Abstract
Summary
Improved approaches to assess functional change over time are needed to optimally reduce fall/fracture risk; jumping mechanography (JM) may be one such methodology. In this study, JM parameters were more reproducible than traditional functional tests. JM may be better able to demonstrate efficacy of interventions to mitigate sarcopenia.
Introduction
Jumping mechanography (JM), a tool using maximal countermovement jumps performed on a force plate, may more reliably assess muscle function than traditional methods. The purpose of this study was to examine JM retest reliability in older adults compared with commonly used muscle and physical function assessments.
Methods
Community-dwelling individuals age ≥70 years performed physical and muscle function assessments including the short physical performance battery (SPPB), grip strength, and JM on multiple occasions over 3 months. JM parameters included body weight-corrected peak power and jump height. Appendicular lean mass was measured by dual energy x-ray (DXA). Mixed effects linear regression models were used to estimate between- and within-person variability summarized as intra-class correlation coefficients (ICC).
Results
Ninety-seven individuals (49 females, 48 males, mean age 80.7 years) participated. All testing was well tolerated; no participant sustained injury. Jump power, height, and grip strength were greater (p < 0.0001) in men than women. Grip strength, jump power, and height had excellent ICCs (0.95, 0.93, and 0.88, respectively); chair rise, SPPB score, and gait speed had lower ICCs (0.81, 0.77, and 0.76, respectively).
Conclusion
In older adults, JM has excellent retest reliability, is stable over time, and can be performed safely. JM retest reliability was comparable to grip strength and possibly better than SPPB and gait speed. JM is a promising tool for muscle function assessment in older adults. Comparison of this approach with traditional assessment tools in longitudinal interventional studies is needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
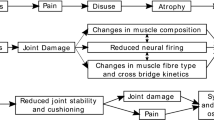
Fragility fracture risk increases dramatically with advancing age, but bone mass does not have a comparable decline [1]. As such, it is apparent that something other than bone loss causes the age-related increase in fracture risk. A major contributor is sarcopenia with resultant impaired physical performance leading to increased falls and hip fracture risk [2]. As such, interest in sarcopenia among the “osteoporosis” field has dramatically increased in recent years.
Sarcopenia was first described as an age-related decline in lean mass that was associated with reduced mobility and independence [3, 4]. Initially, sarcopenia definitions were based solely on muscle mass measurements [5–7]. More recently, it has become clear that physical and muscle function testing and muscle imaging parameters that assess muscle quality, e.g., muscle fat infiltration, better predict outcomes in sarcopenic individuals than lean mass measurement alone [8–15]. Consequently, recent consensus sarcopenia definitions include both muscle mass and function assessment [7, 15–18]. As such, reproducible methods to assess both muscle mass and function are needed.
Numerous techniques exist to assess physical and muscle function [18, 19]. Physical function tests such as gait speed measure overall physical function and are generally characterized by complex movements that require a high degree of coordination of different muscle groups, low intensity (in terms of using maximal muscle force or power), and also rely heavily on other body organs such as the eyes, the vestibular system, or proprioception. In contrast, muscle function tests, e.g., maximal grip strength, focus on single muscle groups or extremities and are of high intensity (power or force). It is possible that tests combining these attributes, i.e., requiring complex and coordinated movements of high intensity, are superior to traditional physical function tests in assessing the effect of sarcopenia interventions on adverse health outcomes such as falls.
These traditional tests include grip strength, gait speed, timed-up and go, chair rise, and the short physical performance battery (SPPB) [9, 20–22], an assessment that combines gait speed, repeated chair rise time, and balance assessment [21, 23–27]. Despite widespread use, these existing functional tests have limitations. For example, some only measure one specific component of muscle function in a particular muscle group, as is the case for grip strength. Others use dichotomous (yes/no) determinations, for example, the tandem stance test. Importantly, many traditional tests, (e.g., chair rise, gait speed, and timed-up and go), include some human subjectivity, potentially contributing error to measurement time. Finally, substantial changes in function are required to detect measured change. The aforementioned factors might decrease test reliability and sensitivity to detect change over time. Availability of highly sensitive and reproducible tools is particularly important for studies that examine potential therapeutic interventions, as more sensitive and reproducible tools can reduce sample size, study duration, and cost, but could also become used in clinical monitoring of an individual patient. Indeed, it is conceivable that medications in development for sarcopenia have failed due to measurement capabilities; specifically, agents that improve muscle mass have not always documented muscle function improvements [28–30]. This observation possibly reflects inability of traditional methods to detect small functional changes.
As such, we, and others, have become interested in using jumping mechanography (JM) as a tool to assess muscle function in populations at risk for muscle impairment and decreased bone strength [31–34]. For the JM evaluation, countermovement jumps are performed on a force platform that calculates jump power and height [27, 31, 33, 35, 36]. JM combines the components of physical and muscle testing by evaluating a high intensity, complex physical task that requires a high degree of muscle force and power and also necessitates the use of other systems (e.g., vestibular, neural, vision) that are required for activities of daily living. While one might be concerned about performing jumping tests in older adults, JM is safely performed, even in very elderly individuals [27, 31, 35]. Existing data suggest that JM has good reproducibility with no significant learning effect over time [35, 37, 38]. However, available studies included healthy adults and only a small number of individuals age 70 years and older. Keeping in mind that performance variance is greater in older adults than in younger adults and that treatment interventions for sarcopenia will require muscle function assessment in older adults, it is important to demonstrate reproducibility and sensitivity to change in this age group. To this end, the purpose of this study was to compare JM reproducibility in older adults with that of other commonly used physical and muscle function tests.
Methods
Participants
Independently living adults age 70 years or older, residing either in the community or retirement facilities, were invited to participate. The study population has been described previously [32]. Briefly, study inclusion criteria required the ability to stand without assistance, absence of clinically significant acute disease, and ability to sign informed consent. Potential participants were excluded if they had sustained a prior fragility fracture and if dual energy x-ray (DXA) measured bone mineral density (BMD) T-score was −3.5 or worse. This study was reviewed and approved by the University of Wisconsin-Madison Institutional Review Board, and was conducted per Federal regulations.
Study design
Potential participants were evaluated at the University of Wisconsin Madison Osteoporosis Clinical Research Center during a screening visit. At that time, following informed consent, BMD measurement and vertebral fracture assessment (VFA) was performed. Volunteers meeting entry criteria noted above underwent muscle/functional testing at the screening visit. They returned for a baseline evaluation 1–3 weeks later (mean 18 days) with subsequent visits 2 weeks and 3 months after baseline.
Physical and muscle function tests
As described above, muscle function tests were conducted at four visits: screening, baseline, 2 weeks, and 3 months post baseline. A window of 2 to 3 weeks was allowed between screening and baseline. Testing included the SPPB as a measure of physical function and JM and grip strength as measures of muscle function. Grip strength was performed at only baseline and 3-month time points as this measure is documented to have high reproducibility [39]. Consequently, acquisition of additional data in this regard was felt to have only limited value. A standardized testing order was followed; JM was always performed first, followed by grip strength, when conducted, then the SPPB. Research study coordinators conducted all tests and read the same scripted instructions to each subject for every test at all visits. One examiner conducted all jump testing and another administered all SPPB and grip strength evaluations.
Subjects performed two-leg countermovement jumps on a Leonardo force platform (Novotec, Pforzheim, Germany). Jumps were recorded and analyzed utilizing Leonardo software version 4.2. Each test session required subjects to perform countermovement jumps as previously described; they were required to complete two successful practice jumps, and the next three technically adequate jumps were recorded [31]. The jump achieving the greatest height from this set of three was used for this study analysis. Specific jump power (W/kg) and maximal jump height (cm) variables are reported.
Components of SPPB were completed in the standard order of chair rise, three tandem balance tests, and a 4-m walk [23]. This test generates a cumulative score based on the performance of the 3 components with a maximum achievable score of 12. For purposes of these data, we utilized total SPPB score and the performance time of the chair rise (seconds) and 4-m gait speed (m/s).
Grip strength was measured using a hand-held dynamometer (Jamar; Bolingbrook, IL) at the baseline and 3-month visits using a previously described technique [39]. Subjects performed the test standing, using the non-dominant hand. Three trials were performed at each exam with subjects resting for 10–20 s between trials. When trial results differed by greater than 3 kg, a fourth trial was obtained and maximal achieved grip strength (kg) was used for analyses.
DXA bone and body composition analysis
Proximal femur, lumbar spine BMD, VFA, and total body composition scans were acquired using a Lunar iDXA densitometer (GE Healthcare, Madison, WI). All scans were acquired and analyzed using enCORE software version 11.0 per manufacturer guidelines. A BMD T-score of ≤−2.5 at the lumbar spine, total femur, or neck was utilized to categorize subjects as osteoporotic. An experienced reader (NB) blinded to subject and time point evaluated all VFA images obtained at screening and 3 months to determine vertebral fracture prevalence and incidence. Lean and fat mass were determined from the total body scans. Specifically, appendicular lean mass (ALM) was calculated by adding the lean mass of the arms and legs and dividing by height squared (arm lean mass [kg] + leg lean mass [kg])/height [m]2). Subjects were classified as sarcopenic or non-sarcopenic by applying the Baumgartner definition to their ALM calculation (females <5.45 and males <7.26 kg/m2) [5].
Statistical analysis
Differences in demographics and functional performance by sex were assessed using Student’s t test. Repeat measures ANOVA examined the change in muscle function for each test and gender over time, i.e., over the four study visits. Microsoft Excel (Seattle WA), JMP, and SAS (Cary, NC, USA) were used for these calculations. Method variance for each test was evaluated by standard deviation and least significant change (LSC). LSC, calculated in routine manner (root mean square SD with 95 % confidence), accounts for test error and represents the minimum longitudinal difference that must occur with each test to document a physical change.
Mixed effects linear regression models were used to estimate between- and within-subject variance parameters for each functional performance outcome. All models included all follow-up visits; additional models also adjusted for sex and body mass index (BMI). Measurement reproducibility was summarized using the intra-class correlation coefficient (ICC). ICCs evaluate the reproducibility of observed measures relative to the variation in true measures between subjects in the population under study. Within a study/population, ICCs facilitate direct comparisons of reproducibility of different muscle function tests by automatically adjusting for the different measurement scales. Confidence intervals were obtained using the bootstrap. All analyses were performed in R version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Demographic data
Average age of the 49 women and 48 men in this trial was 80.7 (range 70–95) years. Group mean BMI was 25.6 kg/m2, 24.7 % were classified as osteoporotic per WHO definition, 22.7 % had prevalent vertebral fracture, and 23.7 % were classified as sarcopenic using the Baumgartner definition. No differences between men or women were observed except men were taller and more women were osteoporotic (mean height 172.7 vs. 160.8 cm; 36.7 vs. 12.5 %, p < 0.05, Table 1). No adverse events related to the functional tests were reported, and no new or incident vertebral fractures were identified on the 3-month VFA.
Physical and muscle function testing
The repeated JM trials at each study visit did not demonstrate a pattern of decline or improvement in performance, suggesting that multiple trials did not cause fatigue or provide “practice” to improve performance (data not shown). Mean jump power and height were 20.0 W/kg and 17.8 cm, respectively; mean grip strength was 25.3 kg. Men generated higher (p < 0.0001) mean measurements than women for jump power 22.5 vs. 17.6 W/kg, jump height 20.5 vs. 15.3 cm, and grip strength 32.4 vs. 18.3 kg. Mean SPPB was 10.1, repeated chair rise 14.0 s, and gait speed 1.08 m/s with no difference in performance by sex. These data are detailed in Table 1.
No clear change in muscle function was observed over time (Table 2). No changes were observed for any test in the male cohort. In contrast, statistically significant differences were present in the female cohort; however, there was no consistent functional change pattern in that chair rise time improved while grip strength and jump height decreased. No clear pattern was seen in SPPB scores (Table 2).
Method variance for each test expressed by standard deviation and LSC is presented in Table 3. LSC values of the different tests varied greatly. This variation was related to the size of the test mean values (see Table 1), i.e., larger mean values were associated with larger LSCs.
All trial visits for each test were utilized to calculate ICC values and all were adjusted for study visit. Grip strength and jump power demonstrated the best reproducibility with ICCs of 0.95 and 0.93, respectively (Table 4). Total SPPB score and 4-m gait speed were the least reproducible with ICCs of 0.77 and 0.76, respectively. Adjustment for visit, sex, and BMI lowered ICCs for jump height, jump power, and grip strength, primarily due to the large sex differences in these parameters. Nonetheless, jump power and grip strength still demonstrated the best reproducibility with ICCs of 0.90 and 0.87, respectively.
Discussion
The development of pharmacologic and non-pharmacologic approaches to mitigate sarcopenia and thereby reduce falls and fracture risk necessitates sensitive and reproducible testing methodologies. The data reported here demonstrate that JM is a highly reproducible and stable functional test over time. JM reproducibility is similar to grip strength, an isometric exercise that evaluates only one muscle group. However, JM requires coordinated activity and safely evaluates an individual’s maximal effort; as such, it may have advantages over traditional muscle/functional tests in older adults. Indeed, JM is a strength measurement that also incorporates the functional components assessed in traditional chair rise and gait speed testing. Considering the low injury risk of JM, it may prove to be a safe, and potentially more sensitive method of evaluating maximal effort in those with functional limitations. Additionally, recent data show that JM is also correlated to pQCT measured cortical bone strength, a finding which further highlights the potential usefulness in those at risk for fracture [34].
In contrast to the high reproducibility found for JM, these data also reinforce the limited ability of SPPB and 4-m gait speed to detect small changes. The high variance and relatively low ICC of these tests may be due to the inclusion of human variability in obtaining the measurements; a confounder minimized by the computerized data acquisition of JM.
Our results are similar to those published by Rittweger et al. [35] who concluded that JM and maximal gait speed performed better than timed get up and go, free gait speed, and chair rise tests. In that study, the gait speed tests were 10 m at full walking speed as distance was added before and after the walking course to remove potential effects of acceleration and deceleration. Consequently, these studies evaluated somewhat different functional tests. Additionally, the Rittweger study evaluated only a small number (n = 58) over a wide age range (19 to 88 years); inclusion of young adults likely increased inter-individual variability of all the functional tests. For example, the range of weight-corrected jump power was 8–65 W/kg, whereas the range was 10–32 W/kg in this cohort. Similarly, Matheson et al. [38] examined JM intra- and inter-rater reproducibility in ten young adults and reported ICCs in the same range as this study. As such, this study finds similar reproducibility over time in older adults as that previously reported in younger cohorts.
Developing optimal tests to monitor sarcopenia interventions are sorely needed to adequately evaluate pharmacological therapies in phase 3 trials and ultimately bring such agents to clinical care [28, 29, 40, 41]. Such testing methods should be reproducible, stable over time (i.e., no learning effect), and sensitive surrogates that predict adverse outcomes of this disease, such as falls and fractures. In this regard, measurement of muscle mass, e.g., DXA lean mass, have good reproducibility, but do not predict clinical outcomes as well as muscle function tests [10, 13]. Although muscle function tests appear valid, there is concern about reproducibility in older adults. The data reported here (ICCs, LSCs) are likely to provide appropriate estimates of reproducibility variables because they focused on an older population at risk. An additional strength of this study is that several measurements (not only two) were obtained over a time period of a few months. This approach likely produced a more robust estimate of the true reproducibility of these physical and muscle function tests. One might argue that in an elderly population such as studied here, a biologic decline in muscle function could occur over 3 months. However, no clear change was observed in this community-dwelling cohort. Additionally, ICCs were also calculated based on only the first three visits and although the absolute measurements changed, the differences between the muscle function tests remained similar (data not shown). As such, true biological change seems unlikely to be confounding these results.
Limitations of this work include a relatively well-functioning older adult cohort as demonstrated by less than 25 % of the sample meeting ALM/height2 diagnostic criteria for sarcopenia. Additionally, the applicability of utilizing various surrogates would be improved if these test results were correlated prospectively with outcomes such as falls, fracture, or chronic disease to assess predictive power. Finally, not all traditional functional tests were evaluated, for example, the fastest gait speed, 30-s chair rise, 6-min walk, and timed get up and go were arbitrarily omitted from the study due to concern about reducing reproducibility by causing fatigue.
In conclusion, JM is a highly reproducible test in older ambulatory adults and demonstrates less test variability than some traditional physical functional tests commonly used in clinical and research settings. Additionally, it evaluates a complex, high-intensity movement, thereby combining features of common physical and muscle function tests. As such, JM may well have enhanced capability to detect change due to interventions, potentially making this a valuable research tool. Further studies are indicated to evaluate whether the ability of JM to measure small increments over a wide range of performance may make it more sensitive to intervention-induced changes in function and to correlate JM parameters with hard outcomes such as falls and fractures.
References
Kelly TL, Wilson KE, Heymsfield SB (2009) Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS One 4:e7038
Cawthon PM, Fullman RL, Marshall L, Mackey DC, Fink HA, Cauley JA, Cummings SR, Orwoll ES, Ensrud KE (2008) Physical performance and risk of hip fractures in older men. J Bone Miner Res 23:1037–1044
Rosenberg IH (1989) Epidemiologic and methodologic problems in determining nutritional status of older persons. (Summary comments). Am J Clin Nutr 50:1231–1233
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990S–991S
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Janssen I, Baumgartner RN, Ross R, Rosenberg IH, Roubenoff R (2004) Skeletal muscle cutpoints associated with elevated physical disability risk in older men and women. Am J Epidemiol 159:413–421
Correa-de-Araujo R, Hadley E (2014) Skeletal muscle function deficit: a new terminology to embrace the evolving concepts of sarcopenia and age-related muscle dysfunction. J Gerontol A Biol Sci Med Sci 69:591–594
Koster A, Ding J, Stenholm S et al (2011) Does the amount of fat mass predict age-related loss of lean mass, muscle strength, and muscle quality in older adults? J Gerontol A Biol Sci Med Sci 66:888–895
Lang T, Cauley JA, Tylavsky F, Bauer D, Cummings S, Harris TB (2010) Computed tomographic measurements of thigh muscle cross-sectional area and attenuation coefficient predict hip fracture: the health, aging, and body composition study. J Bone Miner Res 25:513–519
Visser M, Goodpaster BH, Kritchevsky SB, Newman AB, Nevitt M, Rubin SM, Simonsick EM, Harris TB (2005) Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci 60:324–333
Hairi NN, Cumming RG, Naganathan V, Handelsman DJ, Le Couteur DG, Creasey H, Waite LM, Seibel MJ, Sambrook PN (2010) Loss of muscle strength, mass (sarcopenia), and quality (specific force) and its relationship with functional limitations and physical disability: The Concord health and ageing in men project. J Am Geriatr Soc 58:2055–2062
Cawthon PM, Fox KM, Gandra SR et al (2009) Do muscle mass, muscle density, strength, and physical function similarly influence risk of hospitalization in older adults? J Am Geriatr Soc 57:1411–1419
Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB (2006) Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci 61:72–77
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558
Dam TT, Peters KW, Fragala M et al (2014) An evidence-based comparison of operational criteria for the presence of sarcopenia. J Gerontol A Biol Sci Med Sci 69:584–590
Muscaritoli M, Anker SD, Argiles J et al (2010) Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 29:154–159
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Mijnarends DM, Meijers JM, Halfens RJ, ter Borg S, Luiking YC, Verlaan S, Schoberer D, Cruz Jentoft AJ, van Loon LJ, Schols JM (2013) Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc 14:170–178
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB (1995) Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 332:556–561
Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S, Berkman LF, Wallace RB (2000) Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 55:M221–M231
Miller DK, Wolinsky FD, Andresen EM, Malmstrom TK, Miller JP (2008) Adverse outcomes and correlates of change in the short physical performance battery over 36 months in the African American health project. J Gerontol A Biol Sci Med Sci 63A:487–494
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49:M85–M94
Dixon WG, Lunt M, Pye SR, Reeve J, Felsenberg D, Silman AJ, O’Neill TW (2005) Low grip strength is associated with bone mineral density and vertebral fracture in women. Rheumatology (Oxford) 44:642–646
Rantanen T, Guralnik JM, Foley D, Masaki K, Leveille S, Curb JD, White L (1999) Midlife hand grip strength as a predictor of old age disability. J Am Med Assoc 281:558–560
Coppin AK, Ferrucci L, Lauretani F, Phillips C, Chang M, Bandinelli S, Guralnik JM (2006) Low socioeconomic status and disability in old age: evidence from the InChianti study for the mediating role of physiological impairments. J Gerontol A Biol Sci Med Sci 61:86–91
Runge M, Rittweger J, Russo CR, Schiessl H, Felsenberg D (2004) Is muscle power output a key factor in the age-related decline in physical performance? A comparison of muscle cross section, chair-rising test and jumping power. Clin Physiol Funct Imaging 24:335–340
Buehring B, Binkley N (2013) Myostatin—the holy grail for muscle, bone, and fat? Curr Osteoporos Rep 11:407–414
Rolland Y, Onder G, Morley JE, Gillette-Guyonet S, Abellan van Kan G, Vellas B (2011) Current and future pharmacologic treatment of sarcopenia. Clin Geriatr Med 27:423–447
Dalton JT, Taylor RP, Mohler ML, Steiner MS (2013) Selective androgen receptor modulators for the prevention and treatment of muscle wasting associated with cancer. Curr Opin Support Palliat Care 7:345–351
Buehring B, Krueger D, Binkley N (2010) Jumping mechanography: a potential tool for sarcopenia evaluation in older individuals. J Clin Densitom 13:283–291
Buehring B, Hind J, Fidler E, Krueger D, Binkley N, Robbins J (2013) Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc 61:418–422
Russo CR, Lauretani F, Bandinelli S, Bartali B, Cavazzini C, Guralnik JM, Ferrucci L (2003) High-frequency vibration training increases muscle power in postmenopausal women. Arch Phys Med Rehabil 84:1854–1857
Hardcastle SA, Gregson CL, Rittweger J, Crabtree N, Ward K, Tobias JH (2014) Jump power and force have distinct associations with cortical bone parameters: findings from a population enriched by individuals with high bone mass. J Clin Endocrinol Metab 99:266–275
Rittweger J, Schiessl H, Felsenberg D, Runge M (2004) Reproducibility of the jumping mechanography as a test of mechanical power output in physically competent adult and elderly subjects. J Am Geriatr Soc 52:128–131
Michaelis I, Kwiet A, Gast U, Boshof A, Antvorskov T, Jung T, Rittweger J, Felsenberg D (2008) Decline of specific peak jumping power with age in master runners. J Musculoskelet Neuronal Interact 8:64–70
Veilleux LN, Rauch F (2010) Reproducibility of jumping mechanography in healthy children and adults. J Musculoskelet Neuronal Interact 10:256–266
Matheson LA, Duffy S, Maroof A, Gibbons R, Duffy C, Roth J (2013) Intra- and inter-rater reliability of jumping mechanography muscle function assessments. J Musculoskelet Neuronal Interact 13:480–486
Wadsworth CT, Krishnan R, Sear M, Harrold J, Nielsen DH (1987) Intrarater reliability of manual muscle testing and hand-held dynametric muscle testing. Phys Ther 67:1342–1347
Chumlea WC, Cesari M, Evans WJ, Ferrucci L, Fielding RA, Pahor M, Studenski S, Vellas B, Members IWGoSTF (2011) Sarcopenia: designing phase IIB trials. J Nutr Health Aging 15:450–455
Abellan van Kan G, Cameron Chumlea W, Gillette-Guyonet S, Houles M, Dupuy C, Rolland Y, Vellas B (2011) Clinical trials on sarcopenia: methodological issues regarding phase 3 trials. Clin Geriatr Med 27:471–482
Acknowledgments
All authors contributed to the study concept and design, acquisition of subjects and data, analysis and interpretation of data, and preparation of manuscript. This work was sponsored by an investigator initiated research grant from Merck & Co., Inc. Merck & Co., Inc and did not have any role in the design, methods, subject recruitment, data collection, analysis, or preparation of paper. Dr. Buehring receives research funding from the John A. Hartford Foundation as a Centers of Excellence in Geriatric Medicine and Geriatric Psychiatry scholar. Dr. Binkley is participating in a multicenter trial with Lilly in functional outcomes in older adults. He also consults on the same project.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buehring, B., Krueger, D., Fidler, E. et al. Reproducibility of jumping mechanography and traditional measures of physical and muscle function in older adults. Osteoporos Int 26, 819–825 (2015). https://doi.org/10.1007/s00198-014-2983-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2983-z