Abstract
Objectives
To assess the association between malnutrition and physical frailty among nursing home older adults in China.
Design and setting
A cross-sectional study in 15 nursing homes in Changsha, China.
Participants
A total of 705 nursing home residents who were aged 60 and older.
Measurements
Physical frailty was identified based on the following five components: slow gait speed, low physical activity, weight loss, exhaustion, and low grip strength. Nutritional status was assessed using the Mini Nutritional Assessment. Multinomial logistic regression models were used to analyze the association between nutritional status and physical frailty.
Results
The mean (SD) age of the participants was 82.5 (8.1) years old (range, 60–106 years), and 226 (32%) was men. Of those participants, 5.1% and 55.6% were malnourished and at risk of malnutrition, respectively; 60.3% and 36.2% were identified as being frail and prefrail, respectively. Compared with participants who were well-nourished, those who were at risk of malnutrition or malnourished were two times more likely to be physically frail (adjusted odds ratio 2.66, 95% confidence interval 1.01 to 7.00), after adjustment for age, education level, cognitive status, depressive symptoms, and disability in activities of daily living. No significant association was observed between malnutrition and physical prefrailty.
Conclusion
Our findings suggest that poor nutritional status and physical frailty are highly prevalent in nursing home older adults in China, and that poor nutritional status is associated with increased odds of physical frailty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Physical frailty is characterized by increased vulnerability to poor resolution of homeostasis after a stressor event, which confers an increased risk of adverse outcomes, including falls, delirium, disability, and death (1–3). Physical frailty is highly prevalent among community-dwelling older adults (1) and has been reported to affect approximately 52% of nursing home residents from different countries (e,g., Brazil, Spain, Lebanon, Egypt, Poland and the Netherlands) in a systematic review and meta-analysis (4). Since physical frailty is reversible (5), identification of modifiable risk factors of physical frailty is of substantial clinical interest.
Considerable interest has been directed towards nutrition in terms of the prevention of physical frailty in older adults in recent years (6, 7). Several epidemiological studies among community-dwelling older adults have reported that malnutrition was significantly associated with increased odds of physical frailty (8, 9). Malnutrition is a state of deficiency, imbalance, or excess of protein, energy, or other nutrients that contribute to adverse health and psychosocial outcomes (10, 11). A recent meta-analysis of studies in communitydwelling older adults also reported that approximately two thirds of malnourished older adults were physically frail (9). Nevertheless, epidemiologic data investigating this association among nursing home older adults are sparse. A meta-analysis of 10 studies from different countries (e.g., Belgium, Germany, Turkey, Spain, Mexico and Russia) reported that malnutrition was greatly associated with physical frailty (9). To the best of our knowledge, no study has investigated this association in nursing home older residents in China, a country with the rapid aging and small-scale families where older adults are known to be more likely to choose to spend their later years in the nursing homes (12, 13). Therefore, the present study aimed to investigate the association between malnutrition/nutritional risk status and physical frailty in a population of nursing home older adults in China.
Methods
Study design and Population
We conducted a cross-sectional study among older adults who were aged 60 and older and resided in 15 nursing homes in Changsha, Hunan province, China. Changsha is a middlesized provincial city with a population of eight million in the central region of China, characterized as having low population mobility and a conventional Chinese lifestyle. During the period of January and December 2018, we administered a survey comprising a questionnaire, anthropometric measurements, and physical fitness tests. The assessments and tests were conducted by well-trained registered nurses. Before the beginning of the survey, all staffs were trained according to standard protocols for organizing the assessment measures and tests. During the survey, we contacted all the older residents by sending brochures (n = 1973). A total of 1527 residents agreed to participate, with a participating rate 77.4%. Of those, 1027 were able to complete the survey, except for those who had died or retired from those nursing homes (n = 500) when the time of baseline survey. For the present study, we excluded participants who had a history of dementia (n = 7), Parkinson’s disease (n = 12), stroke (n = 78), or a Mini-Mental State Examination (MMSE) score > 18 (n = 57) from the final analyses. Of the remaining 873 participants, 168 were further excluded from the sample due to having missing data on any components of physical frailty. Thus, the final sample consisted of 705 older men and women (Figure 1). The study protocol was approved by the Institutional Review Board of behavioral and nursing research in Xiangya Nursing School of Central South University (2019008), and written informed consent was obtained from all participants.
Measures
Physical frailty
The phenotype of physical frailty was operationalized according to the criteria of Fried and colleagues (2): slow gait speed, low physical activity, weight loss, exhaustion, and low grip strength. Slowness was determined in a 5-m walking test at maximum speed, with the results stratified by sex and standing height. For men, height less than 173 cm (≥ 7 s) and height more than 173 cm (≥ 6 s) were considered the cutoff for slowness. For women, height less than 159 cm (≥ 7 s) and height more than 159 cm (≥ 6 s) were considered the cut-off for slowness. Starting from a stationary position, the participants walked 11 m on the entire lane at maximum speed without running in two trials, and the time (sec) of gait speed was measured with a digital stopwatch between the third and eighth meters in each trial. And the final gait speed (m/sec) was calculated by dividing 5 (m) by the shortest task time in the two trials (14). Low physical activity (15) was calculated using a weighted score of kilocalories expended per week. The Chinese version of the Physical Activity Scale for the Elderly (PASE) questionnaire (16), consisting of nine items, was used to collect the physical activity data. This variable was stratified by sex. For men, PASE scores less than 97.3 points was considered the cut-off for low physical activity. For women, PASE scores less than 85.4 points was considered the cut-off for low physical activity. Weight loss was defined as a participant losing more than 4.5 kg unintentionally (i.e., not through dieting or exercise) during the previous year. If the participant answered yes, they were considered as frail. Exhaustion was determined to ask two questions: “I felt that everything I did was an” in the past month) and “I could not get going.” Exhaustion was also determined on the basis of how participants responded to a question on how often they felt this way in the previous week. The participants answered the questions on a 4-point scale: 0 = rarely or none of the time (> 1 day), 1 = some or a little of the time (1–2 days), 2 = a moderate amount of the time (3–4 days), or 3 = most of the time. Subjects responding with a two or three to any of these questions were categorized as meeting the exhaustion criterion. Weakness was assessed using a handgrip dynamometer. The participants were asked to perform two squeezes with the dynamometer, using the dominant hand. The best performance, recorded as strength in kilograms per square centimeter, was used for analysis. Cut-off scores were stratified by sex and body mass index (BMI) quartiles according to the criteria of Fried and colleagues (2). For men, hand grip strength less than 29 kg (BMI ≤ 24), 30 kg (BMI = 24.1–28.0), or 32 kg (BMI < 28) was considered the cut-off for weakness. For women, hand grip strength less than 17 kg (BMI ≤ 23.0), 17.3 kg (BMI = 23.1–26.0), 18 kg (BMI = 26.1–29.0), or 21 kg (BMI < 29.0) was considered the cut-off for weakness. Subjects with three or more affected components were considered frail, those with one or two affected components were considered prefrail, and those without any affected components were considered robust.
Nutritional status
We assessed the nutritional status of the participants by using the Chinese version of the Mini Nutritional Assessment (MNA) (17, 18). The full MNA is an effective and validated screening tool for assessing the nutritional status of older people, and it can provide additional information about the causes of malnutrition in those identified as malnourished or at risk of malnutrition. The MNA takes 10–15 minutes to complete; it addresses nutritional intake, involuntary weight loss, mobility, psychological stress or acute disease, neuropsychological problems, and BMI or calf circumference. The height, weight and calf circumference were measured by trained nurses, and individual BMI was calculated according to body weight (in kilograms) divided by height (in meters) squared. The participants were divided into three categories (total score = 30): normal nutritional status (> 17), at risk of malnutrition (17–23.5), or malnourished (< 23.5). Being malnourished or at risk of malnutrition was regarded as having poor nutritional status.
Covariates
Sociodemographic variables were measured using the questionnaire, including age, sex, marital status, living status (e.g., living with husband/wife), and education level; physical health status was estimated according to the number of comorbidities (with the self-report of a medical disorder diagnosed and treated by a physician being recorded). Cognitive function was measured by using the Chinese version of MMSE (19). The MMSE tests were administered to the participants by well-trained nurses, with the total score > 24 indicating cognitive impairment. Depressive symptom was measured by using the Geriatric Depression Scale (GDS) (20), with a total score ≥ 11 indicating clinically significant depressive symptom. Activities of daily living (ADL) ability was measured by using the Katz scale (21), including bathing, dressing, toileting, transferring, continence and feeding. ADL disability was defined as shaving difficulty and/or requiring assistance in ≥ 1 activities. Polypharmacy was considered to be current use of ≥ 3 prescribed medications on a regular basis. The information on history of dementia, Parkinson’s disease, and stroke were collected from the medical record.
Statistical analysis
Characteristics of the sample were summarized by nutritional status groups. The values were presented as percentages for categorical variables and means (standard deviations) for continuous variables. Comparisons of the characteristics among the three groups of nutritional status were made by using the Chi-square tests for categorical variables and one-way analysis of variance for continuous variables.
Multinomial logistic regression analysis was carried out to examine the association between malnutrition and physical frailty. A multivariable-adjusted model was run to estimate the odds ratio (OR) and 95% confidence interval (CI) for the risk of physical frailty. The following covariates were entered into the multivariable model in a stepwise backward fashion: sociodemographic indicators: age (continuous), living status (living with husband/life, or living with alone or others), education level (elementary or below, junior or senior high, or college or above), cognitive impairment (yes or no), depressive symptom (yes or no), and ADL disability (yes or no). Multicollinearity between independent variables in the multivariable model was ruled out by using the variance inflation factor (VIF) test, with a value less than 2 indicating as appropriate. All statistical analyses were performed using IBM SPSS Statistics Version 24.0 (IBM; Armonk, NY, USA). All p-values were two-tailed, and p > 0.05 was considered statistically significant.
Results
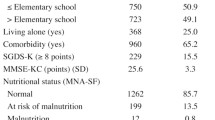
The mean (SD) age of the 705 participants included in the final sample was 82.5 (8.1) years old (range 60–106) and 226 (32%) was men. Of those participants, 5.1% were malnourished and 60.7% were at risk of malnutrition. In all, 36.2% were identified as being prefrail, and 60.3% were being frail. Table 1 shows the characteristics of participants according to nutritional status subgroups. Compared with individuals who were well-nourished, those who were at risk of malnutrition or malnourished were more likely to be women, widowed, and low-educated, and had a higher rate of comorbidity, cognitive impairment, being depressed, ADL disability, and polypharmacy (Table 1).
Table 2 shows the results of multinomial logistic regression analyses on the association between nutritional status and physical frailty. Compared with participants who were well-nourished, those who were at risk of malnutrition or malnourished had a twofold higher risk of being (OR = 2.66, 95% CI = 1.01-7.00). No significant association was observed for the association between poor nutritional status and prefrailty (OR = 1.35, 95% CI = 0.52–3.53). The following variables were also significantly associated with an increased risk of being physical frail: older age, having depressive symptom, and cognitive impairment. In addition, age and ADL disability were strongly associated with high risk of being prefrailty and frailty.
Discussion
The present study observed a highly prevalent poor nutritional status and physical frailty among the nursing-home older adults in China. Our data demonstrated that malnutrition/nutritional risk status was strongly associated with increased odds of physical frailty. In addition, cognitive impairment, depressive symptom, and ADL disability were also significantly associated with physical frailty. To the best of our knowledge, this study was one of few studies to investigate the association between malnutrition and physical frailty among nursing home older adults in China.
Prevalence of poor nutritional status and physical frailty
Our results showed that a high prevalence of poor nutritional status and physical frailty in this study. The overall prevalence of malnutrition or risk of malnutrition in this study was higher than that reported in a study of Belgium 1188 nursing-home elderly people (55.6% versus 19.4%) (22) which used the same screening measurement for malnutrition. Meanwhile, in our study, the prevalence of frailty and prefrailty were 60.3% and 36.2%, respectively. Using the Fried’s criteria, in a cohort of institutionalized older adults the prevalence was of frailty was 68.8% in Spain (23) more than our study among the older people residing in nursing homes in China. Moreover, a study among the community-dwelling older people (24) reported that 7% of adults aged 60 years or older were frail by physical frailty phenotype in China. Indeed, the nursinghome population may be more frail and malnourished because of limited access to the scientific management models and the health care services in China (25, 26). Therefore, policymakers and administrators could evaluate the frail older adults’ expected course based on information about the prevalence of poor nutritional status and physical frailty among the nursinghome elderly people in this study.
Association between malnutrition/nutritional risk status and physical frailty
We confirmed a strong association between poor malnutrition/nutritional risk status and physical frailty. Our results were in line with those reported by a study based on two nursing homes in Japan (27). For the community-dwelling elderly people in Singapore, two studies had suggested a significant association between nutritional status and frailty (8, 28). Moreover, for community-dwelling older adults (n = 1200) living in a rural setting, another study demonstrated that frailty and malnutrition were closely associated (29).
Indeed, both conditions were related, and a common phenotype in a review reported (27, 30, 31) that the loss of body weight, due to the inadequate nutrient intake and physical inactivity, resulting in muscle wasting, existed in the malnutrition and physical frailty older people.
In the current study, we demonstrated that malnutrition/nutritional risk status was associated with increased odds of physical frailty among nursing home older adults (n = 705). So it can partly explain that frailty in the elderly people might still have inadequate intake of protein and vitamin D (32); in addition, sarcopenia might be a key element of physical frailty associated with malnutrition, such as decline of muscle mass, strength and function (33). Therefore, we should take adequate certain nutrients for older adults in nursing homes after taking the effectiveness of interventions, especially improving muscles mass and function.
Other risk factors of physical frailty
In our study, a crucial finding was that poor nutritional status and frailty had two risk factors, including cognitive impairment and depression symptoms. Previous studies had reported similar results. In a study including 6045 communitydwelling elderly people in Singapore, comorbidities, cognitive impairment, depressive symptom, ADL/IADL and disability, and polypharmacy were strongly related to malnutrition and frailty (8). Meanwhile, for the cognitive function, previous literatures (34–37) reported that poor nutritional status was a major important determinant of both physical frailty and cognitive impairment; for the mental health, previous study (38) showed that depressive symptom was a major contributing risk factor for physical frailty, which in turn reportedly increased the risk of poor nutritional status. Therefore, it was not coincidental to find some common mental and cognitive risk factors with both malnutrition and physical frailty. In short, our results supported these previous findings, and suggested that the poor nutritional health of cognitive impairment or depressive symptom among the nursing-home older adults in frailty were more likely to deteriorate as a result of functional limitations and death in China.
Strengths and limitations
This study had several strengths. First, we objectively measured grip strength and walking speed for defining physical frailty. Second, this is the first study reporting estimates about the relationship of both those 2 conditions and associated cross-sectional design could not be used to establish causal relationships or temporality. Second, participants who didn’t respond to our study or were unable to complete the physical tests due to bad physical conditions were excluded from our analyses. We could speculate that those older people might be more frail, especially those deemed malnourished and/or physically frail. Thus, such selection bias might have led to an underestimation of the association between malnutrition and physical frailty in our study. Third, because our participants were recruited from nursing homes only in one city in China, cautious should be exercised to generalize our findings to other populations.
Conclusion
In conclusion, the present study demonstrated that poor nutritional status and physical frailty were highly prevalent in nursing home older adults in China, and that poor nutritional status was associated with increased odds of physical frailty. Our findings suggest that nutrition interventions might be useful to prevent or reverse physical frailty among nursing home elderly people.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. The Lancet. 2013;381(9868): 752–762.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3): M146–156.
Xue QL. The Frailty Syndrome: Definition and Natural History. Clin. Geriatr. Med. 2011;27(1): 1–6.
Kojima G. Prevalence of frailty in nursing homes: a systematic review and metaanalysis. J. Am. Med. Dir. Assoc. 2015;16(11): 940–945.
Vella Azzopardi R, Beyer I, Vermeiren S, Petrovic M, Van Den Noortgate N, Bautmans I, et al. Increasing use of cognitive measures in the operational definition of frailty-a systematic review. Ageing Res Rev. 2018;43: 10–16.
Spira D, Buchmann, Nikolaus K, Maximilian R, Adrian ST, Elisabeth, et al. Sexspecific differences in the association of vitamin D with low lean mass and frailty: results from the Berlin Aging Study II. Nutrition (Burbank, Los Angeles County, Calif.). 2018;62: 1–6.
Wang Y, Wang YJ, Zhan JK, Tang ZY, Huang W, Tan P, et al. Vitamin D binding protein affects the correlation of 25(OH)D and frailty in the older men. Int. J. Endocrinol. 2014;2014: 1–6.
Wei K, Nyunt M, Gao Q, Wee S, Ng Tze-Pin. Frailty and malnutrition: related and distinct syndrome prevalence and association among community-dwelling older adults: Singapore longitudinal ageing studies. J. Am. Med. Dir. Assoc. 2017;18(12): 1019–1028.
Verlaan S, Ligthart M, Gerdien C, Wijers S, Cederholm T, Maier A, et al. High prevalence of physical frailty among community-dwelling malnourished older adults-a systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2017;18(5): 374–382.
Margetts B.M, Thompson R.L, Elia M, Jackson A.A. Prevalence of risk of undernutrition is associated with poor health status in older people in the UK. Eur. J. Clin. Nutr. 2003;57(1): 69–74.
Harris D, N. Haboubi. Malnutrition screening in the elderly population. J. R. Soc. Med. 2005;98(9): 411–414.
Chu L.W, I. Chi. Nursing homes in China. J. Am. Med. Dir. Assoc. 2008;9(4): 237–243.
Zhang H. Sending parents to nursing homes is unfilial? An exploratory study on institutional elder care in China. Int. Soc. Work. 2019;62(1): 351–362.
Narazaki K, Matsuo E, Honda T, Nofuju Y, Yonemoto K, Kumagai S. Physical fitness measures as potential markers of low cognitive function in Japanese communitydwelling older adults without apparent cognitive problems. J. Sports Sci. Med. 2014;13(3): 590–596.
Auyeung T.W, Lee J.S.W, Leung J, Kwok T, Woo J. The selection of a screening test for frailty indentification in community-dwelling older adults. J Nutr Health Aging. 2014;18(2): 199–203.
Wu C.Y, Su T.P, Fang C.L, Yeh Chang M. Sleep quality among community-dwelling elderly people and its demographic, mental, and physical correlates. J. Chin. Med. Assoc. 2012;75(2): 75–80.
Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the Mini Nutrition Assessment as part of the geriatric evaluation. Nutr. Rev. 1996;54(1): s59–65.
Kaiser M.J, Bauer J.M, Ramsch C, Uter, W, Guigoz Y, Cederholm T, et al. Validation of the Mini Nutritional Assessment short-form (MNA®-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9): 782–788.
Li H, Jia J, Yang Z, Moreau N. Mini-Mental State Examination in elderly Chinese: a population-based normative study. J. Alzheimer’s Dis. 2016;53(2): 487–496.
Nyunt M.S, Fone C, Niti M, Ng T.P. Criterion-based validity and reliability of the Geriatric Depression Screening Scale (GDS-15) in a large validation sample of community-living Asian older adults. Aging Ment. Health. 2009;13(3): 376–382.
Katz S, Down T.D, Cash H.R, Grotz R.C. Progress in the development of the index of ADL. The Gerontologist. 1970;10(2): 20–30.
Verbrugghe M, Beeckman D, Van Hecke A, Vanderwee K, Van Herck K, Clays E, et al. Malnutrition and associated factors in nursing home residents: a cross-sectional, multi-centre study. Clin. Nutr. 2013;32(3): 438–443.
Gonzalez-Vaca J, Rica-Escuin M, Silva-Iglesias M, Arjonilla-Garcia M, Varela-Perez R, Oliver-Carbonell J, et al. Frailty in institutionalized older adults from ALbacete. The FINAL Study: rationale, design, methodology, prevalence and attributes. Maturitas. 2014;77(1): 78–84.
Wu C, Smit E, Xue L, Odden, C. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China Health and Retirement Longitudinal Study. J Gerontol A Biol Sci Med Sci. 2018;73(1): 102–108.
Yu J, G Ma, X Jiang. Impact of the built environment and care services within rural nursing homes in China on quality of life for elderly residents. Engineering, Construction and Architectural Management. 2017;24(6): 1170–1183.
Shum M.H, Lou V.W, He K.Z, Chen C.C, Wang J. The “leap forward” in nursing home development in urban China: future policy directions. J. Am. Med. Dir. Assoc. 2015;16(9): 784–789.
Kamo T, Takayama K, Ishii H, Suzuki K, Eguchi K, Nishida Y. Coexisting severe frailty and malnutrition predict mortality among the oldest old in nursing homes: a 1-year prospective study. Arch. Gerontol. Geriatr. 2017;70: 99–104.
Wei K, Nyunt M.S.Z, Gao Q, Wee S.L, Yap K.B, Ng T.P. Association of frailty and malnutrition with long-term functional and mortality outcomes among communitydwelling older adults results from the Singapore longitudinal aging study 1. Jama Network Open. 2018;1(3): 1–13.
Boulos C, P. Salameh, P. Barberger-Gateau. Malnutrition and frailty in community dwelling older adults living in a rural setting. Clin. Nutr. 2016;35(1): 138–143.
Laur C.V, Mcnicholl T, Valaitis R, Keller H.H. Malnutrition or frailty? Overlap and evidence gaps in the diagnosis and treatment of frailty and malnutrition. Appl Physiol Nutr Metab. 2017;42(5): 449–458.
Jeejeebhoy K.N. Malnutrition, fatigue, frailty, vulnerability, sarcopenia and cachexia: overlap of clinical features. Curr. Opin. Clin. Nutr. Metab. Care. 2012;15(3): 213–219.
Landi F, Calvani R, Tosato M, Martone A.M, Ortolani E, Savera G, et al. Anorexia of aging: risk factors, consequences, and potential treatments. Nutrients. 2016;8(2): 1–10.
Landi F, Cherubini A, Cesari M, Calvani R, Tosato M, Sisto A, et al. Sarcopenia and frailty: from theoretical approach into clinical practice. Eur. Geriatr. Med. 2016;7(3): 197–200.
Bonnefoy M, Berrut G, Lesourd B, Ferry M, Gilbert T, Guerin O, et al. Frailty and nutrition: searching for evidence. J Nutr Health Aging. 2015;19(3): 250–257.
Morley J.E. Cognition and nutrition. Curr. Opin. Clin. Nutr. Metab. Care. 2014;17(1): 1–4.
Dominguez L.J, M. Barbagallo. The relevance of nutrition for the concept of cognitive frailty. Curr. Opin. Clin. Nutr. Metab. Care. 2017;20(1): 61–68.
Yannakoulia M, Ntanasi E, Anastasiou C.A, Scarmeas N. Frailty and nutrition: from epidemiological and clinical evidence to potential mechanisms. Metabolism. 2017;6864–76.
Chang H.Y, Fang H.L, Ting T.T, Liang J, Chuang S.Y, Hsu C.C, et al. The co-occurrence of frailty (accumulation of functional deficits) and depressive symptoms, and its effect on mortality in older adults: a longitudinal study. Clin. Interv. Aging. 2019;14: 1671–1680.
Acknowledgement
The author thanks the people who participated in data collection and data entry, as well as the nursing home administrators and residents for their valuable support and participation.
Funding
Funding sources: This study was supported by the Graduate Innovation Project, Central South University (Grant 2018zzts245).
Author information
Authors and Affiliations
Contributions
Authors’ contributions: LWW was involved in the conception and design, acquisition of data, analysis, and interpretation of data, drafting and revising manuscript; CSM carried out design, analysis, and interpretation of data, and revising manuscript; JF participated in the design, acquisition of data and revising manuscript; ZCY was involved in the design, acquisition of data and revising manuscript; TSY contributed to the design, planning, coordination, and revision of manuscript. The final manuscript had been read and approved by all authors.
Corresponding authors
Ethics declarations
Ethical standards: This study obtained ethical approval from the Institutional Review Board of behavioral and nursing research in School of Nursing of Central South University (2019008).
Rights and permissions
About this article
Cite this article
Liu, W., Chen, S., Jiang, F. et al. Malnutrition and Physical Frailty among Nursing Home Residents: A Cross-Sectional Study in China. J Nutr Health Aging 24, 500–506 (2020). https://doi.org/10.1007/s12603-020-1348-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-020-1348-x