Abstract
Objectives
The World Health Organization developed the Risk Factor Model for Falls to describe fall risks in a comprehensive manner. However, there was a lack of study adopting such framework in quantifying falls risk from different factors in a single model. Therefore, this study examined the risk factors from four domains in the Risk Factor Model for Falls among older adults.
Design
Secondary data analysis of 10-year assessment records of the Minimum Data Set-Home Care instrument.
Setting
Hong Kong.
Participants
89,100 community-dwelling adults aged 65 and over who first applied for publicly funded long-term care services from 2005 to 2014.
Measurements
The Minimum Data Set-Home Care instrument was used to ascertain older adults’ care needs and match them with appropriate services. Additionally, meteorological records from the same period were extracted from the Hong Kong Observatory. The logistic regression model was used to examine risk factors and their associations with falls.
Results
In total 70 factors were included in the analysis, of which 37 were significantly associated with falls. Behavioral risk factors generally had greater odds ratios of falling, as compared with biological, socioeconomic, and environmental factors. Out of all significant factors, functional status, alcohol drinking, and locomotion outdoors had the largest odds ratios of falling.
Conclusion
Behavioral risk factors for falls are of remarkable influence yet are modifiable among older adults. Hence, falls prevention programs may need to prioritize addressing these factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generally, around 40% to 60% of falls lead to injuries among the older population, and these injuries result in considerable morbidity, mortality, and high costs to health services (1). It was reported that fall-related injuries account for 40% of the leading cause of older people’s long-term institutional care (1). According to the Centers for Disease Control and Prevention, fall-related injuries were responsible for approximately 32,500 deaths, 3 million emergency department visits, and 900,000 hospitalizations in 2018 among older adults aged 65 and over in the US (2). Concerning the financial burden caused by falls, the annual costs spent on falls for older adults aged 65 and over in the US were more than 50 billion in 2015 (3).
Various identified risk factors have been summarized in a previous systematic review, which were age, gender, history of falls, limitation on physical activity, physical disability, instrumental disability, low educational level, use of walking aid, depression, urinary incontinence, rheumatic disease, dizziness and vertigo, increment of comorbidity, self-perceived low health status, fear of falling, Parkinson’s disease, use of antihypertensives, and vision impairment (4). According to the Risk Factor Model for Falls developed by the World Health Organization (WHO), these risk factors can be categorized into four dimensions that are biological, socioeconomic, behavioral, and environmental domains (Figure 1) (11). Though risk factors for falls have been extensively studied, only one study has investigated risk factors using the WHO’s framework among adults aged 50 and older (6). Meanwhile, only a few studies explored the effects of environmental hazards on falls, together with individual risk factors (7–10). However, these studies only addressed a small number of individual factors and did not involve the meteorological factors from the environmental domain. Identifying the risk factors for falls using the Risk Factor Model for Falls that address the risk factors from four domains simultaneously, allows comparison of the falls risks of factors from different dimensions, as such it could inform the most prominent domain to target with falls prevention initiatives. Therefore, the present study aimed to examine the risk factors for falls from four domains in the WHO’s Risk Factor Model for Falls, among community-dwelling older adults in Hong Kong.
Methods
Data
A retrospective cross-sectional study was conducted. The data set was obtained from the InterRAI Corporation and included the 10-year Minimum Data Set-Home Care (MDS-HC) assessment records of community-dwelling older adults first applying for publicly funded long-term care services in Hong Kong from 2005 to 2014. In Hong Kong, individuals who would like to apply for publicly funded long-term care services have to undergo the standardized assessment by the MDS-HC. Trained assessors conducted the assessment, which included direct questioning of the clients and the primary family caregivers, observation of the clients in their home environment, and a review of secondary documents when available. The MDS-HC is a validated instrument that including nine parts: the general information; the assessment information; the physical and mental patterns; the social supports; the physical function; the health conditions; the living environment; the service utilization; and the medications. Meteorological data from 2005 to 2014 were obtained from the Hong Kong Observatory.
The primary outcome of falls was accessed by a single question in MDS-HC asking the number of falls episodes experienced by the client in the past 90 days. This study extracted and analyzed the data concerning falls outcome (with experiences of falling or not), as well as assessment records of the biological, socioeconomic, behavioral, and environmental domains.
The inclusion criteria were those (1) aged 65 years and older, (2) living in their own homes in Hong Kong, and (3) who underwent the MDS-HC assessment when they first applied for publicly funded long-term care services. The exclusion criterion was those with missing information concerning the outcome of falls. After applying selection criteria to select the eligible subjects, 89,100 individuals were included in the data analysis.
Statistical analysis
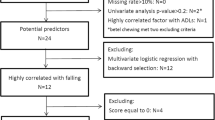
T-test and Chi-square test were used to compare the characteristics of subjects by their fall status (non-fallers and fallers). The logistic regression model was used to examine the association between various factors and falls. The dependent variable was being a faller (versus being a non-faller). The selection of independent variables was based on the WHO’s Risk Factor Model for Falls (11). The independent variables were presented in Table 1. For independent variables in terms of scores, the scores were grouped into classes only when the classes were well defined in the literature. For the IADL-ADL Hierarchy Scale, classes were not well defined, and the score was used as a categorical variable in the regression model because a linear relationship might not hold. The model selection procedure was conducted by using the backward elimination method. Potential multicollinearity was checked by examining VIFs, and variables were removed until all VIFs were below 4 (12). All tests were 2-sided. SPSS version 25.0 was used for data analysis and a significance level of 5% was adopted.
Results
Descriptive statistics
A total of 28,396 subjects (31.9%) experienced at least one fall episode within the previous 90 days (fallers). The majority of subjects were aged between 75 and 84, and 60.1% were female. The mean number of medications taken was 5.4, and hypertension (65.6%) was the most common disease among all subjects. The biological, socioeconomic, behavioral, and environmental characteristics of subjects were presented in Tables 2.
The univariate analysis (T-test or Chi-square) showed that there were significant differences between fallers and non-fallers in most variables from four domains except for these variables: (1) biological factors: gender, vision impairment, severe malnutrition, morbid obesity, coronary artery disease, hypertension, irregularly irregular pulse, peripheral vascular disease, dementia, epilepsy, arthritis, glaucoma, renal failure, and thyroid disease; (2) environmental factors: moved to the current residence within last two years, wind speed, and hazards related to lighting in evening, kitchen, heating and cooling, personal safety (Table 2).
Logistic regression model
There were 70 independent variables initially included in the analysis. After the model selection procedure, 37 independent variables remained in the final model. No variable was further removed as all VIFs were below 4. In the final multiple logistic regression model, the variables that independently associated with falls from four domains were (1) biological factors: male gender, cognitive impairment, functional status, pain, depression, delirium, bladder incontinence, fecal incontinence, unintended weight loss, morbid obesity, congestive heart failure, coronary artery disease, hypertension, hemiplegia, Parkinson’s disease, arthritis, psychiatric diagnosis, unitary tract infection, cancer, diabetes, and emphysema/COPD/asthma; (2) socioeconomic factors: marital status, educational level, and living alone; (3) behavioral factors: medication compliance, locomotion indoor, locomotion outdoor, alcohol drinking, and smoking; (4) environmental factors: hazards related to flooring and carpeting, hazards related to access to home, hazards related to access to room in house, number of very hot days, number of cold days, number of very humid day, number of very dry day, and number of days with heavy rain (Table 3).
Among the 37 significant factors, the magnitudes of the odds ratio of falling ranged from 1.00 to 2.00 for most factors. The factor with the highest odds ratio of falling was functional status, with odds ratios corresponded to different scores of the IADL-ADL Hierarchy Scale ranged from 1.31 to 2.05. The factor with the second-highest odds ratio of falling was alcohol drinking, which had an odds ratio of 1.96. The factor with the third-highest odds ratio of falling was locomotion outdoors, with odds ratios corresponded to different levels of mobility ranged from 1.40 to 1.72. Other than these three factors, the magnitudes of odds ratios of the remaining biological factors ranged from 1.04 to 1.52; those of socioeconomic factors ranged from 1.07 to 1.16; those of the remaining behavioral factors ranged from 1.10 to 1.67; and those of environmental factors ranged from 1.01 to 1.41. The magnitudes of odds ratios in behavioral factors were generally higher compared with other domains.
After taking account of the environmental and individual factors simultaneously, the results showed that the number of cold days and the number of days with heavy rain were positively associated with the risk of falling. For example, there were 14 cold days in total from December 2012 to February 2013, and the falls risk would be 15% higher than the summer months, which with 0 cold days.
Discussion
The current study investigated associations between falls and factors from four domains in the WHO’s Risk Factor Model for Falls among the community-dwelling older population in Hong Kong. While various risk factors were well studied on their own in different studies, there was a lack of studies that examined the strength of associations of these factors when taking into account all factors in the four domains together. Our findings added to knowledge about the extent and nature of risk factors for falls in four domains and provided a reference for specific areas of focus for falls prevention.
The findings of the present study indicate that, out of all risk factors from four domains in the WHO’s Risk Factor Model for Falls, the behavioral risk factors generally had greater odds ratios of falling than biological, socioeconomic, and environmental risk factors. Meanwhile, the risk factors from the socioeconomic domain had the minimum odds ratios of falling. Behavioral risk factors are defined as factors concerning human actions, emotions, or daily choices, and they are potentially modifiable (11). Evidence suggested that behavioral change to a healthy lifestyle in the older population was crucial in encouraging healthy aging and avoiding falls (5). The behavioral intervention was found with flexibility and a promising effect on falls prevention in older adults (13). On the contrary, the socioeconomic risk factors are those related to influence social conditions and economic status of individuals, which are difficult to change (11). Therefore, the efforts on preventing falls among community-dwelling older adults are suggested to focus on the behavioral risk factors to maximize the benefit.
In general, to prevent falls effectively, a multifactorial intervention program has been shown to be effective by addressing multiple risk factors (14, 15). However, in resource-limited situations, if multifactorial interventions are not affordable or accessible, prevention programs might be prioritized toward a particular domain. Our findings showed that risk factors from the behavioral domain had relatively higher falls risks than those from the other three domains in the WHO’s framework. When interpreting the odds ratio, a value of 2.00 to 3.00 has been recognized as having a practically significant effect (16). In the behavioral domain, alcohol drinking had an odds ratio of 1.96, which was approaching this practically significant effect threshold. Therefore, prevention programs targeting the factors from the behavioral domain could be considered. Furthermore, factors from the behavioral domain were mostly modifiable, implying interventions could be implemented. For example, there were cost-effective interventions that could successfully reduce alcohol drinking, smoking, and enhance medicine compliance. Evidence showed that increasing alcohol prices could significantly reduce consumption and the level of alcohol-related problems (17, 18). More intensive interventions, including personalized feedback reports, educational materials, and follow-up, were also reported to effectively reduce alcohol consumption among older adults when maintained up to one year (19). Similarly, the price increase on tobacco products was one of the most valid solutions to reducing smoking (15). Meanwhile, nicotine replacement therapy was the intervention for smoking cessation that most studied, yet limited evidence suggested its effectiveness in the older population (20). For medicine compliance, promising strategies to improve medicine adherence included monitoring through electronic devices, self-report methods, and pill counts (21).
For biological and socioeconomic domains, the odds ratios of falling were small for most risk factors (slightly to moderately exceeded 1.00), except for the functional status in the biological domain. The odds ratios of falling corresponded to different scores of the IADL-ADL Hierarchy Scale ranged from 1.31 to 2.05, of which the odds ratio of 2.05 was considered practically significant (16). Functional status has been well studied as a prominent risk factor for falls (22). At the same time, limited functional status could be associated with the falls outcome (23). As functional status could be both a cause and a consequence of falls within the past 90 days, interpretation of the odds ratios should be paid with extra attention. The same situation might also apply to the use of assistive devices in the behavioral domain. While the use of assistive devices could increase the falls risk, those experienced falls might need assistive devices to help with locomotion after falling (24, 25). Despite the limitation in interpreting the magnitudes of odds ratios in terms of functional status and locomotion, it is still essential to ensure a safe and accessible residential environment as well as more attention from caregivers or communities to reduce the risk of falling for those with functional limitations and need to use assistive devices. Moreover, it is critical to not only instruct the older people the correct method to use the assistive devices safely but also, to educate them on how to avoid falls or other injuries during use.
For the environmental domain, literature suggested that an unfamiliar surrounding environment would increase the risk of falls among older adults (26). However, there were limited studies on this. Our study included a variable on whether the older people moved to the current residence within the last two years. Surprisingly, this factor was not significant, both in univariate analysis and the multiple logistic regression. It might be explained by the tight housing conditions in Hong Kong. Generally, when people are able to move to a new residence, their new residence tends to be improved when comparing to the older one. Hence fewer environmental hazards may present there, which would reduce their risk of falling. On the other hand, our study found that, after taking account of individual risk factors from the other three domains, it was the environmental hazards related to floor and carpeting and the accessibility to house or rooms that were associated with increased fall risks. It is particularly true for a densely populated city such as Hong Kong, where the living environment would be less spacious. Housing design could play a role in improving older adults’ living environments to reduce their falls risk (27). Concerning the meteorological conditions less studied, we found that the occurrence of falls increased with the number of cold days and the number of days with heavy rain. The finding on the number of cold days is consistent with the existing evidence that the falls risk was higher in the winter season (28, 29). Nevertheless, the findings of the impact of rainfall on falls in subtropical regions were contradictory in the published studies, in which one study showed no association between rainfall and falls occurrence in Hong Kong, while another study found rainy days had a greater risk of falling in Taiwan (28, 30). In our study, the number of days with heavy rain was positively associated with falls occurrence, which is consistent with the findings in Taiwan. Possible explanations behind could be the heavy rain makes surfaces slippery, as well as makes cracks and uneven sidewalks difficult to distinguish. These environmental hazards would increase the risk of falling among older adults. Hence, during cold days and heavily rainy days, reminders such as weather alert, broadcast, and message on the television should be implemented for falls prevention.
The strengths of this study are the use of a large cohort and a comprehensive, validated measurement tool. The large sample size included in the study allowed for more reliable results, while the comprehensive and validated instrument improved data collection. Meanwhile, investigating risk factors for falls using the WHO’s Risk Factor Model for Falls facilitated the comparison of factors in different domains in terms of their falls risk. The inclusion of factors from biological, socioeconomic, behavioral, and environmental domains at the same time allowed to precisely examine the interrelation between environmental factors and falls when controlling factors from the remaining domains. Nevertheless, the study is limited by its cross-sectional nature that it could not determine causal effects. Self-reported fall data were subject to possible recall bias, which may influence the reliability of results. Since the falls outcome only contained the number of falls episodes within the previous 90 days and without the exact date of falling, some of the potential associated factors could be the conditions happened after falls occurrences or even could be the consequences caused by falls, which may weaken the evidence of their associations. Due to the same reason, the investigation of meteorological risk factors for falls was limited to the cumulative impact of weather conditions within the previous 90 days. Additionally, some risk factors for falls, such as balance and mobility, were not included in this study as the analysis was subject to the information in the data set. Therefore, a prospective study addressing more risk factors would be needed in the future.
Conclusion
In conclusion, the present findings demonstrated the strength of associations with falls of risk factors from four domains in the WHO’s Risk Factor Model for Falls and recommended prioritization of prevention initiatives of falls.
References
Masud T and Morris R O. Epidemiology of falls. Age Ageing. 2001; 30(suppl_4): 3–7.
Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. Updated July 1, 2020. Accessed September 15, 2020.
Florence C S, et al. Medical costs of fatal and nonfatal falls in older adults. J Am Geriatr Soc. 2018; 66(4): 693–698.
Deandrea S, et al. Risk factors for falls in community-dwelling older people: “a systematic review and meta-analysis”. Epidemiology. 2010; 21(5): 658–668.
World Health Organization. Active Ageing: A Policy Framework, https://apps.who.int/iris/bitstream/handle/10665/67215/WHO_NMH_NPH_02.8.pdf. Published April 2002. Accessed September 15, 2020.
World Health Organization. Measuring prevalence and risk factors for fall-related injury in older adults in low-and middle-income countries: results from the WHO Study on Global AGEing and Adult Health (SAGE), https://www.who.int/healthinfo/sage/SAGEWorkingPaper6_WavelFalls.pdf?ua=l. Published July 2013. Accessed September 15, 2020.
Lo A X, et al. Neighborhood disadvantage and life-space mobility are associated with incident falls in community-dwelling older adults. J Am Geriatr Soc. 2016; 64(11): 2218–2225.
Nicklett E J, Lohman M C, and Smith M L. Neighborhood environment and falls among community-dwelling older adults. Int J Environ Res Public Health. 2017; 14(2): 175.
Quach L, et al. Depression, antidepressants, and falls among community-dwelling elderly people: the MOBILIZE Boston study. J Gerontol A Biol Sci Med Sci. 2013; 68(12): 1575–1581.
Steinman B A, Pynoos J, and Nguyen A Q. Fall risk in older adults: roles of self-rated vision, home modifications, and limb function. J Aging Health. 2009; 21(5): 655–676.
World Health Organization, WHO Global Report on Falls Prevention in Older Age. http://www.who.int/ageing/publications/Falls_prevention7March.pdf. Published March 7 2007. Accessed September 15, 2020.
Hair J F, et al. Multivariate data analysis: International version. New Jersey, Pearson, 2010.
Fleig L, et al. Health behaviour change theory meets falls prevention: feasibility of a habit-based balance and strength exercise intervention for older adults. Psychol Sport Exerc. 2016; 22: 114–122.
Chang J T, et al. Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials. Bmj. 2004; 328(7441): 680.
Gillespie L D, et al. Interventions for preventing falls in elderly people. Cochrane database of systematic reviews, 2003(4).
Ferguson C J. An effect size primer: a guide for clinicians and researchers. In A. E. Kazdin (Ed.), Methodological issues and strategies in clinical research, 2016: 301–310.
Babor T, et al. Alcohol: no ordinary commodity: research and public policy. Rev Bras Psiquiatr, 2010; 26(4): 280–283.
Edwards G. Alcohol policy and the public good. Addiction, 1997; 92(3s1): 73–80.
Kelly S, et al. Interventions to prevent and reduce excessive alcohol consumption in older people: a systematic review and meta-analysis. Age Ageing. 2018; 47(2): 175–184.
Cawkwell P B, Blaum C, and Sherman S E. Pharmacological smoking cessation therapies in older adults: a review of the evidence. Drugs Aging. 2015; 32(6): 443–451.
Marcum Z A, Hanion J T, and Murray M D. Improving medication adherence and health outcomes in older adults: an evidence-based review of randomized controlled trials. Drugs Aging. 2017; 34(3): 191–201.
Rokicki W, et al. Relationship between visual status and functional status and the risk of falls in women. The RAC-OST-POL study. Arch Med Sci: AMS. 2016; 12(6): 1232.
Mamikonian-Zarpas A and Laganá L. The relationship between older adults’ risk for a future fall and difficulty performing activities of daily living. J Aging Gerontol. 2015; 3(1): 8–16.
Ferretti F, Lunardi D, and Bruschi L. Causes and consequences of fall among elderly people at home. FisioterMov. 2013; 26: 753–762.
West B A, et al. Assistive device use and mobility-related factors among adults aged≥ 65 years. J Safety Res. 2015; 55: 147–150.
Lund C and Sheafor M L. Is your patient about to fall? J Gerontol Nurs. 1985; 11(4): 37–41.
Pynoos J, Caraviello R, and Cicero C. Lifelong housing: the anchor in aging-friendly communities. Generations. 2009; 33(2): 26–32.
Yeung P Y, et al. Higher incidence of falls in winter among older people in Hong Kong. Journal of Clinical Gerontology and Geriatrics. 2011; 2(1): 13–16.
Qian X X, et al. Seasonal pattern of single falls and recurrent falls amongst community-dwelling older adults first applying for long-term care services in Hong Kong. Age Ageing. 2020; 49(1): 125–129.
Lin L W, et al. Effect of weather and time on trauma events determined using emergency medical service registry data. Injury. 2015; 46(9): 1814–1820.
Pangman V C, Sloan J, and Guse L. An examination of psychometric properties of the mini-mental state examination and the standardized mini-mental state examination: implications for clinical practice. Appl Nurs Res. 2000; 13(4): 209–213.
Morris J N, et al. Scaling functional status within the interRAI suite of assessment instruments. BMC Geriatr. 2013; 13(1): 128.
Fries B E, et al. Pain in US nursing homes: validating a pain scale for the minimum data set. Gerontologist. 2001; 41(2): 173–179.
Burrows A B, et al. Development of a minimum data set-based depression rating scale for use in nursing homes. Age Ageing. 2000; 29(2): 165–172.
Leung I, Leung A, and Chau P. Risk Estimate of Inadequate Health Literacy (REIHL) for community-dwelling Chinese older adults. Prensented at the International Symposium on Healthy Aging, Hong Kong, March 7–8, 2015.
Hong Kong Observatory. Descriptive terms, https://www.hko.gov.hk/en/wxinfo/currwx/flw_description/flw.htm. Updated February 11 2020. Accessed September 15, 2020.
World Meteorological Organization. SEMDP Workshop: Indonesia & SEA-RCC Node on Data Services. http://www.wmo.int/pages/prog/sat/meetings/SEMDP_Workshop/documents/4.1.2-1p_2018.03.19_Ardhasena_SEMDP.pptx#:-:text=Operational%20definition%20of%20rain%20events%20(daily)%3A&text=Moderate%20rain%20%3A%2020%20%2D%2050%20mm,rain%3A%20%3E100%20mm%2Fday. Published March 19 2018. Accessed September 15, 2020.
Funding
Funding Disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards: Ethics approval was obtained from the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster.
Conflict of Interest: The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Qian, X.X., Chau, P.H., Kwan, C.W. et al. Investigating Risk Factors for Falls among Community-Dwelling Older Adults According to WHO’s Risk Factor Model for Falls. J Nutr Health Aging 25, 425–432 (2021). https://doi.org/10.1007/s12603-020-1539-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1539-5