestyle Medicine Approach in Latin America: Opportunities Within the Chilean Context. Front Nutr. 2021;8:680452. doi: https://doi.org/10.3389/fnut.2021.680452
Sandoval-Insausti H, Pérez-Tasigchana RF, López-García E, et al. Macronutrients Intake and Incident Frailty in Older Adults: A Prospective Cohort Study. J Gerontol A Biol Sci Med Sci. 2016;71(10):1329–1334. doi:https://doi.org/10.1093/gerona/glw033
Chen Z, Drouin-Chartier JP, Li Y, et al. Changes in Plant-Based Diet Indices and Subsequent Risk of Type 2 Diabetes in Women and Men: Three U.S. Prospective Cohorts. Diabetes Care. 2021;44:663–671. doi: https://doi.org/10.2337/dc20-1636
Kahleova H, Tura A, Hill M, Holubkov R, Barnard ND. A Plant-Based Dietary Intervention Improves Beta-Cell Function and Insulin Resistance in Overweight Adults: A 16-Week Randomized Clinical Trial. Nutrients. 2018;10:189. doi: https://doi.org/10.3390/nu10020189
Barnard ND, Levin SM, Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet. 2015;115:954–969. doi: https://doi.org/10.1016/j.jand.2014.11.016
Yokoyama Y, Levin SM, Barnard ND. Association between plant-based diets and plasma lipids: a systematic review and meta-analysis. Nutr Rev. 2017;75:683–698. doi: https://doi.org/10.1093/nutrit/nux030
Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2014;99:181–197. doi: https://doi.org/10.3945/ajcn.113.069880
Stenholm S, Strandberg TE, Pitkälä K, Sainio P, Heliövaara M, Koskinen S. Midlife obesity and risk of frailty in old age during a 22-year follow-up in men and women: the Mini-Finland Follow-up Survey. J Gerontol A Biol Sci Med Sci. 2014 69:73–78. doi: https://doi.org/10.1093/gerona/glt052
Han ES, Lee Y, Kim J. Association of cognitive impairment with frailty in community-dwelling older adults. Int Psychogeriatr. 2014;26:155–163. doi:https://doi.org/10.1017/S1041610213001841
Lohman M, Dumenci L, Mezuk B. Sex differences in the construct overlap of frailty and depression: evidence from the Health and Retirement Study. J Am Geriatr Soc. 2014;62:500–505. doi: https://doi.org/10.1111/jgs.12689
Rehm CD, Peñalvo JL, Afshin A, Mozaffarian DJJ. Dietary intake among US adults, 1999–2012. JAMA. 2016;315:2542–2553. doi: https://doi.org/10.1001/jama.2016.7491
Ministry of Health and Welfare. 2008 survey on the elderly status: national survey results on the elderly life conditions and welfare need [Internet] Seoul: Ministry of Health and Welfare; 2009. Accessed October 9, 2022. http://www.mohw.go.kr/react/jb/sjb030301vw.jsp?PAR_MENU_ID=03&MENU_ID=0321&CONT_SEQ=264469&page=1
Won Y. 2003. The relationship of oral state and dietary habit to health condition among elderly people. [master’s thesis] [Seoul]: Yonsei University.
Gao T, Han S, Mo G, Sun Q, Zhang M, Liu H. Long-term tea consumption reduces the risk of frailty in older Chinese people: Result from a 6-year longitudinal study. Front Nutr. 2022;9:916791. doi:https://doi.org/10.3389/fnut.2022.916791
Gordon EH, Peel NM, Samanta M, Theou O, Howlett SE, Hubbard RE. Sex differences in frailty: A systematic review and meta-analysis. Exp Gerontol. 2017;89:30–40. doi: https://doi.org/10.1016/j.exger.2016.12.021
Oksuzyan A, Juel K, Vaupel JW, Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clin Exp Res. 2008;20:91–102. doi: https://doi.org/10.1007/BF03324754
Yang Y, Lee LC. Dynamics and heterogeneity in the process of human frailty and aging: evidence from the U.S. older adult population. J Gerontol B Psychol Sci Soc Sci. 2010;65B:246–255. doi: https://doi.org/10.1093/geronb/gbp102
Fernandez-Bolaños M, Otero A, Zunzunegui MV, et al. Sex differences in the prevalence of frailty in a population aged 75 and older in Spain. J Am Geriatr Soc. 2008;56:2370–2371. doi: https://doi.org/10.1111/j.1532-5415.2008.02032.x
Alvarado BE, Zunzunegui MV, Béland F, Bamvita JM. Life course social and health conditions linked to frailty in Latin American older men and women. J Gerontol A Biol Sci Med Sci. 2008;63:1399–1406. doi: https://doi.org/10.1093/gerona/63.12.1399
Heydari G, Heidari F, Yousefifard M, Hosseini M. Smoking and diet in healthy adults: a cross-sectional study in tehran, iran, 2010. Iran J Public Health. 2014 43:485–491.
Cade JE, Margetts BM. Relationship between diet and smoking—is the diet of smokers different? J Epidemiol Community Health. 1991;45:270–272. doi: https://doi.org/10.1136/jech.45.4.270
Dallongeville J, Marécaux N, Fruchart JC, Amouyel P. Cigarette smoking is associated with unhealthy patterns of nutrient intake: a meta-analysis. J Nutr. 1998;28:1450–1457. doi: https://doi.org/10.1093/jn/128.9.1450
Goncalves RB, Coletta RD, Silverio KG, et al. Impact of smoking on inflammation: overview of molecular mechanisms. Inflamm Res. 2011;60:409–424. doi: https://doi.org/10.1007/s00011-011-0308-7
Kanapuru B, Ershler WB. Inflammation, coagulation, and the pathway to frailty. Am J Med. 2009;122:605–613. doi: https://doi.org/10.1016/j.amjmed.2009.01.030
Rapuri PB, Gallagher JC, Smith LM. Smoking is a risk factor for decreased physical performance in elderly women. J Gerontol A Biol Sci Med Sci. 2007;62:93–100. doi: https://doi.org/10.1093/gerona/62.1.93
DeClercq V, Duhamel TA, Theou O, Kehler S. Association between lifestyle behaviors and frailty in Atlantic Canadian males and females. Arch Gerontol Geriatr. 2020;91:104207. doi:https://doi.org/10.1016/j.archger.2020.104207
Breslow RA, Guenther PM, Smothers BA. Alcohol drinking patterns and diet quality: the 1999–2000 National Health and Nutrition Examination Survey. Am J Epidemio. 2006;163:359–366. doi: https://doi.org/10.1093/aje/kwj050
Breslow RA, Guenther PM, Juan W, Graubard BI. Alcoholic beverage consumption, nutrient intakes, and diet quality in the US adult population, 1999–2006. J Am Diet Assoc. 2010;110:551–562. doi: https://doi.org/10.1016/j.jada.2009.12.026
Gaxatte C, Faraj E, Lathuillerie O, et al. Alcohol and psychotropic drugs: risk factors for orthostatic hypotension in elderly fallers. J Hum Hypertens. 2017;31:299–304. doi: https://doi.org/10.1038/jhh.2013.82
Cress ME, Buchner DM, Questad KA, Esselman PC, deLateur BJ, Schwartz RS. Exercise: Effects on Physical Functional Performance in Independent Older Adults. J Gerontol A Biol Sci Med Sci. 1999;54:M242–M248. doi: https://doi.org/10.1093/gerona/54.5.M242
Colcombe SJ, Erickson KI, Scalf PE, et al. Aerobic exercise training increases brain volume in aging humans. J Gerontol A Biol Sci Med Sci. 2006;61:1166–1170. doi: https://doi.org/10.1093/gerona/61.11.1166
de Vries NM, van Ravensberg CD, Hobbelen JSM, Rikkert MGMO, Staal JB, Nijhuis-van der Sanden MWG. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing Res Rev. 2012;11:136–149. doi: https://doi.org/10.1016/j.arr.2011.11.002
Nakamoto M, Yun Y, Omine M, et al. Dietary diversity and characteristics of lifestyle and awareness of health in Japanese workers: a cross-sectional study. J Med Invest 2020;67:255–264. doi: https://doi.org/10.2152/jmi.67.255
Acknowledgements
The data used in this study was obtained from the CLHLS, which was managed by the Peking University Center for Healthy Aging and Development Studies. This survey was jointly funded by the National Natural Science Foundation of China (No. 71233001 and 71110107025), NIH (No. R01AG023627) and the United Nations Population Fund.
Funding
The work was supported by the 512 Talent training Project of Bengbu Medical College (BY51201203) and the Natural Science Foundation of Anhui Provincial Educational Committee (KJ2019A0302, 2022AH040217).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The CLHLS study was approved by the Research Ethics Committee of Peking University (IRB00001052-13074), and all participants or their proxy respondents provided written informed consent. The research was performed in accordance with the Declaration of Helsinki. All procedures were performed in accordance with relevant guidelines.
Additional information
Conflict of interests
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Duan, Y., Qi, Q., Gao, T. et al. Plant-Based Diet and Risk of Frailty in Older Chinese Adults. J Nutr Health Aging 27, 371–377 (2023). https://doi.org/10.1007/s12603-023-1918-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1918-9