Abstract
Objectives
To assess the relationship between physical frailty and subsequent decline in global cognitive function in the non-demented elderly.
Design and setting
A prospective population-based study in a west Japanese suburban town, with two-year follow-up.
Participants
Community-dwellers aged 65 and older without placement in long-term care, and not having a history of dementia, Parkinson’s disease and depression at baseline, who participated in the cohort of the Sasaguri Genkimon Study and underwent follow-up assessments two years later (N = 1,045).
Measurements
Global cognitive function was assessed using the Montreal Cognitive Assessment (MoCA). Physical frailty was identified according to the following five components: weight loss, low grip strength, exhaustion, slow gait speed and low physical activities. Linear regression models were used to examine associations between baseline frailty status and the MoCA scores at follow-up. Logistic regression models were used to estimate the risk of cognitive decline (defined as at least two points decrease of MoCA score) according to baseline frailty status.
Results
Seven hundred and eight non-demented older adults were included in the final analyses (mean age: 72.6 ± 5.5 years, male 40.3%); 5.8% were frail, and 40.8% were prefrail at baseline. One hundred and fifty nine (22.5%) participants experienced cognitive decline over two years. After adjustment for baseline MoCA scores and all confounders, being frail at baseline was significantly associated with a decline of 1.48 points (95% confidence interval [CI], -2.37 to -0.59) in MoCA scores, as compared with non-frailty. Frail persons were over two times more likely to experience cognitive decline (adjusted odds ratio 2.28; 95% CI, 1.02 to 5.08), compared to non-frail persons.
Conclusion
Physical frailty is associated with longitudinal decline in global cognitive function in the non-demented older adults over a period of two years. Physically frail older community-dwellers should be closely monitored for cognitive decline that can be sensitively captured by using the MoCA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The co-occurrence of physical frailty and late-life cognitive decline are triggering increasing attentions (1, 2). Physical frailty refers to a medical syndrome of decreased reserve and diminished resistance to stressors and relates to elevated risk of adverse health outcomes (3–5). The biological model of physical frailty comprises five components: unintentional weight loss, low grip strength, exhaustion, low gait speed, and low physical activity (4). A number of previous studies have demonstrated that physical frailty is associated with increased risk of incident dementia (6–8), Alzheimer’s disease (9), mild cognitive impairment (10), and cognitive impairment in older adults (11). However, to date, evidence suggesting the associations between physical frailty and decline in global cognitive function amongst non-demented subjects is limited, and the results are conflicting (11–17). Although cross-sectional studies has consistently observed poorer global cognitive performance in pre-frail and frail persons than the non-frail among non-demented older subjects (12, 13), findings from longitudinal studies are inconsistent. Some longitudinal studies reported that physical frailty, in the absence of dementia at baseline, is associated with increased risk of global cognitive decline (11, 16, 17), whereas other studies showed no significant association between physical frailty and cognitive decline at follow-up (14, 15).
Furthermore, most previous studies that investigated the relationships between physical frailty and cognitive decline have assessed global cognitive function using the Mini-Mental State Examination (MMSE) (11, 15–18), which is reported to be insensitive to subtle cognitive changes, as compared with the Montreal Cognitive Assessment (MoCA), another brief and valid cognitive test for global cognition (19, 20). Practically, individuals without functional impairment in activity of daily living would be better assessed by the MoCA as first cognitive screening, rather than the MMSE (21). Also, existing researches that investigated association between physical frailty and global cognitive decline are mostly limited by various assessments used to operationalize original definition of physical frailty.
Therefore, the purpose of this study was to examine the association of baseline physical frailty status with cognitive decline over time in older adults initially free of dementia. Accordingly, we used the MoCA to assess global cognition, rather than the MMSE, in a functionally independent community-dwelling older population. Data were drawn from the Sasaguri Genkimon Study (SGS) in which operational definition of physical frailty has been previously validated by using comprehensive physical assessments that were close to the original definition developed by Fried and colleagues (4, 22). Based on our prior work on cross-sectional relationship between global cognitive performance and physical frailty (22), we hypothesized that being frail, but not pre-frailty, at baseline, is associated with decline in global cognitive performance over two years.
Methods
Study Population
The data were drawn from the SGS, a longitudinal study in a suburban community-dwelling Japanese older population. The cohort were recruited from the Sasaguri town of Fukuoka Prefecture. A detailed description of the study design and recruitment methods of the SGS has been reported previously (23, 24). Briefly, there were 31,606 inhabitants in the Sasaguri town, and 5,636 were aged 65 years and older at the time of baseline survey in 2011. Of those, 4,979 older inhabitants who were not identified by the national long-term care insurance system as needing long-term care were considered meeting the inclusion criteria of this cohort. Two waves of data were collected in May to August of 2011 and 2013 and were used in the present study.
Initially, 1,060 participants completed measurements at both baseline and follow-up. Of those, 1,045 participants who were free of dementia, Parkinson’s disease, and depression at baseline were included in the present study. Presence of dementia, Parkinson’s disease, and depression was defined according to self-reported medical history of having ever been diagnosed by physicians. We excluded 337 subjects without complete data for baseline physical frailty and other covariates, and assessment of global cognitive function at follow up. The final sample consisted of 708 subjects eligible for analysis. The original survey protocols were approved by the Institutional Review Board of Institute of Health Science, Kyushu University, and written informed consent was obtained from all participants.
Physical Frailty Measures
Physical frailty was identified according to the five physical frailty components proposed and validated by Fried and colleagues (4): weight loss, low grip strength, exhaustion, slow gait speed and low physical activities. Participants who presented three or more affected components were considered being frail; one to two affected components as being pre-frail; and 0 affected component as non-frail. Accordingly, the cut-off points of low grip strength, slow gait speed and low physical activities were operationalized using the population-based lowest quintile approach, in which participants who scored in the lowest quintile in a given component were classified as being affected in that component. Presence of weight loss was identified with self-reported unintentional weight lost more than 2 to 3 kg in the previous 6 months (25). Low grip strength (kg) was measured using a handhold dynamometer (GRIP-D, T.K.K. 5401, Takei Scientific Instruments Co. Ltd., Niigata, Japan), adjusted for gender and body mass index (kg/m2). Exhaustion was indicated by a positive answer to either or both of two questions: “Did you feel that everything you did was an effort?” and “Did you feel exhausted without any reason?” in the last one month. Low gait speed was identified with gender- and standing height- stratified time (sec) over 5-meter walking test at one’s maximum walking speed. Low physical activity (kcal/kg/day) was objectively assessed using a tri-axial accelerometer (Active Style Pro, HJA350-IT, Omron Healthcare, Inc., Kyoto, Japan). The lowest quintile cut-off points were adjusted for weight and stratified by gender for this low physical activity component. The procedure of this operational definition in SGS has already been completed and reported to have satisfactory internal validity (23).
Cognitive Measures
Global cognitive function was defined based on the Japanese version of MoCA. The Japanese version of the MoCA has been cross-culturally adapted and validated in Japanese population (26). A detailed description of the testing process in the SGS can be found elsewhere (24). The total score of the MoCA is 30 points, with lower scores indicating poorer global cognitive performance when being treated as a continuous measure. As previously validated by Nasreddine and colleagues (27), global cognitive decline was defined as a decrease of at least two points in MoCA scores between baseline and follow-up assessment, which is considered possibly reflecting a true deterioration in global cognition (14, 28).
Other variables
Data on baseline sociodemographic characteristics including number of years of education, living condition (“living alone or not”), smoking (“current smoker or not”), and drinking (“current drinker or not”) were collected using questionnaires. Information on age and gender were obtained from the municipality office. Falls were evaluated with one self-reported question of having falls in the past one year. Responses included “yes/no”. Polypharmacy was defined as taking four or more medications by a question asking the current number of prescription medicine. Self-reported medical history of having ever been diagnosed with chronic diseases including hypertension, heart disease, stroke, diabetes, minor trauma fracture, chronic pulmonary disease, digestive disease, chronic kidney disease, osteoarthritis or rheumatism, ear trouble, eye trouble, and cancer were also recorded.
Statistical analysis
Descriptive characteristics were summarized as means and standard deviations (SD) or median and interquartile range (IQR) for continuous variables where appropriate, and percentages for categorical variables. Trends of baseline characteristics across frailty status were tested using the Jonckheere-Terpstra trend test for continuous variables, and the Cochran-Armitage test for categorical variables. The unadjusted means (standard error, SE) of follow-up MoCA scores and least squares means (SE) adjusted for baseline MoCA score were computed according to baseline frailty status using analysis of variance and analysis of covariance, respectively, with multiple comparisons of mean differences between frailty status groups conducted based on Bonferroni correction.
To examine the association between baseline physical frailty and the MoCA scores at follow-up, we conducted multiple linear regression models where follow-up MoCA performance was regressed on baseline frailty status, controlling for baseline MoCA scores and other potential confounders. Of note, in those linear regression models we did not use the difference score (follow-up MoCA score – baseline MoCA score) as the dependent variable, because analyzing difference score does not control for baseline imbalance due to regression to the mean (29). Also, we expected that baseline MoCA scores have an actual causal effect on follow-up MoCA scores. In this case, the model using the "levels" (with each model including follow-up MoCA score as the dependent variable and the baseline MoCA score as a covariate) is preferable to the model using difference scores as the dependent variable (30).
All the multivariate models were adjusted for age, gender, years of education, and the covariates for which p value was < 0.2 in bivariate analysis: living alone, current drinker, falls in the past year, polypharmacy, and number of chronic diseases.
Furthermore, logistic regression models were used to estimate the risk for developing cognitive decline by baseline frailty status, with adjustment for those potential confounders listed above, as well as baseline MoCA scores. In subsequent analyses, we tested whether any confounders modified all the associations by individually introducing the interaction term of each confounder with physical frailty.
Finally, we conducted a sensitivity analysis of excluding participants with a history of stroke or MMSE score < 18 points, as those conditions could potentially indicate possible dementias at baseline (4). All the analyses were done using SAS version 9.3 (SAS Institute Inc., Cary, N.C., USA). Significance level was set at α = 0.05.
Results
As compared with the final sample of 708 participants, participants excluded from the initial sample were older, more likely to be men and frail, and had poorer global cognitive function and a higher rate of falls in the past one year at baseline than those included in the analysis. There were no significant differences between those excluded and included participants in other characteristics including education, rates of living alone, currently smoker and drinker, polypharmacy, and presence of chronic diseases. Comparisons of characteristics between the excluded and the included participants were made and shown in the Supplemental Table 1.
In our study population, 40.3% were men. The average age were 72.6 ± 5.5 years old at baseline. Of those, 5.8% were physically frail, and 40.8% were pre-frail. Baseline characteristics of the study sample according to baseline frailty severity were presented in Table 1. Among the three frailty status groups, frail participants was the oldest, and had the least education, the lowest baseline MoCA scores, the greatest number of chronic diseases, the lowest rate of current drinker, the highest rates of living alone, having falls in the past year, polypharmacy, and presence of medical history of hypertension, digestive disease, osteoarthritis or rheumatism, and minor trauma fracture (all p for trend < 0.05). One hundred and fifty nine (22.5%) participants experienced cognitive decline.
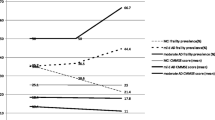
Figure 1 displays the unadjusted and adjusted mean and SE of follow-up MoCA scores, according to baseline frailty status. Frail participants had significantly lower mean scores on MoCA at follow-up than pre-frail and non-frail participants. Pre-frail participants had significantly lower mean scores on MoCA at follow-up than non-frail participants. The significance did not alter after adjustment for baseline MoCA scores. Table 2 shows the results of multivariate linear regression models. After full adjustment for baseline MoCA scores and all confounders, being frail at baseline, but not pre-frailty, was significantly associated with a decline in MoCA score (beta = -1.48; 95% confidence interval [CI], -2.37 to -0.59), as compared to nonfrailty.
Logistic regression analyses for the associations of baseline frailty status with cognitive decline were shown in Table 3. Compared with being non-frail, being physical frail was associated with an increased risk of experiencing cognitive decline, with an adjusted odds ratio (OR) of 2.28 (95% CI, 1.02 to 5.08). There was no significant association between pre-frailty and cognitive decline. The significance of those associations did not vary with the confounders, since none of interaction terms for physical frailty status and any confounder were significant. Associations remained significant after exclusion of participants with stroke or MMSE score < 18 points (n = 24) from the analyses did not alter the results (results not shown).
Discussion
This study demonstrated that physical frailty was associated with cognitive decline over a two-year period in non-demented community-dwelling older adults. These findings were observed using both a continuous measure and a categorical measure of cognitive changes as assessed using the MoCA. The results of multivariate linear regression models showed that being physically frail was significantly associated with poorer global cognitive function at follow-up, independent of baseline cognitive function. As compared with non-frail persons, frail persons experienced a statistically significant decrease of 1.48 points in MoCA scores at follow-up after full adjustment for covariates. Although the estimate was slightly smaller, a recent study reported a decrease of 1.8 points in MoCA scores over 3.5 years as clinically meaningful worse in cognitive function (31). Therefore, we may postulate that the observed difference between frail persons and non-frail counterparts over a two-year period reaches potentially clinical significance. The results of logistic regression models showed that being physical frail posed a higher risk of cognitive decline than non-frailty as well. The significant associations were robust in that they were independent of baseline cognitive status and presence of common chronic diseases, and no significant interaction were observed between physical frailty and any confounder. Further analyses that excluded participants with possible dementia yielded similar results. Unlike previous studies focusing on incidence of dementia, mild cognitive decline, or clinical cognitive impairment in frail subpopulations, this study addressed longitudinal decline in global cognitive function amongst non-demented older adults in relation to baseline frailty severity, suggesting that physical frailty may be an important predictor for cognitive decline that can be sensitively detected by using the MoCA.
Most of previous longitudinal studies, with follow-up period ranging from one to ten years, showed that frail older persons had significantly greater global cognitive decline as evaluated using MMSE or composite cognition measures, than non-frail older adults (9, 11, 17, 18). Our findings extend these prior findings by providing evidence that physical frailty was associated with an increased risk of cognitive decline as assessed using the MoCA. Inconsistently, a recent five-year longitudinal study of 252 non-demented older adults, which assessed global cognition using the MoCA, failed to show significant association between physical frailty and cognitive decline, which was potentially attributed to the small sample size (14).
Evidence on the association between physical pre-frailty and cognitive decline are also conflicting in prior studies (11, 12). We found that the intermediate physical frail status, the pre-frailty, was not significantly associated with a higher risk for cognitive decline, as compared with non-frailty. This observation suggests that cognitive function are more likely to be maintained when deficits in physical function are not sufficiently severe to warrant a diagnosis of frailty. Indeed, all older adults experienced cognitive decline, and there are wide individual variabilities in the magnitude and the timing of exhibiting cognitive decline (32). Further studies are necessary to investigate the trajectory of cognitive ability amongst the frail, as well as the pre-frail subpopulations.
To date, the basis for the association between physical frailty and global cognitive decline is still uncertain. The observed association might be attributable to systematic physiologic alterations that occur with aging and/or correlated with common pathological pathways, such as oxidative stress (33), inflammation (34), and hormonal dysregulation (35). Other common risk factors, such as malnutrition and cardiovascular risk, have been used to explain the observed associations between physical frailty and cognitive decline (1). Our results also support a recently proposed clinical entity, “cognitivefrailty”, hypothetically defined as the presence of both physical frailty and cognitive impairment but in the absence of dementia (36). The cognitive-frailty construct notionally defines reduced cognitive reserve related to physical frailty with a potential reversibility of clinical representation. Individuals with cognitive-frailty have been recently reported to have worse cognitive function than individuals with cognitive impairment and without physical frailty (37).
Interpretations of the present findings should be cautious in concluding causality between frailty and global cognitive decline. Practically, physical frailty often occurs in the absence of cognitive decline, and vice versa. Also, it is speculated that physical frailty and cognitive decline are merely two manifestations of common underlying brain pathological damage (1, 38), which was recently supported by the findings of Buchman and colleagues in showing an independent significant association between Alzheimer’s disease pathology, macroinfarcts, and nigral neuronal loss with simultaneous worsening physical frailty and cognition (39). Although the intrinsic mechanisms underlying this link are not fully understood, the present findings raised the possibility that physical frailty may be a useful predictor for cognitive decline in community-dwelling older adults. It will also be of great practical significance to explore shared modifiable risk/ protective factors of physical frailty and cognitive decline towards preventing or ameliorating the progression of both of the two conditions in older adults, since both of them are not irreversible.
This study has several important limitations. Firstly, generalizability of the results is limited because of the nonrepresentative sample, thus our observations need to be confirmed in other populations. Secondly, exclusion of participants from the initial sample may have led to potential selection bias and distorted the association. The exclusion were mainly due to incomplete data on either physical frailty or cognitive tests, or both. As shown in the results of comparisons between those excluded with available data and those included, those excluded participants simultaneously presented severer physical and cognitive deficits at baseline than those included individuals. Thus, the observed association in the final sample would be weakened, and biased toward the null hypothesis. Therefore, the true association may be stronger than that found in this study. Thirdly, the possibility of undiagnosed dementia cannot be ruled out. However, the similar results from sensitivity analysis of excluding possible dementia might, to some extent, increase the robustness of the findings.
Several strengths of this studies increase confidence in the present findings, which include well-characterized cohort of functional community-dwelling older adults without longterm care, the previously validated operational definition of physical frailty in this cohort which was close to original frailty definition (4), and the use of the MoCA test which is sensitive to subtle changes in global cognition (27).
Conclusion
Physical frailty at baseline was associated with a decline in global cognitive function in this non-demented older sample over a period of two years. Physically frail older communitydwellers should be closely monitored for cognitive decline that can be sensitively captured by using the MoCA. Future investigations of common risk/protective modifiable factors of physical frailty and cognitive decline may of great practical significance towards prevention of both physical frailty and cognitive decline.
Acknowledgements: This study was partly supported by the Health and Labour Sciences Research Grant of the Ministry of Health, Labour and Welfare of Japan (2013-Ninchisho-Ippan-004), a research grant from the Mitsui Sumitomo Insurance Welfare Foundation to CSM, and partly funded by a grant from the Sasaguri Town to SK (2011-2016). We would like to thank Dr. Yu Nofuji, Ms. Eri Shiokawa’s, and the municipal staffs in primary care-giving division of Sasaguri town, especially Ms. Gunjima Kumiko, who helped us coordinate the survey in the community. HT is supported by the Japan Society for the Promotion of Science.
Disclosure statement: We have no financial or non-financial competing interests to declare. All the funders had no role in the study design, data analysis, data interpretation, writing of the manuscript or in the decision to submit the manuscript.
References
Robertson DA, Savva GM, Kenny RA. Frailty and cognitive impairment -A review of the evidence and causal mechanisms. Ageing Res Rev. 2013;12(4):840–851.
Shimada H, Makizako H, Doi T, Yoshida D, Tsutsumimoto K, Anan Y, et al. Combined prevalence of frailty and mild cognitive impairment in a population of elderly Japanese people. J Am Med Dir Assoc. 2013;14(7):518–524.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–156.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762.
Solfrizzi V, Scafato E, Frisardi V, Seripa D, Logroscino G, Maggi S, et al. Frailty syndrome and the risk of vascular dementia: the Italian Longitudinal Study on Aging. Alzheimers Dement. 2013;9(2):113–122.
Gray SL, Anderson ML, Hubbard RA, LaCroix A, Crane PK, McCormick W, et al. Frailty and incident dementia. J Gerontol A Biol Sci Med Sci. 2013;68(9):1083–1090.
Avila-Funes JA, Carcaillon L, Helmer C, Carrière I, Ritchie K, Rouaud O, et al. Is frailty a prodromal stage of vascular dementia? Results from the Three-City Study. J Am Geriatr Soc. 2012;60(9):1708–1712.
Buchman A, Boyle PA, Wilson RS, Tang Y, Bennett DA. Frailty is associated with incident Alzheimer’s disease and cognitive decline in the elderly. Psychosom Med. 2007;69(5):483–489.
Boyle PA, Buchman AS, Wilson RS, Leurgans SE, Bennett DA. Physical frailty is associated with incident mild cognitive impairment in community-based older persons. J Am Geriatr Soc. 2010;58(2):248–255.
Samper-Ternent R, Al Snih S, Raji MA, Markides KS, Ottenbacher KJ. Relationship between frailty and cognitive decline in older Mexican Americans. J Am Geriatr Soc. 2008;56(10):1845–1852.
Robertson DA, Savva GM, Coen RF, Kenny RA. Cognitive function in the prefrailty and frailty syndrome. J Am Geriatr Soc. 2014;62(11):2118–2124.
Wu Y, Liu L, Chen W. Cognitive function in individuals with physical frailty but without dementia or cognitive complaints: results from the I-Lan Longitudinal Aging Study. J Am Med Dir Assoc. 2015;16(10):899.e9-16.
Montero-Odasso MM, Barnes B, Speechley M, Muir SW, Doherty TJ, Duque G, et al. Disentangling cognitive-frailty: results from the Gait and Brain Study. J Gerontol A Biol Sci Med Sci. 2016;71(11):1476–1482.
Dramé M, Novella J-L, Jolly D, Lanièce I, Somme D, Heitz D, et al. Rapid cognitive decline, one-year institutional admission and one-year mortality: analysis of the ability to predict and inter-tool agreement of four validated clinical frailty indexes in the SAFEs cohort. J Nutr Health Aging. 2011;15(8):699–705.
Auyeung TW, Lee JSW, Kwok T, Woo J. Physical frailty predicts future cognitive decline -a four-year prospective study in 2737 cognitively normal older adults. J Nutr Health Aging. 2011;15(8):690–694.
Mitnitski A, Fallah N, Rockwood MRH, Rockwood K. Transitions in cognitive status in relation to frailty in older adults: a comparison of three frailty measures. J Nutr Health Aging. 2011;15(10):863–867.
Alencar MA, Dias JMD, Figueiredo LC, Dias RC. Frailty and cognitive impairment among community-dwelling elderly. Arq Neuropsiquiatr. 2013;71(6):362–367.
Dong Y, Sharma VK, Chan BP, Venketasubramanian N, Teoh HL, Seet RC, et al. The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci. 2010;299(1-2):15–18.
Haley GE, Berteau-Pavy F, Berteau-Pavy D, Raber J. Novel image-novel location object recognition task sensitive to age-related cognitive decline in nondemented elderly. Age (Dordr). 2012;34(1):1–10.
Julayanont P, Phillips N, Chertkow H, Nasreddine ZS. The Montreal Cognitive Assessment (MoCA): concept and clinical review. In: Larner AJ, editor. Cognitive Screening Instruments: A Practical Approach. Berlin: Springer-Verlag; 2013. pp 111–152.
Chen S, Honda T, Narazaki K, Chen T, Nofuji Y, Kumagai S. Global cognitive performance and frailty in non-demented community-dwelling older adults: Findings from the Sasaguri Genkimon Study. Geriatr Gerontol Int. 2016;16(6):729–736.
Chen S, Honda T, Chen T, Narazaki K, Haeuchi Y, Supartini A, et al. Screening for frailty phenotype with objectively-measured physical activity in a west Japanese suburban community: evidence from the Sasaguri Genkimon Study. BMC Geriatr. 2015;15:36.
Narazaki K, Nofuji Y, Honda T, Matsuo E, Yonemoto K, Kumagai S. Normative data for the montreal cognitive assessment in a Japanese community-dwelling older population. Neuroepidemiology. 2013;40(1):23–29.
Fukutomi E, Okumiya K, Wada T, Sakamoto R, Ishimoto Y, Kimura Y, et al. Importance of cognitive assessment as part of the “Kihon Checklist” developed by the Japanese Ministry of Health, Labor and Welfare for prediction of frailty at a 2-year follow up. Geriatr Gerontol Int. 2013;13(3):654–662.
Fujiwara Y, Suzuki H, Yasunaga M, Sugiyama M, Ijuin M, Sakuma N, et al. Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr Gerontol Int. 2010;10(3):225–232.
Julayanont P, Brousseau M, Chertkow H, Phillips N, Nasreddine ZS. Montreal Cognitive Assessment Memory Index Score (MoCA-MIS) as a predictor of conversion from mild cognitive impairment to Alzheimer’s disease. J Am Geriatr Soc. 2014;62(4):679–684.
Suzuki H, Kawai H, Hirano H, Yoshida H, Ihara K, Kim H, et al. One-year change in the Japanese version of the Montreal Cognitive Assessment performance and related predictors in community-dwelling older adults. J Am Geriatr Soc. 2015;63(9):1874–1879.
Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow-up measurements. BMJ. 2001;323(7321):1123–1124.
Allison P. Change scores as dependent variables in regression analysis. Sociol Methodol. 1990;20:93–114.
Krishnan K, Rossetti H, Hynan LS, Carter K, Falkowski J, Lacritz L, et al. Changes in Montreal Cognitive Assessment scores over time. Assessment. 2016 Jun 18. Doi: 10.1177/1073191116654217. (Epub ahead of print)
Hayden KM, Reed BR, Manly JJ, Tommet D, Pietrzak RH, Chelune GJ, et al. Cognitive decline in the elderly: an analysis of population heterogeneity. Age Ageing. 2011;40(6):684–689.
Mulero J, Zafrilla P, Martinez-Cacha A. Oxidative stress, frailty and cognitive decline. J Nutr Health Aging. 2011;15(9):756–760.
Panza F, Solfrizzi V, Frisardi V, Maggi S. Different models of frailty in predementia and dementia syndromes. J Nutr Health Aging. 2011;15(8):711–720.
Maggio M, Dall’ Aglio E, Lauretani F, Cattabiani C, Ceresini G, Caffarra P, et al. The hormonal pathway to cognitive impairment in older men. J Nutr Health Aging. 2012;16(1):40–54.
Kelaiditi E, Cesari M, Canevelli M, Van Kan G, Ousset PJ, Gillette-Guyonnet S, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) International Consensus Group. J Nutr Heal Aging. 2013;17(9):726–734.
Delrieu J, Andrieu S, Pahor M, Cantet C, Cesari M, Ousset PJ, et al. Neuropsychological profile of “cognitive frailty” subjects in MAPT Study. J Prev Alzheimers Dis. 2016;3(3):151–159.
Shatenstein B. Frailty and cognitive decline: links, mechanisms and future directions. J Nutr Health Aging. 2011;15(8):665–666.
Buchman AS, Yu L, Wilson RS, Boyle PA, Schneider JA, Bennett DA. Brain pathology contributes to simultaneous change in physical frailty and cognition in old age. J Gerontol A Biol Sci Med Sci. 2014;69(12):1536–1544.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Supplemental table 1:
Comparisons between the excluded and included sample in this study
Rights and permissions
About this article
Cite this article
Chen, S., Honda, T., Narazaki, K. et al. Physical Frailty is Associated with Longitudinal Decline in Global Cognitive Function in Non-Demented Older Adults: A Prospective Study. J Nutr Health Aging 22, 82–88 (2018). https://doi.org/10.1007/s12603-017-0924-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0924-1