Abstract
Objective
This study examined the associations of 25-hydroxycholecalciferol [25(OH)D3] and intact parathyroid hormone (iPTH) concentrations with bone status parameters in elderly subjects.
Design/Setting
Cross-sectional data based on the follow-up 2008 of the longitudinal study on nutrition and health status of senior citizens in Giessen, Germany.
Participants
One hundred eighty-eight independently living subjects aged 66–96 years.
Measurements
Serum concentrations of 25(OH)D3, iPTH, N-terminal propeptide of type 1 collagen (P1NP) and activity of alkaline phosphatase (ALP) were assessed. Broadband ultrasound attenuation, speed of sound and stiffness index were determined by calcaneal quantitative ultrasound (QUS). Multiple linear regression analyses were performed to analyse associations of 25(OH)D3 and iPTH with bone status parameters.
Results
Median (range) 25(OH)D3 and iPTH concentrations were 62.8 (29.9–106.7) nmol/L and 4.6 (1.3–21.0) pmol/L, respectively. Neither 25(OH)D3 nor iPTH was associated with calcaneal bone characteristics measured by QUS, whereas negative associations between 25(OH)D3 and bone formation markers (P1NP and ALP) were found. In a sub analysis, 25(OH)D3 was negatively associated with ALP only in subjects with iPTH concentrations > 4.59 pmol/L.
Conclusion
The present study provides no evidence for independent associations of 25(OH)D3 and iPTH with calcaneal bone characteristics in community-dwelling elderly subjects with 25(OH)D3 concentrations between 30 and 107 nmol/L. However, 25(OH)D3 interacts with bone formation markers, particularly in subjects with high iPTH concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D and parathyroid hormone (PTH) are crucial for calcium and phosphorus homeostasis and thus play an important role in the development and maintenance of bone architecture. Several observational studies have investigated the impact of 25-hydroxyvitamin D [25(OH)D], the established biomarker of vitamin D status, and/or PTH on bone status (1–15), but with inconsistent findings. Likewise, supplementation trials yielded conflicting results regarding the effect of vitamin D on bone health and fracture risk. A recent Cochrane review concluded that supplementation of vitamin D combined with calcium, but not vitamin D alone, may protect against fractures in older subjects (16). Therefore, 25(OH)D may not exert substantial effects on bones independent of calcium homeostasis. Another explanation for the inconsistent study results is the presence of nonlinear associations between circulating 25(OH)D and bone status parameters, i.e. that 25(OH)D may impact bone status predominantly at low 25(OH)D concentrations (4, 11). Concentrations below 25 nmol/L represent vitamin D deficiency and are linked to hyperparathyroidism, increased bone turnover and mineralisation defects and consequently osteomalacia (17). Although less clear, vitamin D insufficiency, i.e. 25(OH)D concentrations above 25 up to 50 nmol/L or even higher, has been associated with elevated PTH concentrations and the development of osteoporosis (17). At present, there is no general consensus on which 25(OH)D and PTH concentrations are optimal to maintain bone health and prevent fractures. According to the Institute of Medicine, 25(OH)D concentrations ≥ 50 nmol/L cover the needs of most subjects as regards skeletal health outcomes (18), whereas the Endocrine Society recommends concentrations ≥ 75 nmol/L (19).
For clinical diagnosis of osteoporosis, dual-energy X-ray absorptiometry (DXA) is commonly used (20). Other techniques, such as quantitative ultrasound (QUS), may be useful to gain information on structural and quality aspects of bones, including elasticity and connectivity of trabecular bone (21). The risk profile can be completed by using bone turnover markers, such as N-terminal propeptide of type 1 collagen (P1NP) and alkaline phosphatase (ALP), in conjunction with an assessment of classical risk factors for osteoporosis (20, 22).
At present, data on the associations of 25(OH)D and PTH with calcaneal bone characteristics measured by QUS and bone turnover markers in non-vitamin D-deficient, independently living elderly subjects are scarce. In view of the frequently observed sex differences in vitamin D status (9, 14) and the differences between women and men as regards bone formation and bone loss over the lifecycle (23), sex may impact these associations, but this has been seldom addressed in previous studies.
The primary objective of the present study was to analyse whether concentrations of 25-hydroxycholecalciferol [25(OH)D3] and intact PTH (iPTH) are independently associated with calcaneal QUS parameters and bone formation markers in noninstitutionalised elderly subjects with 25(OH)D3 concentrations above 25 nmol/L. In this context, we analysed whether the associations differed by sex, vitamin D status or iPTH status.
Methods
Study design and subjects
The here presented cross-sectional data based on the followup 2008 of the longitudinal study on nutrition and health status of senior citizens in Giessen (GISELA study), Germany (latitude 50.6°N), in which 275 Caucasian subjects participated (24). General inclusion criteria for enrolment in the GISELA study were an age of at least 60 years and physical mobility, which meant that subjects should be able to visit the institute without assistance.
For the present explorative investigation, subjects with incomplete data on relevant parameters (i.e. serum 25(OH)D3, serum iPTH, bone status, body composition, nutrient intake, current time spent outdoors, physical activity and smoking behaviour) were excluded (n = 73). Subjects with reported diagnosis of chronic kidney disease in the last four years (n = 5) and history of chronic liver disease/liver cancer (n = 11) or kidney/bladder cancer (n = 3) were also not considered in this analysis, as these diseases were shown to impair vitamin D and/or bone metabolism (25–28). However, a few of these subjects were already excluded for missing data. Because bone status parameters did not differ between subjects with and without a lifetime history of rheumatism, diabetes mellitus or hyperthyroidism in sex-specific analyses (all P > 0.05), subjects who suffered from these diseases were not excluded. The final study population consisted of 134 postmenopausal women and 54 men, aged 66–96 years.
Ethics statement
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and the research protocol was approved by the Ethical Committee of the Faculty of Medicine at the Justus-Liebig-University of Giessen, Germany. Written informed consent was obtained from all participants before examinations.
Biochemical analyses
In 2008, fasting blood samples were collected from the end of July to September, and serum aliquots were stored at −70 °C until analysed. Serum concentrations of 25(OH)D3, iPTH, total P1NP, cortisol and thyroid stimulating hormone were measured by an electrochemiluminescence immunoassay (ECLIA) using Modular E170 (Roche Diagnostics GmbH, Mannheim, Germany) in the Limbach Laboratory, Heidelberg, Germany (29–33). Total ALP activity was assessed by photometric detection (Modular Hitachi, Roche Diagnostics GmbH, Mannheim, Germany) in the Limbach Laboratory, Heidelberg, Germany (34). The 25(OH)D3 assay has been standardised against liquid chromatography-tandem mass spectrometry (31). The laboratory performing the 25(OH)D3 analyses participated in the Vitamin D External Quality Assessment Scheme.
Serum concentrations of 17β-estradiol, luteinising hormone, follicle stimulating hormone and testosterone were measured by ECLIA using Modular E170 (Roche Diagnostics GmbH, Mannheim, Germany) in the Limbach Laboratory, Heidelberg, Germany (35–38).
Serum creatinine was determined by photometric detection (Shimadzu UV-160A, Shimadzu, Kyoto, Japan) and the estimated glomerular filtration rate (eGFR) was calculated by using the simplified Modification of Diet in Renal Disease study formula (39).
Calcaneal bone status as judged by quantitative ultrasound
Bone status was determined by QUS via water-based Achilles+ Solo Ultrasonometer (Lunar Corporation, Madison, WI, USA) and the software version 3.0. Measurements were carried out in the left calcaneus and in an uprightseated position (40). The QUS parameters were broadband ultrasound attenuation (BUA, dB/MHz), speed of sound (SOS, m/s) and stiffness index (SI, %). SI was calculated by the Achilles system: SI = 0.67 × BUA + 0.28 × SOS – 420 (41). The phantom provided by the manufacturer was used for calibration. The calculated coefficients of variation for repeated measurements over 20 consecutive days in 10 subjects aged 25–52 years were 2.4 %, 0.5 % and 2.3 % for BUA, SOS and SI, respectively (40).
According to the definition of the World Health Organization, which based on DXA measurements in white postmenopausal women, osteoporosis is defined as a BMD of –2.5 standard deviations equal or less than the average value of a young healthy reference group (expressed as T-score ≤ –2.5) (20). For QUS measurements, no generally accepted T-score to discriminate osteoporotic subjects from non-osteoporotic subjects exists (40). Therefore, we used additional T-scores of ≤ –2.94 and ≤ –3.68 as threshold values for identification of osteoporotic subjects. The first T-score represents the best relation between sensitivity and specificity as regards the identification of osteoporotic females and the second T-score was found to identify the same percentage of osteoporotic women in the GISELA population as with DXA measurements at the femoral neck (40). T-score and Z-score were calculated by the device-specific software of the Achilles system.
Anthropometric data and body composition
Body mass index (BMI) was calculated from the measured weight and height (kg/m2), which were determined in light clothing without shoes using a calibrated scale with an integrated stadiometer (Seca, Vogel & Halke GmbH & Co. KG, Hamburg, Germany). Fat mass and fat-free mass were assessed by a single-frequency (50 kHz) bioelectrical impedance analyser in a supine position (Akern-RJL BIA 101/S, Data Input, Frankfurt, Germany) according to the formula of Roubenoff et al. (42).
Lifestyle factors
A self-administered questionnaire on health and lifestyle characteristics was handed out to the participants. Among others, study participants were asked to record their current time spent on different physical activities in hours per week and the physical activity level was calculated by dividing the total energy expenditure by the resting metabolic rate measured by indirect calorimetry as described previously (43). Sunlight exposure was estimated by asking the subjects, how much time they currently spent outdoors in minutes per day. Subjects were classified as current/ex-smokers and as non-smokers when they have never smoked.
Information on fractures, cortisone therapy and hormone replacement therapy
The incidence of fractures was assessed by a selfadministered questionnaire on the occurrence of any fractures in the last four years prior to completion of the questionnaire. Subjects were asked on their use of cortisone and whether they have undergone hormone replacement therapy (HRT).
Dietary assessment and use of anti-osteoporotic drugs and vitamin D/calcium supplements
Daily intake of proteins, vitamin D, calcium, phosphorus and alcohol was determined using a validated three-day estimated dietary record consisting of 146 food items and beverages (44).
Data on the use of anti-osteoporotic drugs and vitamin D/calcium supplements were collected via self-administered questionnaire and subjects were accordingly classified into users and non-users. Except for one subject, all vitamin D supplement users supplemented also calcium and except for one subject, all users of anti-osteoporotic drugs reported to use vitamin D and/or calcium supplements as well. Therefore, we created a dichotomous variable (‘use of vitamin D/calcium supplements and/or anti-osteoporotic drugs (no vs. yes)’).
Statistical analyses
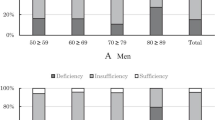
Continuous data are expressed as median and 25th–75th percentiles due to the presence of non-normally distributed data. Descriptive characteristics were compared between women and men via Mann–Whitney U test for continuous variables. Chisquared or Fisher’s exact test was used to assess differences in proportions. Subjects with insufficient and sufficient 25(OH)D3 concentrations (two cut-off values were used: 25(OH)D3 < vs. ≥ 50.0 nmol/L and < vs. ≥ 75.0 nmol/L) as well as subjects with and without hyperparathyroidism (iPTH ≤ vs. > 6.9 pmol/L) were compared with regard to bone status parameters using the Mann–Whitney U test.
In linear regression analyses, normal distribution of residuals was checked by Shapiro-Wilk test and by visual inspection of diagrams. In view of the skewed distributions, P1NP and ALP were logarithmically transformed (lg10). Residuals for QUS parameters showed to some extent deviations from normal distribution. In this case, lg10 transformation of QUS parameters to approximate normal distribution yielded comparable results. Therefore, non-transformed QUS data are presented.
Simple regression analyses were performed to investigate the non-adjusted associations between 25(OH)D3 or iPTH with bone status parameters. Using sex-adjusted linear regression analyses (enter procedure), we analysed whether age, month of blood sampling, body mass, BMI, fat mass, fat-free mass, lifestyle factors, alcohol consumption, dietary calcium to phosphorus ratio, dietary intake of proteins and vitamin D, use of vitamin D/calcium supplements and/or antiosteoporotic drugs, HRT of more than 12 months during or after menopause (only women), eGFR, thyroid stimulating hormone concentration, cortisol concentration and concentrations of sex hormones correlated with bone status parameters, respectively. Those parameters that showed significant associations with bone status parameters were included in subsequent multiple linear regression analyses with 25(OH)D3 and iPTH as independent variables and QUS parameters, P1NP or ALP as dependent variable. Relevant covariables were included in the model by using stepwise selection procedure, whereas 25(OH)D3 and iPTH were kept in the model regardless of statistical significance. As regards body mass, BMI, fat mass and fat-free mass, we created separate models to prevent collinearity. In multiple regression analyses, variance inflation factors were < 5.0 and tolerance statistics were > 0.20. Effect modification by sex was investigated by adding interaction terms (sex × 25(OH)D3 and sex × iPTH, respectively) to the regression models (enter procedure; P < 0.100 as significance level).
A sensitivity analysis was conducted to examine the consistency of the results by excluding subjects with oedema, immobility for more than one month within the last two years prior to examination, fracture in the last four years, bilateral oophorectomy before the age of 46, amenorrhea > 6 months during reproductive years, pre-menopausal antioestrogen treatment, cortisone therapy > 6 months in the last four years and current use of vitamin D/calcium supplements, anti-osteoporotic drugs, antiepileptic drugs, tamoxifen or arimidix. In addition, the multiple regression analyses were performed stratified by the median 25(OH)D3 and iPTH status to investigate whether the associations differed by vitamin D or iPTH status. The median was used as splitting criterion to get two equal-sized groups. Due to the reduction/subdivision of the sample size, no additional stratification by sex was performed in these analyses.
Because of the explorative character of the present study, no adjustment for multiple hypotheses testing has been performed. Statistical analyses were conducted with IBM® SPSS® Statistics for Windows, version 22.0 (IBM Corporation, USA). Significance level was set at P < 0.05 if not otherwise indicated, and all tests were two-tailed.
Results
Characteristics of the study subjects
Sex-specific descriptive characteristics are presented in Table 1. A T-score of ≤ −2.50, ≤ –2.94 and ≤ –3.68 was observed in 20 %, 12 % and 3 % of the study population, respectively. In contrast, no subject had a Z-score ≤ −2.50. p ]Median (range) 25(OH)D3 and iPTH concentrations were 62.8 (29.9–106.7) nmol/L and 4.6 (1.3–21.0) pmol/L, respectively. Serum 25(OH)D3 concentrations < 50.0 nmol/L and ≥ 75.0 nmol/L were evident in 21 % and 20 % of the subjects, respectively. Subjects with 25(OH)D3 concentrations < 50.0 nmol/L had lower BUA (109 vs. 117 db/MHz), SOS (1513 vs. 1522 m/s), SI (77 vs. 84 %), T-score (−1.7 vs. −1.2) and Z-score (0.1 vs. 0.7) than subjects with higher concentrations (all P < 0.05). However, except for higher ALP values in subjects with 25(OH)D3 concentrations < 75.0 nmol/L (69 vs. 60 U/L, P < 0.05), no differences in bone status parameters were found between subjects with 25(OH)D3 concentrations < and ≥ 75.0 nmol/L (all P > 0.05). Hyperparathyroidism (iPTH > 6.9 pmol/L) was found in 16 % of the subjects. Except for higher ALP values in subjects with iPTH concentrations > 6.9 pmol/L (74 vs. 67 U/L, P < 0.05), no differences in bone status parameters were found as regards the presence of hyperparathyroidism (all P > 0.05).
Both lg10 P1NP (B = −20.58, β = −0.138, P = 0.049) and lg10 ALP (B = −42.51, β = −0.154, P = 0.028) correlated negatively with SOS in sex-adjusted linear regression analyses, but not with BUA or SI (all P > 0.05).
Simple regression analyses of 25(OH)D3 and iPTH with bone status parameters
In simple regression analyses, concentrations of 25(OH)D3 and iPTH showed no significant associations with QUS parameters (Supplementary material 1). However, 25(OH)D3 was negatively associated with lg10 P1NP in women (B = −0.002, β = −0.178, P = 0.039) and with lg10 ALP in women (B = −0.002, β = −0.225, P = 0.009) and in the entire cohort (B = −0.002, β = −0.201, P = 0.006), whereas men showed no associations.
Selection of covariables for the final multiple regression analyses
Those parameters, which were significantly associated at least with one of the bone status parameters according to sex-adjusted regression analyses are presented in Table 2. Age, body mass, BMI, fat mass, fat-free mass, month of blood sampling and use of vitamin D/calcium supplements and/or anti-osteoporotic drugs were identified as relevant covariables. Consequently, these parameters were considered in addition to sex as covariables in the subsequent multiple regression analyses. As regards body mass, BMI, fat mass and fat-free mass, we created separate models. In Table 3, the model with absolute fat-free mass is presented because of the higher adjusted coefficient of determination (R2) in sex-specific analyses compared to the models with body mass, BMI and fat mass. The results of the regression analyses with body mass, BMI and fat mass are available as supplementary material.
Multiple linear regression analyses of 25(OH)D3 and iPTH with bone status parameters
In multiple linear regression analyses, 25(OH)D3 and iPTH were not associated with QUS parameters or lg10 P1NP, whereas 25(OH)D3 was associated with lg10 ALP in the entire cohort and in women after adjustment for sex (if women and men combined), iPTH, age, fat-free mass, month of blood sampling and use of vitamin D/calcium supplements and/or anti-osteoporotic drugs (Table 3). The results remained essentially unchanged when sex was not considered as covariable or when absolute fat-free mass was replaced by body mass, BMI or fat mass (Supplementary material 2–5). However, when a subject with a P1NP concentration of 135 μg/L, who was identified as an outlier in view of the residuals, was excluded from the analysis, a negative association between 25(OH)D3 and lg10 P1NP was found in women (B = −0.003, β = −0.203, P = 0.026). As to the regression models presented in Table 3, effect modification by sex was found for the associations of 25(OH)D3 and iPTH with lg10 P1NP and the association between iPTH and BUA (all P < 0.100).
The sensitivity analysis, which compromised 116 subjects after the exclusion of subjects reporting conditions which may have influenced bone, 25(OH)D3 or iPTH status, yielded comparable results by indicating only a significant association between 25(OH)D3 and lg10 ALP (B = −0.002, β = −0.213, P = 0.025) after adjustment for iPTH, sex, age, fat-free mass and month of blood sampling.
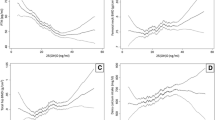
Associations of 25(OH)D3 and iPTH with bone status parameters as a function of vitamin D and iPTH status
When the study population was stratified according to the median vitamin D and iPTH status, respectively, no significant associations of 25(OH)D3 and iPTH with bone status parameters were present after adjustment for sex, age, fat-free mass, month of blood sampling and use of vitamin D/calcium supplements and/or anti-osteoporotic drugs, except for an association between 25(OH)D3 and lg10 ALP in subjects with iPTH concentrations > 4.59 pmol/L (Table 4). Excluding one subject with an ALP value of 143 U/L, who was identified as an outlier in view of the residuals, resulted in a negative association between 25(OH)D3 and lg10 ALP in subjects with 25(OH)D3 concentrations ≤ 62.8 nmol/L (B = −0.003, β = −0.217, P = 0.048). Likewise, a positive association between iPTH and lg10 P1NP was present in subjects with 25(OH)D3 concentrations > 62.8 nmol/L (B = 0.018, β = 0.214, P = 0.039), when an outlier was excluded (P1NP = 135 μg/L).
Discussion
The results of the present investigation indicate inverse associations between 25(OH)D3 and bone formation markers, but no associations of 25(OH)D3 and iPTH with QUS parameters. These findings corroborate the hypothesis that 25(OH)D3 and iPTH are not significantly associated with calcaneal bone characteristics in independently living elderly with a vitamin D status between 30 and 107 nmol/L and an iPTH status, which is primarily in the reference range. However, 25(OH)D3 concentrations still play a role in bone metabolism by interacting with bone formation markers, particularly in elderly women and in subjects with iPTH concentrations ≥ 4.6 pmol/L.
The observed sex difference in the association between 25(OH)D3 and bone formation markers could be due to the unequal sample sizes, the lower QUS parameters and the lower fat-free mass in women compared to men. In addition, bone turnover assessed by bone formation markers tended to be higher in women than in men. However, interaction by sex for the association between 25(OH)D3 and ALP did not reach significance. In the present study, P1NP and ALP were predominantly in a range considered as adequate for this age group (27, 33, 34, 45). Given that only a low fraction of the variance in P1NP and ALP could be explained by the final multiple regression models and the fact that we measured total ALP, the clinical relevance of the negative associations between 25(OH)D3 and bone formation markers as regards bone health requires further investigation. The fact that the GISELA subjects showed predominantly a vitamin D status > 50 nmol/L, an iPTH status in the reference range and a median calcium intake of 1 g/d may explain the missing associations of 25(OH)D3, iPTH and QUS parameters.
A special feature of the present study is the comprehensive consideration of potential confounding factors. Thereby, we could not confirm a relevance of lifestyle factors, nutrient intake, eGFR and concentrations of cortisol, thyroid stimulating hormone and sex hormones with respect to the analysed bone status parameters. The negative associations between the use of vitamin D/calcium supplements and/or anti-osteoporotic drugs and QUS parameters, which we found in the present study, indicate the presence of confounding by indication. Subjects who are aware of their low bone status might have undergone lifestyle changes or were advised to take vitamin D/calcium supplements and/or anti-osteoporotic drugs to counteract a further deterioration of bone status. This hypothesis is in accordance with a recent study showing that osteoporosis diagnosis positively predicted the use of calcium and vitamin D supplements in ≥ 40 years old subjects (46). Nevertheless, the results of the present study remained essentially unchanged when subjects reporting conditions which may have influenced bone, 25(OH)D3 or iPTH status were excluded from the analyses.
Several studies showed a positive association between 25(OH)D and BMD measured by DXA (8–10, 13), whereas other studies failed to demonstrate an independent relationship (2–5). Likewise, some (2, 10), but not all (12), studies reported an inverse association between PTH and BMD. QUS measurements have shown a good overall agreement with DXA measurements in participants of the GISELA study (40) and in other study populations (47). Nevertheless, studies that have simultaneously investigated the associations of 25(OH)D with BMD by DXA and QUS often reported different results for DXA and QUS (7, 11, 13). One can speculate that BMD and bone structure/quality might not be equally affected by vitamin D, but the findings on the associations between 25(OH) D and QUS parameters are also inconsistent. Some studies showed significant positive associations (6, 13); others could not confirm independent associations (7, 14, 15). The situation is similarly controversial for the associations of 25(OH)D and PTH with bone turnover markers. For instance, 25(OH) D was negatively associated with P1NP in a study of early postmenopausal women (8). In a study with postmenopausal women aged 50–80 years, 25(OH)D showed no associations with P1NP or bone ALP, whereas PTH was slightly positively correlated with bone ALP, but not with P1NP (4). P1NP was not associated with 25(OH)D in some studies with middleaged and older men, but showed a positive association with PTH (13, 48). In a study with 1107 men and 832 women aged 25–79 years, PTH was not associated with P1NP or bone ALP (45). Nevertheless, for osteoporotic subjects, higher P1NP concentrations were frequently reported (3, 22, 48), and it has been suggested that higher concentrations of bone formation markers indicate an increased bone remodelling caused by elevated PTH concentrations (48).
In general, the inconsistent findings in literature as regards the associations of 25(OH)D and PTH with bone status might be explained by discrepancies in study designs, methods, considered covariables and participants characteristics, such as age range, postmenopausal status, health status, body composition as well as 25(OH)D and PTH status. There is evidence that bone-related effects of 25(OH)D and PTH may differ depending on the skeletal site (1, 9–11, 13). Furthermore, it has been suggested that the detrimental effect of vitamin D deficiency on BMD is mediated by reduced lean mass and/or elevated PTH levels in elderly subjects (1, 2). In the present study, 25(OH)D3 was not significantly associated with QUS parameters neither before nor after adjusting for fat-free mass and iPTH, whereas inverse associations with bone formation markers were found. However, the association between 25(OH)D3 and ALP may rely on the presence of relatively high iPTH levels, as revealed by the stratified analysis. Apart from that, it has been hypothesised that the inconsistent study findings may result from the non-linear nature of the association, such that the impact of 25(OH)D on bone status may be more pronounced in vitamin D-deficient subjects (4, 11). We are not aware of a previous study analysing the associations of both 25(OH)D3 and iPTH concentrations with QUS parameters and bone formation markers stratified by vitamin D and iPTH status. In the present study, 25(OH)D3 was negatively associated with ALP and non-significantly positively associated with QUS parameters in subjects with 25(OH)D3 concentrations below and iPTH concentrations above the median concentration, respectively. Because we used the median concentrations as stratification criteria, we cannot rule out that the potential inflection points at which the associations of 25(OH)D3 and iPTH with bone status parameters may reach a plateau are below or above 62.8 nmol/L and 4.6 pmol/L, respectively. However, in a previous study with elderly subjects, a concentration of 65 nmol/L was found to present the point at which the association between 25(OH)D and BUA reaches a plateau (11). This value approximates the median 25(OH)D3 concentration of the present cohort.
An unsolved problem is the determination of evidence-based cut-off values to classify the vitamin D status as sufficient and insufficient. The relationship between insufficient 25(OH) D concentrations and bone formation markers with regard to bone health should be further explored. In addition, the question whether 25(OH)D has substantial effects on bones independent of the interaction with PTH warrants further investigations.
Strengths and limitations
Besides the limited generalisability of the results, other limitations have to be considered when interpreting the findings. Given the cross-sectional nature of this study, cause and effect cannot be determined and confounding by indication cannot be ruled out. While P1NP is a specific bone formation marker, total ALP reflects not only bone formation but also liver function (28). Therefore, the results have to be interpreted with caution, although subjects with reported liver diseases were excluded. We have no information about bone resorption markers. Because we used calcaneal QUS measurements, extrapolation of our results to other skeletal sites or measurement systems should be undertaken with caution. Data on lifestyle factors, disease history and nutrient intake based on self-report and we could not discriminate between weight-bearing and non-weight-bearing activities. Finally, the power could have been insufficient to detect significant associations with QUS parameters in this homogenous cohort given the limited sample size.
The present study has several strengths. Blood samples were collected in fasting state in the morning hours from July to September to minimise biological variability. Further strengths are the combined examination of 25(OH)D3, iPTH, QUS parameters and bone formation markers, the stratified analyses, the sensitivity analysis and the consideration of potential confounding factors.
Conclusion
The present study indicates no associations of 25(OH)D3 and iPTH with calcaneal bone characteristics in elderly subjects with 25(OH)D3 concentrations between 30 and 107 nmol/L and mainly non-pathological iPTH concentrations. However, despite the absence of 25(OH)D3 concentrations below 30 nmol/L, negative associations between 25(OH)D3 and bone formation markers may be present, particularly in women. The results of the analyses stratified by median vitamin D and iPTH status indicate that associations of 25(OH)D3 with bone status parameters are predominantly evident in subjects with 25(OH)D3 levels ≤ 62.8 nmol/L and iPTH levels ≥ 4.6 pmol/L. Consequently, these results imply that 25(OH)D concentrations > 62.8 nmol/L do not provide further benefit with regard to bone health. Overall, sex and baseline concentrations of both 25(OH)D and PTH should be considered when investigating effects of vitamin D and PTH on bones and before taking a decision on intervention measures for improving bone health.
Acknowledgements: The authors thank all participants in the GISELA study as well as the staff of the Department of Human Nutrition who helped in the data acquisition
Conflict of interest: The authors have no conflicts of interest to declare.
Funding: This investigation received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Authors’ contributions: AJ and MNB formulated the research question. AJ performed the statistical analysis, interpreted the data and wrote the manuscript. MNB had primary responsibility of the study, designed the study and critically proofread the manuscript. Both authors read and approved the final manuscript.
Abbreviations
- 25(OH)D:
-
25-hydroxyvitamin D
- 25(OH)D3 :
-
25-hydroxycholecalciferol
- ALP:
-
alkaline phosphatase
- B:
-
non-standardised coefficient beta
- ß:
-
standardised coefficient beta
- BMD:
-
bone mineral density
- BMI:
-
body mass index
- BUA:
-
broadband ultrasound attenuation
- DXA:
-
dual-energy X-ray absorptiometry
- ECLIA:
-
electrochemiluminescence immunoassay
- eGFR:
-
estimated glomerular filtration rate
- FSH:
-
follicle stimulating hormone
- GISELA:
-
longitudinal study on nutrition and health status of senior citizens in Giessen
- HRT:
-
hormone replacement therapy
- iPTH:
-
intact parathyroid hormone
- LH:
-
luteinising hormone
- P1NP:
-
N-terminal propeptide of type 1 collagen
- QUS:
-
quantitative ultrasound
- R²:
-
adjusted coefficient of determination
- SOS:
-
speed of sound
- SI:
-
stiffness index
- TSH:
-
thyroid stimulating hormone
References
Arabi A, Baddoura R, Awada H, Salamoun M, Ayoub G, El-Hajj Fuleihan G. Hypovitaminosis D osteopathy: is it mediated through PTH, lean mass, or is it a direct effect? Bone 2006;39: 268–75.
Arabi A, Baddoura R, El-Rassi R, El-Hajj Fuleihan G. PTH level but not 25 (OH) vitamin D level predicts bone loss rates in the elderly. Osteoporos Int 2012;23:971–80.
Bhattoa HP, Nagy E, More C, Kappelmayer J, Balogh A, Kalina E, Antal-Szalmas P. Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age: the HunMen Study. Osteoporos Int 2013;24: 179–86.
Garnero P, Munoz F, Sornay-Rendu E, Delmas PD. Associations of vitamin D status with bone mineral density, bone turnover, bone loss and fracture risk in healthy postmenopausal women. The OFELY study. Bone 2007;40: 716–22.
Ilich JZ, Brownbill RA, Tamborini L. Bone and nutrition in elderly women: protein, energy, and calcium as main determinants of bone mineral density. Eur J Clin Nutr 2003;57: 554–65.
Kauppi M, Impivaara O, Mäki J, Heliövaara M, Marniemi J, Montonen J, Jula A. Vitamin D status and common risk factors for bone fragility as determinants of quantitative ultrasound variables in a nationally representative population sample. Bone 2009;45: 119–24.
Kuchuk NO, Pluijm SM, van Schoor NM, Looman CW, Smit JH, Lips P. Relationships of serum 25-hydroxyvitamin D to bone mineral density and serum parathyroid hormone and markers of bone turnover in older persons. J Clin Endocrinol Metab 2009;94: 1244–50.
Macdonald HM, Mavroeidi A, Barr RJ, Black AJ, Fraser WD, Reid DM. Vitamin D status in postmenopausal women living at higher latitudes in the UK in relation to bone health, overweight, sunlight exposure and dietary vitamin D. Bone 2008;42: 996–1003.
Olmos JM, Hernández JL, García-Velasco P, Martínez J, Llorca J, González-Macías J. Serum 25-hydroxyvitamin D, parathyroid hormone, calcium intake, and bone mineral density in Spanish adults. Osteoporos Int 2016;27: 105–13.
Saquib N, von Mühlen D, Garland CF, Barrett-Connor E. Serum 25-hydroxyvitamin D, parathyroid hormone, and bone mineral density in men: the Rancho Bernardo study. Osteoporos Int 2006;17: 1734–41.
Sohl E, de Jongh RT, Swart KM, Enneman AW, van Wijngaarden JP, van Dijk SC, Ham AC, van der Zwaluw NL, Brouwer-Brolsma EM, van der Velde N, de Groot CP, te Velde SJ, Lips P, van Schoor NM. The association between vitamin D status and parameters for bone density and quality is modified by body mass index. Calcif Tissue Int 2015;96: 113–22.
van Ballegooijen AJ, Robinson-Cohen C, Katz R, Criqui M, Budoff M, Li D, Siscovick D, Hoofnagle A, Shea SJ, Burke G, de Boer IH, Kestenbaum B. Vitamin D metabolites and bone mineral density: the multi-ethnic study of atherosclerosis. Bone 2015;78: 186–93.
Vanderschueren D, Pye SR, O’Neill TW, Lee DM, Jans I, Billen J, Gielen E, Laurent M, Claessens F, Adams JE, Ward KA, Bartfai G, Casanueva FF, Finn JD, Forti G, Giwercman A, Han TS, Huhtaniemi IT, Kula K, Lean ME, Pendleton N, Punab M, Wu FC, Boonen S. Active vitamin D (1,25-dihydroxyvitamin D) and bone health in middle-aged and elderly men: the European Male Aging Study (EMAS). J Clin Endocrinol Metab 2013;98: 995–1005.
Zhen D, Liu L, Guan C, Zhao N, Tang X. High prevalence of vitamin D deficiency among middle-aged and elderly individuals in northwestern China: its relationship to osteoporosis and lifestyle factors. Bone 2015;71: 1–6.
Zochling J, Sitoh YY, Lau TC, Cameron ID, Cumming RG, Lord SR, Schwarz J, Trube A, March LM, Sambrook PN. Quantitative ultrasound of the calcaneus and falls risk in the institutionalized elderly: sex differences and relationship to vitamin D status. Osteoporos Int 2002;13: 882–7.
Avenell A, Mak JC, O’Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev 2014;4:CD000227.
Rizzoli R, Boonen S, Brandi ML, Bruyère O, Cooper C, Kanis JA, Kaufman JM, Ringe JD, Weryha G, Reginster JY. Vitamin D supplementation in elderly or postmenopausal women: a 2013 update of the 2008 recommendations from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Curr Med Res Opin 2013;29: 305–13.
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 2011;96: 53–8.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2011;96: 1911–30.
Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet 2002;359: 1929–36.
Blanchet C, Giguère Y, Prud’homme D, Turcot-Lemay L, Dumont M, Leduc G, Côte S, Laflamme N, Rousseau F, Dodin S. Leisure physical activity is associated with quantitative ultrasound measurements independently of bone mineral density in postmenopausal women. Calcif Tissue Int 2003;73: 339–49.
Martínez J, Olmos JM, Hernández JL, Pinedo G, Llorca J, Obregón E, Valero C, González-Macías J. Bone turnover markers in Spanish postmenopausal women: the Camargo cohort study. Clin Chim Acta 2009;409: 70–4.
Khosla S. Pathogenesis of age-related bone loss in humans. J Gerontol A Biol Sci Med Sci 2013;68: 1226–35.
Jungert A, Neuhäuser-Berthold M. Sex-specific determinants of serum 25-hydroxyvitamin D3 concentrations in an elderly German cohort: a cross-sectional study. Nutr Metab (Lond) 2015;12:2.
Alcaraz A, González-López R, Morote J, de la Piedra C, Meseguer C, Esteban E, Climent M, González-Gragera B, Alvarez-Ossorio JL, Chirivella I, et al. Biochemical markers of bone turnover and clinical outcome in patients with renal cell and bladder carcinoma with bone metastases following treatment with zoledronic acid: The TUGAMO study. Br J Cancer 2013;109: 121–30.
Dusso A, González EA, Martin KJ. Vitamin D in chronic kidney disease. Best Pract Res Clin Endocrinol Metab 2011;25: 647–55.
Vasikaran SD, Chubb SP, Ebeling PR, Jenkins N, Jones GR, Kotowicz MA, Morris HA, Schneider HG, Seibel MJ, Ward G. Harmonised Australian reference intervals for serum PINP and CTX in adults. Clin Biochem Rev 2014;35: 237–42.
Woitge HW, Seibel MJ, Ziegler R. Comparison of total and bone-specific alkaline phosphatase in patients with nonskeletal disorder or metabolic bone diseases. Clin Chem 1996;42: 1796–804.
Roche Diagnostics GmbH. Elecsys 1010/2010/Modular analytics E170. Parathyroid hormone PTH, intact. Mannheim, Germany: Roche Diagnostics; 2003.
Roche Diagnostics GmbH. Elecsys 1010/2010 and Modular analytics E170, Cortisol. Mannheim, Germany: Roche Diagnostics; 2005.
Roche Diagnostics GmbH. Elecsys and cobas analyzer. 25-Hydroxyvitamin D3, Vitamin D3 (25-OH). Mannheim, Germany: Roche Diagnostics; 2007.
Roche Diagnostics GmbH. Elecsys and cobas e analyzers. Thyrotropin, TSH. Mannheim, Germany: Roche Diagnostics; 2007.
Roche Diagnostics GmbH. Elecsys and cobas e analyzers. Total procollagen type 1 amino-terminal propeptide, total P1NP. Mannheim, Germany: Roche Diagnostics; 2007.
Roche Diagnostics GmbH. Roche/Hitachi. Alkalische Phosphatase flüssig nach IFCC (alkaline phosphatase), ALP. Mannheim, Germany: Roche Diagnostics; 2008.
Roche Diagnostics GmbH. Elecsys 1010/2010/Modular analytics E170. Follikelstimulierendes Hormon (follicle stimulating hormone), FSH. Mannheim, Germany: Roche Diagnostics; 2004.
Roche Diagnostics GmbH. Elecsys 1010/2010/Modular analytics E170. Testosterone. Mannheim, Germany: Roche Diagnostics; 2004.
Roche Diagnostics GmbH. Elecsys 1010/2010 and Modular analytics E170. Estradiol -E2. Mannheim, Germany: Roche Diagnostics; 2005.
Roche Diagnostics GmbH. Elecsys 1010/2010 and Modular analytics E170. Luteinizing hormone, LH. Mannheim, Germany: Roche Diagnostics; 2005.
Levey AS, Greene T, Kusek J, Beck G. A simplified equation to predict glomerular filtration rate from serum creatinine (abstract). J Am Soc Nephrol 2000;11:155A.
Edelmann-Schäfer B, Berthold LD, Stracke H, Lührmann PM, Neuhäuser-Berthold M. Identifying elderly women with osteoporosis by spinal dual X-ray absorptiometry, calcaneal quantitative ultrasound and spinal quantitative computed tomography: a comparative study. Ultrasound Med Biol 2011;37: 29–36.
Njeh CF, Blake GM. Calcaneal quantitative ultrasound devices: water coupled. In: Njeh CF, Hans D, Fuerst T, Glüer CC, Genant HK, (eds). Quantitative ultrasound. Assessment of osteoporosis and bone status. London: Martin Dunitz;1999. pp. 109–24.
Roubenoff R, Baumgartner RN, Harris TB, Dallal GE, Hannan MT, Economos CD, Stauber PM, Wilson PW, Kiel DP. Application of bioelectrical impedance analysis to elderly populations. J Gerontol A Biol Sci Med Sci 1997;52:M129–36.
Krems C, Lührmann PM, Neuhäuser-Berthold M. Physical activity in young and elderly subjects. J Sports Med Phys Fitness 2004;44: 71–6.
Lührmann PM, Herbert BM, Gaster C, Neuhäuser-Berthold M. Validation of a self-administered 3-day estimated dietary record for use in the elderly. Eur J Nutr 1999;38: 235–40.
Michelsen J, Wallaschofski H, Friedrich N, Spielhagen C, Rettig R, Ittermann T, Nauck M, Hannemann A. Reference intervals for serum concentrations of three bone turnover markers for men and women. Bone 2013;57: 399–404.
Lee S, Teschemaker AR, Daniel M, Maneno MK, Johnson AA, Wutoh AK, Lee E. Calcium and vitamin D use among older adults in U.S.: results from national survey. J Nutr Health Aging 2016;20: 300–5.
Trimpou P, Bosaeus I, Bengtsson BA, Landin-Wilhelmsen K. High correlation between quantitative ultrasound and DXA during 7 years of follow-up. Eur J Radiol 2010;73: 360–4.
Olmos JM, Hernández JL, Martínez J, Pariente E, Llorca J, González-Macías J. Bone turnover markers in Spanish adult men The Camargo Cohort Study. Clin Chim Acta 2010;411: 1511–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jungert, A., Neuhäuser-Berthold, M. No associations of 25-hydroxycholecalciferol and parathyroid hormone concentrations with calcaneal bone characteristics in community-dwelling elderly subjects: A cross-sectional study. J Nutr Health Aging 21, 733–742 (2017). https://doi.org/10.1007/s12603-016-0785-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0785-z