Abstract
Background
Inflammation is a critical component of normal tissue repair, as well as being fundamental to the body’s defense against infection. Environmental factors, such as smoking, have been reported to modify the host response and hence modify inflammation progression, severity and outcome. Therefore, a comprehensive understanding of the molecular mechanisms by which smoking affects inflammation is vital for preventive and therapeutic strategies on a clinical level.
Aim
The purpose of the present article is to review the potential biological mechanisms by which smoking affects inflammation, emphasizing recent developments.
Results
Smoking is reported to effect a number of biological mediators of inflammation through its effect on immune-inflammatory cells, leading to an immunosuppressant state. Recent evidence strongly suggests that the molecular mechanisms behind the modulation of inflammation by smoking mainly involve the nuclear factor-kappa B (NF-kB) family, through the activation of both an inhibitor of IkB kinase (IKK)-dependent and -independent pathway. In addition to NF-kB activation, a number of transcriptional factors including GATA, PAX5 and Smad 3/4, have also been implicated.
Conclusion
Multiple mechanisms may be responsible for the association of smoking and inflammation, and the identification of potential therapeutic targets should guide future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tobacco use has been considered the single greatest contributor to preventable illness and premature death worldwide. In the United States, tobacco use accounts for over 435,000 deaths each year, making it the leading cause of death. Smoking affects multiple organs and significantly increases the risk of heart diseases, cancers, chronic obstructive pulmonary diseases, autoimmune diseases, neurodegenerative diseases, and microbial infections, including periodontitis [1]. The putative influence of tobacco smoking in the immune and inflammatory processes was identified in the 1960s. However, the relationship between smoking and systemic diseases is based mostly on epidemiological studies, and the mechanisms behind these effects are still under investigation. Although increasing efforts have been made over the past decades to understand the genetic, molecular, and cellular basis of the consequences of smoking on the immune system, knowledge has been impaired by conflicting results, which are associated with differences in the experimental models (human vs. animal, and in vivo vs. in vitro), composition of tobacco-smoking (all vs. fractionated smoking), and duration of smoking (acute vs. chronic exposure), and variations may also be related to gender and ethnicity of the subjects in the clinical studies. A direct effect of carcinogens and cytotoxic substances circulating systemically, resulting in DNA and tissue damage, can explain many of the consequences of chronic smoking; however, the indirect consequences of exposure should also be considered. Several lines of evidence suggest that many of the adverse systemic consequences of chronic smoking might be due to its effects on oxidative stress and the immune–inflammatory system. This review will focus on the effects of smoking on the immune–inflammatory system, discussing the biological mechanisms that have recently been implicated in the smoking-induced suppression of the immune and inflammatory systems.
Effect of smoking on systemic and periodontal inflammation
The concept that tobacco smoking may negatively affect systemic and periodontal health is not recent. An overwhelming body of evidence from cross-sectional and longitudinal studies, which will not be the focus of this review, has established tobacco smoking, mostly in the form of cigarette smoking, as the most important environmental risk factor in the development and progression of various forms of periodontal disease. Over the last 15 years, there have been excellent reviews that have addressed the biological basis and pathogenic mechanisms, in addition to clinical and epidemiological aspects, by which tobacco smoking impacts on periodontal homeostasis [2–4]. This section of the present review will focus on recent data that address specific mechanisms by which tobacco smoking may primarily affect systemic and periodontal inflammation. Before starting the discussion itself, it seems important to briefly emphasize the different nature of tobacco exposure in the periodontal tissues and oral cavity. There are two types of tobacco exposure for individuals who use tobacco as a smoking product, which are chronic and acute smoke exposure. While the low concentration of tobacco found in chronic exposure may have one type of effect on the host response, the much higher concentrations reported for acute exposure may impact differently on the immune response. Similarly, the complexity of the composition of tobacco smoke (2,000–3,000 toxic substances) represents a challenge for understanding the wide spectrum of interactions between tobacco smoking and the host immune response. For instance, a tobacco component may have both destructive and protective actions on the host response. The challenge of developing a review describing the complex interactions between the host and the smoking factors led us to organize this section of the paper into a series of subjects that will help to guide readers through the complexities of the host response to tobacco smoking.
Effect of smoking on neutrophils
Neutrophils are the primary inflammatory cells and contribute significantly to phagocytosis in clearing of microbes. Exposure to cigarette smoke leads to increased influx of macrophages and neutrophils in the airways; however, it reduces the ability of those cells to respond to stimuli, phagocytose, kill pathogens, and secrete cytokines [5, 6]. This augmentation of neutrophils in smokers causes increased levels of proteolytic enzymes (neutrophil elastase, proteases-3). Cigarette smoke also inhibits cellular adhesion, disturbs glycolysis and arachidonic metabolism, and inhibits calcium and magnesium ATPase [7]. Tissue damage and oxidative stress, associated with smoking, are considered the main causes for increased numbers of neutrophils. Oxidative stress causes elevated concentration of cytokines which are capable of neutrophil polymorphonuclear activation, and which prolong the life of these cells [8]. The main chemo-attractants for these cells are interleukin (IL)-8 and leukotriene B4 and the adhesion molecules MAC1/ICAM1 that seem crucial for neutrophil migration [9]. However, a recent study demonstrated that nicotine also stimulates neutrophil IL-8 production via nicotinic acetylcholine receptors by generating peroxynitrite and subsequent nuclear factor-kappa B (NF-κB) activation, contributing to leukocytosis in tobacco smokers [10]. Neutrophil function, such as chemotaxis, glycolytic activity and interaction with particles (zymosan), is significantly affected by cigarette smoke. Exposure to smoke makes neutrophils lose their ability to generate respiratory burst in the phagosome, which makes these cells less effective against bacteria and more noxious towards surrounding tissues [11]. When neutrophils from healthy non-smoking individuals are incubated with nicotine, the ability of these cells to promote phagocytosis is compromised. This is in part related to a decrease in the ability of the neutrophils to form actin filaments due to interference in calcium signaling [12]. Some studies indicated that neutrophils from smokers exhibited enhanced oxygen metabolism and dysfunctional regulation of extracellular proteases. Cigarette smoke and neutrophils are potential sources of reactive oxygen intermediates. These molecules can oxidize and thereby inhibit the activities of the protease inhibitors (α1-PI) that normally control tissue destruction [13].
In terms of periodontal disease, tobacco smoke exposure does not seem to affect the number of neutrophils in the periodontium. In fact, the majority of studies have reported either no major differences in neutrophil numbers in the periodontal pocket [14] or a decreased number of neutrophils reaching the gingival sulcus [15]. While impaired chemotaxis has been reported for neutrophils [16], Ryder et al. [17] suggested that smoking may stimulate the migration of neutrophils into the periodontal connective tissue from blood vessels by up-regulating the expression of adhesion integrins (CD11/18 integrin) and down-regulating the surface expression of selectins (L-selectin). In a recent study, Güntsch et al. [18] evaluated the influence of smoking on the number and function of polymorphonuclear neutrophils in periodontally healthy smokers and non-smokers. Crevicular washings were obtained and data analysis demonstrated that the number of neutrophils was higher in light (<5 cigarettes/day) and moderate (5–15 cigarettes/day) smokers and was lower in heavy (>15 cigarettes/day) smokers. Furthermore, they found that neutrophils’ viability and ability to phagocytose were lower in smokers regardless of smoking status. It has further been suggested that smoking may shift the net balance of neutrophil activities in a more destructive direction in the periodontium by increasing the proteolytic activity of neutrophils [19]. While the tobacco-induced release of proteolytic enzymes from neutrophils has not been demonstrated definitively in the periodontal tissues themselves, Söder et al. [20] and Persson et al. [21] observed that smokers had higher functional elastase activity in the gingival crevicular fluid than non-smokers with severe periodontal diseases.
Effect of smoking on macrophages
Macrophages serve as the first line of cellular defense against pollutants and elimination of microbial agents, due to their antigen presentation function and phagocytic properties. Cigarette smoking increases the number of alveolar macrophages [1] and activates them to produce pro-inflammatory mediators, reactive oxygen species and proteolytic enzymes [22], thereby providing a cellular mechanism that links smoking with inflammation and tissue damage. The number of macrophages is increased (2–3-fold) in bronchoalveolar lavage of smokers, and exposure to cigarette smoke also changes macrophage phenotype. In general, macrophages obtained from tobacco smokers are less mature, have elevated expression of CD14, have a condensed cytoplasm, and are hyperdense [23]. The phagocytic function of macrophages is significantly reduced by cigarette smoke [24]. Local levels of inflammatory mediators have also been reported to be significantly affected by smoking. After acute smoke inhalation, the local levels of tumor necrosis factor (TNF)-α, macrophage inflammatory proteins (MIPs) and monocyte chemoattractant protein (MCP)-1 released by macrophages are increased, while leukotriene B4, another important chemoattractant, decreases directly after acute exposition [25]; this may explain a reduced immune response to infectious agents in smokers. Cigarette smoke compromises the ability of alveolar macrophages to phagocytose bacteria [26] and apoptotic cells [24], and to sense pathogen-associated molecular patterns (PAMPs) [27, 28]. It is conceivable that decreased expression of pro-inflammatory mediators in response to Toll-like receptor (TLR) stimulation is the result of an altered activation threshold due to repeated activation of the corresponding pathway by cigarette smoke. Macrophages of smokers had a decreased surface expression of TLR2 compared with non-smokers [29]. Karimi et al. [30] found that neutralization of TLR4 but not TLR2 inhibits cigarette smoke medium-induced IL-8 secretion by human macrophages and concluded that the mechanism underlying IL-8 production by human macrophages after cigarette smoke medium exposure involves activation of TLR4-specific signaling pathways. Evidence suggests that acute smoke-induced pulmonary inflammation is mediated through TLR4 and myeloid differentiation primary-response gene 88 (MyD88)-dependent pathways, probably following the induction of the TLR4 agonist heat-shock protein 70 [31]. In addition, Sarir et al. [32] showed that cigarette smoke-induced oxidative stress was involved in modulation of TLR4 mRNA and surface protein expression as well as the cascade of TLR4 signaling pathways and cytokine production. Recently, the immune response of cord blood monocytes obtained from neonates of smoking and non-smoking mothers has been examined. It was showed that infants of smoking mothers had a significantly attenuated innate TLR-mediated response in monocytes compared with infants of non-smokers [33]. Furthermore, smoking seems to cause regional immunosuppression of alveolar macrophages’ reactivity to TLR2 and TLR4 agonists, manifested by impaired gene expression and secretion of pro-inflammatory cytokines (TNF-α, IL-1β, and IL-6) and chemokines (IL-8 and RANTES) [27]. The incidence of respiratory tract infections is increased in cigarette smokers, indicating that the immune response to microorganisms may be compromised. In a mouse model of Pseudomonas aeruginosa lung infection, it was found that cigarette smoke impaired bacterial clearance leading to increased inflammation and morbidity related to epithelial damage and inflammation [34]. Together, these studies suggest that smoking may switch the alveolar macrophage inflammatory response towards to a more harmful pattern.
Effect of smoking on natural killer (NK) cells
NK cells, lymphoid cells that play essential roles in the innate host defense against microbial infections and tumor surveillance, are also modulated by smoking [1]. Several studies have shown that NK cell numbers and activity are decreased in smokers compared with non-smokers. Exposure to cigarette smoke attenuates the cytotoxic activity and cytokine production of NK cells in humans and mice [35]. It has been shown that NK cells isolated from smokers may display a significant reduction in interferon (IFN)-γ and TNF-α synthesis compared with non-smokers, and that cigarette smoke attenuated NK cell cytotoxic activity, which was associated with decreased perforin expression. These data were confirmed in animal models, where suppression of NK activation and attenuation of NK activity by cigarette smoke were associated with increased indices of tumor development and high numbers of lung metastases, thereby linking NK cell defects to increased infection risk and cancer. It has recently been suggested that this is, at least in part, due to defective NK cell function in smokers, increasing the re-emergence of cervical cancer metastases [36].
Effect of smoking on dendritic cells
Dendritic cells (DC) are potent antigen-presenting cells and indispensable for initiating the cell-mediated immune response. The number of DC has been shown to be decreased in smokers [37, 38]. Clinical studies suggest that the number of mature DC is reduced in the large airways of patients with chronic obstructive pulmonary disease (COPD) who smoke [39]. Following smoking cessation, the number of mature DC increases and is similar to non-smoking healthy controls. In contrast, the number of immature DC is increased in the small airways of patients with COPD compared with individuals who have never smoked and individuals who smoke but do not have COPD [40]. DC differentiated in a nicotinic environment have been shown to produce higher amounts of IL-10, to display an altered ratio of co-stimulatory molecules, and to fail to produce polarizing IL-12, reducing T-cell stimulation and Th1 differentiation [37]. Similarly, Tsoumakidou and collaborators [38] demonstrated that both cigarette smoke extract and nicotine have a dose-dependent effect on DC maturation, suppressing their T-cell stimulatory capacity and reducing their stimulatory Th1-cell polarization. In a time-course study in mice, D’Hulst et al. [41] revealed that DC of smoke-exposed mice showed up-regulation of major histocompatibility complex (MHC) class II molecules and co-stimulatory molecules CD40 and CD86, compared with DC of air-exposed mice, supporting the predominant increase of CD4+ cells rather than CD8+ cells. Together, these studies indicate that the immunosuppressive effect of smoking is, at least in part, due to its direct effect on the number, maturity state and activity of DC, reducing the activation of CD8+ T cells.
Effect of smoking on eosinophils
Eosinophils are multifunctional leukocytes that play a key role during allergic inflammation. Besides inflammatory proteins, eosinophils secrete mediators like eotaxin and leukotrienes that might enhance chemotaxis. Cigarette smoke increases the percentage of eotaxin-positive cells in smokers as compared with non-smokers [42]. Furthermore, an elevated proportion of eosinophils has been found in sputum of active smokers with COPD compared with ex-smokers [43]. Recently, it was significantly elevated proportions of cells positive to eosinophil peroxidase were found in biopsies of healthy smokers compared with non-smokers [44]. The influx of eosinophils into airways of smokers seems to be a rapid reaction, and the number of these cells normalizes after smoking cessation in asymptomatic smokers and in patients with COPD [43]. Theses findings suggest that eosinophils may play an important role in the inflammatory pathway in smokers.
Effect of smoking on mast cells
Mast cells are implicated in a variety of inflammatory responses due to their ability to degranulate upon activation, releasing cytoplasmic stores of cytokines, proteases, histamine, and heparin. Cigarette smoke increases the absolute number of mast cells in smokers [45]. Furthermore, smoking promotes expression of the chemokines MIP-1α and MIP-2 by mast cells, suggesting that mast cells can promote and prolong the local inflammatory process in the lungs of smokers [46]. In contrast, several studies have shown that cigarette smoke may reduce allergic activation of mast cells, resulting in decreased degranulation and cytokine production (TNF-α and IL-6). These effects seem to be mediated by the NF-κB signal transduction pathway and, possibly, through the ATF-1 transcription factor. However, further studies should be considered in order to determine to what extent the inhibitory effect of cigarette smoke on the activation of mast cells contributes to a decrease in allergic symptoms in smokers [47].
Effects of smoking on B lymphocytes
B lymphocytes are generated throughout life by differentiation from hematopoietic stem progenitors. At the mature stage, they possess a system that can sense the presence of microorganisms and contribute to their destruction. In addition to secreting immunoglobulins (Igs), B cells are able to present antigen (Ag), up-regulate co-stimulatory molecules, express anti-microbial activity by producing reactive oxygen intermediates and other inflammatory cytokines, and secrete factors that can directly mediate microbial destruction [48]. It has been hypothesized that smoke may impair host defense by reducing the proliferation and activity of B cells [1]. It is well recognized that one common feature of smokers is that they have decreased serum levels of Is. Earlier studies and more recent ones, such as Gonzalez-Quintela et al. [49], demonstrated that serum IgG levels were significantly lower in smokers than in non-smokers. Interestingly, the reduction in serum IgG seems to be due to a reduction in IgG2, since neither IgG1 nor IgG3 concentrations appear to be affected by smoking. Furthermore, multivariate analyses have demonstrated that IgG levels, which can be modulated by aging, gender, and systemic disorders, are independently associated with smoking. On the other hand, serum levels of IgA and IgM in smokers are not significantly different from those of non-smokers [49].
In terms of the effect of smoking on humoral immunity in periodontal patients, Quinn et al. [50] reported depressed serum levels of IgG2 in white periodontally healthy and generalized aggressive periodontitis subjects, whereas only black subjects with generalized aggressive periodontitis showed a significant reduction in IgG2 serum levels. IgG1 and IgG3 serum levels were not affected in either black or white subjects. Tangada et al. [51] reported much lower concentrations of IgG2 antibody in serum from smokers than non-smokers presenting generalized aggressive periodontitis. Later, Quinn et al. [50] found that white subjects, including chronic periodontitis subjects, have substantially less IgG2 in their serum than black subjects, whereas no significant reduction in IgG2 was observed in black subjects with chronic periodontitis. In addition, serum IgG1 and IgG4 levels suffered a reduction in black smokers with chronic periodontitis. Graswinckel et al. [52] showed that non-smoker periodontitis patients had higher plasma levels of total IgG and IgG2 than smokers with periodontitis. In a recent investigation, Al-Ghamdi and Anil [53] assessed the alterations of serum immunoglobulin levels in smokers with periodontitis. Data analysis demonstrated that IgG and IgA serum levels were significantly lower in smokers compared to non-smokers and healthy controls; and that IgM serum levels tended to be lower in smokers. Furthermore, of the four subclasses of IgG investigated (IgG1, IgG2, IgG3, IgG4), IgG2 was found to be significantly lower among smokers diagnosed with periodontitis.
Recently, Zavitz and collaborators [54] demonstrated no impairment on proliferation or calcium flux generation in cultured B cells from stimulated lymph node and spleen from smoke- and sham-exposed animals. In addition, the authors demonstrated that cells from smoke- and sham-exposed mice secreted equivalent amounts of IgG, suggesting that B-cell responses may be impaired not by a direct effect of smoke but rather by an effect on cells of the innate immunity, which activated them. In support of this evidence, alveolar macrophages from chronic smoke-exposed mice significantly inhibited B-cell proliferation stimulated with bacterial lipopolysaccharide (LPS) compared with macrophages from non-chronic smoke-exposed mice. Generation of superoxide and hydrogen peroxide was significantly increased in chronic smoke-exposed macrophages compared with non-chronic smoke-exposed macrophages, and inhibition of B-lymphocyte proliferation stimulated with LPS by macrophages from chronic smoke-exposed mice was clearly recovered by addition of superoxide dismutase and catalase, suggesting that the inhibition by chronic smoke-exposed macrophages of LPS-induced B-lymphocyte proliferation may be caused by the increased superoxide and hydrogen peroxide generation of chronic smoking [55]. Collectively, these observations suggest that the immunosuppressive effects of smoking on B lymphocytes are indirect and related to smoke-induced altered function of cells of the innate immune system.
Effect of smoking on T lymphocytes
T lymphocytes (T cells) are the main cell type involved in cell-mediated immunity, and these cells display extensive diversity in terms of phenotype, function, and anatomical distribution. In general, activation through T-cell receptors results in proliferation and the acquisition of a variety of effector functions that ultimately produce an array of effectors and memory cell types. These cells differ in their capacity to proliferate in response to antigen, mediate cytotoxic responses, and execute regulatory functions. T cells differentiate into several different subsets, including CD8+ T cells (cytotoxic T cells), which act to kill cells infected with intracellular microbes, and CD4+ T cells (helper T cells), which regulate cellular and humoral immune responses. Inhibition of T-cell proliferation with consequent reduction on cellular function is a mechanism associated with smoke-induced immunosuppression and impaired host defense [56]. Indeed, it is consistent in the literature, in both human and animal models, that smoke reduces proliferation of T cells and alters CD4+ and CD8+ cells [57]. T-cell activation, proliferation, and expression of the cytotoxic proteins granzyme-b and TIA-1 were significantly reduced in response to cigarette smoke extract [58]. In addition, the same effects observed on B cells by Zavitz and collaborators [54] were found in T cells from lung, lymph node, and spleen of smoke-exposed animals. Moreover, several studies have demonstrated that smokers have an increased CD8+ T cell count, altering the CD4+/CD8+ ratio compared with non-smokers [6]. In mixed-leukocyte reaction assay, cigarette smoke-primed dendritic cells potentiate CD8+ T-cell proliferation via CCL3, whereas proliferation of CD4+ T cells is suppressed via an unknown mechanism [47]. The effect of smoke on T cells of children exposed to passive smoke were examined by Avanzini et al. [59], revealing that children who were exposed to passive tobacco smoke had a significantly lower percentage of IFN-γ-producing CD4+ and CD8+ cells in the adenoids. Moreover, there was a significant correlation between the quantity of exposure and reduction in Th1 (CD4+IFNγ+ and CD8+IFNγ+) cells in adenoids, adding a possible explanation for the increased susceptibility of children exposed to passive smoking to develop respiratory tract infections. Interesting, smoking affects several immune parameters leading to immunosuppression in pregnant women at 14–20 weeks gestation, including increase in the frequency of CD3+ lymphocytes and decrease in CD56+ cells [60].
Although there is a number of studies reporting different findings regarding T lymphocytes in smokers, very limited information is available regarding the effect of smoking on T cells in the periodontal environment. Orback et al. [61] evaluated changes in T lymphocytes in smokers and non-smokers. They found that lymphocyte values observed for smokers were lower than those in non-smokers and this difference was statistically significant after periodontal treatment. Loos et al. [62] examined 112 adults, 76 with periodontitis and 36 control subjects. Subjects were classified into non-smokers, light smokers (those who smoked <10 cigarettes/day) or heavy smokers (≥10 cigarettes/day). It was found that a more severe periodontal breakdown in smokers was associated with a higher number of CD3+ T cells, as well as CD4+ and CD8+ T-cell subsets, and increased T-cell proliferation, whereas the number of B cells was not affected by smoking. Taken together, the current data suggest that the main effects of smoke on T cells are reductions in their proliferation and alterations in the specific subpopulations of CD4 + and CD8+ cells.
Effect of smoking on other cell types
Among several effects, cigarette smoking decreases expression of several genes that regulate airway inflammation in bronchial airway epithelial cells [63]. Indeed, studies have revealed that smoke extracts or whole smoke alter the production of inflammatory mediators, including IL-1β, IL-6 and IL-8, by airway epithelial cells [64]. Floreani and collaborators [65] showed that human bronchial epithelial cells constitutively express C5a receptors and that cell-surface C5a receptor expression is increased in the cells upon exposure to cigarette smoke extract. In addition, initial exposure of bronchial epithelial cells to cigarette smoke extract followed by treatment of the cells with C5a resulted in a significant increase in the release of IL-8 compared with cells exposed to cigarette smoke extract or C5a alone. Later, this same group demonstrated that cigarette smoke modulated the responsiveness of airway epithelial cells to C5a by up-regulating C5a receptor numbers on the cell surface, which is beneficial in the recruitment of neutrophils and lymphocytes in response to smoke [66]. Furthermore, exposure of primary human epithelial cells to cigarette smoke extract significantly reduced vascular endothelial growth factor production, modulating the cellular enviroment and the inflammatory response [67]. It has been suggested that cigarette smoke may impair the innate antiviral defense in human fibroblasts and epithelial cells through decreased expression of INF-stimulated gene, exposing smokers to an increased burden of viral infection [68].
Smoking has also been described to alter endothelial cell function, leading to an increased risk of cardiovascular diseases, and endothelial dysfunction induced by smoke may also modulate the responses of immune and inflammatory cells. Impairment of nitric oxide (NO) production and increase in oxidative stress by a large number of free radicals known to exist in smoke are two of the main mechanisms responsible for acute endothelial dysfunction observed in smokers. Since NO production from endothelial cells is reduced, the burden of reactive oxygen species is increased, which is able to induce cell damage and infiltration of inflammatory cells. Evidence also suggests that NO may directly affect immune and inflammatory cells.
Gingival and periodontal ligament fibroblasts have been used in in vitro studies to assess the effects of components of tobacco smoke, such as acrolein, acetaldehyde, nicotine, and cotinine. Overall, the data published to date have shown a detrimental effect on these cell lines, including disruption of cell orientation, inhibition of cell proliferation, cytoplasmic vacuolation and attachment, inhibition of collagen production, and reduction in cell viability [69]. In contrast to these findings, Peacock et al. [70] showed a positive effect of nicotine on the proliferation and attachment of gingival fibroblasts to culture dishes. Additionally, treatment of human gingival fibroblasts with nicotine has been shown to modulate cyclooxygenase (COX)-2 protein expression (Ho and Chang [71]). Zhou et al. [72] assessed the effects that nicotine in combination or not with P. gingivalis supernatant had on human gingival fibroblast-mediated collagen degradation. They found that nicotine increased human gingival fibroblast-mediated collagen cleavage. MMP-14 and MMP-2 produced by nicotine-treated human gingival fibroblasts more readily underwent zymogen activation, and, additionally, nicotine treatment resulted in tissue inhibitor of metalloproteinase (TIMP)-2 redistribution to the cell surface. An additive collagen cleavage effect was observed when human gingival fibroblasts were treated with both nicotine and P. gingivalis. More recently, cigarette smoke condensate has been shown to stimulate urokinase production and plasmin activation in human gingival fibroblasts [73]. Although most of these studies used higher concentrations in vitro than those expected in plasma of smokers, the evidence might lead one to believe that tobacco smoking impacts on the inflammatory process in the periodontium through its effect on fibroblasts. Table 2 summarizes the main findings regarding the effect of smoking on inflammatory cells in periodontal sites.
Effect of smoking on immune–inflammatory mediators
Immune and inflammatory cells produce a great variety of inflammatory mediators in response to smoking, which can have both local and systemic effects, since some are detected at high levels in the plasma of smokers. Wannamethee and colleagues [74], in a large-scale analysis with more that 2,920 subjects, found that, compared with never smokers, cigarette smokers have significantly higher levels of C-reactive protein (2.53 vs. 1.35 mg/L), white cell count (7.92 vs. 6.42 × 109/L), and fibrinogen (3.51 vs. 3.13 g/L). Other studies confirmed significant higher levels of C-reactive protein in the plasma of smokers compared with non-smokers, and also demonstrated elevated levels of IL-6, a traditional marker of inflammation [75]. Helmersson et al. [76] did not find differences in the plasma levels of C-reactive protein between smokers and non-smokers. However, these authors demonstrated increased plasma levels of IL-6 and prostaglandin F2α. Together, these data from large-scale population-based studies show a strong association between smoking and various markers of systemic inflammation in men. Most important, these studies point to a possible mechanism for several of the adverse effects of smoking, such as elevated risk for infections and cardiovascular diseases. Local levels of inflammatory mediators are also modulated by smoking. As previously mentioned in this review, local levels of TNF-α, MIPs and MCP-1 released by macrophages are increased, while leukotriene B4, another important chemoattractant, decreases directly after acute exposure to cigarette smoke [25]. Levels of mRNA for IL-6, IFN-γ, TNF-β, IL-13, and chemokines CCL5, CCL3, CCL4, and CCL20 were significantly lowered in bronchoalveolar lavage cells of smokers compared with never-smokers [77]. Another proof that smoking affects cytokine content was demonstrated by Mishra et al. [78], who showed that nicotine dramatically suppresses mRNA and protein expression of the Th2 cytokines/chemokines IL-4, IL-5, IL-13, IL-25 and eotaxin, leukotriene C4, and total as well as allergen-specific IgE [78]. A recent study showed that cigarette smoke extract induces the release of CCL3 and CXCL2 in a reactive oxygen species-dependent manner in denditic cells but does not alter the production of TNF-α, IL-2, IL-6, IL-10, IL-12p70, MCP-1, and IFN-γ, and even suppressed the production of these cytokines induced by LPS [47].
In relation to the pathogenesis of periodontal disease, there is a general concept that local levels of pro- and anti-inflammatory cytokines will be modulated during periodontal disease, and that cytokine production would therefore play a pivotal role in directing the status of the disease. Although of relevance to the field, the effect of smoking on cytokine production in periodontal patients has scarcely been investigated. Bostrom et al. [79] showed higher levels of TNF-α in the gingival crevicular fluid in smokers and former smokers compared with non-smokers with comparable levels of moderate/severe periodontitis. On the other hand, Erdemir et al. [80] found that smoking did not influence IL-6 and TNF-α levels in gingival crevicular fluid contents of patients with chronic periodontitis. Others cytokines, such as IL-1β and IL-1ra (receptor antagonist), were also evaluated by Bostrom et al. [81] in non-smokers versus smokers with moderate to severe periodontal disease. They reported no influence of smoking on the levels of IL-1β and IL-1ra in gingival crevicular fluid. In contrast, Rawlinson et al. [82] found levels of IL-1β and IL-1ra to be lower in diseased sites in smokers versus non-smokers. In an in vitro study, Almasri et al. [83] investigated the influence of nicotine alone and a combination of nicotine with LPS on cytokine expression from human gingival fibroblasts using protein arrays. They found that nicotine significantly increased the expression of growth-regulated oncogene-alpha, IL-7, IL-10, and IL-15 compared to the untreated control, and that when nicotine was combined with LPS, an additional effect was seen on the levels of RANTES and INF-γ. In order to further investigate the events involved in the modulation of cytokine production by smoking, our group has simultaneously assessed the profile of a number of pro- and anti-inflammatory cytokines plus pro- and anti-resorptive agents in the gingival tissues of smokers versus non-smokers with moderate to severe chronic periodontitis, including IL-1β, IL-1ra, IL-6, IL-8, IL-10, INF-γ, TNF-α, MMP-2 and -8, receptor activator of NF-κB ligand (RANKL), and osteoprotegerin (OPG) [84, 85]. In general, data analysis demonstrated that mRNA levels of IL-1β, IL-8, IL-10, TNF-α, MMP-8, and OPG were lower in the gingival tissues of smokers than non-smokers with comparable types of periodontitis, while IL-6, INF-γ, and IL-1ra were higher. Increased RANKL:OPG and IL-6:IL-10 ratios were found in sites with periodontitis in smokers versus non-smokers. In a recent study, Torres de Heens et al. [86] compared the pro-inflammatory cytokine production in ex vivo whole blood cell cultures of smoking and non-smoking chronic periodontitis patients. The results demonstrated that smokers showed a lower IL-12 p40:IL-10 ratio than non-smokers. IL-1β production was significantly lower in smokers compared with non-smokers after stimulation, and IL-6 and IL-8 production was similar in both smokers and non-smokers. A list of the main findings on the effect of smoking on inflammatory mediators in the pulmonary and extra-pulmonary environments, and in periodontal patients, is shown in Tables 1 and 2, respectively.
Effect of smoking on the molecular mechanisms of cytokine production
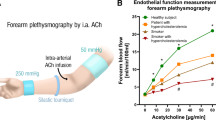
The molecular mechanisms behind the smoking-induced expression, production, and release of cytokines by inflammatory cells are starting to be revealed. They involve activation of IKK (inhibitor of IκB kinase), phosphorylation of IκB (inhibitor of NF-κB), NF-κB nuclear translocation, and histone acetylation [87–89]. NF-κB is found in the cytoplasm in an inactive state, associated with its inhibitory protein IκB. Activation of IKK, which induces proteasomal degradation of IΚB, unmasks the nuclear localization signal of NF-κB, permitting it to enter the nucleus, bind DNA, and initiate gene transcription, is considered to be the classic pathway of NF-κB activation [90]. IKK is a kinase complex composed of three subunits, IKK-α (IKK1) and IKK-β (IKK2) that are bona fide kinases, and IKK-γ (NEMO) that has no catalytic activity but plays a critical regulatory role [91]. IKK can be activated by several factors, but the most potent are the pro-inflammatory cytokines TNF-α and IL-1 [92]. However, gene transcription is not only dependent on transcription factor binding to DNA, but also on alterations in the structure of chromatin. Histone modifications such as acetylation, realized by histone acetylases (HAC), and deacetylation, performed by histone deacetylases (HDAC), facilitate or block the accessibility of DNA to transcription factors and co-factors respectively, regulating gene expression. NF-κB, like many other transcription factors, relies on the lysine acetylation of histones by HACs, in particular CBP/p300, to initiate DNA unwrapping and allow accessibility for binding. Moreover, several reports demonstrated that changes in HDAC activity might also enhance or repress NF-κB-mediated gene transcription [93]. Numerous studies have linked NF-κB activation to regulation of cytokine expression in smokers. IΚB-α levels were significantly decreased in smokers and ex-smoking patients when compared with non-smokers, with an associated increase in NF-κB DNA binding in current smokers [88]. Di Stefano and colleagues [94] demonstrated increased expression of NF-κB in bronchial tissue from smokers and from patients with COPD. Likewise, Yagi et al. [95] demonstrated by immunohistochemistry that airway epithelial cells from ex-smokers with or without COPD also have elevated activation of NF-κB, since increased phosphorylated IκB-α was found. Although most of the studies have demonstrated that increased NF-κB activation is dependent on IKK activation, Zhao et al. [96] showed a novel mechanism of NF-κB activation modulated by tobacco smoke. These authors revealed that in A549 cells, a human lung cancer cell line, tobacco smoke exposure significantly induces the microtubule-associated protein kinase (MAPK) signaling pathway via activation of extracellular signal-regulated kinases 1 and 2 (ERK1/ERK2), resulting in direct IκB phosphorylation and NF-κB activation. Recently, some studies have shown that NF-κB activation can be independent of IKK, when induced by reactive oxygen and nitrogen species produced by smoking-induced oxidative stress [87, 89]. In addition, a recent study demonstrated that IKKα activation trigged by cigarette smoke might directly activate the RelA/p65 subunit of NF-κB and promote acetylation of histones H3 and H4 [97]. These authors demonstrated that, in response to cigarette smoke, IKKα is phosphorylated at ser176/180 residue, leading to direct activation of NF-κB by acetylation of RelA/p65 at lys310 and direct phosphorylation/acetylation of specific histones H3 and H4 on promoters of pro-inflammatory cytokines, including IL-6 and MIP-2. Expression and activity of HDAC2 is decreased in smokers and in patients with COPD, and there is a correlation between cytokine production and HDAC activity in alveolar macrophages from smokers and non-smokers [88]. Likewise, decreased HDAC2 expression and activity was observed in rat lungs exposed to cigarette smoke [98]. In addition, cigarette smoke extract-mediated reduction in HDAC2 was associated with increased RelA/p65, indicating that RelA/p65 interacts with HDAC2 and RelA/p65 becomes available or is retained in the nucleus for pro-inflammatory gene transcription when HDAC2 is decreased [89]. Recently, in another independent study, Yang et al. [97] demonstrated that in MonoMac 6 cells cigarette smoke extract exposure causes dose- and time-dependent decreases in the production and activity of sirtuin 1, a member of the class III histone/protein deacetylase family, which was concomitant to increased NF-κB-dependent IL-8 and TNF-α secretion. A model summarizing smoking effects on inflammatory cytokine gene transcription is depicted in Fig. 1. Besides NF-κB, Zhao et al. [96], using a protein/DNA array approach, identified 19 other transcriptional factors regulated by tobacco smoke. Among these are GATA, PAX5, and Smad 3/4 that were significantly stimulated by tobacco smoke, and ISRE and ICSBP that had their DNA-binding activities significantly decreased after tobacco smoke treatment. Smoke can also trigger inflammation via AP-1 activation, resulting in pro-inflammatory gene overexpression [99]. Smoking-induced cytokine expression is thus a complex and multi-step process with the participation and cooperation of multiple signaling pathways.
A model for the pathological effects of smoking on transcriptional control of inflammatory genes via NF-κB activation. In an inactive state, NF-κB, the heterodimeric complex formed by p50 and p65, is found in association with IκB in the cytoplasm. Proteasomal degradation of IκB is the key event for NF-κB activation, translocation into the nucleus, DNA binding, and recruitment of HACs, leading to the expression of inflammatory cytokines. Smoking can modulate activation of NF-κB in many ways: (1) activation of IKK by IL-1 and TNF-α, resulting in IκB degradation, (2) NF-κB activation via Toll-like receptors associated with smoking oxidative stress and ERK1/ERK2 MAPK signaling pathway activation, (3) activation of IKK by smoking, resulting in stimulation of p65 subunit acetylation, and (4) smoking-induced reduction of HDAC expression and activity, leading to prolonged NF-κB activation. IL interleukin, TNF-α tumor necrosis factor-α, ERK extracellular signal-regulated kinase, NF-κB nuclear factor-kappa B, HACs histone acetylases, IκB inhibitor of NF-κB, IKK inhibitor of IκB kinase, HDACs histone deacetylases
Nicotine and anti-inflammatory effect
The cholinergic anti-inflammatory pathway has been identified as a major modulator of immune cell function in a wide variety of inflammatory disease states [100]. The physiological activation of the cholinergic anti-inflammatory pathway occurs through the parasympathetic nervous system which induces the release of acetylcholine (ACh) [100–102]. A recent study found that ACh reduced the secretion of IL-6, IL-8, MCP-1, MIP-1, and CCL5 (RANTES) in rheumatoid arthritis [103]. Nicotine, like ACh, is a nicotinic cholinergic agonist that binds to and activates nicotinic acetylcholine receptors [104], and also exerts anti-inflammatory activities in vitro and in vivo [101, 105–107]. Wang et al. [105] were the first authors to identify which nicotinic acetylcholine receptor (nAChR) subunit responds to nicotine treatment by inhibiting cytokine synthesis. They investigated whether the alpha7 subunit was essential for the cholinergic anti-inflammatory pathway in vivo by measuring TNF-α production in alpha7 knockout mice. After administration of endotoxin, the serum TNF-α level was significantly higher than in wild-type mice (18.1 vs. 8.0 ng/mL). Next, Wang et al. [105] observed that macrophages derived from alpha7 knockout mice were refractory to cholinergic agonists, and produced TNF-α normally in the presence of nicotine or acetylcholine. Mabley et al. [106] evaluated the effects of activating the cholinergic anti-inflammatory pathway with exogenous nicotine on acute lung inflammation induced in mice. The results demonstrated that nicotine treatment reduced the LPS-mediated infiltration of leukocyte in alveolar spaces, and myeloperoxidase activity. Nicotine also down-regulated lung production of pro-inflammatory chemokines (MIP-1α, MIP-2, and eotaxin) and cytokines (IL-1, IL-6, and TNF-α). Recently, Zhou et al. [107] investigated the anti-inflammatory role of nicotine in rheumatoid arthritis fibroblast-like synoviocytes cells (FLS). They found that TNF-α-induced secretion of IL-6 and IL-8 in FLS cells was significantly reduced by pre-incubation with low concentrations of nicotine (0.1–100 μM). Furthermore, Zhou et al. [107] demonstrated that nicotine exerts an anti-inflammatory in FLS cells by inhibiting TNF-α-induced nuclear translocation of NF-κB. Although these studies have addressed the potential immune-suppressant effect of nicotine, Breivik et al. [108] demonstrated that chronic treatment with nicotine enhanced the progression of ligature-induced periodontitis, and LPS-provoked pre-treatment with mecamylamine, an antagonist of alpha7 nicotinic acetylcholine receptor, significantly reduces periodontal bone loss. Breivik et al. [108] further assessed serum levels of pro-inflammatory (TNF-α) and anti-inflammatory and T-regulatory cytokines (TGF-β1 and IL-10) in rats exposed to LPS. The authors found lower TNF-α, TGF-β1, and IL-10 serum levels in nicotine-treated rats, indicating that nicotine enhances susceptibility to periodontitis via nAChRs, which may act by suppressing protective immune responses through the cholinergic anti-inflammatory pathway. Thus, the mechanism through which nicotine may activate the intracellular anti-inflammatory pathway as well as the pharmacological concentrations of nicotine that inhibit pro-inflammatory mediators need still to be clarified.
Overall conclusions
Cigarette smoke has a major impact on health issues worldwide. The possible biological mechanisms responsible for the observed association of smoking with various diseases and global mortality are numerous and, in spite of many attempts to find causal relationships, are still unclear. Due to space limitations and to the wide range of evidence in this field, this review article focused on summarizing well-known concepts and exploring recent developments over the last 5 years. A number of laboratory models have been designed to investigate the various aspects of smoking behavior and nicotine-dependence phenomena. In vitro, different cell types have been exposed to single or multiple components of cigarette smoke, cigarette smoke extract and cigarette smoke as a whole. In vivo, experimental models usually included the administration of smoke components (especially nicotine), using different systems (subcutaneous injection, osmotic pumps, etc.), and nasal and/or oral cigarette smoke inhalation. Differences in effects between animals and humans, and between different animal species, may result from biological differences, for example in absorption, distribution, metabolism, and elimination. In addition, the limitations of assessing the biological effect of isolated smoke components versus whole cigarette smoke, and acute or limited exposure in contrast to the chronic exposure that occurs in smokers, has to be taken into account for most laboratory models. Therefore, the lack of animal and human laboratory models with sufficient predictive clinical validity to support the translation of knowledge from laboratory studies into clinical research is an obstacle to the identification of major players regarding the effect of smoking on the immune–inflammatory process, and research to refine models is welcome (see Lerman et al. [109] and Wright et al. [110] for review).
Many related adverse effects of exposure to cigarettes may result from the ability of cigarette smoke to interfere with the immune–inflammatory system towards smoke as an immunosuppressant. Smoking also causes activation of resident cells and the recruitment of inflammatory cells into the lungs, which leads to release of pro-inflammatory cytokines, chemotactic factors, oxygen radicals and proteases, which alter the function of immune cells. The qualitative and quantitative effects of cigarette smoke on the immune system might depend on the duration of smoking, as well as the sex and ethnicity of the subjects who are studied, and therefore the extent of the reported effects of smoking on the immune–inflammatory system varies significantly between studies. Finally, although the effects of smoking on inflammatory markers may persist for many years, the majority of the adverse health effects of smoking is reversible. Therefore, quitting smoking avoids much of the excess health-care risk associated with smoking and allows increasing life expectancy.
References
Sopori M. Effects of cigarette smoke on the immune system. Nat Rev Immunol. 2002;2:372–7.
Barbour SE, Nakashima K, Zhang JB, Tangada S, Hahn CL, Schenkein HA. Tobacco and smoking: environmental factors that modify the host response (immune system) and have an impact on periodontal health. Crit Rev Oral Biol Med. 1997;8:437–60.
Kinane DF, Chestnutt IG. Smoking and periodontal disease. Crit Rev Oral Biol Med. 2000;11:356–65.
Ryder MI. The influence of smoking on host responses in periodontal infections. Periodontol 2000. 2007;43:267–77.
Gualano RC, Hansen MJ, Vlahos R, Jones JE, Park-Jones RA, Deliyannis G, et al. Cigarette smoke worsens lung inflammation and impairs resolution of influenza infection in mice. Respir Res. 2008;9:53.
Martorana PA, Lunghi B, Lucattelli M, De Cunto G, Beume R, Lungarella G. Effect of roflumilast on inflammatory cells in the lungs of cigarette smoke-exposed mice. BMC Pulm Med. 2008;8:17.
Green GM. Mechanisms of tobacco smoke toxicity on pulmonary macrophage cells. Eur J Respir Dis Suppl. 1985;139:82–5.
Kim S, Nadel JA. Role of neutrophils in mucus hypersecretion in COPD and implications for therapy. Treat Respir Med. 2004;3:147–59.
Stockley RA. Neutrophils and the pathogenesis of COPD. Chest. 2002;121:151S–5S.
Iho S, Tanaka Y, Takauji R, Kobayashi C, Muramatsu I, Iwasaki H, et al. Nicotine induces human neutrophils to produce IL-8 through the generation of peroxynitrite and subsequent activation of NF-kappaB. J Leukoc Biol. 2003;74:942–51.
Zappacosta B, Persichilli S, Minucci A, Fasanella S, Scribano D, Giardina B, et al. Effects of aqueous cigarette smoke extract on the chemiluminescence kinetics of polymorphonuclear leukocytes and on their glycolytic and phagocytic activity. Luminescence. 2001;16:315–9.
Ryder MI. Nicotine effects on neutrophil F-actin formation and calcium release: implications for tobacco use and pulmonary diseases. Exp Lung Res. 1994;20:283–96.
Ogushi F, Hubbard RC, Vogelmeier C, Fells GA, Crystal RG. Risk factors for emphysema. Cigarette smoking is associated with a reduction in the association rate constant of lung alpha I-antitrypsin for neutrophil elastase. J Clin Invest. 1991;87:1060–5.
Petropoulos G, McKay I, Hughes F. The association between neutrophil numbers and interleukin-1α concentrations in gingival crevicular fluid of smokers and non-smokers with periodontal disease. J Clin Periodontol. 2004;31:390–5.
Pauletto NC, Liede K, Nieminen A, Larjava H, Uitto VJ. Effect of cigarette smoking on oral elastase activity in adult periodontitis patients. J Periodontol. 2000;71:58–62.
Kraal JH, Chancellor MB, Bridges RB, Bemis KG, Hawke JE. Variations in the gingival polymorphonuclear leukocyte migration rate in dogs induced by chemotactic autologous serum and migration inhibitor from tobacco smoke. J Periodontal Res. 1977;12:242–9.
Ryder MI, Fujutaki R, Lebus S, Mahboub M, Hyum W. Alterations of neutrophil L-selectin and CD18 expression by tobacco smoke: Implications for periodontal diseases. J Periodontol Res. 1998;33:359–68.
Güntsch A, Erler M, Preshaw PM, Sigusch BW, Klinger G, Glockmann E. Effect of smoking on crevicular polymorphonuclear neutrophil function in periodontally healthy subjects. J Periodontal Res. 2006;41:184–8.
Donaldson K, Brown GM, Drost E, Selby C, MacNee W. Does cigarette smoke enhance the proteolytic activity of neutrophils? Ann NY Acad Sci. 1999;624:325–7.
Söder B, Jin LJ, Wickholm S. Granulocyte elastase, matrix metalloproteinase-8 and prostaglandin E2 in gingival crevicular fluid in matched clinical sites in smokers and non-smokers with persistent periodontitis. J Clin Periodontol. 2002;29:384–91.
Persson L, Bergström J, Gustafsson A. Effect of tobacco smoking on neutrophil activity following periodontal surgery. J Periodontol. 2003;74:1475–82.
Russell RE, Thorley A, Culpitt SV, Dodd S, Donnelly LE, Demattos C, et al. Alveolar macrophage-mediated elastolysis: roles of matrix metalloproteinases, cysteine, and serine proteases. Am J Physiol Lung Cell Mol Physiol. 2002;283:867–73.
Hoser G, Domagała-Kulawik J, Droszcz P, Droszcz W, Kawiak J. Lymphocyte subsets differences in smokers and nonsmokers with primary lung cancer: A flow cytometry analysis of broncoalveolar lavage fluid cells. Med Sci Monit. 2003;9:310–5.
Hodge S, Hodge G, Ahern J, Jersmann H, Holmes M, Reynolds PN. Smoking alters alveolar macrophage recognition and phagocytic ability: implications in chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2007;37:748–55.
van der Vaart H, Postma DS, Timens W, ten Hacken NH. Acute effects of cigarette smoke on inflammation and oxidative stress: a review. Thorax. 2004;59:713–21.
Berenson CS, Garlipp MA, Grove LJ, Maloney J, Sethi S. Impaired phagocytosis of nontypeable Haemophilus influenzae by human alveolar macrophages in chronic obstructive pulmonary disease. J Infect Dis. 2006;194:1375–84.
Chen H, Cowan MJ, Hasday JD, Vogel SN, Medvedev AE. Tobacco smoking inhibits expression of proinflammatory cytokines and activating of IL-1R-associated kinase, p38, and NF-κB in alveolar macrophages stimulates with TLR2 and TLR4 agonists. J Immunol. 2007;179:6097–106.
Gaschler GJ, Zavitz CC, Bauer CM, Skrtic M, Lindahl M, Robbins CS, et al. Cigarette smoke exposure attenuates cytokine production by mouse alveolar macrophages. Am J Respir Cell Mol Biol. 2008;38:218–26.
Droemann D, Goldmann T, Tiedje T, Zabel P, Dalhoff K, Schaaf B. Toll-like receptor 2 expression is decreased on alveolar macrophage in cigarette smokers and COPD patients. Respir Res. 2005;6:68.
Karimi K, Sarir H, Mortaz E, Smit JJ, Hosseini H, De Kimpe SJ, et al. Toll-like receptor-4 mediates cigarette smoke-induced cytokine production by human macrophages. Respir Res. 2006; 7:66.
Doz E, Noulin N, Boichot E, Guénon I, Fick L, Le Bert M, et al. Cigarette smoke-induced pulmonary inflammation is TLR4/MyD88 and IL-1R1/MyD88 signaling dependent. J Immunol. 2008;180:1169–78.
Sarir H, Mortaz E, Karimi K, Kraneveld AD, Rahman I, Caldenhoven E, et al. Cigarette smoke regulates the expression of TLR4 and IL-8 production by human macrophages. J Inflamm. 2009;6:12.
Noakes PS, Hale J, Thomas R, Lane C, Devadason SG, Prescott SL. Maternal smoking is associated with impaired neonatal toll-like-receptor-mediated immune responses. Eur Respir J. 2006;28:721–9.
Drannik AG, Pouladi MA, Robbins CS, Goncharova SI, Kianpour S, Stämpfli MR. Impact of cigarette smoke on clearance and inflammation after Pseudomonas aeruginosa infection. Am J Respir Crit Care Med. 2004;170:1164–71.
Mian MF, Lauzon NM, Stampfli MR, Mossman KL, Ashkar AA. Impairment of human NK cell cytotoxic activity and cytokine release by cigarette smoke. J Leukoc Biol. 2008;83:774–84.
Ng AK, Travis LB. Subsequent malignant neoplasm in cancer survivors. Cancer J. 2008;14:429–34.
Nouri-Shirazi M, Guinet E. A possible mechanism linking cigarette smoke to higher incidence of respiratory infection and asthma. Immunol Lett. 2006;103:167–76.
Tsoumakidou M, Demedts IK, Brusselle GG, Jeffery PK. Dendritic cells in chronic obstructive pulmonary disease: new players in an old game. Am J Respir Crit Care Med. 2008;177:1180–6.
Jahnsen FL, Strickland DH, Thomas JA, Tobagus IT, Napoli S, Zosky GR, et al. Accelerated antigen sampling and transport by airway mucosal dendritic cells following inhalation of a bacterial stimulus. J Immunol. 2006;177:5861–7.
McComb JG, Ranganathan M, Liu XH, Pilewski JM, Ray P, Watkins SC, et al. CX3CL1 up-regulation is associated with recruitment of CX3CR1+ mononuclear phagocytes and T lymphocytes in the lungs during cigarette smoke-induced emphysema. Am J Pathol. 2008;173:949–61.
D’Hulst AI, Vermaelen KY, Brusselle GG, Joos GF, Pauwels RA. Time course of cigarette smoke-induced pulmonary inflammation in mice. Eur Respir J. 2005;26:204–13.
Yamamoto K, Takanashi S, Hasegawa Y, Kanehira Y, Kaizuka M, Okumura K. Eotaxin level in induced sputum is increased in patients with bronchial asthma and in smokers. Respiration. 2003;70:600–5.
Domagała-Kulawik J, Maskey-Warzechowska M, Kraszewska I, Chazan R. The cellular composition and macrophage phenotype in induced sputum in smokers and ex-smokers with COPD. Chest. 2003;123:1054–9.
Amin K, Ekberg-Jansson A, Löfdahl CG, Venge P. Relationship between inflammatory cells and structural changes in the lungs of asymptomatic and never smoker: a biopsy study. Thorax. 2003;58:135–42.
Small-Howard A, Turner H. Exposure to tobacco-derived materials induces overproduction of secreted proteinases in mast cells. Toxicol Appl Pharmacol. 2005;204:152–63.
Mortaz E, Redegeld FA, Sarir H, Karimi K, Raats D, Nijkamp FP, et al. Cigarette smoke stimulates the production of chemokines in mast cells. J Leukoc Biol. 2008;83:575–80.
Mortaz E, Folkerts G, Engels F, Nijkamp FP, Redegeld FA. Cigarette smoke suppresses in vitro allergic activation of mouse mast cells. Clin Exp Allergy. 2009;39:679–87.
Viau M, Zouali M. B-lymphocytes, innate immunity, and autoimmunity. Clin Immunol. 2005;114:17–26.
Gonzalez-Quintela A, Alende R, Gude F, Campos J, Rey J, Meijide LM, et al. Serum levels of immunoglobulins (IgG, IgA, IgM) in a general adult population and their relationship with alcohol consumption, smoking and common metabolic abnormalities. Clin Exp Immunol. 2008;151:42–50.
Quinn SM, Zhang JB, Gunsolley JC, Schenkein HA, Tew JG. The influence of smoking and race on adult periodontitis and serum IgG2 levels. J Periodontol. 1998;69:171–7.
Tangada SD, Califano JV, Nakashima K, Quinn SM, Zhang JB, Gunsolley JC. The effect of smoking on serum IgG2 reactive with Actinobacillus actinomycetemcomitans in early-onset periodontitis patients. J Periodontol. 1997;68:842–50.
Graswinckel JE, van der Velden U, van Winkelhoff AJ, Hoek FJ, Loos BG. Plasma antibody levels in periodontitis patients and controls. J Clin Periodontol. 2004;31:562–8.
Al-Ghamdi HS, Anil S. Serum antibody levels in smoker and non-smoker saudi subjects with chronic periodontitis. J Periodontol. 2007;78:1043–50.
Zavitz CC, Gaschler GJ, Robbins CS, Botelho FM, Cox PG, Stampfli MR. Impact of cigarette smoke on T and B cell responsiveness. Cell Immunol. 2008;253:38–44.
Ishida T, Pinkerton KE, Takeuchi M. Alveolar macrophage from cigarette smoke-exposed mice inhibits B lymphocyte proliferation stimulated with LPS. Respiration. 2009;77:91–5.
Mehta H, Nazzal K, Sadikot RT. Cigarette smoking and innate immunity. Inflamm Res. 2008;57:497–503.
Maeno T, Houghton AM, Quintero PA, Grumelli S, Owen CA, Shapiro SD. CD8+ T cells are required for inflammation and destruction in cigarettesmoke-induced emphysema in mice. J Immunol. 2007;178:8090–6.
Glader P, Möller S, Lilja J, Wieslander E, Löfdahl CG, von Wachenfeldt K. Cigarette smoke extract modulates respiratory defense mechanisms through effects on T-cells and airway epithelial cells. Respir Med. 2006;100:818–27.
Avanzini MA, Ricci A, Scaramuzza C, Semino L, Pagella F, Castellazzi AM, et al. Deficiency of INFgamma producing cells in adenoids of children exposed to passive smoke. Int J Immunopathol Pharmacol. 2006;19:609–16.
Luppi P, Lain KY, Jeyabalan A, DeLoia JA. The effects of cigarette smoking on circulating maternal leukocytes during pregnancy. Clin Immunol. 2007;122:214–9.
Orbak R, Erciyas K, Kaya H. Flow-cytometric analysis of T-lymphocyte subsets after different treatment methods in smokers and non-smokers with chronic periodontitis. Int Dent J. 2003;53:159–64.
Loos BG, Roos MT, Schellekens PT, van der Velden U, Miedema F. Lymphocyte numbers and function in relation to periodontitis and smoking. J Periodontol. 2004;75:557–64.
Spira A, Beane J, Shah V, Liu G, Schembri F, Yang X, et al. Effects of cigarette smoke on the human airway epithelial cell transcriptome. Proc Natl Acad Sci USA. 2004;101:10143–8.
Phillips J, Kluss B, Richter A, Massey E. Exposure of bronchial epithelial cells to whole cigarette smoke: assessment of cellular responses. Altern Lab Anim. 2005;33:239–48.
Floreani AA, Heires AJ, Welniak LA, Miller-Lindholm A, Clark-Pierce L, Rennard SI, et al. Expression of receptors for C5a anaphylatoxin (CD88) on human bronchial epithelial cells: enhancement of C5a-mediated release of IL-8 upon exposure to cigarette smoke. J Immunol. 1998;160:5073–81.
Allen-Gipson DS, Floreani AA, Heires AJ, Sanderson SD, MacDonald RG, Wyatt TA. Cigarette smoke extract increases C5a receptor expression in human bronchial epithelial cells. J Pharmacol Exp. 2005;14:476–82.
Thaikoottathil JV, Martin RJ, Zdunek J, Weinberger A, Rino JG, Chu HW. Cigarette smoke extract reduces VEGF in primary human airway epithelial cells. Eur Respir J. 2009;33:835–43.
Bauer CM, Dewitte-Orr SJ, Hornby KR, Zavitz CC, Lichty BD, Stämpfli MR, et al. Cigarette smoke suppresses type I interferon-mediated antiviral immunity in lung fibroblast and epithelial cells. J Interferon Cytokine Res. 2008;28:167–79.
Giannopoulo C, Roehrich N, Mombelli A. Effect of nicotine-treated epithelial cells on the proliferation and collagen production of gingival fibroblasts. J Clin Periodontol. 2001;28:769–75.
Peacock ME, Sutherland DE, Schuster GS, Brennan WA, O’Neal RB, Strong SL. The effect of nicotine on reproduction and attachment of human gingival fibroblasts in vitro. J Periodontol. 1993;64:658–65.
Ho YC, Chang YC. Regulation of nicotine-induced cyclooxygenase-2 protein expression in human gingival fibroblasts. Acta Pharmacol Sin. 2006;27:409–13.
Zhou J, Olson BL, Windsor LJ. Nicotine increases the collagen-degrading ability of human gingival fibroblasts. J Periodontal Res. 2007;42:228–335.
Gonzalez R, Arancibia R, Cáceres M, Martínez J, Smith PC. Cigarette smoke condensate stimulates urokinase production through the generation of reactive oxygen species and activation of the mitogen activated protein kinase pathways in human gingival fibroblasts. J Periodontal Res. 2009;44:386–94.
Wannamethee SG, Lowe GD, Shaper AG, Rumley A, Lennon L, Whincup PH. Associations between cigarette smoking, pipe/cigar smoking, and smoking cessation, and haemostatic and inflammatory markers for cardiovascular disease. Eur Heart J. 2005;26:1765–73.
Bermudez EA, Rifai N, Buring JE, Manson JE, Ridker PM. Relation between markers of systemic vascular inflammation and smoking in women. Am J Cardiol. 2002;89:1117–9.
Helmersson J, Larsson A, Vessby B, Basu S. Active smoking and a history of smoking are associated with enhanced prostaglandin F(2alpha), interleukin-6 and F2-isoprostane formation in elderly men. Atherosclerosis. 2005;181:201–7.
Meuronen A, Majuri ML, Alenius H, Mäntylä T, Wolff H, Piirilä P, et al. Decreased cytokine and chemokine mRNA expression in bronchoalveolar lavage in asymptomatic smoking subjects. Respiration. 2008;75:450–8.
Mishra A, Wang M, Pemmaraju VR, Collins MH, Fulkerson PC, Abonia JP, et al. Esophageal remodeling develops as a consequence of tissue specific IL-5-induced eosinophilia. Gastroenterology. 2008;134:204–14.
Boström L, Linder LE, Bergström J. Clinical expression of TNF-alpha in smoking-associated periodontal disease. J Clin Periodontol. 1998;25:767–73.
Erdemir EO, Duran I, Haliloglu S. Effects of smoking on clinical parameters and the gingival crevicular fluid levels of IL-6 and TNF-alpha in patients with chronic periodontitis. J Clin Periodontol. 2004;31:99–104.
Boström L, Linder LE, Bergström J. Smoking and GCF levels of IL-1beta and IL-1ra in periodontal disease. J Clin Periodontol. 2000;27:250–5.
Rawlinson A, Grummitt JM, Walsh TF, Ian Douglas CW. Interleukin 1 and receptor antagonist levels in gingival crevicular fluid in heavy smokers versus non-smokers. J Clin Periodontol. 2003;30:42–8.
Almasri A, Wisithphrom K, Windsor LJ, Olson B. Nicotine and lipopolysaccharide affect cytokine expression from gingival fibroblasts. J Periodontol. 2007;78:533–41.
César-Neto JB, Duarte PM, de Oliveira MC, Casati MZ, Tambeli CH, Parada CA, et al. Smoking modulates INF-γ expression in the gingival tissues of patients with chronic periodontitis. Eur J Oral Sci. 2006;114:403–8.
César-Neto JB, Duarte PM, de Oliveira MC, Tambeli CH, Sallum EA, Nociti FH Jr. Smoking modulates IL-6:IL-10 and RANKL:OPG ratios in the periodontal tissues. J Periodontal Res. 2007;42:184–91.
Torres de Heens GL, Kikkert R, Aarden LA, van der Velden U, Loos BG. Effects of smoking on the ex vivo cytokine production in periodontitis. J Periodont Res. 2009;44:28–34.
Hasnis E, Bar-Shai M, Burbea Z, Reznick AZ. Mechanisms underlying cigarette smoke-induced NF-kappaB activation in human lymphocytes: the role of reactive nitrogen species. J Physiol Pharmacol. 2007;58:275–87.
Szulakowski P, Crowther AJ, Jiménez LA, Donaldson K, Mayer R, Leonard TB, et al. The effect of smoking on the transcriptional regulation of lung inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;174:41–50.
Yang SR, Chida AS, Bauter MR, Shafiq N, Seweryniak K, Maggirwar SB, et al. Cigarette smoke induces proinflammatory cytokine release by activation of NF-kappaB and posttranslational modifications of histone deacetylase in macrophages. Am J Physiol Lung Cell Mol Physiol. 2006;291:L46–57.
Karin M. The IkappaB kinase—a bridge between inflammation and cancer. Cell Res. 2008;18:334–342.
Clement JF, Meloche S, Servant MJ. The IKK-related kinases: from innate immunity to oncogenesis. Cell Res. 2008;18:889–99.
Li H, Lin X. Positive and negative signaling components involved in TNFalpha-induced NF-kappaB activation. Cytokine. 2008;41:1–8.
Yao H, Yang SR, Kode A, Rajendrasozhan S, Caito S, Adenuga D, et al. Redox regulation of lung inflammation: role of NADPH oxidase and NF-kappaB signalling. Biochem Soc Trans. 2007;35:1151–5.
Di Stefano A, Caramori G, Oates T, Capelli A, Lusuardi M, Gnemmi I, et al. Increased expression of nuclear factor-kappaB in bronchial biopsies from smokers and patients with COPD. Eur Respir J. 2002;20:556–63.
Yagi O, Aoshiba K, Nagai A. Activation of nuclear factor-kappaB in airway epithelial cells in patients with chronic obstructive pulmonary disease. Respiration. 2006;73:610–6.
Zhao J, Harper R, Barchowsky A, Di YP. Identification of multiple MAPK-mediated transcription factors regulated by tobacco smoke in airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2007;293:L480–90.
Yang SR, Wright J, Bauter M, Seweryniak K, Kode A, Rahman I. Sirtuin regulates cigarette smoke-induced proinflammatory mediator release via RelA/p65 NF-kappaB in macrophages in vitro and in rat lungs in vivo: implications for chronic inflammation and aging. Am J Physiol Lung Cell Mol Physiol. 2007;292:L567–76.
Marwick JA, Kirkham PA, Stevenson CS, Danahay H, Giddings J, Butler K, et al. Cigarette smoke alters chromatin remodeling and induces proinflammatory genes in rat lungs. Am J Respir Cell Mol Biol. 2004;31:633–42.
Li YT, He B, Wang YZ. Exposure to cigarette smoke upregulates AP-1 activity and induces TNF-alpha overexpression in mouse lungs. Inhal Toxicol. 2009;21:641–7.
Ballina-Rosas M, Tracey KJ. Cholinergic control of inflammation. J Int Med. 2009;265:663–79.
Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000;405:458–62.
van Westerloo DJ, Giebelen IA, Florquin S, Daalhuisen J, Bruno MJ, de Vos AF, et al. The cholinergic anti-inflammatory pathway regulates the host response during septic peritonitis. J Infect Dis. 2005;191:2138–48.
Waldburger JM, Boyle DL, Pavlov VA, Tracey KJ, Firestein GS. Acetylcholine regulation of synoviocyte cytokine expression by the alpha7 nicotinic receptor. Arthritis Rheum. 2008;58:3439–49.
Brioni JD, Decker MW, Sullivan JP, Arneric SP. The pharmacology of (−)nicotine and novel cholinergic channel modulators. Adv Pharmacol. 1997;37:153–214.
Wang H, Yu M, Ochnal M, Amella CA, Tanovic M, Susaria S, et al. Nicotinic acetylcholine receptor α7 subunit is an essential regulator of inflammation. Nature. 2003;421:384–7.
Mabley J, Gordon S, Pacher P. Nicotine exerts an anti-inflammatory effect in a murine model of acute lung injury. Inflammation 2010. doi:10.1007/s10753-010-9228-x
Zhou Y, Zuo X, Li Y, Wang Y, Zhao H, Xiao X. Nicotine inhibits tumor necrosis factor-α induced IL-6 and IL-8 secretion in fibroblast-like synoviocytes from patients with rheumatoid arthritis. Rheumatol Int 2010. doi:10.1007/s00296-010-1549-4
Breivik T, Gundersen Y, Gjermo P, von Horsten S, Opstad PK. Nicotinic acethylcholine receptor activation mediates nicotine-induced enhancement of experimental periodontitis. J Periodont Res. 2009;44:110–6.
Lerman C, LeSage MG, Perkins KA, O’Malley SS, Siegel SJ, Benowitz NL, et al. Translational research in medication development for nicotine dependence. Nat Rev Drug Discov. 2007;6:746–62.
Churg A, Wright JL. Animal models of cigarette smoke-induced chronic obstructive lung disease. Contrib Microbiol. 2007;14:113–25.
Quinn SM, Zhang JB, Gunsolley JC, Schenkein JG, Schenkein HA, Tew JG. Influence of smoking and race on immunoglobulin G subclass concentrations in early-onset periodontitis patients. Infect Immun. 1996;64:2500–5.
Bostrom L, Linder LE, Bergstrom J. Smoking and crevicular fluid levels of IL-6 and TNF-alpha in periodontal disease. J Clin Periodontol. 1999;26:352–7.
Acknowledgments
Because of space constraints, we were unable to cite all relevant, especially primary, publications, and apologize to any author whose work we have not referenced. Dr. Francisco Nociti Jr. was supported by the National Council of Research (CNPq, Grant # 305471/2006-6).
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: Kumar Visvanathan.
Rights and permissions
About this article
Cite this article
Gonçalves, R.B., Coletta, R.D., Silvério, K.G. et al. Impact of smoking on inflammation: overview of molecular mechanisms. Inflamm. Res. 60, 409–424 (2011). https://doi.org/10.1007/s00011-011-0308-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-011-0308-7