Abstract
Objective
To determine normative values for weight-bearing, countermovement leg extension (“jump”) tests in the oldest men and characteristics of those not completing vs. completing tests
Design
2014-16 cross-sectional exam.
Setting
Six U.S. sites from the Osteoporotic Fractures in Men (MrOS) Study.
Participants
Community-dwelling men (N=1,841) aged 84.5±4.2 (range: 77-101) years.
Interventions
N/A.
Measurements
Jump tests on a force plate measured lower-extremity muscle peak power/kg, velocity and force/kg at peak power, with normative values for 5-year age groups and by limitations in moderate-intensity activities of daily living (ADLs) and climbing several flights of stairs.
Results
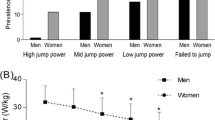
Jump completion was 68.9% (N=1,268/1,841) and 98% (1,242/1,268) had >1 analyzable trial/participant. Exclusions primarily were due to poor mobility and/or balance: 24.8% (456/1,841) prior to and 6.4% (N=117/1,841) after attempting testing. Peak power was 20.8±5.3 W/kg, with 1.2±0.3 m/s for velocity, and 16.7±1.9 N/kg for force at peak power. Each 5-year age group >80 years had subsequently 10% lower power/kg, with 30% lower power/kg at >90 vs. <80 years (all p<0.05). Velocity and force/kg at peak power were 24% and 9% lower respectively, at >90 vs. <80 years (all p<0.05). Limitations in both moderate ADLs and climbing several flights of stairs were associated with 16% lower age-adjusted power/kg, equivalent to 5–10 years of aging, with 11% and 6% lower age-adjusted velocity and force/ kg respectively, vs. those without limitation (all p<0.05). Men not completing vs. completing jumps had older age, higher BMI, lower physical activity, more comorbidities, worse cognition, more IADLs/ADLs and more falls in the past year (all p<0.05). Post-jump pain occurred in 4.6% (58/1,268), with 2 participants stopping testing due to pain. Only 24/1,242 (2%) had all trials/participant without flight (i.e., inability to lift feet), with 323/1,242 having ≥1 trial/participant without flight (total of 28%). No serious adverse safety events (e.g., injury) occurred.
Conclusions
A multicenter cohort of oldest men with a range of function had higher declines in jump power/kg and velocity vs. force/kg across each 5-year age group >80 years. Future research should examine age- and functional-related declines in jump measures related to physical performance decline, falls, fractures, and disability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower-extremity muscle power (force*velocity) may be a differential or independent determinant of physical function and falls compared to traditional lower-extremity muscle strength (1-4) and predicts mortality independently of strength and muscle mass (5). Similar to strength declines, lower muscle power is associated with comorbid conditions of old age (6). Growing evidence has indicated that a more marked age-related power decline compared to strength decline exists (7-11). Population studies often measure isometric strength (maximum isometric force), which is a component in recent sarcopenia definitions (12). Age-related strength declines have been found to be three times greater than muscle mass declines, implying that muscle function loss occurs prior to mass loss and is not fully explained by decreased muscle mass (13, 14). Therefore, while characterization of muscle power loss may be important in predicting future functional decline in old age, age-related decline has not been well described for the “oldest old”, aged >80 years, and normative values from large studies are not available.
Typical muscle power tests assess isolated single/multijoint muscle groups independently of an individual’s function, often using non-weight bearing seated positions in which a participant pushes against a fixed load (e.g., power rig) or as a % of 1 repetition maximum (1RM) (6). Weight-bearing muscle power tests have previously used repeated chair stands, which do not allow the maximum body acceleration throughout the entire push-off phase due to voluntary deceleration of the movement (e.g. by antagonist muscle contraction). Countermovement jumps are weight-bearing tests assessing muscle power ballistically, separating its components into velocity and force at peak power, and allowing absolute maximum power to be generated, which may more closely approximate functional abilities related to daily living. Since older adults with poor function are at higher risk of disability, falls and fall injuries (15-18), “functional power” may be a more appropriate muscle function predictor.
Although jump protocols have been developed for older adults using force plates, past studies did not include older adults unable to lift the feet off the ground or normative values for the oldest ages (11, 19-26). Additionally, our novel protocol allowed power to be calculated without flight (i.e. inability to jump), which may enable lower functioning older adults to be measured compared to previous jump test protocols. The objective of the study was to determine: 1) normative values for muscle power and its force and velocity components from weight-bearing countermovement jump tests in a large multicenter study of community-dwelling men aged 77–101 years with a range of function, and 2) characteristics of those not completing vs. completing tests. We hypothesized that the jump tests would provide normative ranges by age and functional level for the oldest old men, those able to complete testing would have fewer chronic conditions and better physical function, and that men with older ages and poorer self-reported function would have lower jump power, force and velocity.
Methods
Participants
The Osteoporotic Fractures in Men (MrOS) Study is a longitudinal cohort initially designed to evaluate risk factors for osteoporosis and fractures in ambulatory men aged >65 years. Baseline visits occurred between March 2000 and April 2002 at six U.S. sites (N=5,994; aged 73.7±5.9 years) (27). Eligibility criteria included ability to walk without assistance or walking aid; provide self-reported data and informed consent as approved by the site-specific institutional review board; residence near a clinical site; and absence of bilateral hip replacement or severe diseases/conditions. Of 5,994 men, 3,570 did not have a follow-up visit in 2014–16 (2,822 deaths, 386 prior terminations, 362 refusals) when the jump test was implemented. Of those with 2014–16 visit, 1,841/2,424 (75.9%) were included and 583/2,424 (24.1%) with only questionnaires were excluded, as these participants did not have eligibility assessed for in-person measures or attend the clinic visit.
Force plate equipment and software
The Advanced Mechanical Technology Inc. (AMTI) AccuPower force plate (Netforce Acquisition Software Version 3.05.01 with Accugait RS-232 setting and Biosoft Analysis software version 2.3.0) collected force signals at a 1000 Hz sampling rate.
Jump test
Exclusions were due to health-related issues (unable to walk or stand either with or without an aid, self-reported severe pain, or in the past 6 months: spinal surgery, lower extremity surgery, knee or hip replacement) or other safety and/or logistical reasons (e.g., examiner deemed test unsafe, unable to perform without orthotics, shortened visit). Further exclusions included inability or refusal to perform tests, failure to understand instructions, or severe pain. Three calf rise trials were completed as a warm-up prior to a practice jump. Three countermovement jumps (4–5 maximum, if >1/3 had data quality/technical problems) on the force plate were performed. Instructions were to jump as quickly and as high as possible without pausing between bending the knees, land smoothly, stand up straight and remain still. Clinical examiners were trained to identify safety issues and data quality/technical issues. Pain (scale of 0–10, “0”=none to “10”=severe pain) and location of pain were reported, with testing stopped for severe pain.
Jump test data processing
Force plate data were transferred to the University of Pittsburgh Reading Center and reviewed with the Southern Denmark University Processing Center (SDUPC). Valid trials were batch analyzed by SDUPC with custom-designed MatLab software (19-22). Briefly, the vertical velocity of the body center of mass was obtained by time integration of the instantaneous acceleration. Power (P) was calculated continuously as the product of force (F) times velocity (v): P=F*v as previously described (19, 20). Body weight per trial, determined from the force plate during the most stable 200 ms prior to movement, was used to standardize peak power and force at peak power by body weight. Data outside of valid pre-specified ranges, extreme SD outliers, and jumps without flight time were individually reviewed. Either the trial with highest jump height, or highest peak power if all jump trials/participant were without flight, was selected for analysis. Analytic variables from selected trials were: peak concentric power (Watts/kg body weight), velocity (m/s) at peak power, and force (Newton/kg body weight) at peak power.
Quality control and reproducibility
Sites performed weekly calibration of the force plates, with the first several months of data reviewed to verify proper operation of the plates. In comparison to the expert review (PC, ESS, MEW) and evaluation of the first 50 participants at each site, clinic examiners identified 94% of safety (spotter stabilization during the test, failure to maintain stability after landing), data quality (i.e., movement prior to the test, such as trunk/lower body swaying, and/or pausing substantially between starting movement and before jumping) and technical problems (lacking 1–2 seconds of data prior to movement, jump not during the recording time, excessive external plate vibration during recording, incorrect plate/software settings, unrecorded/ unsaved trials). The intra-person jump reproducibility (N=11; N=6 at site 1 and N=5 at site 2) was assessed as a further quality control check. Two sites completed testing twice on the same day with two separate examiners per site (N=3 discordant, N=8 concordant). Signed rank tests, paired t-tests and intraclass correlation coefficients (ICCs) were used for comparing intraperson measures. Two-sided t-test approximations for the Wilcoxon rank sum test were used for coefficients of variation (CVs) within participants. Although not statistically powered as a main finding, the two same-day measures (N=11) of peak power/kg, velocity and force/kg had high ICCs (0.85, 0.92, 0.93, respectively) and low CVs (7.2%, 4.7%, 2.8%, respectively) for intra-person measures.
Descriptive characteristics
Age, race, tobacco use and alcohol consumption (28), hip/ joint pain and any fall in the past year (y/n) were from selfadministered questionnaires. BMI was calculated from balance beam scale weight and Harpenden stadiometer height. Average SBP and DBP were measured with BP Tru automated blood pressure monitor (29). Total hip bone mineral density (BMD) was assessed by DXA (30). Cognitive function was scored using Teng 3MS (31) and executive function was scored with Trails B (32, 33). Total number of medications was calculated from current prescription medications brought to the clinic visit and recorded by staff. Comorbidities included diabetes (selfreported treated by doctor/hypoglycemic use), hypertension (self-reported treated by doctor/antihypertensive use) and selfreported history of congestive heart failure (CHF), myocardial infarction (MI), stroke, Parkinson’s Disease and chronic obstructive pulmonary disease (COPD). Physical activity total energy expenditure was collected from accelerometry (SenseWear armband; N=1,088) (34, 35). Total number of instrumental activites of daily living (IADL) impairments was self-reported and calculated from difficulty (yes/no): 1) walking 2/3 blocks outside on level ground; 2) climbing up 10 steps without rest; 3) preparing meals; 4) doing heavy housework; 5) shopping for groceries/clothes. Self-reported health and activities of daily living (ADL) impairments were measured by the SF-12 questionnaire: 1) excellent/good health for age (vs. fair/poor/very poor); 2) limitations in moderateintensity activities (yes/no); 3) limitations in climbing several flights of stairs (yes/no); 4) limitations in work/activities due to physical health (yes/no); 5) pain interfering with normal work moderately/quite a bit/extremely (vs. none/little). The SF-12 physical health summary scale was scored from physical function questions using norm based methods with regression weighting (36, 37).
Statistical analyses
Normative values for peak power/kg, velocity, and force/ kg were described, including analysis of variance (ANOVA) for means and Wilcoxon ranked-sum test for medians with pairwise comparisons across 5-year (<80, 81–85, 86–90, >90 years) age groups (with 3-year age groups from <80 to >90 years as supplemental analyses), and self-reported limitations for moderate ADLs and climbing several flights of stairs. Skewness <1 and >-1 and kurtosis <2 and >-2 indicated symmetric distributions. Linear regression adjusted for age was used to calculate age-adjusted means by functional limitations. Descriptive statistics by jump trials and by participant were calculated. Descriptive characteristics were compared using two-sided t-tests and Chi-square tests of proportions for those with jump tests and ≥1 analyzable trial (n=1,242) vs. without completion of jump tests (n=573), as well as subgroups without jump tests that were excluded from testing (n=456/573) and attempted but did not complete jump tests (n=117/573). All analyses used SAS version 9.4 (SAS Institute, Cary, NC).
Results
In men aged 77–101 years, completion of the jump test was 68.9% (N=1,268/1,841), with 24.8% (456/1,841) excluded primarily due to poor mobility and/or poor balance. An additional 6.4% (N=117/1,841) that attempted but did not complete jumps were often unable (N=38) or refused (N=5) to perform the practice calf rises due to balance issues. Other exclusions were for severe pain prior to calf rises (N=2) or during practice jumps (N=8), inability to understand calf rise (N=2) or jump instructions (N=2), refusal to attempt a practice jump test (N=34), and unrecorded/unsaved tests (N=26). No serious adverse safety events (e.g., fall or injury) occurred. Post-jump pain was reported in 4.6% (58/1,268), with only 2 participants stopping further testing due to pain. Analyzable trials existed for 98% (1,242/1,268) of participants with tests.
Peak power/kg (20.8±5.3 W/kg), velocity at peak power (1.2±0.3 m/s), and force/kg (16.7±1.9 N/kg) at peak power had normal distributions with wide ranges (Figure 1a-c; Table 1). Normative values for 5-year age groups (Figure 2a-c; Table 1) indicated that overall mean and median values were lower with each increasing age group >80 years. However at older age groups, the range expanded in the lower values but remained fairly consistent in the upper range of values for normal distributions without skewness or issues with kurtosis. Each 5-year age group >80 years had a 10% lower of power/kg, with 30% lower power/kg at >90 years vs. <80 years (all p<0.05; Figure 3). Velocity and force/kg at peak power was 24% and 9% lower at >90 years respectively vs. <80 years (all p<0.05; Figure 3). Results were consistent when 3-year age groups were considered (Appendix Table A), though 90+ years vs. 87–89 years differences for force/kg were not significant.
The overall age-adjusted mean and median values for peak power/kg, velocity and force/kg at peak power were lower with each limitation and lowest for the combined limitations (Table 2). For limitations, the range expanded in the lower range of the values and remained fairly consistent with the upper range of values, with normal distributions and no skewness or issues with kurtosis. Men with both self-reported difficulties in moderate ADLs and climbing several flights of stairs had 16% lower age-adjusted power/kg, a magnitude equivalent to 5–10 years of aging, with a 11% and 6% lower age-adjusted velocity and force/kg, respectively, vs. those without limitations (all p<0.05). Power/kg was 5% lower for limitations only in moderate-intensity ADLs and 11% lower for limitations only in climbing several flights of stairs, with 2% and 8% lower velocity respectively and 2% and 3% lower force/kg respectively (all p<0.05 vs. no limitations).
Participants not completing vs. completing tests were older, had higher BMI, lower physical activity, more hip/joint pain, poorer self-reported health, more comorbidities (diabetes, CHF, MI, stroke, Parkinson’s disease, COPD, medication use), worse cognitive and executive function scores, more IADLs and ADLs, and were more likely to fall in the past year (Table 3). No differences in smoking, drinking or BMD existed between any of the groups. Participants excluded from jumps vs. those attempting and not completing tests had lower SBP and DBP, more CHF, worse cognitive function scores, more IADLs and poorer self-reported health; however other characteristics did not differ.
Only 24/1,242 (2%) had all trials/participant without flight. However an additional N=323 had ≥1 trial/participant without flight, for a total of 28% including N=24 with all trials without flight. Of 26/1,268 (2%) with all trials excluded from analyses, technical (N=21) and data processing problems (N=5) existed. Data quality issues (7%=332/4,714) were due to data collection (N=142), technical (N=151), or data processing problems (N=39). Of total trials (range 1–5 trials/participant: mean 3.9+0.9; median=3), 93% (N=4,382/4,714) had good data quality.
Discussion
This study was the first to implement jump tests in a large multicenter cohort of older adults with a range of function and comorbidities and showed substantially lower power and velocity at the oldest ages from the late 70s to 101 years. With increasing 5-year age groups, power and velocity at peak power were 10% and 7% lower respectively with overall lower power of 30% and overall lower velocity of 24% from <80 years to >90 years. While the force at peak power was also lower over these ages, the magnitude was 3 times less. Our findings may imply that the higher disability and loss of physical function at the oldest ages is due to disproportionately higher decreases in functional power and velocity vs. force.
Our protocol in >1,500 community-dwelling men captured a wide range of dynamic, functional peak power as well as velocity and force at peak power. Importantly, we characterized peak power also in participants without flight during the jump test, unlike previous protocols in older adults (11, 19-26, 38). Through custom designed software, peak power was obtained for 98%, including a third of participants having >1 jump without flight. The lower values with wider ranges in the oldest adults and with functional limitation suggested that jump power was able to differentiate within poor functioning individuals, which may not possible for traditional weight-bearing measures (e.g., chair rise). Our future analyses will focus on jump measures predicting objectively measured functional decline, falls, fractures, and disability at the oldest ages.
Muscle power may decline faster with age than strength (7, 8, 11, 20) with power decline potentially affected by age-related diseases and conditions (6). Men with a range of physical function and chronic conditions were able to complete testing, though had overall fewer chronic conditions and better physical function than those excluded or attempting and unable to complete jumps. Our data indicated a 3 times higher decline in power (10% lower with each 5-year age group) vs. the force component of muscle power (3% lower with each 5-year age group) through the oldest ages. Lower mean jump peak power/ kg was found compared to our past studies of older men (19, 21, 39) possibly due to our inclusion of ages to 101 years with more comorbidities and poorer physical function. For example, higher odds of combined mobility issues were noted in Korean older adults that were not able to jump (38) and we included these individuals. Past smaller cross-sectional studies also found lower jump peak power at older ages (11, 19, 39-42) and relationships with lower BMD (43) and sarcopenia (26, 39, 44). Poor strength predicts incident falls (45), lower physical function (13, 46, 47) mobility disability (48) hospitalization (49, 50) and mortality (51, 52). Peak power, though cross sectionally associated with falls and physical function (1-4, 26, 39, 53-57) is not extensively investigated vs. strength as a predictor of future geriatric outcomes.
The lack of flight during a jump test likely captures specific attributes of the power-load relationship due to body movement biomechanics whereas non-weight bearing methods to assess muscle power (e.g., leg press) would not. Assessing muscle power under weight-bearing conditions has two main advantages: 1) the power output not only depends on the muscle group properties but also reflects dynamic postural control ability in addition to other neuromuscular determinants (e.g. timing of joint to joint muscle activation) (58); and 2) muscle power is tested under real-life conditions with higher external loading corresponding to the subject’s body weight, which due to the power-load relationship may be remarkably different compared to the absolute muscle power that the same individual could generate with with lower loading (e.g., leg press test with 30% of 1RM) (59). Therefore, individuals with non-flight jump tests are likely at higher risk for prospective geriatric functional outcomes.
Our study had several additional strengths. Previous studies have not had characterized normative data for the oldest ages and our large sample size aged 77–101 years allowed description of the magnitude of differences in lower power, velocity and force at peak power by 5-year age groups >80 years. Jump trials without flight were common in the oldest adults and our custom designed software allowed analysis of these trials. Our protocol prioritized participant safety through conservative exclusions for poor balance, mobility issues and pain. Correspondingly, only 2 participant tests stopped for pain and no participants experienced a fall or injury related to the jump test. The viability of jump tests in multicenter studies was supported by consistent reproducibility and reliability as in previous single-center studies (22, 23), high examiner competency, and high data quality.
Limitations
Jump tests may not be practical for general clinical care but are likely well suited for specialized clinics (e.g. falls clinic), and clinical trials, in which measuring small changes in functional power over a short period of time in response to treatment or an intervention is desirable. Harnesses may be needed for observational studies to ensure safety for participants with mobility or balance issues. Force plate methodology required extensive data processing with engineering algorithms addressing a variety of patterns and ranges of data, which may not be feasible for many studies. Although force plate costs are similar to other equipment to measure lower-extremity muscle power and strength, currently available commercial software does not include automated data algorithms to analyze jumps without flight, which is needed to efficiently process data for large studies in older adults. Our population was community-dwelling oldest men and largely white; therefore populations with diverse demographic characteristics need to be examined.
Conclusions
The jump test for peak power was able to be implemented in a large multicenter cohort of the oldest old men, with a range of function and lower jump power/kg and velocity vs. force/kg across each 5-year age group >80 years. Future studies should investigate if jump tests predict prospective geriatric outcomes of physical performance decline, falls, fractures, and disability, particularly vs. maximal strength tests.
Disclosure statement: No authors have disclosures.
Ethical standard: This study complies with the current laws of the United States.
Conflicts of interest: None of the authors have disclosures.
Acknowledgments: The authors are grateful for the contributions of Tue Skallgaard (Department of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense, Denmark) for providing engineering expertise for the development of the custom jump analysis software. The preliminary results were presented to the Gerontological Society of America 68th Annual Scientific Meeting, November 21, 2015, Orlando, FL, USA. The Osteoporotic Fractures in Men (MrOS) Research Group: Administrative Center (Oregon Health & Sciences University): E. Orwoll (Principal Investigator), J. Lapidus (co-Investigator), C. Nielson (co-Investigator), L. Marshall (co-Investigator), C. Pedersen (Project Director), M. Abrahamson, Y. Wang, J. Wiedrick, N. Fino, E. Hooker, J. Nava; Coordinating Center (California Pacific Medical Center Research Institute and University of California, San Francisco): S.R. Cummings (Principal Investigator), D.C. Bauer (co-Investigator), D.M. Black (co-Investigator), P.M. Cawthon (co-Investigator), K.L. Stone (co-Investigator), R. Collins (Project Director), B. Black, T. Blackwell, A. Burghardt, L. Concepcion, S. Ewing, S.L. Harrison, L.Y. Lui, S. Majumdar, C. Navy, N. Parimi, S. Patel, K. Peters, A. Schafer, C. Schambach, A. Schwartz, A. Yu; University of Alabama, Birmingham: J. Shikany (Principal Investigator), C. Lewis (co-Investigator), M. Kilgore (co-Investigator), P. Johnson (Project Director), M. Young (Study Coordinator), N. Webb, S. Felder, C. Collier, K. Hardy; University of Minnesota: K. Ensrud (Principal Investigator), H. Fink (co-Investigator), S. Diem (co-Investigator), J. Schousboe (co-Investigator), B. Taylor (co-Investigator), L. Langsetmo (co-Investigator), S. Potter (Project Director), N. Nelson (Clinic Coordinator), P. Van Coevering (Program Director), K. Jacobson, A. Kats, S. Luthi, K. Moen, E. Penland-Miller, T. Vo; Stanford University: M. Stefanick (Principal Investigator), A. Hoffman (co-Investigator), N. Ellsworth, K. Kent; University of Pittsburgh: J. Cauley (Principal Investigator), J. Zmuda (co-Investigator), E. Strotmeyer (co-Investigator), D. Cusick (Project Director), C. Newman, A. Flaugh, S. Happe; University of California, San Diego: E. Barrett-Connor (Principal Investigator), G. Laughlin (co-Investigator), D. Kado (co-Investigator), M.L. Carrion-Petersen (Project Director), P. Miller, M. Stephens, J Smith, L Claravall.
Funding: The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), and NIH Roadmap for Medical Research under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, and UL1 TR000128. Additional support was provided by the Department of Epidemiology, University of Pittsburgh, NIH National Institute on Aging T32-AG000181 (Newman AB), Department of Sports Science and Clinical Biomechanics and the Center for Active and Healthy Ageing, University of Southern Denmark (Caserotti P), and in part, by NIH, National Institute on Aging, Intramural Research Program (Harris TB).
References
Foldvari M, Clark M, Laviolette LC, et al. Association of muscle power with functional status in community-dwelling elderly women. J Gerontol A Biol Sci Med Sci. 2000;55(4):M192–199.
Skelton DA, Kennedy J, Rutherford OM. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing. 2002;31(2):119–125.
Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003;58 (8):728–733.
Suzuki T, Bean JF, Fielding RA. Muscle power of the ankle flexors predicts functional performance in community-dwelling older women. J Am Geriatr Soc. 2001;49(9):1161–1167.
Metter EJ, Talbot LA, Schrager M, Conwit RA. Arm-cranking muscle power and arm isometric muscle strength are independent predictors of all-cause mortality in men. J Appl Physiol. 2004;96(2):814–821.
Strollo S, Caserotti P, Ward RE, Glynn NW, Goodpaster BH, Strotmeyer ES. A review of the relationship between leg power and selected chronic disease in older adults. Review. J Nutr Health Aging. 2015;19(2):240–248.
Skelton DA, Greig CA, Davies JM, Young A. Strength, power and related functional ability of healthy people aged 65–89 years. Age Ageing. 1994;23(5):371–377.
Lauretani F, Russo CR, Bandinelli S, et al. Age-associated changes in skeletal muscles and their effect on mobility: an operational diagnosis of sarcopenia. J Appl Physiol. 2003;95(5):1851–1860.
Jakobi JM, Rice CL. Voluntary muscle activation varies with age and muscle group. J Appl Physiol. 2002;93(2):457–462.
Klass M, Baudry S, Duchateau J. Age-related decline in rate of torque development is accompanied by lower maximal motor unit discharge frequency during fast contractions. J Appl Physiol. 2008;104(3):739–746.
Dietzel R, Gast U, Heine T, Felsenberg D, Armbrecht G. Cross-sectional assessment of neuromuscular function using mechanography in women and men aged 20–85 years. J Musculoskelet Neuronal Interact. 2013;13(3):312–319.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al; European Working Group on Sarcopenia in Older People. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–423.
Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60(3):324–333.
Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the Health, Aging and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–1064.
Ward RE, Leveille SG, Beauchamp MK, et al. Functional performance as a predictor of injurious falls in older adults. J Am Geriatr Soc. 2015;63(2):315–320.
Peeters GM, Jones M, Byles J, Dobson AJ. Long-term consequences of noninjurious and injurious falls on well-being in older women. J Gerontol A Biol Sci Med Sci. 2015;70(12):1519–1525.
Clemson L, Kendig H, Mackenzie L, Browning C. Predictors of injurious falls and fear of falling differ: an 11-year longitudinal study of incident events in older people. J Aging Health. 2015;27(2):239–256.
Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and fall in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–1129.
Caserotti P, Aagaard P, Simonsen EB, Puggaard L. Contraction-specific differences in maximal muscle power during stretch shortening cycle movements in elderly males and females. Eur J Appl Physiol. 2001;84(3):206–212.
Caserotti P, Aagaard P, Larsen JB, Puggard L. Explosive-heavy resistance training in old and very old adults: changes in rapid muscle force, strength and power. Scand J Med Sci Sports. 2008;18(6):773–782.
Caserotti P, Aagaard P, Puggaard L. Changes in power and force generation during coupled concentric-eccentric versus concentric muscle contractions with training and aging. Eur J Appl Physiol. 2008;103(2):151–161.
Holgaard Larson A, Caserotti P, Puggaard L, Aagaard P. Reproducibility and relationship of single-joint strength vs multi-joint strength and power in aging individuals. Scand J Med Sci Sports. 2007;17(1):43–53.
Rittweger J, Schiessl H, Felsenberg D, Runge M. Reproducibility of the jumping mechanography as a test of mechanical power output in physically competent adult and elderly subjects. J Am Geriatr Soc. 2004;52(1):128–131.
De Vito G, Bernardi M, Forte R, Pulejo C, Macaluso A, Figura F. Determinants of maximal instantaneous muscle power in women aged 50–75 years. Eur J Appl Physiol Occup Physiol. 1998;78(1):59–64.
Michaelis I, Kwiet A, Gast U, et al. Decline of specific peak jumping power with age in master runners. J Musculoskelet Neuronal Interact. 2008;8(1):64–70.
Dietzel R, Felsenberg D, Armbrecht G. Mechanography performance tests and their association with sarcopenia, falls and impairment in the activities of daily living -a pilot cross-sectional study in 293 older adults. J Musculoskelet Neuronal Interact. 2015;15(3):249–256.
Orwoll E, Blank JB, Barrett-Connor E, et al. Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. Contemp Clin Trials. 2005;26(5):569–585.
Ewing JA. Detecting alcoholism. The CAGE questionnaire. JAMA. 1984;252(14):1905–1907.
Myers MG, Godwin M, Dawes M, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286.
Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: scientific review. JAMA. 2002;288(15):1889–1897.
Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318.
Reitan RM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955;19(5):393–394.
Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8:271–276.
Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9):S498–504.
Andre D, Pelletier R, Farringdon J, et al. The development of the SenseWear armband, a revolutionary energy assessment device to assess physical activity and lifestyle. BodyMedia, Inc. 2006.
Ware JE, Kosinski M, Keller SD, QualityMetric Inc, New England Medical Center Hospital, Health Assessment Lab. SF-12: how to score the SF-12 physical and mental health summary scales. Lincoln, R.I.; Boston, Mass.: QualityMetric Inc.; Health Assessment Lab; 2002.
Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233.
Hong N, Kim CO, Youm Y, Kim HC, Rhee Y. Low peak jump power is associated with elevated odds of dysmobility syndrome in community-dwelling elderly individuals: the Korean Urban Rural Elderly (KURE) study. [published online March 8, 2018]. Osteoporos Int. DOI: 10.1007/s00198-018-4466-0.
Siglinsky E, Krueger D, Ward RE, et al. Effect of age and sex on jumping mechanography and other measures of muscle mass and function. J Musculoskelet Neuronal Interact. 2015;15(4):301–308.
Buehring B, Krueger D, Binkley N. Jumping mechanography: a potential tool for sarcopenia evaluation in older individuals. J Clin Densitom. 2010;13(3):283–291.
Rantalainen T, Nikander R, Heinonen A, et al. Neuromuscular performance and body mass as indices of bone loading in premenopausal and postmenopausal women. Bone. 2010;46(4):964–969.
Runge M, Rittweger J, Russo CR, Schiessl H, Felsenberg D. Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin Physiol Funct Imaging. 2004;24(6):335–340.
Singh H, Kim D, Kim E, et al. Jump test performance and sarcopenia status in men and women, 55 to 75 years of age. J Geriatr Phys Ther. 2014;37(2):76–82.
Hardcastle SA, Gregson CL, Rittweger J, Crabtree N, Ward K, Tobias JH. Jump power and force have distinct associations with cortical bone parameters: Findings from a population enriched by individuals with high bone mass. J Clin Endocrinol Metab. 2014;99(1):266–275.
Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and fall in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004;52(7):1121–1129.
Ferrucci L, Guralnik JM, Buchner D, et al. Departures from linearity in the relationship between measures of muscular strength and physical performance of the lower extremities: the Women’s Health and Aging Study. J Gerontol A Biol Sci Med Sci. 1997;52(5):M275–285.
Visser M, Deeg DJ, Lips P, Harris TB, Bouter LM. Skeletal muscle mass and muscle strength in relation to lower-extremity performance in older men and women. J Am Geriatr Soc. 2000;48(4):381–386.
Marsh AP, Rejeski WJ, Espeland MA, et al; LIFE Study Investigators. Muscle strength and BMI as predictors of major mobility disability in the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P). J Gerontol A Biol Sci Med Sci. 2011;66(12):1376–1383.
Cawthon PM, Fox KM, Gandra SR, et al; Health, Aging and Body Composition Study. Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? J Am Geriatr Soc. 2009;57(8):1411–1419.
Alley DE, Koster A, Mackey D, et al; Health, Aging and Body Composition Study. Hospitalization and change in body composition and strength in a population-based cohort of older persons. J Am Geriatr Soc. 2010;58(11):2085–2091.
Rantanen T, Harris T, Leveille SG, et al. Muscle strength and body mass index as long-term predictors of mortality in initially healthy men. J Gerontol A Biol Sci Med Sci. 2000;55(3):M168–173.
Newman AB, Kupelian V, Visser M, et al. Strength, but not muscle mass, is associated with mortality in the Health, Aging and Body Composition Study cohort. J Gerontol A Biol Sci Med Sci. 2006;61(1):72–77.
Bean JF, Kiely DK, LaRose S, Alian J, Frontera WR. Is stair climb power a clinically relevant measure of leg power impairments in at-risk older adults? Arch Phys Med Rehabil. 2007;88(5):604–609.
Kuo HK, Leveille SG, Yen CJ, et al. Exploring how peak leg power and usual gait speed are linked to late-life disability: data from the National Health and Nutrition Examination Survey (NHANES), 1999–2002. Am J Phys Med Rehabil. 2006;85(8):650–658.
Cuoco A, Callahan DM, Sayers S, Frontera WR, Bean J, Fielding RA. Impact of muscle power and force on gait speed in disabled older men and women. J Gerontol A Biol Sci Med Sci. 2004;59(11):1200–1206.
Marsh AP, Miller ME, Saikin AM, et al. Lower extremity strength and power are associated with 400-meter walk time in older adults: The InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2006;61(11):1186–93.
Hicks GE, Shardell M, Alley DE, et al. Absolute strength and loss of strength as predictors of mobility decline in older adults: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2012;67(1):66–73.
Edwards MH, Buehring B. Novel approaches to the diagnosis of sarcopenia. J Clin Densitom. 2015;18(4):472–477.
Zbinden-Foncea H, Valenzuela T, Espíldora F, Peñailillo L, Willems PA. Muscular power as a function of load in elderly women. Comput Methods Biomech Biomed Engin. 2014;17(1):92–93.
Buehring B, Krueger D, Fidler E, Gangnon R, Heiderscheit B, Binkley. N. Reproducibility of jumping mechanography and traditional measures of physical and muscle function in older adults. Osteoporos Int. 2015;26(2):819–825.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Strotmeyer, E.S., Winger, M.E., Cauley, J.A. et al. Normative Values of Muscle Power using Force Plate Jump Tests in Men Aged 77–101 Years: The Osteoporotic Fractures in Men (MrOS) Study. J Nutr Health Aging 22, 1167–1175 (2018). https://doi.org/10.1007/s12603-018-1081-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-018-1081-x