Abstract
Background
Poor medication adherence is a major public health problem in older adults often resulting in negative health outcomes.
Objective
The objective of this review was to provide an updated summary of evidence from randomized controlled studies to determine whether interventions aimed at improving medication adherence also improve the health outcomes of older adults residing in community-based settings.
Methods
Articles that assessed medication adherence interventions and related health outcomes in elderly individuals were identified through searches of MEDLINE (1970–June 2016), the Cochrane Database of Systematic Reviews (through to June 2016), and Google Scholar. Across the 12 included studies, interventions were grouped into three main categories: behavioral/educational (n = 3), pharmacist-led (n = 7), and reminder/simplification (n = 2).
Results
Among the behavioral/educational intervention studies, two showed improvements in both adherence and related health outcomes, whereas one found no changes in adherence or health outcomes. Among the pharmacist-led studies, three showed improvements in both adherence and related health outcomes, while three reported no changes in adherence or health outcomes. One found an improvement in adherence but not health outcomes. Among the reminder/simplification studies, both studies reported improvements in adherence without a significant impact on related health outcomes.
Conclusion
This evidence-based review of medication adherence interventions in older adults revealed promising strategies in the larger context of a largely mixed body of literature. Future patient-centered and multidisciplinary interventions should be developed and tested using evidence-based principles to improve medication adherence and health outcomes in older adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prior reviews of medication adherence interventions are limited in that they were not specific to the elderly population, did not include studies outside the USA, or have not been updated recently. |
Of the 12 included studies, five interventions successfully improved both medication adherence and related health outcomes in older adults: two studies involved behavioral/educational interventions and three pharmacist interventions. |
Future patient-centered and multidisciplinary interventions should be developed and tested using evidence-based principles to improve medication adherence with attention to the health outcomes of older adults. |
1 Introduction
Poor medication adherence is a major public health problem in older adults [1–3]. It has been estimated that medication non-adherence (i.e., filling a prescription for a drug at a pharmacy but subsequently taking the medication erratically or entirely stopping) may occur in 50% of older adults, resulting in substantial morbidity and health services use with annual costs in the USA between US$100 billion and US$300 billion [1, 2, 4]. While older adults are no more likely than younger adults to have medication adherence difficulties, they often have higher co-morbidity burden with greater numbers of prescribed drugs and, as such, stand to face worse health-related risks when non-adherence does occur.
Given the scope of this public health problem, it is not surprising that several reviews have summarized the published evidence to improve medication adherence [5–7]. However, these reviews were limited in that they were not specific to the elderly population, did not include studies outside the USA, or were outdated [5–7]. Thus, the objective of this review article was to provide an updated summary of evidence from randomized controlled studies to determine whether interventions aimed at improving medication adherence also improve the health outcomes of older adults residing in community-based settings.
2 Methods
Articles that assessed medication adherence interventions and related health outcomes in elderly individuals were identified through searches of MEDLINE (1970–June 2016), the Cochrane Database of Systematic Reviews (through June 2016), and Google Scholar. For the purpose of this review, we defined medication adherence as the extent to which the patient’s behavior in terms of taking medications coincides with the clinical prescription [1–3]. The search used a combination of the following terms: elderly and medication adherence. Additional publications were identified by a manual search of the reference lists of identified articles, the authors’ own materials, and published reviews [5–7]. Studies were included that met the following criteria: the sample focused on older adults (i.e., mean age ≥60 years), the design was a randomized controlled trial, and the primary or secondary outcome was medication adherence and other important health outcomes related to drug therapy, including the ‘Ds’: death, disease, dollars (such as those associated with increased health services use), disability, discomfort, and dissatisfaction [8].
3 Data Synthesis/Results
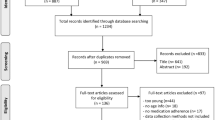
The initial literature search identified 3305 abstracts, which were reviewed for further assessment. A total of 21 manuscripts were pulled for review among the authors. Nine were excluded either because medication adherence was not the primary/secondary outcome or the study only included intermediate process measures (i.e., blood pressure, cholesterol) [9–17]. Thus, this review includes 12 articles, which are summarized in Table 1 [18–29]. In Sects. 3.1–3.3 we provide an annotation and critique for each included study. Study annotations have been categorized by the type of intervention employed: behavioral/educational (n = 3), pharmacist-led (n = 7), and reminder/simplification (n = 2).
3.1 Behavioral/Educational Interventions
Daley et al. [18] studied the impact of a brief, cognitive-behavioral approach aimed at facilitating a process of shared decision making (called ‘adherence therapy’) on medication adherence and quality of life in older adults with idiopathic Parkinson’s disease. Participants were included if at baseline they demonstrated medication non-adherence per the Morisky Medication Adherence Scale (MMAS). Intervention participants received seven weekly one-to-one ‘adherence therapy’ sessions in their home. Key components of the intervention included modifying beliefs and exploring ambivalence in taking medications. It incorporated four main skills: keeping patients engaged/minimizing resistance, exchanging information, using Socratic dialogues to generate belief discrepancies, and identification/amplification of the personally relevant benefits to treatment. Primary outcomes were change in adherence (per the MMAS) and quality of life from baseline to week 12 of follow-up.
A total of 76 patients were randomized to intervention (n = 38) or control (n = 38). At week 12, the intervention significantly improved adherence compared with control. The number needed to treat was 2.2. The intervention also significantly improved Parkinson’s disease-related quality of life, including improvements in mobility, activities of daily living, emotional well-being, cognition, communication, and body discomfort. Strengths of the study included a novel intervention that can be delivered following a short training period, inclusion of medication non-adherent patients, and delivery of the intervention in patients’ homes. Limitations included a relatively short-term follow-up, use of only one therapist for intervention delivery, and use of a crude measure of medication adherence.
Goeman et al. [19] conducted a trial comparing person-centered education including inhaler device technique versus written information-only education among community-dwelling older adults (>55 years) with asthma. The intervention tested was called the Patient Asthma Concerns Tool (PACT), which is an instrument to tailor education to improve asthma-related health literacy and address patient concerns and unmet needs. A total of 114 participants were randomized to the intervention group (n = 58) or control group (n = 56). Outcomes were asthma control measured using the Asthma Control Questionnaire [30], adherence to preventer medication (measured via electronic monitoring by dose counter), asthma-related quality of life, asthma exacerbations, and written action plan ownership. All outcomes were assessed at baseline, and 3 and 12 months post-intervention.
Overall, the study found that intervention participants had improvements in asthma control, adherence to asthma preventer medication, reduced exacerbations, improved quality of life, and an increase in asthma action plan ownership at 3 and 12 months. Strengths included the patient-centered intervention allowing for tailored education, use of an objective adherence measure, and a relatively long-term follow-up period. Limitations included the delivery of unblinded patient education and exclusion of older adults with moderate to severe cognitive impairment.
Solomon et al. [20] conducted a study designed to improve osteoporosis medication adherence (i.e., estrogen, bisphosphonates, teriparatide, calcitonin), measured by the medication possession ratio. Participants were randomized to intervention (n = 1046) or control (n = 1041), and all were ≥65 years, lived in Pennsylvania, USA, and were enrolled in a state-run medication assistance program for those with low income. The intervention included ten motivational interviewing counseling sessions by a well-trained and monitored health educator who discussed topics such as talking with physicians about their medication, managing medication adverse effects, the need for calcium and vitamin D use, and fall prevention. In addition, intervention participants were asked open-ended questions to share their attitudes about medication adherence and any barriers to long-term osteoporosis medication use. Both groups were mailed written information on topics such as exercise, fall prevention, and calcium use.
Overall, there was no statistically significant difference in median adherence by group status (intervention group = 49%; control group = 41%). Moreover, the intervention had no effect on the secondary outcomes of medication persistence, self-reported fractures, falls, or health. Strengths of the study included the large sample size and the use of a novel intervention. Limitations included missing data due to patients changing to Medicare Part D and greater numbers lost to follow-up and dropouts in the intervention group.
3.2 Pharmacist-Led Interventions
Al-Rashed et al. [21] studied the effect of pharmaceutical counseling on medication adherence, medication knowledge, and health services utilization in 83 hospitalized elderly patients who were prescribed four or more drugs at hospital discharge. Patients in both control and intervention arms received a medication discharge summary and a simple medicine reminder card, and arrangements for pharmacist home visits to patients 2–3 weeks and 3 months after discharge to assess medication discrepancies and health services utilization. The main intervention tested in this study was pharmacist counseling on medications and adherence before discharge.
Adherence (measured via pill counts) was significantly better at the two home visits in the intervention group than in the control group. Importantly, at visit two, the intervention group had significantly fewer outpatient physician visits than the control group and significantly fewer hospital readmissions (p < 0.05). Some potential limitations include that adherence measurement may not have been blinded, there may have been differences between the two hospital wards from which the patients were enrolled, there was no examination to determine whether the health services use was drug related (i.e., due to therapeutic failure), and the analyses were not adjusted for important confounders.
Lipton and Bird [22] examined the impact of a pharmacist intervention at hospital discharge on medication adherence and healthcare utilization in 706 older adults who were prescribed three or more drugs at discharge. Patients in both control and intervention arms received a booklet in which to record medication information such as purpose, dosage, and schedule. The pharmacists conducted a face-to-face consultation with every intervention patient before hospital discharge to discuss the purpose and use of their medications and potential drug-related problems. Follow-up visits (primarily via telephone) were conducted at 1 week, 2–4 weeks, 2 months, and 3 months post-discharge.
Medication adherence (measured via structured telephone interviews) was found to be significantly higher at the first assessment in the intervention group than in the control group (mean score 94.4 vs. 91.4; p = 0.04) as well as at the second assessment (96.3 vs. 91.2; p < 0.001). There were no significant differences between groups in the pre-specified healthcare utilization measures. Some potential limitations include the fact that the adherence analysis did not measure a change score over time, but rather it was simply cross-sectional analyses at each follow-up period. The study also measured adherence using only one approach—self-reported. In addition, the study was likely underpowered to detect differences in drug-related healthcare utilization.
Murray et al. [23] studied the effect of a pharmacist intervention in inner-city outpatients (≥50 years) with heart failure. They randomized 314 patients with heart failure to the intervention, aimed at persons with limited resources and low health literacy; patients were randomly assigned to the intervention (n = 122) or usual pharmacy care (n = 192). The intervention protocol was designed to address the self-care needs of older adults, such as communicating with physicians, lack of in-home support, impaired cognition, and poor vision or hearing. In addition, specially designed and tested written medication materials were provided to patients, including icon stickers placed on medication containers and the corresponding medication information sheet (such as the Ace of Hearts for ACE inhibitors). At baseline, the pharmacist met with participants to conduct a comprehensive medication history, and to describe the use of the electronic adherence monitors. The intervention lasted 9 months with a 3-month post-intervention follow-up period to determine post-intervention effects on treatment adherence (measured with electronic monitors, prescription refills, and self-report). Primary outcomes included adherence measured by electronic monitors and heart failure exacerbation requiring emergency department care or hospitalization.
Medication adherence during the 9-month intervention period was 78.8% in the intervention group versus 67.9% in the usual care group. The intervention effect dissipated in the 3-month post-intervention period, suggesting the importance of a sustained intervention by the pharmacist. Emergency department visits and hospitalizations were significantly lower in the intervention group than in the control group, and direct health care costs per patient were US$2960 less. The study was limited by the inclusion of relatively young older adults (62 ± 8 years) and use of only one pharmacist, which precluded studying the effects of pharmacist characteristics.
Nazareth et al. [24] conducted a randomized controlled trial of a pharmacist intervention involving 362 hospitalized patients aged >75 years who were taking more than four medications. At hospital discharge, a hospital pharmacist assessed patients’ medication-management skills and provided written and verbal information to enhance adherence. This was followed by a community pharmacist home visit within 2 weeks of discharge, who again stressed adherence and medication knowledge. A research assistant collected information about outcome measures at 3 and 6 months.
Overall, there were no significant between-group differences in hospital readmissions, use of other health services, general well-being, satisfaction, medication adherence, or medication knowledge at 3 or 6 months. Strengths of this study included having the community pharmacist conducting a home visit and the measurement of important distal health outcomes. This study was limited by high dropout rates (26%) and the use of a simple medication adherence measure (i.e., 0 = none, 1 = total/highest level for each drug and an overall mean calculated for the regimen). In addition, no mention of blinding was made regarding outcome assessment, and the study was underpowered to detect drug-related readmissions.
Olesen et al. [25] studied the effect of pharmaceutical care in outpatients from Denmark who were ≥65 years taking five or more drugs without supervision. The original study randomized 945 participants to two types of intervention (i.e., pharmaceutical care or an electronic reminder system) or a usual care control group. The electronic reminder system intervention arm was not included in their article; thus, the reported pharmaceutical care intervention included 315 participants and the control group 315 participants. The intervention entailed three aspects of pharmaceutical care, namely the identification of drug-related problems, taking steps to correct these problems, and preventing potential problems. Intervention participants were visited at their homes by one of nine pharmacists and followed by three telephone calls over the course of 1 year. The primary aim was to determine the impact of pharmaceutical care on medication adherence (assessed by pill count), hospitalization, and death.
The results failed to show a statistically significant impact of the intervention on any of the outcomes of interest. The study was sufficiently powered to assess the effect of treatment adherence but may have been underpowered to assess the endpoints of hospitalization and mortality. The study was limited by an 18% overall dropout that was greater in the intervention group (20 vs. 16%), largely owing to a lack of patient interest. The study highlights the need to include patients who have some interest in the pharmaceutical care components in order to improve retention.
Wu et al. [26] conducted a study in Hong Kong hospital-based outpatient clinics. Patients were included if they were taking five or more long-term medications and were deemed to have adherence problems. The intervention consisted of a brief (10- to 15-min) telephone call from a pharmacist between clinic visits throughout the study period. During this phone call, the pharmacist reviewed any concerns about the patient’s medications and stressed the importance of medication adherence. Medication adherence was assessed after 2 years for each drug and was defined as taking between 80 and 120% of the amount prescribed daily. A composite measure for the entire medication regimen was calculated by dividing the number of drugs that the patient was adherent to by the total number of medications. Distal outcomes measured included mortality and health services use.
The intervention improved adherence and reduced death (25 vs. 38 in the intervention vs. control groups). The intervention group also had fewer hospitalization and emergency room visits. There is low risk of bias that the death outcome measure was misclassified. However, the authors reported that between screening and randomization slightly more than 50% of patients resolved their medication adherence problems. Moreover, they used a crude adherence measure, and outcome assessment was not blinded. In addition, information discussed between the pharmacist and the patient was not fed back to the clinic staff due to frequent changes of attending doctors. In summary, this intervention improved outcomes, but it is not clear that the study findings can be scaled or replicated.
Volume et al. [27] conducted a randomized controlled cluster trial of comprehensive pharmaceutical care services at 12 community pharmacies in Alberta, Canada (five intervention, seven controls). Community-dwelling older adults (≥65 years) using three or more medications at participating pharmacies were included. The intervention focused on identifying, preventing, and resolving drug-related problems. Treatment pharmacies used an initial interview and frequent follow-up communication with the patient and other caregivers. Outcomes included medication adherence (measured by 4-item MMAS), patients’ expectations of the care they receive from their pharmacist, patients’ satisfaction with pharmacy services, and health-related quality of life. A telephone survey was used to collect data at baseline, 6–7 months post-intervention, and 12–13 months post-baseline.
A total of 292 patients completed all three telephone interviews. Medication adherence and health-related quality of life were not significantly affected by the intervention. Small positive changes on patients’ expectations and satisfaction (e.g., pharmacists’ communication with physicians) were found among intervention pharmacies. Strengths of the study included use of a robust study design and broad inclusion criteria. Limitations iincluded enrolling patients with high adherence at baseline and use of a coarse measure of adherence.
3.3 Reminder/Simplification Interventions
Fulmer et al. [28] examined whether daily videotelephone or regular telephone reminders would increase medication adherence in older adults with heart failure. Community-dwelling older adults (≥65 years) were randomized to one of three arms: a control group that received usual care (n = 18); a group that received regular daily telephone call reminders (n = 15); and a group that received videotelephone call reminders (n = 17). The study included a 2-week period of baseline adherence monitoring, a 6-week intervention phase with daily telephone or videotelephone calls, and a 2-week post-intervention adherence monitoring period. During the 6-week intervention period, a telephone or videotelephone call was made daily, and the patients were asked whether they had taken their medications the previous day. Medication adherence was measured by Medication Event Monitoring System (MEMS) caps for a maximum of four heart failure medications per patient. Quality of life and heart failure symptoms were measured at baseline and the end of the study (10 weeks).
There was a significant improvement in adherence for both groups receiving calls (either by telephone or videotelephone) compared with control, but there were no significant differences between the two intervention groups. There was no significant change in quality of life, but there was significant improvement in the heart failure symptom scores across all groups. However, there were no differences among groups, suggesting no differential impact of the interventions compared with control. Strengths included use of an objective measure of medication adherence across multiple medications and assessment of two interventions. Limitations included a small sample size, short-term follow-up, and use of what would now be considered outdated technology.
Schneider et al. [29] studied the effect of a daily-dose blister-pack calendar for patients ≥65 years from two US health systems (Ohio and Arizona) prescribed the ACE inhibitor lisinopril over 1 year. The blister pack contained 28 days of lisinopril, requiring return to the pharmacy for refills at regular intervals. Of 112 randomized participants, 24% were dropped from analysis because they did not fill their prescriptions (nine intervention and ten controls) or they filled fewer than six prescriptions over the course of study (four intervention and four controls). Adherence was measured as the percentage of refills on time (±5 days) and the medication possession ratio. Other endpoints assessed by chart review included blood pressure at baseline and 6 and 12 months; evidence of angina, stroke, or myocardial infarction; and emergency department visits and hospitalizations.
After excluding obvious non-adherers, intervention participants had greater on-time lisinopril refills (80.4 vs. 66.1%; p = 0.012) and a higher medication possession ratio (0.93 vs. 0.87; p = 0.039). There was a modest effect on diastolic blood pressure but not on systolic blood pressure. The effects on cardiovascular events, emergency department visits, and hospitalizations were not significant. The study was limited by the post-randomization exclusion of 24% of participants. Furthermore, the calendar blister pack only contained one medication (i.e., lisinopril) and could be impractical for multiple medications, which is often the case in older adults.
4 Discussion
This evidence-based review, to the best of our knowledge, is among the first to annotate and critique studies of medication adherence interventions tailored towards older adults and focused on improving health outcomes. We identified 12 relevant studies, of which three were initiated at time of hospital discharge [21, 22, 24] and four in part or entirely used a telephone intervention [20, 22, 25, 26, 28]. The remaining studies were conducted face-to-face in community or ambulatory care sites. It is also of interest to note that the most common target populations were those with polypharmacy (n = 6) [21, 22, 24–26] and congestive heart failure [23, 28]. There was no dominating approach to measure adherence. Three studies used pharmacy claims alone [20, 26, 29], two used electronic monitoring alone [19, 28], four used self-report alone [18, 22, 24, 27], and two used pill counts alone [21, 25]. Only the study by Murray et al. [23] used three approaches (i.e., electronic monitors, prescription refills, and self-report) to measure medication adherence.
This review of medication adherence interventions designed to improve related health outcomes in older adults revealed promising strategies in the larger context of a largely mixed body of literature. Overall, among the behavioral/educational intervention studies, two showed improvements in both adherence and related health outcomes [18, 19], whereas one found no changes in adherence or health outcomes [20]. Among the pharmacist-led studies, three showed improvements in both adherence and related health outcomes [21, 23, 26], while three reported no changes in adherence or health outcomes [24, 25, 27]. One study found an improvement in adherence but not health outcomes [22]. Finally, among the reminder/simplification studies, both studies reported improvements in adherence without a significant impact on related health outcomes [28, 29].
Taken together, there are a few important lessons to be learned from the medication adherence intervention literature. First, the measurement of medication adherence is complex and widely heterogeneous. While guidelines exist to standardize the measurement of claims-based medication adherence [31], huge variation remains across studies. Because different methods of adherence measurement capture different constructs, future investigators should use multiple measurements to capture a broader range of adherence information and should assess adherence at multiple timepoints [4]. Second, interventions should target individuals who stand to benefit from medication adherence interventions. Studies with high baseline adherence rates face difficulty in showing any positive impact of the intervention due to a ceiling effect. Conn et al. [32] showed in a systematic review and meta-analysis that interventions targeting those with medication adherence problems have modest but significant effects on medication-taking behavior. Third, small sample sizes leading to low power limited most identified studies. As such, future studies should be adequately powered to detect important clinical differences in health outcomes. Fourth, interventions incorporating behavior change techniques hold tremendous promise. Kahwati et al. [33] conducted a qualitative comparative analysis in order to identify necessary or sufficient configurations of behavior change techniques among effective medication adherence interventions; they found that increasing knowledge and self-efficacy was the most empirically relevant intervention configuration. Fifth, pharmacist-led interventions hold promise but should be designed carefully. We found a 50% success rate among the identified pharmacist-led studies in terms of improving adherence and outcomes. Most of the negative studies were limited by small sample sizes and short-term follow-up. Sixth, medication adherence is a necessary but not always sufficient component to improving health outcomes (as seen in the reminder/simplification studies). This is important because future studies should consider factors other than medication adherence that could impact the outcomes in order to draw valid inferences. Finally, interventions not targeting a specific condition should measure the outcome of adverse drug events, specifically therapeutic failures. This is important because a study of therapeutic failure-related hospitalizations among older veterans found that the majority of preventable therapeutic failure-related hospitalizations were due to medication non-adherence [34].
Furthermore, a paper by Bosworth et al. [35] highlights the promise of using patient-centered care approaches, such as motivational interviewing, counseling, and shared decision-making, to improve medication adherence for those with chronic conditions. The authors recommend the following strategies to improve medication adherence: (1) generate options to give the patient an opportunity to be involved in his or her care; (2) decide on a mutually agreeable and measureable regimen; (3) understand a patient’s knowledge on their chronic condition; and (4) screen for readiness to change (i.e., improve adherence) [35]. Future studies are needed to examine the impact of these strategies on medication adherence and related health outcomes in older adults.
Moreover, a group of experts in geriatrics, pharmacology, epidemiology, and public health published a consensus statement on the best possible interventions to improve medication adherence in older adults [36]. They identified seven interventions, including (1) comprehensive geriatric assessment; (2) patient (and caregiver) education to improve patient empowerment; (3) optimization of treatment; (4) use of adherence aids; (5) physician and other healthcare professionals’ education; (6) adherence assessment; and (7) facilitating access to medicine by service integration [36]. The authors emphasize the importance of a multidisciplinary approach in order to make progress in this area. Future patient-centered interventions are clearly needed to improve adherence and, in turn, related health outcomes. It is important to note that patient-centered interventions are also needed to improve overall prescribing quality, a first important step toward improving adherence [37].
This review has several potential limitations worth mentioning. Publication bias may exist because negative studies are less likely to have been published. In addition, although MEDLINE, the Cochrane Database of Systematic Reviews, and Google Scholar were searched for relevant articles, it is possible that some studies may have been missed if they were indexed in other databases. To minimize the chance of missing such studies, the authors manually searched the reference lists of the identified articles, recent review articles, as well as their personal files to identify potential studies for inclusion. The search strategy was also limited to the English language, to older adults, and to randomized controlled trials because the intent of the review was to evaluate the impact of medication adherence interventions on older adults. Using such strict inclusion criteria may limit the generalizability of this review.
5 Conclusion
Studies using various types of interventions have reported mixed findings with regard to improving adherence and related health outcomes in older adults in the community. Successful interventions involved behavioral/educational and pharmacist interventions. Future patient-centered and multidisciplinary interventions should be developed and tested using evidence-based principles to improve medication adherence and health outcomes in older adults.
References
Hughes CM. Medication non-adherence in the elderly: how big is the problem? Drug Aging. 2004;21(12):793–811.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97.
Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23.
Marcum ZA, Gellad WF. Medication adherence to multidrug regimens. Clin Geriatr Med. 2012;28(2):287–300.
Conn VS, Hafdahl AR, Cooper PS, Ruppar TM, Mehr DR, Russell CL. Interventions to improve medication adherence among older adults: meta-analysis of adherence outcomes among randomized controlled trials. Gerontologist. 2009;49(4):447–62.
Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RC, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157(11):785–95.
Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014;(11):CD000011.
Lohr KN. Outcome measurement: concepts and questions. Inquiry. 1988;25(1):37–50.
Gray TA, Fenerty C, Harper R, Spencer AF, Campbell M, Henson DC, et al. Individualised patient care as an adjunct to standard care for promoting adherence to ocular hypotensive therapy: an exploratory randomised controlled trial. Eye (Lond). 2012;26(3):407–17.
Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol. JAMA. 2006;296(21):2563–71.
Mosca C, Castel-Branco MM, Ribeiro-Rama AC, Caramona MM, Fernandez-Llimos F, Figueiredo IV. Assessing the impact of multi-compartment compliance aids on clinical outcomes in the elderly: a pilot study. Int J Clin Pharm. 2014;36(1):98–104.
Obreli-Neto PR, Guidoni CM, de Oliveira Baldoni A, Pilger D, Cruciol-Souza JM, Gaeti-Franco WP, et al. Effect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patients. Int J Clin Pharm. 2011;33(4):642–9.
Porter AK, Taylor SR, Yabut AH, Al-Achi A. Impact of a pill box clinic to improve systolic blood pressure in veterans with uncontrolled hypertension taking 3 or more antihypertensive medications. J Manag Care Pharm. 2014;20(9):905–11.
Ruppar TM. Randomized pilot study of a behavioral feedback intervention to improve medication adherence in older adults with hypertension. J Cardiovasc Nurs. 2010;25(6):470–9.
Stewart K, George J, Mc Namara KP, Jackson SL, Peterson GM, Bereznicki LR, et al. A multifaceted pharmacist intervention to improve antihypertensive adherence: a cluster-randomized, controlled trial (HAPPy trial). J Clin Pharm Ther. 2014;39(5):527–34.
Tinsel I, Buchholz A, Vach W, Siegel A, Durk T, Buchholz A, et al. Shared decision-making in antihypertensive therapy: a cluster randomised controlled trial. BMC Fam Pract. 2013;14:135.
Hanlon JT, Weinberger M, Samsa GP, Schmader KE, Uttech KM, Lewis IK, et al. A randomized, controlled trial of a clinical pharmacist intervention to improve inappropriate prescribing in elderly outpatients with polypharmacy. Am J Med. 1996;100:428–37.
Daley DJ, Deane KH, Gray RJ, Clark AB, Pfeil M, Sabanathan K, et al. Adherence therapy improves medication adherence and quality of life in people with Parkinson’s disease: a randomized controlled trial. Int J Clin Pract. 2014;68(8):963–71.
Goeman D, Jenkins C, Crane M, Paul E, Douglass J. Educational intervention for older people with asthma: a randomised controlled trial. Pat Educ Counsel. 2013;93(3):586–95.
Solomon DH, Gleeson T, Iversen M, Avorn J, Brookhart MA, Lii J, et al. A blinded randomized controlled trial of motivational interviewing to improve adherence with osteoporosis medications: design of the OPTIMA trial. Osteoporos Intern. 2010;21(1):137–44.
Al-Rashed SA, Wright DJ, Roebuck N, Sunter W, Chrystyn H. The value of inpatient pharmaceutical counselling to elderly patients prior to discharge. Br J Clin Pharmacol. 2002;54(6):657–64.
Lipton HL, Bird JA. The impact of clinical pharmacists’ consultations on geriatric patients’ compliance and medical care use: a randomized controlled trial. Gerontol. 1994;34:307–15.
Murray MD, Young J, Hoke S, Tu W, Weiner M, Morrow D, et al. Pharmacist intervention to improve medication adherence in heart failure: a randomized trial. Ann Intern Med. 2007;146(10):714–25.
Nazareth I, Burton A, Shulman S, Smith P, Haines A, Timberal H. A pharmacy discharge plan for hospitalized elderly patients—a randomized controlled trial. Age Ageing. 2001;30(1):33–40.
Olesen C, Harbig P, Buus KM, Barat I, Damsgaard EM. Impact of pharmaceutical care on adherence, hospitalisations and mortality in elderly patients. Int J Clin Pharm. 2014;36(1):163–71.
Wu JY, Leung WY, Chang S, Lee B, Zee B, Tong PC, et al. Effectiveness of telephone counselling by a pharmacist in reducing mortality in patients receiving polypharmacy: randomised controlled trial. BMJ. 2006;333(7567):522.
Volume CI, Farris KB, Kassam R, Cox CE, Cave A. Pharmaceutical care research and education project: patient outcomes. J Am Pharm Assoc (Wash). 2001;41(3):411–20.
Fulmer TT, Feldman PH, Kim TS, Carty B, Beers M, Molina M, et al. An intervention study to enhance medication compliance in community-dwelling elderly individuals. J Gerontol Nurs. 1999;25(8):6–14.
Schneider PJ, Murphy JE, Pedersen CA. Impact of medication packaging on adherence and treatment outcomes in older ambulatory patients. J Am Pharm Assoc (2003). 2008;48(1):58–63.
Juniper EF, O’Byrne PM, Ferrie PJ, King DR, Roberts JN. Measuring asthma control. Am J Respir Crit Care Med. 2000;162(4 Pt 1):1330–4.
Peterson AM, Nau DP, Cramer JA, Benner J, Gwadry-Sridhar F, Nichol M. A checklist for medication compliance and persistence studies using retrospective databases. Value Health. 2007;10(1):3–12.
Conn VS, Ruppar TM, Enriquez M, Cooper P. Medication adherence interventions that target subjects with adherence problems: systematic review and meta-analysis. Res Soc Admin Pharm. 2016;12(2):218–46.
Kahwati L, Viswanathan M, Golin CE, Kane H, Lewis M, Jacobs S. Identifying configurations of behavior change techniques in effective medication adherence interventions: a qualitative comparative analysis. Syst Rev. 2016;5:83.
Marcum ZA, Pugh MV, Amuan ME, Aspinall SL, Handler SM, Ruby CM, et al. Prevalence of potentially preventable unplanned hospitalizations caused by therapeutic failures and adverse drug withdrawal events among older veterans. J Gerontol A Biol Sci Med Sci. 2012;67(8):867–74.
Bosworth HB, Fortmann SP, Kuntz J, Zullig LL, Mendys P, Safford M, et al. Recommendations for providers on person-centered approaches to assess and improve medication adherence. J Gen Intern Med. (Epub 2016 Sep 6).
Marengoni A, Monaco A, Costa E, Cherubini A, Prados-Torres A, Muth C, et al. Strategies to improve medication adherence in older persons: consensus statement from the Senior Italia Federanziani Advisory Board. Drugs Aging. 2016;33:629–37.
Onder G, van der Cammen TJM, Petrovic M, Somers A, Rajkumar C. Strategies to reduce the risk of iatrogenic illness in complex older adults. Age Ageing. 2013;42:284–91.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Dr. Marcum is supported by funding from the Agency for Healthcare Research and Quality (AHRQ) (K12HS022982). Dr. Hanlon is supported by funding from National Institutes of Health (NIH)/National Institute on Aging (NIA) (P30AG024827, T32AG021885, U13AG047008) and AHRQ (R18HS023779). Dr. Murray is supported by funding from an endowment on medication safety from Purdue University (Indianapolis, IN, USA) and the Regenstrief Foundation.
Conflict of interest
The authors have no conflicts of interest, including financial interests, activities, relationships or affiliations, relevant to this study.
Rights and permissions
About this article
Cite this article
Marcum, Z.A., Hanlon, J.T. & Murray, M.D. Improving Medication Adherence and Health Outcomes in Older Adults: An Evidence-Based Review of Randomized Controlled Trials. Drugs Aging 34, 191–201 (2017). https://doi.org/10.1007/s40266-016-0433-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-016-0433-7