Abstract
The Montreal Cognitive Assessment (MoCA) is a cognitive screening instrument developed to detect mild cognitive impairment (MCI). It is a simple 10 minute paper and pencil test that assesses multiple cognitive domains including memory, language, executive functions, visuospatial skills, calculation, abstraction, attention, concentration, and orientation. Its validity has been established to detect mild cognitive impairment in patients with Alzheimer’s disease and other pathologies in cognitively impaired subjects who scored in the normal range on the MMSE. MoCA’s sensitivity and specificity to detect subjects with MCI due to Alzheimer’s disease and distinguish them from healthy controls are excellent. MoCA is also sensitive to detect cognitive impairment in cerebrovascular disease and Parkinson’s disease, Huntington’s disease, brain tumors, systemic lupus erythematosus, substance use disorders, idiopathic rapid eye movement sleep behaviour disorder, obstructive sleep apnoea, risk of falling, rehabilitation outcome, and epilepsy. There are several features in MoCA’s design that likely explain its superior sensitivity for detecting MCI. The MoCA’s memory testing involves more words, fewer learning trials, and a longer delay before recall than the MMSE. Executive functions, higher-level language abilities, and complex visuospatial processing can also be mildly impaired in MCI participants of various etiologies and are assessed by the MoCA with more numerous and demanding tasks than the MMSE. MoCA was developed in a memory clinic setting and normed in a highly educated population. Norms in lesser educated, community based, multi-cultural samples will hopefully be available to help first line healthcare providers better assess subjects presenting with cognitive complaints. The MoCA is freely accessible for clinical and educational purposes (www.mocatest.org), and is available in 36 languages and dialects.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Montreal Cognitive Assessment (MoCA)
- Alzheimer’s disease
- Mild cognitive impairment
- Vascular cognitive impairment
- Dementia
6.1 Introduction
The Montreal Cognitive Assessment (MoCA) was developed as a brief screening instrument to detect Mild Cognitive Impairment [1]. It is a paper-and-pencil tool that requires approximately 10 minutes to administer, and is scored out of 30 points. The MoCA assesses multiple cognitive domains including attention, concentration, executive functions, memory, language, visuospatial skills, abstraction, calculation and orientation. It is widely used around the world and is translated to 36 languages and dialects. The test and instructions are freely available on the MoCA official website at www.mocatest.org. No permission is required for clinical or educational use.
This chapter will describe how each MoCA sub-test/domain, assesses various neuro-anatomical areas, and often overlapping cognitive functions. A comprehensive review of studies using the MoCA in multiple clinical settings and populations is provided. An algorithm for using the MoCA in clinical practice is suggested. In conclusion, MoCA limitations, future research and developments are discussed.
6.2 Cognitive Domains Assessed by the MoCA
6.2.1 Visuospatial/Executive
6.2.1.1 Modified Trail Making Test
Beside visuomotor and visuoperceptual skills, the trail making test–B (TMT-B) requires mental flexibility to shift between numbers and letters which mainly rely on frontal lobe function [2–5]. In functional Magnetic Resonance Imaging (fMRI) studies, shifting ability in the TMT-B revealed greater activation relative to the trail making test A in the left dorsolateral and medial frontal cortices, right inferior and middle frontal cortices, right precentral gyrus, left angular and middle temporal gyri, and bilateral intraparietal sulci [6–8]. A study of patients with frontal and non-frontal lobe lesions reported that all patients who had more than one error in the TMT-B had frontal lobe lesions. Specifically, patients with damage in the dorsolateral frontal area were mostly impaired [9]. Left frontal damage tended to cause more impairment than controls and right frontal damage groups, either for execution time or number of errors [10]. Nonetheless, specificity of the TMT-B to frontal lobe lesions is debated as one study reported comparable performance between frontal and non-frontal stroke patients [11].
6.2.1.2 Copy of the Cube
To copy a cube, subjects have to initially convert a two-dimensional contour to a three-dimensional cube. This ability is enhanced by learning experiences [12, 13]. After spatial planning, visuomotor coordination also plays a role in copying the cube. Various brain areas are involved; visual perception in the parieto-occipital lobe, planning in the frontal lobe, and integration of visual and fine motor sequences in the fronto-parieto-occipital cortices.
The cognitive mechanisms underlying performance in copying a figure are different according to the underlying disease. Alzheimer’s disease (AD) patients with spatial perception/attention impairment had significant atrophy in the right parietal cortex. Complex two-dimensional figure copy was negatively associated with degree of right inferior temporal atrophy and reduction of cerebral blood flow in the right parietal cortex [14, 15]. Patients with behavioral variant fronto-temporal dementia with spatial planning and working memory dysfunction had significant atrophy in the right dorsolateral prefrontal cortex [16]. A correlation between neuro-imaging and cube copying specifically has not yet been reported.
Even though a high proportion of either normal subjects (40 %) or Alzheimer patients (76 %) performed poorly on cube drawing on verbal command, persistent failure to copy a cube from a previously drawn cube is highly discriminative to detect patients with Alzheimer’s disease [17]. Less educated, older age, female and depressed subjects performed poorly in drawing-to-command and copying conditions.
6.2.1.3 The Clock Drawing Test
The Clock Drawing Test (CDT) has been widely used and studied for detection of dementia and mild cognitive impairment (see Chap. 5). Planning, conceptualization, and symbolic representation are involved in drawing a clock’s face and in placing all the numbers correctly [18, 19]. Inhibitory response is required when placing each hand to tell the time of “ten past eleven”. Self-initiated-clock-drawing also requires intact visuoconstructive skills which are mainly represented in the parietal lobe.
In volunteers, fMRI demonstrated bilateral activation of the posterior parietal cortex and the dorsal premotor area during task performance suggesting the contribution of the parieto-frontal cortical networks to integrate visuospatial elements and motor control in self-initiated clock drawing [20].
In AD patients, errors in CDT were mainly conceptual and due to semantic memory impairment [21–23]. This was supported by various neuroimaging studies that found negative correlation between CDT performance and atrophy of the right/left temporal cortices [24, 25], atrophy of the medial temporal lobe [23], reduction in the activation of the left superior parietal lobe [26], and hypometabolism of the right parietal cortex [27] in patients with cognitive impairment caused by AD pathology.
White matter hyperintensities (WMH) are also related to performance on CDT [23]. Patients with severe WMH and patients with Parkinson’s disease (PD) performed poorly and similarly on all subscales of CDT [28]. Even though both groups were different in terms of neuropathology, they both have disrupted subcortico-frontal pathways. PD affects the subcortical dopaminergic pathway projecting to the prefrontal cortex [28, 29].
The scoring criteria for the CDT in the MoCA have been simplified to decrease scoring complexity, scoring time, and minimize inter rater variability.
Despite the simpler scoring instructions, suboptimal inter and intra-rater reliability for MoCA’s CDT were recently reported [30]. CDT may be influenced by literacy status and education level [21, 31, 32].
6.2.2 Naming
The three animals in the MoCA (Lion, Rhinoceros and Camel) are infrequently seen in Western and even in Asian countries. The failure to name these animals may point to various types of cognitive impairment. If subjects cannot name but can give contextual information about the animal, for example, “It lives in the desert (Camel)”, this could suggest either word finding difficulty or semantic memory impairment. If subjects cannot tell both the name and the context, they may have impaired visuoperceptual skills with inability to recognize the animal (failure in the cube copy and the CDT can support this possibility). They may also be impaired in both visuoperception and semantic memory such as in moderate to severe AD or advanced PD with dementia. Low education or cultural exposition to such animals can also be responsible.
In AD, impairment tends to reflect a breakdown in semantic processes which is different from visuoperceptual deficits caused by subcortical dementia such as Huntington’s disease (HD) [33, 34]. Some studies have shown that semantic dysfunction is the primary cause of misnaming in both cortical or subcortical dementia [35, 36].
The neuronal network involved in naming is category-dependent [37–41]. In healthy subjects, the commonly activated regions were bilateral occipital lobes including the fusiform gyri, and pars triangularis of the left inferior frontal gyrus [38–40]. This activation pattern may be explained by processing of visual features and shape analysis in the primary visual cortex and fusiform gyri, and the subsequent retrieval process from semantic and conceptual knowledge of animals mediated by the pars triangularis of the left inferior frontal gyrus [40, 42]. Interestingly, animal naming was also associated with activation of the frontal regions linked to the limbic emotional system, namely the left supplementary motor area and the anterior cingulate gyrus [38, 39]. It has also been shown that animal naming is more associated with primary visual cortex activation than naming of tools which is associated with frontal and parietal lobe activation (premotor cortex and postcentral parietal cortex) [38].
6.2.3 Attention
6.2.3.1 The Digit Span
Digit Span Forward (DSF) measures retention of auditory stimuli and articulatory rehearsal. Digit span backward (DSB) requires working memory, and a more demanding ability in transforming digits into a reversed order before articulating. This extra-step requires central executive processing [43].
Neuronal networks involved in digit span processing have been shown in many neuroimaging studies. In healthy subjects, using near-infrared spectroscopy (NIRS) a relationship between activation of the right dorsolateral prefrontal cortex and performance on DSB was observed [44]. Other studies have shown greater activation of the bilateral dorsolateral prefrontal cortices, prefrontal cortex and left occipital visual regions for DSB compared to DSF [43–46]. These findings confirm the need for executive function to complete the DSB task. Activation of the visual cortex during DSB supports the hypothesis that visuospatial processing may be involved during mental reversal imaging of digit sequences [44, 45].
Amnestic Mild Cognitive Impairment (MCI) and AD patients performed poorly on both tasks compared with normal controls [47–49]. PD patients with amnestic MCI had some impairment in DSB, but not DSF [50]. Early impairment of executive function caused by subcortico-frontal dopaminergic dysfunction explains the isolated poor performance on DSB among PD patients. At the cutoff <3 digits, the sensitivity and specificity of DSB in detection of major cognitive disorders (including dementia, delirium and cognitive impairment not otherwise specified) are 77 and 78 %, respectively [51]. With the same cutoff, DSB can detect 81 % of the delirium patients, however, with false positive rate of 37 % [51]. Moreover, impaired digit span in elderly subjects with subjective memory complaints is a predictor for the conversion from subjective memory complaints to mild cognitive impairment [52].
6.2.3.2 Concentration and Calculation: Letter A Tapping Test
In this test the subject listens and taps when the letter A is read out among a series of other letters. Concentration, which is defined as sustained and focused attention, is the primary function required for proper identification of the letter A and inhibition of inappropriate non-letter A tapping. It has good sensitivity to detect cognitive impairment in mild traumatic brain injury and persistent post-concussion syndrome [53, 54]. Speed of response to externally-paced stimuli accounts for this test’s sensitivity [54]. This task has not been well studied in neurodegenerative diseases. In the MoCA validation study, MCI subjects and Normal Controls had comparable normal performance, however, AD subjects were significantly more impaired on this task [1].
6.2.3.3 Concentration and Calculation: Serial 7 Subtractions
Calculation is an essential part of everyday social and living activities. In normal subjects, bilateral parietal and prefrontal cortices have been reported to be consistently activated during mental calculation, along with left inferior frontal lobe and angular gyrus activation [55–59]. Some studies suggest that the linguistic representation and visuospatial imagery also play a role in mental calculation [56, 60]. Specific to serial 7 subtraction, fMRI studies have reported similar greater activation in the bilateral premotor, the posterior parietal and the prefrontal cortices when normal participants performed this task compared with the control condition [61]. The prefrontal cortex activation is associated with working memory which is required to maintain the previous answer in a loop for further subtractions.
In AD patients, a reduction of fMRI activation or PET glucose metabolism in the inferior parietal cortex was observed during mental calculation [55, 62]. Some studies also reported a reduction in activation in the bilateral lateral prefrontal cortices [55], and the left inferior temporal gyrus [62]. These hypofunctional areas are the same as the ones reported being significantly activated in normal subjects.
6.2.4 Language
6.2.4.1 Sentence Repetition
Sentence repetition assesses language skills which are supported by left temporo-parieto-frontal circuit. Repeating complex sentences also requires attention and concentration to memorize the words which are supported by working memory systems in the frontal lobes [63]. AD patients had lower scores on this task compared with normal subjects [1, 63, 64]. Education also plays a role in sentence repetition, and interpretation of the results should take into consideration subjects’ education level [65].
6.2.4.2 Letter F Fluency
Verbal fluency is divided into phonemic (letter) and semantic (category) fluency. Letter F fluency in the MoCA mainly depends on frontal lobe function compared with semantic fluency, which is sustained by both temporal and frontal lobes. Letter F fluency requires coordination of lexico-semantic knowledge, shifting from word to word, working memory, searching strategy and inhibition of irrelevant words which all highly depend on frontal lobe function and to a lesser extent the temporal lobe.
Patients with frontal lesions produced fewer words than healthy controls [66–69]. Left frontal lesions play a greater role in letter fluency impairment than right frontal lesions [66, 69, 70]. However, specificity of the frontal lobe dysfunction to letter fluency impairment is still debated as patients with non-frontal left hemisphere lesions also performed worse than patients with right hemisphere frontal and non-frontal lesions [69].
Neuroimaging studies indicate that letter fluency activates a variety of frontal (left dorsolateral prefrontal cortex, left inferior frontal gyrus, supplementary motor area) and non-frontal areas (anterior cingulate cortex, bilateral temporal and parietal lobes) [71–73]. Both lesional and neuroimaging studies suggest high sensitivity of the test, but low specificity, to detect frontal lobe dysfunction [74]. Low specificity may partly depend on education level and literacy status, as this task requires grapheme-phoneme correspondence. Lower educated and illiterate subjects generate fewer words than subjects with higher education [75–77]. Since letters do not exist in certain languages, letter fluency was replaced by semantic fluency (animal naming) for languages such as Chinese, Korean, in the MoCA test [78, 79].
As phonemic fluency is highly associated with frontal executive function, pathologies affecting frontal lobe or fronto-subcortical circuits, such as in PD and HD patients, frequently impair this function more than lesions of the temporo-parietal lobe which are associated with storage of lexicosemantic knowledge [50, 80–82]. In contrast, patients with Alzheimer’s pathology will more likely have semantic fluency impairment early in the course of their disease [83]. Patients with depression have also impaired phonemic fluency as a result of probable overall global cognitive slowing [84].
6.2.5 Abstraction
Similarity between objects requires semantic knowledge and conceptual thinking. In right-handed subjects, the left perisylvian glucose metabolism was closely associated with performance on the Wechsler Similarities Test (WST) [59]. On PET imaging, the metabolic reduction in the left temporal lobe and left angular gyrus of Alzheimer’s disease patients correlates with impairment on test for similarities [85]. Frontal executive function and the parieto-temporal semantic knowledge may be involved in this task for more difficult and demanding word pairs [85]. AD and Huntington’s disease patients performed poorly on the WST compared to normal controls. Patients with frontotemporal dementia have more deficits than AD patients in the similarities subtest of the Frontal Assessment Battery when controlled for MMSE level [86]. Moreover, performance decline in the WST is predictive of AD conversion in non-demented participants [87].
6.2.6 Delayed Recall
More words to recall (5 versus 3), less learning trials (2 versus up to 6), and more time between immediate recall and delayed recall (5 versus 2 min) probably explains MoCA’s superior sensitivity for amnestic MCI detection compared to the MMSE. In the first MoCA validation study, MCI patients recalled on average 1.17 words out of 5, while normal controls recalled 3.73 words [1].
Category and multiple choice cues provide useful information to distinguish encoding memory impairment, which does not improve with cueing, from retrieval memory impairment that does improve with cueing.
Retrieval memory impairment may be associated with medial parietal and frontal white matter loss [88], posterior cingulate hypometabolism [89], pathologies affecting subcortical structures [90] and the hippocampo-parieto-frontal network [88]. Retrieval memory deficits are seen in pathologies affecting sub-cortical structures such as Vascular Cognitive Impairment [91, 92], Parkinson’s disease [93], and Huntington’s disease [94, 95]. However, the retrieval deficit hypothesis of PD-related memory impairment has been debated, as some studies have shown that even given cues, PD patients still had impairment in recognition [96, 97]. Retrieval memory deficits can also be seen in depression [98, 99], frontotemporal dementia [100, 101], normal pressure hydrocephalus [102], and HIV cognitive impairment [103, 104].
Encoding memory impairment correlates with hippocampal atrophy and hypometabolism [88, 89, 105]. AD patients typically perform poorly on delayed free recall without improvement after cueing, and also have higher rates of intrusion compared with PD and HD patients [106]. Encoding memory deficits are also seen in Wernicke and Korsakoff syndromes, strategically located ischemic or hemorrhagic strokes or tumors that affect the Papez circuit (hippocampus, fornix, mamillary bodies, thalamus, and cingulate cortex), and post surgical excision of the medial temporal lobes for epilepsy control, as first described in patient HM by Milner [107–109].
6.2.7 Orientation
Impairment in orientation has been shown to be the single best independent predictor of daily functions in patients with dementia, and is also associated with caregiver burden and psychological distress [110, 111]. Temporal orientation yields high sensitivity in detection of dementia and patients with delirium. Errors in identifying the date has the highest sensitivity (95 %), but also lowest specificity (38 %) [112]. Identification of the year or month was suggested to detect cognitively impaired subjects with optimal validity [112]. However, orientation is not a good indicator to detect milder stages of cognitive impairment [1]. Temporal orientation can also predict overall cognitive decline over time [113]. Moreover, patients with temporal disorientation tend to be impaired on verbal memory as well [114]. Orientation to place is not discriminative in milder stages of cognitive impairment and dementia, but may be able to detect very severe cognitive impairment which is also obvious without cognitive screening.
6.3 MoCA Development and Validation
The MoCA (Copyright: Z. Nasreddine M.D.) was developed based on the clinical intuition of one of the authors of the validation study (ZN) regarding domains of impairment commonly encountered in MCI and best adapted to a screening test [1]. An initial version covered ten cognitive domains using rapid, sensitive, and easy-to-administer cognitive tasks. Iterative modification of the MoCA took place over 5 years of clinical use. An initial test version was administered to 46 consecutive patients (mostly diagnosed with MCI or AD) presenting to the Neuro Rive-Sud (NRS) community memory clinic with cognitive complaints, a MMSE score of 24 or higher, and impaired neuropsychological assessment. They were compared with 46 healthy controls from the same community with normal neuropsychological performance. Five items did not discriminate well and were replaced. Scoring was then adjusted, giving increased weight to the most discriminant items. The final revised version of the MoCA (version 7.1) covers eight cognitive domains and underwent a validation study at the Neuro Rive-Sud (NRS) community memory clinic on the south-shore of Montreal and the Jewish General Hospital memory clinic in Montreal [1]. Participants were both English and French speaking subjects divided into three groups based on cognitive status; normal control (n = 90), Mild Cognitive Impairment (n = 94), and mild Alzheimer’s disease (n = 93). MoCA was administered to all groups, and its sensitivity and specificity were compared with those of the MMSE for detection of MCI and mild AD.
6.3.1 Optimal Cutoff Scores
Sensitivity was calculated separately for the MCI and AD groups. One point was added to the total MoCA score to correct for education effect for subjects with 12 years or less education. The MoCA exhibited excellent sensitivity in identifying MCI and AD (90 and 100 %, respectively). In contrast, the sensitivity of the MMSE was poor (18 and 78 %, respectively). Specificity was defined as the percentage of NCs that scored at or above the cutoff score of 26. The MMSE had excellent specificity, correctly identifying 100 % of the NCs. The MoCA had very good to excellent specificity (87 %). When MMSE and MoCA scores were plotted together (Fig. 6.1), the large majority of NC participants scored in the normal range, and the large majority of AD patients scored in the abnormal range on both MMSE and MoCA. In contrast, 73 % of MCI participants scored in the abnormal range on the MoCA but in the normal range on the MMSE [1].
Scatter plot of the Montreal Cognitive Assessment (MoCA) and the Mini-mental State Examination (MMSE) scores for normal controls (NC) and subjects with Mild Cognitive Impairment (MCI) and mild Alzheimer’s disease (AD) (Reproduced with permission [1])
The test-retest reliability was 0.92. The internal consistency of the MoCA was good with a Cronbach alpha on the standardized items of 0.83 [1]. In addition, the positive and negative predictive values for the MoCA were excellent for MCI (89 and 91 %, respectively) and mild AD (89 and 100 %, respectively).
6.3.2 Recommendations
The Third Canadian Consensus Conference on the Diagnosis and Treatment of Dementia (CCCDTD3) recommended administering the MoCA to subjects suspected to be cognitively impaired who perform in the normal range on the MMSE [115]. Immediate and Delayed recall, Orientation, and letter F fluency subtest of the MoCA have been proposed by the National Institute for Neurological Disorders and Stroke (NINDS) and the Canadian Stroke Network (CSN) to be a 5-minute Vascular Cognitive Impairment screening test administrable by telephone [116]. The MoCA has also been recommended for MCI or dementia screening in review articles [117–119].
6.3.3 Practical Approach
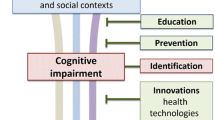
It is important to emphasize that MoCA is a cognitive screening instrument and not a diagnostic tool, hence clinical judgment, based on thorough clinical evaluation, is important in interpreting MoCA test results and correctly diagnosing patients who present with cognitive complaints. Figure 6.2 illustrates a practical approach to evaluate patients with cognitive complaints. Patients presenting with cognitive complaints and no functional impairment in their activities of daily living (ADL) would be better assessed by the MoCA as first cognitive screening test. Subjects presenting with cognitive complaints and ADL impairment would probably be better assessed by the MMSE first, then the MoCA if the MMSE is in the normal range.
Practical approach to evaluate patients who present with cognitive complaints. ADL Activities of Daily Living. NPV Negative Predictive Value, PPV Positive Predictive Value, MCI Mild Cognitive Impairment (Adapted from Nasreddine et al. [1])
6.4 Demographic Effect on MoCA Performance
Originally a highly educated normative group was used, suggesting a correction of one added point for education of 12 years or less [1]. Subsequent studies locally in Montreal suggest to better adjust the MoCA for lower educated subjects, 2 points should be added to the total MoCA© score for subjects with 4–9 years of education, 1 point for 10–12 years of education [120]. Education has been consistently reported around the world affecting total MoCA scores [1, 78, 121–126]. Trail making test and digit span of the Japanese version of the MoCA significantly correlate with years of schooling [127]. The cube copy, semantic fluency (substitution of letter F fluency), abstraction, serial-7 subtraction and naming in the Korean version of the MoCA positively correlated with education [79]. There are many cutoff scores reported according to the level of education of the studied population. In general, studies recruiting a higher proportion of low educated subjects recommend lower cutoff scores for the education correction.
The MoCA has been shown to be age [78, 122, 124, 125] and gender independent [78, 122, 124–126]. However, in a large normative study in the USA, age negatively correlated with MoCA scores. Upon further analysis, age was a significant factor in MoCA scores mostly for less educated subjects [126] which could be explained by low cognitive reserve among less educated individuals which may result in lessened ability to recruit neuronal networks and compensate age-related cognitive changes. Moreover, lower educated subjects are known to have more vascular risk factors that could also impair their cognition [128].
6.5 Mild Cognitive Impairment (MCI) and Alzheimer’s Disease (AD)
The MoCA has been extensively studied as a screening tool for detection of MCI and Alzheimer Disease (see Table 6.1; [1, 79, 121–123, 127, 129–137]). Sensitivity for MCI detection has been on average 86 % (range 77–96 %). Sensitivity to detect AD has been on average 97 % (range 88–100 %). Specificity, defined as correctly identifying normal controls, was on average 88 % (range 50–98 %). Table 6.1 summarizes the MoCA validation in MCI and AD in diverse populations and languages. Variability in sensitivity and specificity is explainable by differences in selection criteria for normal controls, diagnostic criteria for MCI and AD, community or memory clinic setting, confirmation with neuropsychological battery, age and education levels, and possibly linguistic and cultural factors.
6.6 Vascular Cognitive Impairment (VCI)
Multiple studies have addressed the usefulness of the MoCA in Vascular Cognitive Impairment (See Table 6.2; [78, 124, 138–149]).
6.6.1 Asymptomatic Cerebrovascular Disease Patients with Vascular Risk Factors
The MoCA has been shown to detect cognitive decline in asymptomatic subjects with hypertension alone, or thickening of the carotid artery wall, or multiple vascular risk factors [138, 139]. Cognitive decline was also detected in subjects with transient ischaemic attack (TIA) or first ever stroke if they had more than two vascular risk factors or low cerebral perfusion on transcranial Doppler ultrasound [138, 139]. MoCA also correlated with the Framingham coronary and stroke risk scores [150].
Advanced internal carotid artery stenosis (>70 %) occlusion is also negatively correlated with MoCA but not MMSE scores in asymptomatic subjects [141, 142].
Subtle cognitive impairment among subjects from cardiac and diabetic/endocrine outpatient clinics of a tertiary-referral hospital were detected using the MoCA with sensitivity of 83–100 %, but with lower specificity of 50–52 % [148].
6.6.2 Symptomatic Cerebrovascular Disease
6.6.2.1 Cognitive Impairment Post-stroke or TIA
The MoCA has been shown to detect cognitive impairment in 65 % of subjects 3 months post-stroke [145]. Also 30–58 % of subjects with TIA or stroke who were considered normal on the MMSE scored below the normal cut-off on the MoCA ranging from 14 days to up to 5 years after the event [143, 144]. Table 6.2 summarises studies of the MoCA for vascular cognitive impairment. Another study, using neuropsychological assessment as gold standard, found that MoCA had a sensitivity of 67 %, and a specificity of 90 % for detection of cognitive impairment post acute stroke [147]. In this study, the neuropsychological battery was not performed at the same time as the MoCA (24 versus 7 days respectively) which could explain significant differences in sensitivity and specificity compared to other studies, and the MoCA cut-off used was MoCA ≤20 [151].
6.6.2.2 Heart Failure
Fifty-four to seventy percent of non-demented community-dwelling adults with heart failure (HF) (ejection fraction 37–40 %) had low cognitive scores on the MoCA (≤26) [149, 151]. Reduction in ejection fraction and various associated vascular risk factors such as hypertension, dyslipidemia or diabetes mellitus may contribute to chronic reduction of cerebral blood flow in HF patients [152–154].
6.6.2.3 Sub-optimal Self-Care and Functional Dependency
MoCA identified MCI in patients with heart failure that had suboptimal self-care behaviours [155]. Using the MoCA as a cognitive assessment instrument, the self-rated version of the instrumental activities of daily living (IADL) scale was administered to evaluate functional dependence among 219 non-demented patients with cardiovascular diseases and risk factors [156]. MCI was diagnosed when MoCA was less than 23/30. Less dependence was associated with higher MoCA scores, and a person who scored in the MCI range was 7.7 times more likely to report need for assistance with one or more activity of daily living. This study indicated that subtle cognitive impairment was an independent predictor of functional status in patient with cardiovascular disease [156].
6.6.2.4 Cerebral Small Vessel Disease
MoCA was shown to be sensitive to white matter disease and a history of stroke, detecting cognitive impairment with a sensitivity of 73 % and specificity of 75 % [78].
6.6.2.5 Subcortical Ischaemic Vascular Dementia (SIVD)
Subcortical ischemic vascular injury has been proposed to be associated with cognitive impairment as a result of neuronal circuit disconnection between subcortical regions, frontal cortex and other cerebral regions following repeated silent subcortical injuries [157–160]. Vascular dementia was also detected by the MoCA with a sensitivity of 86.8 % and specificity of 92.9 % [124].
6.6.2.6 Monitoring of Treatment
Cognitive outcomes after undergoing carotid endarterectomy (CEA) in severe unilateral internal carotid artery stenosis were studied using MoCA and MMSE as primary outcome measures. Symptomatic carotid stenosis (SCS) and asymptomatic severe carotid stenosis ≥60 % (ACS) patients with the age- and sex-matched control subjects who underwent laparoscopic cholecystectomy (LC) were compared. At baseline, the SCS group, but not the ACS, was significantly more impaired on the MoCA and MMSE total scores compared with the LC group. Postoperatively, only the SCS patients had significant improvement on both tests when comparing pre-operative and 12-month post-operative performance [161].
6.7 Parkinson’s Disease (PD)
The prevalence of dementia in PD is between 20 and 40 % [162]. The early cognitive changes are mediated by fronto-striatal disconnection, such as executive function and attention [163]. Single domain impairment is found more frequently than multiple domain deficits in early stage disease [163, 164]. Progression of PD affects other cognitive domains such as memory [162, 165]. The association between cognitive impairment and cholinergic denervation and frontostriatal dopaminergic deficits among patients with PD and PD with dementia (PDD) has been demonstrated by neuroimaging studies [166, 167]. Detection of cognitive impairment in PD is clinically useful as it predicts the conversion to PDD [165], contributes to caregiver’s distress [168], and guides timing to initiate cognitive enhancing treatment [169].
The MoCA has an adequate sensitivity as a screening tool for detection of PD-MCI or PDD in a clinical setting (see Table 6.3), based on diagnostic criteria and neuropsychological test batteries [173, 174]. Half of PD patients with normal age and education-adjusted MMSE scores were cognitively impaired according to the recommended MoCA cutoff (25/26) [172, 177] as it lacks a ceiling [170, 171, 173]. Sensitivity and specificity for PDD was 81–82 and 75–95 % respectively. Sensitivity and specificity for PD-MCI was 83–90 and 53–75 % respectively [173, 174].
Baseline MoCA scores predicted the rate of cognitive deterioration among PD patients. The group of rapid decliners had lower scores on total MoCA score, clock drawing, attention, verbal fluency and abstraction subtest when compared with slow decliners [175].
MoCA was shown to have good reliability in this population. The test–retest correlation coefficient is 0.79, and the inter-rater correlation coefficient is 0.81 [170]. The superiority of the MoCA compared to the MMSE is probably explained by its more sensitive testing of executive, visuospatial, and attention domains which are frequently impaired in PD. Some of MoCA’s limitations are that there are no studies yet regarding its sensitivity to detect of cognitive change over time or after treatment [178] and MoCA contains items that require fine motor movement such as the trail making test, cube copy and clock drawing (5/30 points), which can impact on the results when administering the test to patients with severe motor symptoms.
6.8 Huntington’s Disease
Subtle cognitive impairment has been shown to precede motor manifestations of Huntington’s disease (HD) [179–182]. While global cognitive function is relatively preserved in asymptomatic carriers of HD mutation (AC), attention, psychomotor speed, working memory, verbal memory and executive function are often impaired early [180–182]. These impaired functions are caused by abnormal fronto-striatal circuitry as shown in morphological and functional studies [183, 184]. It is interesting to note that AC participants who were intact in memory subtest performed similarly to non-carriers on all other domains, and AC subjects with cognitive deficits performed qualitatively similarly to the symptomatic HD patients [182].
Two studies compared the ability of the MoCA and the MMSE to detect cognitive impairment in HD patients with mild to moderate motor symptoms. Compared with the MMSE, the MoCA achieved higher sensitivity (MoCA 97.4 %; MMSE 84.6 %), however, comparable but not impressive specificity (MoCA 30.1 %; MMSE 31.5 %), in discriminating the HD from normal subjects [185, 186]. The superiority of the MoCA compared to the MMSE in this population is explained by more emphasis in the MoCA on cognitive domains frequently impaired in early HD. Clock drawing, trail making, cube copy, abstraction and letter F fluency in the MoCA increase its ability to detect executive and visuo-spatial dysfunction. Five word delayed recall, digit span, letter tapping/vigilance test in the MoCA provide a better assessment of memory and attention. The limitation for interpreting these results is that the available studies did not use standardized neuropsychological evaluation as a gold standard for classifying cognitive function in HD.
6.9 Brain Tumours
MoCA detected cognitive impairment among patients with brain metastases in 70 % of patients who performed the MMSE in the normal range (≥26/30). Patients had abnormal delayed recall (90 %) or language (90 %) followed by deficits in visuo-spatial/executive function (60 %) and the other sub-domains [187].
Detection of MCI among patients with primary and metastatic brain tumors using a standardized neuropsychological assessment as a gold standard has also shown the superiority of the MoCA compared to the MMSE in sensitivity but at the expense of lower specificity. MoCA sensitivities and specificities were 62 and 56 % respectively, whereas MMSE sensitivities and specificities were 19 and 94 % respectively. Visuospatial/executive function items of the MoCA correlated with patients’ perceived quality of life (ability to work, sleep, enjoy life, enjoy regular activities and accept their illness) [188].
The cognitive function is one of the survival prognostic factors and correlates with tumor volume in metastatic brain cancer [189, 190]. The survival prognostic value of the MoCA was studied among patients with brain metastases [191]. After dichotomizing MoCA scores into two groups based on average scores (≥22 and <22), below-average MoCA scores were predictive of worse median overall survival (OS) compared with above-average group (6.3 versus 50.0 weeks). Stratified MoCA scores were also predictive of median OS, as the median OS of patients who performed with MoCA scores in the range of >26, 22–26, and <22, were 61.7, 30.9 and 6.3 weeks, respectively. MoCA scores were superior to the MMSE scores as a prognostic marker. Although the MoCA scores correlated with the median OS, it is essential to clarify that cognitive impairment does not directly result in decreased survival. Lower MoCA scores may represent other unmeasured confounders such as the extent of disease, location of tumor or previous treatment [191].
6.10 Systemic Lupus Erythematosus (SLE)
Cognitive dysfunction is a common symptom of SLE-associated neuropsychiatric manifestation. It can occur independently of clinical overt neuropsychiatric SLE [192–198]. Magnetic resonance spectroscopy reveals the association between metabolic change in white matter of non-neuropsychiatric SLE (non-NSLE) patients and cognitive impairment [193, 199]. Early cognitive impairments in non-NSLE patients are verbal fluency, digit symbol substitution and attention [198–200]. Some investigators suggested that the pattern of cognitive decline in non-NSLE is mostly classified as subcortical brain disease since the psychomotor and mental tracking impairment are observed early [201]. The domains which are subsequently impaired in patients who develop neuropsychiatric SLE (NSLE) symptoms are memory, psychomotor speed, reasoning and complex attention [200, 202].
The MoCA was validated among SLE patients in hospital-based recruitment, using the Automated Neuropsychologic Assessment Metrics (ANAM) as a gold standard. At the standard cutoff scores <26/30, the MoCA provided good sensitivity (83 %), specificity (73 %) and overall accuracy (75 %) in detection of cognitive impairment [203].
6.11 Substance Use Disorders
The validity of the MoCA to detect cognitive impairment in subjects with non-nicotine substance dependence disorders according to the DSM-IV criteria was established by using the Neuropsychological Assessment Battery-Screening Module (NAB-SM) as a gold standard to define cognitively impaired participants. The NAB-SM is composed of five domains: attention, language, memory, visuospatial, and executive function. The participants were composed of alcohol dependence (65 %; n = 39), dependence on opioids (32 %; n = 19), cocaine (17 %; n = 10), cannabis (12 %; n = 7), benzodiazepine (10 %; n = 6), and amphetamine (8 %; n = 5). At the optimal cutoff point of 25/26, the MoCA provided acceptable sensitivity and specificity of 83 and 73 %, respectively, with good patient acceptability [204].
6.12 Idiopathic Rapid Eye Movement Sleep Behavior Disorder (Idiopathic RBD)
RBD is characterized by the intermittent loss of REM sleep electromyographic atonia that elaborate motor activity associated with dream mentation. Approximately 60 % of cases are idiopathic [205]. MCI is found in 50 % of idiopathic RBD and most of them are single domain MCI with executive dysfunction and attention impairment [206]. Visuospatial construction and visuospatial learning may be impaired in neuropsychologically asymptomatic idiopathic RBD patients who have normal brain MRI [207]. Subtle cognitive changes in idiopathic RBD may reflect the early stage of neurodegenerative diseases [207] as some studies reported an association between idiopathic RBD and subsequent development of Parkinson’s disease (PD), Lewy body dementia (LBD) and multiple system atrophy [208–210]. Moreover, cognitive changes in idiopathic RBD are similar (visuoconstructional and visuospatial dysfunction) to LBD [211] and (executive dysfunction) to early PD [163].
The MCI screening property of the MoCA was validated among 38 idiopathic RBD patients, based on neuropsychological assessment as a gold standard. At the original cutoff point of 25/26, the MoCA had sensitivity for cognitive impairment of 76 % and specificity of 85 % with an accuracy of 79 %. However, for screening purposes, the higher cutoff (26/27) may be applied as it increases sensitivity to 88 %, at the expense of reduced specificity (61 %). The demanding visuospatial/executive functions subtests of the MoCA makes it sensitive for detection of mild cognitive impairment in idiopathic RBD patients who are impaired early in these domains [212].
6.13 Obstructive Sleep Apnoea (OSA)
In a recent study by Chen et al. [213], the MoCA was administered to 394 obstructive sleep apnea (OSA) patients categorized into four groups according to severity based on the total number of apnea and hypopnea per hour of sleep (AHI), measured by polysomnography. The groups were composed of primary snoring (AHI < 5 events/h), mild OSA (AHI 5–20 events/h), moderate OSA (AHI 21–40 events/h) and severe OSA (AHI > 40 events/h). The total MoCA scores progressively decreased as the severity of OSA increased. The scores of moderate-to-severe OSA groups were significantly lower than the scores of the primary snoring and mild OSA groups. Furthermore, defining MCI with a cutoff of 25/26, the moderate-to-severe OSA groups were more classified as MCI than the other groups. Domains that were significantly impaired in severe OSA group, compared to the primary snoring group, were delayed recall, visuospatial/executive function, and attention/concentration. Even though the mild OSA group performed similarly to the primary snoring group on total MoCA scores, impairment in the visuospatial/executive function and delayed recall domains were more prominent. Moreover, MoCA scores correlated with oxygen saturation levels [213].
6.14 Risk of Falls
Liu-Ambrose and colleagues used the MoCA to classify 158 community-dwelling women as MCI or cognitively intact by the cutoff point of 25/26 [214]. The short form of Physiologic Profile Assessment (PPA) was used to assess the fall risk profile. In the PPA, the postural sway, quadriceps femoris muscle strength, hand reaction time, proprioception and edge contrast sensitivity are evaluated. Participants with MCI had higher global physiological risk of falling and greater postural sway compared with the counterparts. However, the other four PPA components were not significantly different between the two groups. This study suggested that screening for MCI using the MoCA is valuable in preventing falls in the elderly.
6.15 Rehabilitation Outcome
The MoCA has been shown to be more sensitive than the MMSE for detection of MCI in inpatient rehabilitation setting [215]. The association between cognitive status measured by the MoCA and rehabilitation outcomes was studied among 47 patients admitted to a geriatric rehabilitation inpatient service [216]. Patients had an orthopedic injury (62 %), neurological condition (19 %), medically complex condition (11 %) and cardiac diseases (4 %). MoCA had good sensitivity (80 %), but poor specificity (30 %), at the cutoff scores 25/26 to predict successful rehabilitation outcome. The patients who reached the successful rehabilitation criteria tended to have higher MoCA scores at admission than the patients who did not achieve the rehabilitation goal. Many studies have reported the negative effect of cognitive impairment on rehabilitation outcomes [216–219].
In a short term rehabilitation program in post-stroke patients (median time post-stroke 8.5 days) who had MCI, the MoCA had a significant association with discharge functional status. The discharge functional status was measured by the motor subscale of Functional Independence Measures (mFIM) and motor relative functional efficacy taking the individual’s potential for improvement into account [220]. The visuospatial/executive domain of the MoCA was the strongest predictor of functional status and improvement. This domain was previously shown as an independent predictor of post-stroke long term functional outcome [221].
6.16 MoCA in Epilepsy
A cross-sectional study examined the MoCA performance in cryptogenic epileptic patients aged more than 15 years with normal global cognition according to the MMSE score. The mean MoCA score was 22.44 (± 4.32). In spite of a normal MMSE score, which was an inclusion criterion, cognitive impairment was detected in 60 % patients based on the MoCA score. The variable that correlated with a higher risk of cognitive impairment was the number of antiepileptic drugs (polytherapy: OR 2.71; CI 1.03–7.15). No neuropsychological batteries were used for comparison [222].
6.17 Normative Data in Multiple Languages, Cultures, Age and Education Levels
The Montreal Cognitive Assessment has been translated into 36 languages and dialects and has been used in several populations (Table 6.4 summarizes published studies and not abstracts). Test and instructions for all languages and dialects are available on the MoCA’s official website (www.mocatest.org).
Performance on the MoCA varied significantly among populations. Differences on MoCA performance in healthy subjects are probably accounted for by cultural, ethnic, age, educational, and linguistic factors. As with all neuropsychological tests, it is recommended that local normative values be obtained in communities around the world utilizing the MoCA. A large community based cognitive survey in Texas included a multi-ethnic sample of Caucasians, Blacks, and Hispanics, of varying educational levels. In this study, the majority of subjects (62 %) scored below 26 on the MoCA [126]. When one considers only the more educated Caucasian group of normal participants in this study, the mean score was 25.6/30 which is only slightly lower than the original cutoff score (25/26). However since standard neuropsychological assessment, neurological examination, and imaging studies, were not performed on the healthy volunteers, subtle cognitive deficits, neurological conditions, or imaging abnormalities may have been missed, which could account for lower performance on the MoCA [128]. This is most likely to happen in subjects with lower education and in ethnic communities that are prone to vascular risk factors with consequent subtle vascular cognitive impairment [128].
6.18 MoCA for the Blind
A version of the MoCA for assessment of cognition in the blind population has been published [225].
6.19 Future Research
To provide reliable and valid intercultural multi-lingual norms on the MoCA, a strict protocol (see MoCA-ACE: Age, Culture and Education Study, unpublished protocol) defining cognitively healthy subjects has been devised with strict criteria excluding subjects with any known risks for cognitive impairment. The MoCA-ACE protocol excludes for example subjects with vascular risk factors, sleep apnea, obesity, or who take sedative medications that may be important confounders in community based surveys [126].
To decrease possible learning effects when administering the MoCA multiple times in a short period of time, two new alternative and equivalent English versions of the MoCA have been validated [120], and are available on www.mocatest.org.
To better address the need for a specific and sensitive cognitive screening tool for illiterate and lower educated populations, a new version of the MoCA, the MoCA-Basic (MoCA-B) is being validated.
To better predict AD conversion among MCI subjects, a new MoCA Memory Index Score (MoCA-MIS) that takes into account delayed recall cueing performance has been devised (Abstract submitted for presentation at the Alzheimer Association International Conference, Vancouver, July 2012).
6.20 Conclusion
The MoCA promises to be a potentially useful, sensitive and specific cognitive screening instrument for detection of mild cognitive impairment in multiple neurological and systemic diseases that affect cognition across various cultures and languages.
References
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–9.
Kortte KB, Horner MD, Windham WK. The trail making test, part B: cognitive flexibility or ability to maintain set? Appl Neuropsychol. 2002;9:106–9.
Sánchez-Cubillo I, Periáñez JA, Adrover-Roig D, Rodríguez-Sánchez JM, Ríos-Lago M, Tirapu J, et al. Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc. 2009;15:438–50.
Crowe SF. The differential contribution of mental tracking, cognitive flexibility, visual search, and motor speed to performance on parts A and B of the Trail Making Test. J Clin Psychol. 1998;54:585–91.
O’Rourke JJF, Beglinger LJ, Smith MM, Mills J, Moser DJ, Rowe KC, et al. The Trail Making Test in prodromal Huntington disease: contributions of disease progression to test performance. J Clin Exp Neuropsychol. 2011;33:567–79.
Jacobson SC, Blanchard M, Connolly CC, Cannon M, Garavan H. An fMRI investigation of a novel analogue to the Trail-Making Test. Brain Cogn. 2011;77:60–70.
Zakzanis KK, Mraz R, Graham SJ. An fMRI study of the Trail Making Test. Neuropsychologia. 2005;43:1878–86.
Moll J, de Oliveira-Souza R, Moll FT, Bramati IE, Andreiuolo PA. The cerebral correlates of set-shifting: an fMRI study of the trail making test. Arq Neuropsiquiatr. 2002;60:900–5.
Stuss DT, Bisschop SM, Alexander MP, Levine B, Katz D, Izukawa D. The Trail Making Test: a study in focal lesion patients. Psychol Assess. 2001;13:230–9.
Gouveia PAR, Brucki SMD, Malheiros SMF, Bueno OFA. Disorders in planning and strategy application in frontal lobe lesion patients. Brain Cogn. 2007;63:240–6.
Tamez E, Myerson J, Morris L, White DA, Baum C, Connor LT. Assessing executive abilities following acute stroke with the trail making test and digit span. Behav Neurol. 2011;24:177–85.
Sinha P, Poggio T. Role of learning in three-dimensional form perception. Nature. 1996;384:460–3.
Wallach H, O’Connell DN, Neisser U. The memory effect of visual perception of three-dimensional form. J Exp Psychol. 1953;45:360–8.
Boxer AL, Kramer JH, Du A-T, Schuff N, Weiner MW, Miller BL, et al. Focal right inferotemporal atrophy in AD with disproportionate visual constructive impairment. Neurology. 2003;61:1485–91.
Tippett WJ, Black SE. Regional cerebral blood flow correlates of visuospatial tasks in Alzheimer’s disease. J Int Neuropsychol Soc. 2008;14:1034–45.
Possin KL, Laluz VR, Alcantar OZ, Miller BL, Kramer JH. Distinct neuroanatomical substrates and cognitive mechanisms of figure copy performance in Alzheimer’s disease and behavioral variant frontotemporal dementia. Neuropsychologia. 2011;49:43–8.
Gaestel Y, Amieva H, Letenneur L, Dartigues J-F, Fabrigoule C. Cube drawing performances in normal ageing and Alzheimer’s disease: data from the PAQUID elderly population-based cohort. Dement Geriatr Cogn Disord. 2006;21:22–32.
Shulman KI, Shedletsky R, Silver IL. The challenge of time: clock-drawing and cognitive function in the elderly. Int J Geriatr Psychiatry. 1986;1:135–40.
Pinto E, Peters R. Literature review of the Clock Drawing Test as a tool for cognitive screening. Dement Geriatr Cogn Disord. 2009;27:201–13.
Ino T, Asada T, Ito J, Kimura T, Fukuyama H. Parieto-frontal networks for clock drawing revealed with fMRI. Neurosci Res. 2003;45:71–7.
Kim H, Chey J. Effects of education, literacy, and dementia on the Clock Drawing Test performance. J Int Neuropsychol Soc. 2010;16:1138–46.
Rouleau I, Salmon DP, Butters N, Kennedy C, McGuire K. Quantitative and qualitative analyses of clock drawings in Alzheimer’s and Huntington’s disease. Brain Cogn. 1992;18:70–87.
Kim Y-S, Lee K-M, Choi BH, Sohn E-H, Lee AY. Relation between the clock drawing test (CDT) and structural changes of brain in dementia. Arch Gerontol Geriatr. 2009;48:218–21.
Cahn-Weiner DA, Sullivan EV, Shear PK, Fama R, Lim KO, Yesavage JA, et al. Brain structural and cognitive correlates of clock drawing performance in Alzheimer’s disease. J Int Neuropsychol Soc. 1999;5:502–9.
Thomann PA, Toro P, Dos Santos V, Essig M, Schröder J. Clock drawing performance and brain morphology in mild cognitive impairment and Alzheimer’s disease. Brain Cogn. 2008;67:88–93.
Parks RW, Thiyagesh SN, Farrow TFD, Ingram L, Wilkinson K, Hunter MD, et al. Performance on the clock drawing task correlates with FMRI response to a visuospatial task in Alzheimer’s disease. Int J Neurosci. 2010;120:335–43.
Lee DY, Seo EH, Choo IH, Kim SG, Lee JS, Lee DS, et al. Neural correlates of the Clock Drawing Test performance in Alzheimer’s disease: a FDG-PET study. Dement Geriatr Cogn Disord. 2008;26:306–13.
Cosentino S, Jefferson A, Chute DL, Kaplan E, Libon DJ. Clock drawing errors in dementia: neuropsychological and neuroanatomical considerations. Cogn Behav Neurol. 2004;17:74–84.
Liss B, Roeper J. Individual dopamine midbrain neurons: functional diversity and flexibility in health and disease. Brain Res Rev. 2008;58:314–21.
Price CC, Cunningham H, Coronado N, Freedland A, Cosentino S, Penney DL, et al. Clock drawing in the Montreal Cognitive Assessment: recommendations for dementia assessment. Dement Geriatr Cogn Disord. 2011;31:179–87.
Nitrini R, Caramelli P, Herrera Júnior E, Porto CS, Charchat-Fichman H, Carthery MT, et al. Performance of illiterate and literate nondemented elderly subjects in two tests of long-term memory. J Int Neuropsychol Soc. 2004;10:634–8.
Brodaty H, Moore CM. The Clock Drawing Test for dementia of the Alzheimer’s type: a comparison of three scoring methods in a memory disorders clinic. Int J Geriatr Psychiatry. 1997;12:619–27.
Hodges JR, Salmon DP, Butters N. The nature of the naming deficit in Alzheimer’s and Huntington’s disease. Brain. 1991;114:1547–58.
Chertkow H, Bub D. Semantic memory loss in dementia of Alzheimer’s type. What do various measures measure? Brain. 1990;113:397–417.
Bayles KA, Tomoeda CK. Confrontation naming impairment in dementia. Brain Lang. 1983;19:98–114.
Frank EM, McDade HL, Scott WK. Naming in dementia secondary to Parkinson’s, Huntington’s, and Alzheimer’s diseases. J Commun Disord. 1996;29:183–97.
Smith CD, Andersen AH, Kryscio RJ, Schmitt FA, Kindy MS, Blonder LX, et al. Differences in functional magnetic resonance imaging activation by category in a visual confrontation naming task. J Neuroimaging. 2001;11:165–70.
Chouinard PA, Goodale MA. Category-specific neural processing for naming pictures of animals and naming pictures of tools: an ALE meta-analysis. Neuropsychologia. 2010;48:409–18.
Bai H-M, Jiang T, Wang W-M, Li T-D, Liu Y, Lu Y-C. Functional MRI mapping of category-specific sites associated with naming of famous faces, animals and man-made objects. Neurosci Bull. 2011;27:307–18.
Okada T, Tanaka S, Nakai T, Nishizawa S, Inui T, Sadato N, et al. Naming of animals and tools: a functional magnetic resonance imaging study of categorical differences in the human brain areas commonly used for naming visually presented objects. Neurosci Lett. 2000;296:33–6.
Fung TD, Chertkow H, Murtha S, Whatmough C, Péloquin L, Whitehead V, et al. The spectrum of category effects in object and action knowledge in dementia of the Alzheimer’s type. Neuropsychology. 2001;15:371–9.
Mainy N, Jung J, Baciu M, Kahane P, Schoendorff B, Minotti L, et al. Cortical dynamics of word recognition. Hum Brain Mapp. 2008;29:1215–30.
Kaneko H, Yoshikawa T, Nomura K, Ito H, Yamauchi H, Ogura M, et al. Hemodynamic changes in the prefrontal cortex during digit span task: a near-infrared spectroscopy study. Neuropsychobiology. 2011;63:59–65.
Hoshi Y, Oda I, Wada Y, Ito Y, Yutaka Y, Oda M, et al. Visuospatial imagery is a fruitful strategy for the digit span backward task: a study with near-infrared optical tomography. Brain Res Cogn Brain Res. 2000;9:339–42.
Sun X, Zhang X, Chen X, Zhang P, Bao M, Zhang D, et al. Age-dependent brain activation during forward and backward digit recall revealed by fMRI. Neuroimage. 2005;26:36–47.
Gerton BK, Brown TT, Meyer-Lindenberg A, Kohn P, Holt JL, Olsen RK, et al. Shared and distinct neurophysiological components of the digits forward and backward tasks as revealed by functional neuroimaging. Neuropsychologia. 2004;42:1781–7.
Belleville S, Peretz I, Malenfant D. Examination of the working memory components in normal aging and in dementia of the Alzheimer type. Neuropsychologia. 1996;34:195–207.
Morris RG, Baddeley AD. Primary and working memory functioning in Alzheimer-type dementia. J Clin Exp Neuropsychol. 1988;10:279–96.
Muangpaisan W, Intalapaporn S, Assantachai P. Digit span and verbal fluency tests in patients with mild cognitive impairment and normal subjects in Thai-community. J Med Assoc Thai. 2010;93:224–30.
Petrova M, Raycheva M, Zhelev Y, Traykov L. Executive functions deficit in Parkinson’s disease with amnestic mild cognitive impairment. Am J Alzheimers Dis Other Demen. 2010;25:455–60.
Leung JLM, Lee GTH, Lam YH, Chan RCC, Wu JYM. The use of the Digit Span Test in screening for cognitive impairment in acute medical inpatients. Int Psychogeriatr. 2011;23:1569–74.
Kurt P, Yener G, Oguz M. Impaired digit span can predict further cognitive decline in older people with subjective memory complaint: a preliminary result. Aging Ment Health. 2011;15:364–9.
Cicerone KD. Clinical sensitivity of four measures of attention to mild traumatic brain injury. Clin Neuropsychol. 1997;11:266–72.
Cicerone KD, Azulay J. Diagnostic utility of attention measures in postconcussion syndrome. Clin Neuropsychol. 2002;16:280–9.
Rémy F, Mirrashed F, Campbell B, Richter W. Mental calculation impairment in Alzheimer’s disease: a functional magnetic resonance imaging study. Neurosci Lett. 2004;358:25–8.
Dehaene S, Spelke E, Pinel P, Stanescu R, Tsivkin S. Sources of mathematical thinking: behavioral and brain-imaging evidence. Science. 1999;284:970–4.
Menon V, Rivera SM, White CD, Glover GH, Reiss AL. Dissociating prefrontal and parietal cortex activation during arithmetic processing. Neuroimage. 2000;12:357–65.
Roland PE, Friberg L. Localization of cortical areas activated by thinking. J Neurophysiol. 1985;53:1219–43.
Chase TN, Fedio P, Foster NL, Brooks R, Di Chiro G, Mansi L. Wechsler Adult Intelligence Scale performance: cortical localization by fluorodeoxyglucose F 18-positron emission tomography. Arch Neurol. 1984;41:1244–7.
Zago L, Pesenti M, Mellet E, Crivello F, Mazoyer B, Tzourio-Mazoyer N. Neural correlates of simple and complex mental calculation. Neuroimage. 2001;13:314–27.
Rueckert L, Lange N, Partiot A, Appollonio I, Litvan I, Le Bihan D, et al. Visualizing cortical activation during mental calculation with functional MRI. Neuroimage. 1996;3:97–103.
Hirono N, Mori E, Ishii K, Imamura T, Shimomura T, Tanimukai S, et al. Regional metabolism: associations with dyscalculia in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 1998;65:913–6.
Small JA, Kemper S, Lyons K. Sentence repetition and processing resources in Alzheimer’s disease. Brain Lang. 2000;75:232–58.
Kopelman MD. Recall of anomalous sentences in dementia and amnesia. Brain Lang. 1986;29:154–70.
Meyers JE, Volkert K, Diep A. Sentence repetition test: updated norms and clinical utility. Appl Neuropsychol. 2000;7:154–9.
Baldo JV, Shimamura AP, Delis DC, Kramer J, Kaplan E. Verbal and design fluency in patients with frontal lobe lesions. J Int Neuropsychol Soc. 2001;7:586–96.
Baldo JV, Shimamura AP. Letter and category fluency in patients with frontal lobe lesions. Neuropsychology. 1998;12:259–67.
Troyer AK, Moscovitch M, Winocur G, Alexander MP, Stuss D. Clustering and switching on verbal fluency: the effects of focal frontal- and temporal-lobe lesions. Neuropsychologia. 1998;36:499–504.
Perret E. The left frontal lobe of man and the suppression of habitual responses in verbal categorical behaviour. Neuropsychologia. 1974;12:323–30.
Pendleton MG, Heaton RK, Lehman RA, Hulihan D. Diagnostic utility of the Thurstone Word Fluency Test in neuropsychological evaluations. J Clin Neuropsychol. 1982;4:307–17.
Frith CD, Friston K, Liddle PF, Frackowiak RS. Willed action and the prefrontal cortex in man: a study with PET. Proc Biol Sci. 1991;244:241–6.
Parks RW, Loewenstein DA, Dodrill KL, Barker WW, Yoshii F, Chang JY, et al. Cerebral metabolic effects of a verbal fluency test: a PET scan study. J Clin Exp Neuropsychol. 1988;10:565–75.
Phelps EA, Hyder F, Blamire AM, Shulman RG. FMRI of the prefrontal cortex during overt verbal fluency. Neuroreport. 1997;8:561–5.
Alvarez JA, Emory E. Executive function and the frontal lobes: a meta-analytic review. Neuropsychol Rev. 2006;16:17–42.
Ostrosky-Solís F, Ardila A, Rosselli M, Lopez-Arango G, Uriel-Mendoza V. Neuropsychological test performance in illiterate subjects. Arch Clin Neuropsychol. 1998;13:645–60.
Ostrosky-Solís F, Ardila A, Rosselli M. NEUROPSI: a brief neuropsychological test battery in Spanish with norms by age and educational level. J Int Neuropsychol Soc. 1999;5:413–33.
Rosselli M, Ardila A, Rosas P. Neuropsychological assessment in illiterates. II. Language and praxic abilities. Brain Cogn. 1990;12:281–96.
Wong A, Xiong YY, Kwan PWL, Chan AYY, Lam WWM, Wang K, et al. The validity, reliability and clinical utility of the Hong Kong Montreal Cognitive Assessment (HK-MoCA) in patients with cerebral small vessel disease. Dement Geriatr Cogn Disord. 2009;28:81–7.
Lee J-Y, Dong WL, Cho S-J, Na DL, Hong JJ, Kim S-K, et al. Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J Geriatr Psychiatry Neurol. 2008;21:104–10.
Henry JD, Crawford JR. Verbal fluency deficits in Parkinson’s disease: a meta-analysis. J Int Neuropsychol Soc. 2004;10:608–22.
Larsson MU, Almkvist O, Luszcz MA, Wahlin T-BR. Phonemic fluency deficits in asymptomatic gene carriers for Huntington’s disease. Neuropsychology. 2008;22:596–605.
Ho AK, Sahakian BJ, Robbins TW, Barker RA, Rosser AE, Hodges JR. Verbal fluency in Huntington’s disease: a longitudinal analysis of phonemic and semantic clustering and switching. Neuropsychologia. 2002;40:1277–84.
Murphy KJ, Rich JB, Troyer AK. Verbal fluency patterns in amnestic mild cognitive impairment are characteristic of Alzheimer’s type dementia. J Int Neuropsychol Soc. 2006;12:570–4.
Henry J, Crawford JR. A meta-analytic review of verbal fluency deficits in depression. J Clin Exp Neuropsychol. 2005;27:78–101.
Woo BKP, Harwood DG, Melrose RJ, Mandelkern MA, Campa OM, Walston A, et al. Executive deficits and regional brain metabolism in Alzheimer’s disease. Int J Geriatr Psychiatry. 2010;25:1150–8.
Slachevsky A, Villalpando JM, Sarazin M, Hahn-Barma V, Pillon B, Dubois B. Frontal assessment battery and differential diagnosis of frontotemporal dementia and Alzheimer disease. Arch Neurol. 2004;61:1104–7.
Fabrigoule C, Rouch I, Taberly A, Letenneur L, Commenges D, Mazaux JM, et al. Cognitive process in preclinical phase of dementia. Brain. 1998;121:135–41.
Fouquet M, Desgranges B, La Joie R, Rivière D, Mangin J-F, Landeau B, et al. Role of hippocampal CA1 atrophy in memory encoding deficits in amnestic mild cognitive impairment. Neuroimage. 2012;59:3309–15.
Chetelat G, Desgranges B, de la Sayette V, Viader F, Berkouk K, Landeau B, et al. Dissociating atrophy and hypometabolism impact on episodic memory in mild cognitive impairment. Brain. 2003;126:1955–67.
Cummings JL, Benson DF. Subcortical dementia. Review of an emerging concept. Arch Neurol. 1984;41:874–9.
Lafosse JM, Reed BR, Mungas D, Sterling SB, Wahbeh H, Jagust WJ. Fluency and memory differences between ischemic vascular dementia and Alzheimer’s disease. Neuropsychology. 1997;11:514–22.
Traykov L, Baudic S, Raoux N, Latour F, Rieu D, Smagghe A, et al. Patterns of memory impairment and perseverative behavior discriminate early Alzheimer’s disease from subcortical vascular dementia. J Neurol Sci. 2005;229–230:75–9.
Ibarretxe-Bilbao N, Zarei M, Junque C, Marti MJ, Segura B, Vendrell P, et al. Dysfunctions of cerebral networks precede recognition memory deficits in early Parkinson’s disease. Neuroimage. 2011;57:589–97.
Fine EM, Delis DC, Wetter SR, Jacobson MW, Hamilton JM, Peavy G, et al. Identifying the “source” of recognition memory deficits in patients with Huntington’s disease or Alzheimer’s disease: evidence from the CVLT-II. J Clin Exp Neuropsychol. 2008;30:463–70.
Massman PJ, Delis DC, Butters N, Levin BE, Salmon DP. Are all subcortical dementias alike? Verbal learning and memory in Parkinson’s and Huntington’s disease patients. J Clin Exp Neuropsychol. 1990;12:729–44.
Whittington CJ, Podd J, Kan MM. Recognition memory impairment in Parkinson’s disease: power and meta-analyses. Neuropsychology. 2000;14:233–46.
Higginson CI, Wheelock VL, Carroll KE, Sigvardt KA. Recognition memory in Parkinson’s disease with and without dementia. J Clin Exp Neuropsychol. 2005;27:516–28.
Fossati P, Deweer B, Raoux N, Allilaire JF. Deficits in memory retrieval: an argument in favor of frontal subcortical dysfunction in depression [in French]. Encéphale. 1995;21:295–305.
Mesholam-Gately RI, Giuliano AJ, Zillmer EA, Barakat LP, Kumar A, Gur RC, et al. Verbal learning and memory in older adults with minor and major depression. Arch Clin Neuropsychol. 2012;27:196–207.
Pasquier F, Grymonprez L, Lebert F, Van der Linden M. Memory impairment differs in frontotemporal dementia and Alzheimer’s disease. Neurocase. 2001;7:161–71.
Wicklund AH, Johnson N, Rademaker A, Weitner BB, Weintraub S. Word list versus story memory in Alzheimer disease and frontotemporal dementia. Alzheimer Dis Assoc Disord. 2006;20:86–92.
Kazui H. Cognitive impairment in patients with idiopathic normal pressure hydrocephalus. Brain Nerve. 2008;60:225–31.
Peavy G, Jacobs D, Salmon DP, Butters N, Delis DC, Taylor M, et al. Verbal memory performance of patients with human immunodeficiency virus infection: evidence of subcortical dysfunction. The HNRC Group. J Clin Exp Neuropsychol. 1994;16:508–23.
Becker JT, Caldararo R, Lopez OL, Dew MA, Dorst SK, Banks G. Qualitative features of the memory deficit associated with HIV infection and AIDS: cross-validation of a discriminant function classification scheme. J Clin Exp Neuropsychol. 1995;17:134–42.
Leube DT, Weis S, Freymann K, Erb M, Jessen F, Heun R, et al. Neural correlates of verbal episodic memory in patients with MCI and Alzheimer’s disease – a VBM study. Int J Geriatr Psychiatry. 2008;23:1114–8.
Kramer JH, Levin BE, Brandt J, Delis DC. Differentiation of Alzheimer’s, Huntington’s, and Parkinson’s disease patients on the basis of verbal learning characteristics. Neuropsychology. 1989;3:111–20.
Caulo M, Van Hecke J, Toma L, Ferretti A, Tartaro A, Colosimo C, et al. Functional MRI study of diencephalic amnesia in Wernicke-Korsakoff syndrome. Brain. 2005;128:1584–94.
Scoville WB, Milner B. Loss of recent memory after bilateral hippocampal lesions. J Neurol Neurosurg Psychiatry. 1957;20:11–21.
Milner B. Psychological defects produced by temporal lobe excision. Res Publ Assoc Res Nerv Ment Dis. 1958;36:244–57.
Razani J, Wong JT, Dafaeeboini N, Edwards-Lee T, Lu P, Alessi C, et al. Predicting everyday functional abilities of dementia patients with the Mini-Mental State Examination. J Geriatr Psychiatry Neurol. 2009;22:62–70.
Razani J, Kakos B, Orieta-Barbalace C, Wong JT, Casas R, Lu P, et al. Predicting caregiver burden from daily functional abilities of patients with mild dementia. J Am Geriatr Soc. 2007;55:1415–20.
O’Keeffe E, Mukhtar O, O’Keeffe ST. Orientation to time as a guide to the presence and severity of cognitive impairment in older hospital patients. J Neurol Neurosurg Psychiatry. 2011;82:500–4.
Guerrero-Berroa E, Luo X, Schmeidler J, Rapp MA, Dahlman K, Grossman HT, et al. The MMSE orientation for time domain is a strong predictor of subsequent cognitive decline in the elderly. Int J Geriatr Psychiatry. 2009;24:1429–37.
Ryan JJ, Glass LA, Bartels JM, Bergner CM, Paolo AM. Predicting neuropsychological test performance on the basis of temporal orientation. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2009;16:330–7.
Chertkow H, Nasreddine Z, Joanette Y, Drolet V, Kirk J, Massoud F, et al. Mild cognitive impairment and cognitive impairment, no dementia: part A, concept and diagnosis. Alzheimers Dement. 2007;3:266–82.
Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37:2220–41.
Howe E. Initial screening of patients for Alzheimer’s disease and minimal cognitive impairment. Psychiatry (Edgmont). 2007;4(7):24–7.
Ismail Z, Rajji TK, Shulman KI. Brief cognitive screening instruments: an update. Int J Geriatr Psychiatry. 2010;25:111–20.
Mitchell AJ, Malladi S. Screening and case finding tools for the detection of dementia. Part I: evidence-based meta-analysis of multidomain tests. Am J Geriatr Psychiatry. 2010;18:759–82.
Chertkow H, Nasreddine Z, Phillips N, Johns E, Whitehead V, McHenry C, et al. The Montreal Cognitive Assessment (MoCA): Validation of alternate forms and new recommendations for education corrections. Alzheimers Dement. 2011;7 Suppl 1:S156–7 (abstract P1–143).
Zhao S, Guo C, Wang M, Chen W, Wu Y, Tang W, et al. A clinical memory battery for screening for amnestic mild cognitive impairment in an elderly Chinese population. J Clin Neurosci. 2011;18:774–9.
Luis CA, Keegan AP, Mullan M. Cross validation of the Montreal Cognitive Assessment in community dwelling older adults residing in the Southeastern US. Int J Geriatr Psychiatry. 2009;24:197–201.
Ng Hoi Yee K. The validity of the Montreal Cognitive Assessment (Cantonese version) as a screening tool for mild cognitive impairment in Hong Kong Chinese. The University of Hong Kong; 2008.
You JS, Chen RZ, Zhang FM, Cai YF, Li GF. The Chinese (Cantonese) Montreal Cognitive Assessment in patients with subcortical ischemic vascular dementia. Dement Geriatr Cogn Dis Extra. 2011;1:276–82.
Bernstein IH, Lacritz L, Barlow CE, Weiner MF, Defina LF. Psychometric evaluation of the Montreal Cognitive Assessment (MoCA) in three diverse samples. Clin Neuropsychol. 2011;25:119–26.
Rossetti HC, Lacritz LH, Cullum CM, Weiner MF. Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology. 2011;77:1272–5.
Fujiwara Y, Suzuki H, Yasunaga M, Sugiyama M, Ijuin M, Sakuma N, et al. Brief screening tool for mild cognitive impairment in older Japanese: validation of the Japanese version of the Montreal Cognitive Assessment. Geriatr Gerontol Int. 2010;10:225–32.
Nasreddine ZS, Phillips NA, Chertkow H, et al. Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology. 2012;78:765–6.
Smith T, Gildeh N, Holmes C. The Montreal Cognitive Assessment: validity and utility in a memory clinic setting. Can J Psychiatry. 2007;52:329–32.
Rahman TTA, El Gaafary MM. Montreal Cognitive Assessment Arabic version: reliability and validity prevalence of mild cognitive impairment among elderly attending geriatric clubs in Cairo. Geriatr Gerontol Int. 2009;9:54–61.
Tangwongchai S, Phanasathit M, Charernboon T, Akkayagorn L, Hemrungrojn H, Phanthumchinda K et al. The validity of Thai version of The Montreal Cognitive Assessment (MoCA-T). In: International Psychogeriatric Association conference, Montreal, Abstract, 2009.
Duro D, Simões MR, Ponciano E, Santana I. Validation studies of the Portuguese experimental version of the Montreal Cognitive Assessment (MoCA): confirmatory factor analysis. J Neurol. 2010;257:728–34.
Selekler K, Cangoz B, Uluç S. Power of discrimination of Montreal Cognitive Assessment (MoCA) Scale in Turkish patients with mild cognitive impairment and Alzheimer’s disease. Turk J Geriatr. 2010;13:166–71.
Larner AJ. Screening utility of the Montreal Cognitive Assessment (MoCA): in place of – or as well as – the MMSE? Int Psychogeriatr. 2012;24:391–6.
Karunaratne S, Hanwella R, Silva VD. Validation of the Sinhala version of the Montreal Cognitive Assessment in screening for dementia. Ceylon Med J. 2011;56:147–53.
Damian AM, Jacobson SA, Hentz JG, Belden CM, Shill HA, Sabbagh MN, et al. The Montreal Cognitive Assessment and the mini-mental state examination as screening instruments for cognitive impairment: item analyses and threshold scores. Dement Geriatr Cogn Disord. 2011;31:126–31.
Freitas S, Simões MR. Construct validity of the Montreal Cognitive Assessment (MoCA). J Int Neuropsychol Soc. 2012;18:1–9.
Martinić-Popović I, Šerić V, Demarin V. Early detection of mild cognitive impairment in patients with cerebrovascular disease. Acta Clin Croatica. 2006;45:77–85.
Martinić-Popović I, Serić V, Demarin V. Mild cognitive impairment in symptomatic and asymptomatic cerebrovascular disease. J Neurol Sci. 2007;257:185–93.
Wong A, Kwan P, Chan A, Lam W, Wang K, Nyenhuis D, et al. The validity, reliability and utility of the Cantonese Montreal Cognitive Assessment (MoCA) in Chinese patients with confluent white matter lesions. Hong Kong Med J. 2008;14 Suppl 6:7 (Abstract FP1).
Martinic-Popovic I, Lovrencic-Huzjan A, Demarin V. Assessment of subtle cognitive impairment in stroke-free patients with carotid disease. Acta Clin Croatica. 2009;48:231–40.
Martinic-Popovic I, Lovrencic-Huzjan A, Simundic A-M, Popovic A, Seric V, Demarin V. Cognitive performance in asymptomatic patients with advanced carotid disease. Cogn Behav Neurol. 2011;24:145–51.
Dong Y, Sharma VK, Chan BP-L, Venketasubramanian N, Teoh HL, Seet RCS, et al. The Montreal Cognitive Assessment (MoCA) is superior to the Mini-Mental State Examination (MMSE) for the detection of vascular cognitive impairment after acute stroke. J Neurol Sci. 2010;299:15–8.
Pendlebury ST, Cuthbertson FC, Welch SJV, Mehta Z, Rothwell PM. Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke. 2010;41:1290–3.
Cumming TB, Bernhardt J, Linden T. The Montreal Cognitive Assessment: short cognitive evaluation in a large stroke trial. Stroke. 2011;42:2642–4.
Harkness K, Demers C, Heckman GA, McKelvie RS. Screening for cognitive deficits using the Montreal cognitive assessment tool in outpatients ≥65 years of age with heart failure. Am J Cardiol. 2011;107:1203–7.
Godefroy O, Fickl A, Roussel M, Auribault C, Bugnicourt JM, Lamy C, et al. Is the Montreal Cognitive Assessment superior to the Mini-Mental State Examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation. Stroke. 2011;42:1712–6.
McLennan SN, Mathias JL, Brennan LC, Stewart S. Validity of the Montreal Cognitive Assessment (MoCA) as a screening test for mild cognitive impairment (MCI) in a cardiovascular population. J Geriatr Psychiatry Neurol. 2011;24:33–8.
Athilingam P, King KB, Burgin SW, Ackerman M, Cushman LA, Chen L. Montreal Cognitive Assessment and Mini-Mental Status Examination compared as cognitive screening tools in heart failure. Heart Lung. 2011;40:521–9.
Weiner MF, Hynan LS, Rossetti H, Warren MW, Cullum CM. The relationship of Montreal Cognitive Assessment scores to Framingham coronary and stroke risk scores. Open J Psychiatry. 2011;01:49–55.
Blackburn DJ, Walters S, Harkness K. Letter by Blackburn et al regarding article, “Is the Montreal cognitive assessment superior to the mini-mental state examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation”. Stroke. 2011;42:e582.
Loncar G, Bozic B, Lepic T, Dimkovic S, Prodanovic N, Radojicic Z, et al. Relationship of reduced cerebral blood flow and heart failure severity in elderly males. Aging Male. 2011;14:59–65.
Gruhn N, Larsen FS, Boesgaard S, Knudsen GM, Mortensen SA, Thomsen G, et al. Cerebral blood flow in patients with chronic heart failure before and after heart transplantation. Stroke. 2001;32:2530–3.
Pullicino PM, Hart J. Cognitive impairment in congestive heart failure? Embolism vs hypoperfusion. Neurology. 2001;57:1945–6.
Cameron J, Worrall-Carter L, Page K, Riegel B, Lo SK, Stewart S. Does cognitive impairment predict poor self-care in patients with heart failure? Eur J Heart Fail. 2010;12:508–15.
McLennan SN, Mathias JL, Brennan LC, Russell ME, Stewart S. Cognitive impairment predicts functional capacity in dementia-free patients with cardiovascular disease. J Cardiovasc Nurs. 2010;25:390–7.
Corbett A, Bennett H, Kos S. Cognitive dysfunction following subcortical infarction. Arch Neurol. 1994;51:999–1007.
Corbett AJ, Bennett H, Kos S. Frontal signs following subcortical infarction. Clin Exp Neurol. 1992;29:161–71.
Nagaratnam N, Bou-Haidar P, Leung H. Confused and disturbed behavior in the elderly following silent frontal lobe infarction. Am J Alzheimers Dis Other Demen. 2003;18:333–9.
Xu Q, Zhou Y, Li Y-S, Cao W-W, Lin Y, Pan Y-M, et al. Diffusion tensor imaging changes correlate with cognition better than conventional MRI findings in patients with subcortical ischemic vascular disease. Dement Geriatr Cogn Disord. 2010;30:317–26.
Baracchini C, Mazzalai F, Gruppo M, Lorenzetti R, Ermani M, Ballotta E. Carotid endarterectomy protects elderly patients from cognitive decline: a prospective study. Surgery. 2012;151:99–106.
Marder K. Cognitive impairment and dementia in Parkinson’s disease. Mov Disord. 2010;25 Suppl 1:S110–6.
Caviness JN, Driver-Dunckley E, Connor DJ, Sabbagh MN, Hentz JG, Noble B, et al. Defining mild cognitive impairment in Parkinson’s disease. Mov Disord. 2007;22:1272–7.
Mamikonyan E, Moberg PJ, Siderowf A, Duda JE, Have TT, Hurtig HI, et al. Mild cognitive impairment is common in Parkinson’s disease patients with normal Mini-Mental State Examination (MMSE) scores. Parkinsonism Relat Disord. 2009;15:226–31.
Williams-Gray CH, Foltynie T, Brayne CEG, Robbins TW, Barker RA. Evolution of cognitive dysfunction in an incident Parkinson’s disease cohort. Brain. 2007;130:1787–98.
Cropley VL, Fujita M, Bara-Jimenez W, Brown AK, Zhang X-Y, Sangare J, et al. Pre- and post-synaptic dopamine imaging and its relation with frontostriatal cognitive function in Parkinson disease: PET studies with [11C]NNC 112 and [18F]FDOPA. Psychiatry Res. 2008;163:171–82.
Bohnen NI, Kaufer DI, Hendrickson R, Ivanco LS, Lopresti BJ, Constantine GM, et al. Cognitive correlates of cortical cholinergic denervation in Parkinson’s disease and parkinsonian dementia. J Neurol. 2006;253:242–7.
Aarsland D, Larsen JP, Karlsen K, Lim NG, Tandberg E. Mental symptoms in Parkinson’s disease are important contributors to caregiver distress. Int J Geriatr Psychiatry. 1999;14:866–74.
Maidment I, Fox C, Boustani M. Cholinesterase inhibitors for Parkinson’s disease dementia (Review). Cochrane Database Syst Rev. 2006;(1):CD004747.
Gill DJ, Freshman A, Blender JA, Ravina B. The Montreal cognitive assessment as a screening tool for cognitive impairment in Parkinson’s disease. Mov Disord. 2008;23:1043–6.
Zadikoff C, Fox SH, Tang-Wai DF, Thomsen T, de Bie RM, Wadia P, et al. A comparison of the mini mental state exam to the Montreal cognitive assessment in identifying cognitive deficits in Parkinson’s disease. Mov Disord. 2008;23:297–9.
Nazem S, Siderowf A, Duda J, Have TT, Colcher A, Horn SS, et al. Montreal Cognitive Assessment performance in patients with Parkinson’s disease with “normal” global cognition according to Mini-Mental State Examination score. J Am Geriatr Soc. 2009;57:304–8.
Hoops S, Nazem S, Siderowf AD, Duda JE, Xie SX, Stern MB, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology. 2009;73:1738–45.
Dalrymple-Alford JC, MacAskill MR, Nakas CT, Livingston L, Graham C, Crucian GP, et al. The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75:1717–25.
Luo X-G, Feng Y, Liu R, Yu H-M, Wang L, Wu Z, et al. Cognitive deterioration rates in patients with Parkinson’s disease from northeastern China. Dement Geriatr Cogn Disord. 2010;30:64–70.
Robben SHM, Sleegers MJM, Dautzenberg PLJ, van Bergen FS, ter Bruggen J-P, Rikkert MGMO. Pilot study of a three-step diagnostic pathway for young and old patients with Parkinson’s disease dementia: screen, test and then diagnose. Int J Geriatr Psychiatry. 2010;25:258–65.
Hanna-Pladdy B, Enslein A, Fray M, Gajewski BJ, Pahwa R, Lyons KE. Utility of the NeuroTrax computerized battery for cognitive screening in Parkinson’s disease: comparison with the MMSE and the MoCA. Int J Neurosci. 2010;120:538–43.
Chou KL, Amick MM, Brandt J, Camicioli R, Frei K, Gitelman D, et al. A recommended scale for cognitive screening in clinical trials of Parkinson’s disease. Mov Disord. 2010;25:2501–7.
Lemiere J, Decruyenaere M, Evers-Kiebooms G, Vandenbussche E, Dom R. Longitudinal study evaluating neuropsychological changes in so-called asymptomatic carriers of the Huntington’s disease mutation after 1 year. Acta Neurol Scand. 2002;106:131–41.
Lemiere J, Decruyenaere M, Evers-Kiebooms G, Vandenbussche E, Dom R. Cognitive changes in patients with Huntington’s disease (HD) and asymptomatic carriers of the HD mutation a longitudinal follow-up study. J Neurol. 2004;251:935–42.
Verny C, Allain P, Prudean A, Malinge M-C, Gohier B, Scherer C, et al. Cognitive changes in asymptomatic carriers of the Huntington disease mutation gene. Eur J Neurol. 2007;14:1344–50.
Hahn-Barma V, Deweer B, Dürr A, Dode C, Feingold J, Pillon B, et al. Are cognitive changes the first symptoms of Huntington’s disease? A study of gene carriers. J Neurol Neurosurg Psychiatry. 1998;64:172–7.
Bäckman L, Robins-Wahlin T-B, Lundin A, Ginovart N, Farde L. Cognitive deficits in Huntington’s disease are predicted by dopaminergic PET markers and brain volumes. Brain. 1997;120:2207–17.
Montoya A, Price BH, Menear M, Lepage M. Brain imaging and cognitive dysfunctions in Huntington’s disease. J Psychiatry Neurosci. 2006;31:21–9.
Mickes L, Jacobson M, Peavy G, Wixted JT, Lessig S, Goldstein JL, et al. A comparison of two brief screening measures of cognitive impairment in Huntington’s disease. Mov Disord. 2010;25:2229–33.
Videnovic A, Bernard B, Fan W, Jaglin J, Leurgans S, Shannon KM. The Montreal Cognitive Assessment as a screening tool for cognitive dysfunction in Huntington’s disease. Mov Disord. 2010;25:401–4.
Olson RA, Chhanabhai T, McKenzie M. Feasibility study of the Montreal Cognitive Assessment (MoCA) in patients with brain metastases. Support Care Cancer. 2008;16:1273–8.
Olson RA, Iverson GL, Carolan H, Parkinson M, Brooks BL, McKenzie M. Prospective comparison of two cognitive screening tests: diagnostic accuracy and correlation with community integration and quality of life. J Neurooncol. 2011;105:337–44.
Meyers CA, Smith JA, Bezjak A, Mehta MP, Liebmann J, Illidge T, et al. Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: results of a randomized phase III trial. J Clin Oncol. 2004;22:157–65.
Chang EL, Wefel JS, Maor MH, Hassenbusch SJ, Mahajan A, Lang FF, et al. A pilot study of neurocognitive function in patients with one to three new brain metastases initially treated with stereotactic radiosurgery alone. Neurosurgery. 2007;60:277–83; discussion 283–284.
Olson R, Tyldesley S, Carolan H, Parkinson M, Chhanabhai T, McKenzie M. Prospective comparison of the prognostic utility of the Mini Mental State Examination and the Montreal Cognitive Assessment in patients with brain metastases. Support Care Cancer. 2011;19:1849–55.
Hanly JG, Fisk JD, Sherwood G, Jones E, Jones JV, Eastwood B. Cognitive impairment in patients with systemic lupus erythematosus. J Rheumatol. 1992;19:562–7.
Kozora E, Arciniegas DB, Filley CM, Ellison MC, West SG, Brown MS, et al. Cognition, MRS neurometabolites, and MRI volumetrics in non-neuropsychiatric systemic lupus erythematosus: preliminary data. Cogn Behav Neurol. 2005;18:159–62.
Kozora E, Arciniegas DB, Filley CM, West SG, Brown M, Miller D, et al. Cognitive and neurologic status in patients with systemic lupus erythematosus without major neuropsychiatric syndromes. Arthritis Rheum. 2008;59:1639–46.
Monastero R, Bettini P, Del Zotto E, Cottini E, Tincani A, Balestrieri G, et al. Prevalence and pattern of cognitive impairment in systemic lupus erythematosus patients with and without overt neuropsychiatric manifestations. J Neurol Sci. 2001;184:33–9.
Carlomagno S, Migliaresi S, Ambrosone L, Sannino M, Sanges G, Di Iorio G. Cognitive impairment in systemic lupus erythematosus: a follow-up study. J Neurol. 2000;247:273–9.
Carbotte RM, Denburg SD, Denburg JA. Prevalence of cognitive impairment in systemic lupus erythematosus. J Nerv Ment Dis. 1986;174:357–64.
Kozora E, Thompson LL, West SG, Kotzin BL. Analysis of cognitive and psychological deficits in systemic lupus erythematosus patients without overt central nervous system disease. Arthritis Rheum. 1996;39:2035–45.
Filley CM, Kozora E, Brown MS, Miller DE, West SG, Arciniegas DB, et al. White matter microstructure and cognition in non-neuropsychiatric systemic lupus erythematosus. Cogn Behav Neurol. 2009;22:38–44.
Denburg SD, Carbotte RM, Denburg JA. Cognitive impairment in systemic lupus erythematosus: a neuropsychological study of individual and group deficits. J Clin Exp Neuropsychol. 1987;9:323–39.
Leritz E, Brandt J, Minor M, Reis-Jensen F, Petri M. “Subcortical” cognitive impairment in patients with systemic lupus erythematosus. J Int Neuropsychol Soc. 2000;6:821–5.
Loukkola J, Laine M, Ainiala H, Peltola J, Metsänoja R, Auvinen A, et al. Cognitive impairment in systemic lupus erythematosus and neuropsychiatric systemic lupus erythematosus: a population-based neuropsychological study. J Clin Exp Neuropsychol. 2003;25:145–51.
Adhikari T, Piatti A, Luggen M. Cognitive dysfunction in SLE: development of a screening tool. Lupus. 2011;20:1142–6.
Copersino ML, Fals-Stewart W, Fitzmaurice G, Schretlen DJ, Sokoloff J, Weiss RD. Rapid cognitive screening of patients with substance use disorders. Exp Clin Psychopharmacol. 2009;17:337–44.
Thorpy MJ. International classification of sleep disorders, revised: diagnostic and coding manual. Chicago: American Academy of Sleep Medicine; 2001.
Gagnon J-F, Vendette M, Postuma RB, Desjardins C, Massicotte-Marquez J, Panisset M, et al. Mild cognitive impairment in rapid eye movement sleep behavior disorder and Parkinson’s disease. Ann Neurol. 2009;66:39–47.
Ferini-Strambi L, Gioia MRD, Castronovo V, Oldani A, Zucconi M, Cappa SF. Neuropsychological assessment in idiopathic REM sleep behavior disorder (RBD): does the idiopathic form of RBD really exist? Neurology. 2004;62:41–5.
Iranzo A, Molinuevo JL, Santamaría J, Serradell M, Martí MJ, Valldeoriola F, et al. Rapid-eye-movement sleep behaviour disorder as an early marker for a neurodegenerative disorder: a descriptive study. Lancet Neurol. 2006;5:572–7.
Boeve BF, Silber MH, Ferman TJ, Lucas JA, Parisi JE. Association of REM sleep behavior disorder and neurodegenerative disease may reflect an underlying synucleinopathy. Mov Disord. 2001;16:622–30.
Claassen DO, Josephs KA, Ahlskog JE, Silber MH, Tippmann-Peikert M, Boeve BF. REM sleep behavior disorder preceding other aspects of synucleinopathies by up to half a century. Neurology. 2010;75:494–9.
Mori E, Shimomura T, Fujimori M, Hirono N, Imamura T, Hashimoto M, et al. Visuoperceptual impairment in dementia with Lewy bodies. Arch Neurol. 2000;57:489–93.
Gagnon J-F, Postuma RB, Joncas S, Desjardins C, Latreille V. The Montreal Cognitive Assessment: a screening tool for mild cognitive impairment in REM sleep behavior disorder. Mov Disord. 2010;25:936–40.
Chen R, Xiong KP, Huang JY, Lian YX, Jin F, Li ZH, et al. Neurocognitive impairment in Chinese patients with obstructive sleep apnoea hypopnoea syndrome. Respirology. 2011;16:842–8.
Liu-Ambrose TY, Ashe MC, Graf P, Beattie BL, Khan KM. Increased risk of falling in older community-dwelling women with mild cognitive impairment. Phys Ther. 2008;88:1482–91.
Aggarwal A, Kean E. Comparison of the Folstein Mini Mental State Examination (MMSE) to the Montreal Cognitive Assessment (MoCA) as a cognitive screening tool in an inpatient rehabilitation setting. Neurosci Med. 2010;1:39–42.
Sweet L, Van Adel M, Metcalf V, Wright L, Harley A, Leiva R, et al. The Montreal Cognitive Assessment (MoCA) in geriatric rehabilitation: psychometric properties and association with rehabilitation outcomes. Int Psychogeriatr. 2011;23:1582–91.
Heruti RJ, Lusky A, Dankner R, Ring H, Dolgopiat M, Barell V, et al. Rehabilitation outcome of elderly patients after a first stroke: effect of cognitive status at admission on the functional outcome. Arch Phys Med Rehabil. 2002;83:742–9.
Heruti RJ, Lusky A, Barell V, Ohry A, Adunsky A. Cognitive status at admission: does it affect the rehabilitation outcome of elderly patients with hip fracture? Arch Phys Med Rehabil. 1999;80:432–6.
Barnes C, Conner D, Legault L, Reznickova N, Harrison-Felix C. Rehabilitation outcomes in cognitively impaired patients admitted to skilled nursing facilities from the community. Arch Phys Med Rehabil. 2004;85:1602–7.
Toglia J, Fitzgerald KA, O’Dell MW, Mastrogiovanni AR, Lin CD. The Mini-Mental State Examination and Montreal Cognitive Assessment in persons with mild subacute stroke: relationship to functional outcome. Arch Phys Med Rehabil. 2011;92:792–8.
Wagle J, Farner L, Flekkøy K, Bruun Wyller T, Sandvik L, Fure B, et al. Early post-stroke cognition in stroke rehabilitation patients predicts functional outcome at 13 months. Dement Geriatr Cogn Disord. 2011;31:379–87.
Phabphal K, Kanjanasatien J. Montreal Cognitive Assessment in cryptogenic epilepsy patients with normal Mini-Mental State Examination scores. Epileptic Disord. 2011;13:375–81.
Memoria CM, Yassuda MS, Nakano EY, Forlenza OV. Brief screening for mild cognitive impairment: validation of the Brazilian version of the Montreal cognitive assessment. Int J Geriatr Psychiatry. 2012. doi:10.1002/gps.3787 [Epub ahead of print].
Thissen AJAM, van Bergen F, de Jonghe JFM, Kessels RPC, Dautzenberg PLJ. Applicability and validity of the Dutch version of the Montreal Cognitive Assessment (MoCA-d) in diagnosing MCI [in Dutch]. Tijdschr Gerontol Geriatr. 2010;41:231–40.
Wittich W, Phillips N, Nasreddine ZS, Chertkow H. Sensitivity and specificity of the Montreal Cognitive Assessment modified for individuals who are visually impaired. J Vis Impair Blind. 2010;104:360–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag London
About this chapter
Cite this chapter
Julayanont, P., Phillips, N., Chertkow, H., Nasreddine, Z.S. (2013). Montreal Cognitive Assessment (MoCA): Concept and Clinical Review. In: Larner, A. (eds) Cognitive Screening Instruments. Springer, London. https://doi.org/10.1007/978-1-4471-2452-8_6
Download citation
DOI: https://doi.org/10.1007/978-1-4471-2452-8_6
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-2451-1
Online ISBN: 978-1-4471-2452-8
eBook Packages: MedicineMedicine (R0)