Abstract
Alzheimer’s disease (AD) is an irreversible neurological disorder that progresses gradually and can cause severe cognitive and behavioral impairments. This disease is currently considered a social and economic incurable issue due to its complicated and multifactorial characteristics. Despite decades of extensive research, we still lack definitive AD diagnostic and effective therapeutic tools. Consequently, one of the most challenging subjects in modern medicine is the need for the development of new strategies for the treatment of AD. A large body of evidence indicates that amyloid-β (Aβ) peptide fibrillation plays a key role in the onset and progression of AD. Recent studies have reported that amyloid hypothesis–based treatments can be developed as a new approach to overcome the limitations and challenges associated with conventional AD therapeutics. In this review, we will provide a comprehensive view of the challenges in AD therapy and pathophysiology. We also discuss currently known compounds that can inhibit amyloid-β (Aβ) aggregation and their potential role in advancing current AD treatments. We have specifically focused on Aβ aggregation inhibitors including metal chelators, nanostructures, organic molecules, peptides (or peptide mimics), and antibodies. To date, these molecules have been the subject of numerous in vitro and in vivo assays as well as molecular dynamics simulations to explore their mechanism of action and the fundamental structural groups involved in Aβ aggregation. Ultimately, the aim of these studies (and current review) is to achieve a rational design for effective therapeutic agents for AD treatment and diagnostics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer disease (AD) is the most common neurodegenerative condition and behavioral impairment, which in 1907, Alois Alzheimer first diagnosed AD in a German woman (Graeber et al. 1997). AD is considered an age-dependent disease affecting people of 65, 80, and 90 years of age with approximately 5%, 20%, and 33% levels of incidence respectively (Hajipour et al. 2017). Based on data from the Center for Disease Control and Prevention in the USA, AD is the fifth greatest cause of mortality for those aged 65 years and older. While deaths from stroke, human immunodeficiency virus (HIV), and heart disease have reduced in number over the 2000–2013 period by 23%, 40%, and 14%, respectively, deaths from AD increased by 71% over the same period. In 2015, the prevalence of AD was estimated around 46.8 million people worldwide, from which 43% need a high level of care (such as a home nurse) with an estimated caring burden of about 236 billion dollars for people age ≥ 65 years with dementia (Alzheimer’s Association 2016). It is expected that this number will surge to more than 131.5 million people worldwide by 2050 (Prince et al. 2016).
In the early stages of the disease, AD is diagnosed with an impairment in short-term memory, which gradually progresses and presents as other neurological changes and behavioral disorders (McKhann et al. 1984, Ahmad Fazili et al., 2015). The elderly population is growing worldwide, and there is currently no cure for AD. Medical advances are urgently required for the early diagnosis, prevention, and treatment for AD.
AD is likely to become one of the major healthcare and economic challenges in the world in an early future (Sloane et al. 2002; Wimo et al. 2013). The limited success of nearly all therapeutic agents on the course of the development AD has created great concern for researchers. This has led to the search for improved diagnostic and therapeutic agents to overcome such obstacles.
Pathophysiology
Death of neurons and synaptic damages the brain regions including the hippocampus, cortex, and ventral striatum which are the main neuropathological properties of AD. This pathology is responsible for brain atrophy and subsequent display of the cognitive symptoms of AD (Selkoe 2001). Brain atrophy associated with narrowed gyri, enlarged ventricles, and sulci can be observed in radiological tests of AD-affected brains (Rossor et al. 2000). However, these hallmarks are not specific to AD and may be detected in other dementia disorders. Nevertheless, the extracellular amyloid plaques, intracellular neurofibrillary tangles (NFTs), and vascular amyloid deposits are likely to reveal on postmortem AD brain at histological examination (Jaruszewski et al. 2012). In particular, extracellular amyloid-β plaques, formed by amyloid-β peptide (Aβ) aggregation, can be a unique histopathologic feature of this disease (Mandelkow and Mandelkow 1998).
The many risk factors involved in AD pathogenesis can be classified into two major categories, genetic and nongenetic. Both genetic and nongenetic factors play a major role in the causation and progression of AD. It is estimated that approximately 1% or less of Alzheimer’s cases are reported because of the mutation in three specific genes (Bekris et al. 2010). These mutations influence the gene encoding the amyloid precursor protein (APP) on chromosome 21, and the gene encoding presenilin 1 (PS-1) protein on chromosome 14 and the gene encoding presenilin 2 (PS-2) protein on the chromosome (Sahni et al. 2011). Mutations in these genes lead to familial forms of AD.
People with Down syndrome are at high risk of AD. This is likely due to those with Down syndrome possessing an additional full or partial copy of chromosome 21 which contains the gene that encodes APP (Lott and Dierssen 2010). The APOE-e4 allele type is another genetic factor correlating with AD. Factors such as age, family history, diabetes, obesity, smoking, cardiovascular disease, and education have been described as the nongenetic abnormalities. The apolipoprotein E protein (ApoE) transports triglycerides, lipoproteins, and phospholipids in blood circulation and are also believed to play a key role in nerve regeneration and synaptic remodeling (Ignatius et al. 1986). The ApoE gene on chromosome 19 in humans has three major isoforms E2, E3, and E4 (Emi et al. 1988). People with the Apo ε4 polymorphism of ApoE gene are at higher risk and typically present with an earlier start of AD disease than those without the ε4 allele (Corder et al. 1993). APOE4 can behave like a pathological chaperone for Aβ peptide and can both significantly enhance Aβ deposition and diminish clearance of Aβ. However, the small ε2 allele may be protective against AD (Corder et al. 1994).
In general, two main hypotheses have been proposed to describe the etiology and pathophysiology observed in AD. The first, known as the amyloid cascade hypothesis, depends on an amyloid cascade that stimulates neurofibrillary tangle formation, with both playing a prominent role in the neurodegeneration processes. According to this hypothesis, AD advances via enzymatic cleavage of APP leading to overproduction, clearance failure, aggregation, and ultimately fibrillation of amyloid-β peptide (Aβ) with amyloid plaque formation. These conditions are related to inflammation and cell death, which is reflected in memory damage and behavioral impairment (Fig. 1) (Hardy and Selkoe 2002; Finder and Glockshuber 2007).
The pathway of amyloid-β fibrillation formation and cellular damage. Amyloid precursor protein (APP) is cleaved by proteolytic enzymes of β- and γ-secretases, respectively, and a 39–42 amino acid peptide fragment is produced regarding with cleavage position. Unfolded Aβ monomers self-assembly into soluble toxic oligomers and insoluble fibrils lead to neural death, synaptic dysfunction, and memory impairment
Mutation in APP and presenilin (PS) genes leads to an increase in Aβ senile plaques in these patients (Mattson 2004). Therefore, according to the proposed mechanism, probably, Aβ deposition can be the first pathological event that occurs years before the appearance of clinical symptoms in the brain. The intracellular neurofibrillary tangles are the driving forces in the progression towards detectable clinical symptoms (Knopman 2016; Reiman 2016).
The Aβ protein is produced in the brain and the peripheral tissues. APP is a large single-transmembrane glycoprotein that includes a large extracellular domain (590–680 amino acids) and cytoplasmic end of 55 amino acids which plays a role in intracellular trafficking. When the APP is cleaved through proteolytic processing by enzymes of β- and γ-secretases, respectively, a 39–42 amino acid protein fragment is derived from APP cleavage position (Haass and Selkoe 1993). Aβ40 accounts for approximately 90% from total formed Aβ peptide while Aβ42 approximately 10%. It has been reported that Aβ levels in the brain tissue, CSF, and plasma of a healthy individual are in equilibrium reflecting this 90:10 ratio, which is disturbed during AD progression (Fig. 2).
The distribution and degradation pathway of Aβ peptide monomer between brain and blood circulation. BBB can regulate Aβ levels in the plasma and brain parts through the receptor for advanced glycation end products (RAGE) and low-density lipoprotein receptor-related protein 1 (LRP1) receptor that transports Aβ proteins to abluminal and luminal directions, respectively. Aβ proteins in the brain parenchyma may come together as amyloid plaques in cerebrovascular and parenchymal parts or degraded via various protease enzymes such as insulin-degrading enzyme (IDE), neprilysin (NEP), and angiotensin-converting enzyme (ACE) in liver
In addition, it is believed that the blood-brain barrier (BBB) can help to regulate Aβ levels in the plasma and brain through the action of the receptor for advanced glycation end products (RAGE) and low-density lipoprotein receptor–related protein 1 (LRP1) receptor. LRP1 transports Aβ proteins in the abluminal and luminal direction respectively (Deane et al. 2003; Giedraitis et al. 2007; Deane et al. 2009). Aβ proteins in the brain parenchyma may form into fibrils or be degraded via various protease enzymes such as insulin-degrading enzyme (IDE), neprilysin (NEP), and angiotensin-converting enzyme (ACE).
In the AD brain, plaques can be made from several different peptides, but their cores are composed primarily of amyloid-β peptides. Due to the existence of two hydrophobic residues in the C-terminal of Aβ42 rather than Aβ40, Aβ shows a higher tendency to misfolding and self-aggregation as well as more cell cytotoxicity than Aβ40 protein. For this reason, Aβ42 peptide forms the prominent segment of neuritic plaques in AD brain, while Aβ40 peptide is later deposited (Wisniewski and Wegiel 1995). The concentrations of both of these peptides are decreased in CSF assays of AD patients providing indirect confirmation of the presence of amyloid plaque formation (Tamaoka et al. 1997). The Aβ peptides have various aggregation forms including low molecular weight oligomers, protofibrils, and mature fibrils that eventually come together as parenchymal plaques or cerebrovascular amyloid deposits. Recent research indicates that soluble low molecular weight Aβ aggregates are more toxic to neurons and the BBB endothelial cells and are correlated with greater loss of cognitive function than the insoluble amyloid plaque burden (Glabe 2005; Walsh and Selkoe 2007; Hall and Edskes 2009; Hall and Edskes 2012).
Tau protein is a neuronal protein, mostly expressed in axons of neuronal cells; binds to microtubules; and improves their stability. The hyperphosphorylated (P-tau) form is one of the main components in Alzheimer’s neurofibrillary tangles. It is reported that P-tau cannot effectively interact with microtubules, leading to cellular dysfunction and death. It is also reported that Ptau levels in cerebrospinal fluid (CSF) raise are not only elevated in AD but also in other neurodegenerative disorders such as Creutzfeldt–Jakob, depression, and Parkinson’s disease. Therefore, neurofibrillary tangles are not specific to AD, and because of their location inside cells, their presence is difficult to be directly compared with production and aggregation of the Aβ peptide (Larbanoix et al. 2011).
The second hypothesis concerns the cholinergic system deficiency. Based on the hypothesis of the cholinergic pathway, the cholinergic neurons dysfunction is adequate to create animal models with a memory impairment similar to AD (Bartus and Emerich 1999). The obtained results of Rossor et al. (1980) and Henke and Lang (1983) studies demonstrated that there is a marked degeneration in cholinergic neurons and cholinergic markers in the brains of AD patients. Additionally, both AChE levels and choline acetyltransferase (ChAT) efficacy were decreased in the cortex of AD patients (Rossor et al. 1980; Henke and Lang 1983).
In another study, Soininen et al. (1995) reported AD patients possessing the APOE-ε4 allele to have a severe defect in cholinergic systems in comparison with those of without the APOE-ε4 allele. An effective cure for AD is not yet a reality, and approved drugs for treatment of the cognitive and behavioral impairments in AD are based on neurotransmitter or enzyme modulation that can only improve symptoms (Sood et al. 2014). Acetylcholinesterase (AChE) inhibitors such as tacrine, donepezil, rivastigmine, and galantamine are currently being utilized to reduce the rate of AD progression (Han et al. 2015).
Due to their unfavorable pharmacokinetics and pharmacodynamics properties, there are several limitations associated with therapy such as dizziness, confusion, and adverse gastrointestinal effects (such as nausea, constipation, and vomiting) that most usually result in the defeat of therapy (Mehta et al. 2012; Colovic et al. 2013). In recent years, a significant volume of research has been focused on achieving a better understanding of AD pathogenesis and development of a new class of therapeutic strategies that could stop disease progress by targeting special pathophysiological mechanisms in the AD process.
Amyloid hypothesis summary
Although the pathogenesis of AD is not yet entirely understood, among the reported biological pathways, the amyloid cascade hypothesis has developed as the dominant theory to explain the etiology and the fundamental focus on neurodegenerative studies. As a consequence, many scientists are currently investigating therapeutic strategies targeting the molecular mechanisms of the processes of production, aggregation, and clearance of Aβ. Based on this hypothesis, Aβ monomers self-assemble into soluble toxic oligomers and insoluble fibrils, leading to neural death, synaptic dysfunction, and memory impairment. Although Aβ hypothesis-related therapy strategies are more developed than other strategies, there have been to date no demonstrated clinical benefits by them.
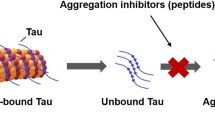
It is believed that low molecular weight oligomers of Aβ proteins can be more toxic to neurons and BBB endothelial cells than the monomers or large fibrils (Hall and Edskes 2009; Laganowsky et al. 2012). Therefore, there are strategies to prevent or reduce Aβ aggregation that include either metal chelators or β-sheet breakers based on nanotechnology, organic molecules, or peptides/antibodies (Figs. 3 and 4).
Sigmoid kinetics diagram of Aβ peptide fibrillation formation including lag, elongation, and saturation phase. a β fibril formation is a self-assembly process which depends on nucleation, which has three phases including lag phase (critical oligomer cores formation), elongation phase (oligomers polymerization), and fibril saturation phase. b Kinetic profiles of Aβ42 aggregation alone and in the presence of CyD6IOX (conjugated cyclodextrin to quinoline derivative, Oliveri et al. 2017). c TEM image of Aβ40 fibrils. d Inhibition of Aβ40-fibril growth in the presence SLOH (carbazole-based fluorophores, Yang et al. 2012)
a Schematic illustration of the structure of the Aβ fibril. b Behavioral test for memory impairment in AD model and treated with 1.0 mg/mL (low dose) and 1.5 mg/mL (high dose) with PtII-PW11; latency for escape to platform in the training phase, number of crossing platform time in probe test and percentage (%) of time spent in the target quadrant in probe test. c Immunofluorescence images for senile plaques (Aβ42 deposition) in the hippocampus (HIP) of WT, AD, and treated with PtII-PW11 (organoplatinum-substituted polyoxometalate, Liu et al., 2019a, b, c)
Different strategies for Aβ fibrillation inhibition have been designed and proposed in vitro, but experimental investigations alone are not adequate for having a clear understanding of the subject. Also, the mechanism of molecular interaction between inhibitors and the Aβ peptides is often unknown. Therefore, in order to improve and develop new inhibitor compounds, it is necessary that the field should acquire sufficient knowledge about interactions at the molecular and atomic levels. Moreover, computational methods, like molecular docking and molecular dynamics simulations, are an essential supplement to experimental studies and have provided novel viewpoints in many fields. Furthermore, these techniques have been widely applied for the design of Aβ aggregation inhibitors on the conformational transitions, metal chelation, and aggregation formation (Bruce et al. 2010; Lemkul and Bevan 2012; Rao et al. 2015).
Metal chelators
Metal ions have a vital role in the process of production and clearance of Aβ peptide through the regulation of the activity of enzymes involved in this process (Sastre et al. 2015). They are considered an important factor in determining neuronal function and AD progression. Although the exact mechanism of metal ion interactions with Aβ peptide is not still clear, a preponderance of evidence indicates that these ions can attach with high affinity to N-terminal residues of Aβ peptide, such as His6, His13, and His14 imidazole, as well as the Asp1 and Ala2 carbonyl groups (Schöneich and Williams 2002).
It is believed that heavy metal ions like copper, iron, manganese, zinc, and aluminum (especially copper) can stimulate both Aβ aggregation and fibril formation as well as accelerate oxidative stress by generating neurotoxic reactive oxygen species (ROS) containing oxygen free radicals and hydrogen peroxide (H2O2), thereby causing synaptic dysfunction (Singer et al. 2005). In addition, it was reported that Cu2+ ions exhibit a higher catalyzing effect at slightly acidic condition (< pH 6.8) on Aβ aggregation compared with Zn2+ ions at physiological pH (Atwood et al. 1998; Pedersen et al. 2015).
Chelation therapy has been suggested as a possible treatment method for AD due to its ability to absorb and reduce the concentration of available metal ions in the brain. However, their application may be associated with challenges like low CNS bioavailability and notable systemic toxicity. In addition, metal ion chelators can inhibit the interaction of Aβ peptide with the lipid membrane—a process known to influence Aβ peptide aggregation (Mandel et al. 2007).
Many metal chelators such as ethylenediaminetetraacetic acid (EDTA) (Casdorph 1981; Chauhan and Siegel 2007), diethylenetriaminepentaacetic acid (DTPA), desferrioxamine (Atwood et al. 2000; Liu et al. 2006), and clioquinol have been considered agents for inhibition of Cu2+-mediated Aβ aggregation in vitro (Table 1). Among these traditional metal chelators, only a few agents, such as clioquinol (CQ) (Ritchie et al. 2003) and 25,7-dichloro-2-((dimethylamino) methyl) 8-quinolinol (PBT2) (a 8-hydroxyquinoline derivative), have been evaluated in murine AD models and AD human patients (Adlard et al. 2008). The result revealed that they have significant inhibitor activity and they have currently passed phase II clinical trials (Crouch and Barnham 2012). However, it is likely that the potential side effects of these metal chelators may prevent their public clinical use.
Cherny et al. reported modified polymeric nanoparticles with d-penicillamine via a disulfide bond as a copper chelator (Cherny et al. 2001; Cui et al. 2005). The resulting nanoparticles displayed a good ability to disaggregate Aβ plaques in vitro. In another study, an ultra-thin structure of graphite-phase carbon nitride (g-C3N4) was described as a nanochelator able to prevent Aβ40 fibrillation (Li et al. 2016). This nanostructure could specifically bind to Cu2+ ions, thereby inhibiting fibrillation and causing depolymerization of the deposited Aβ40 aggregates in conjugation with Cu2+ ions. Sun et al. attached iminodiacetic acid (IDA) to the human lysozyme (h-Lys)–coated surface of polymeric-based nanoparticles and demonstrated a strong binding affinity to Zn2+ ions (Liu et al. 2017a; Li et al. 2018). This nanochelator can inhibit Aβ40 fibrillation, rapidly destabilizing Zn2+-associated Aβ aggregates and modulating the resulting cytotoxicity.
In 2019, Liu and colleagues developed a potent multifunctional inhibitor of Cu2+-mediated Aβ aggregation based on the d-enantiomeric RTHLVFFARK-NH2 decapeptide a peptide sequence shown to act as a high-affinity chelator to Cu2+ ions (Meng et al. 2018; Liu et al. 2019b). In the same study, they showed that the d-enantiomer peptide had an inhibitory effect on Aβ40 fibrillogenesis and significantly decreased the cytotoxicity caused by Aβ42-Cu2+ complexes in comparison to that showed by using its l-enantiomeric analog. In a similar study, the in vivo pharmacodynamics effects of a bifunctional inhibitor peptide GR (GGHRYYAAFFARR) were investigated on the basis of its dual ability to act both as a chelator of Cu ions and a β-sheet breaker able to reduce ROS toxicity and inhibit Aβ40 fibrils, respectively (Zhang et al. 2016; Wang et al. 2018). The in vivo results indicated that the GR peptide could improve damaged spatial memory and reduce the number of senile plaques within the brain of AD model rats. Recently, in our research group, a new multifunctional peptide LPFFDGNSM for metal chelation and Aβ42 inhibition was designed based on the iAβ5 peptide lead compound (Shamloo et al. 2018). Subsequently, its chemical inhibitory mechanism involving Zn2+ and Cd2+ ions was evaluated using MD simulation techniques. The findings indicated that these ions interact with six druggable regions with considerable affinities on the Aβ42 peptide. According to the conducted free energy analysis, the ions showed higher affinity to the LPFFDGNSM sequence rather than the Aβ42 peptide. In fact, the formation of the reported LPFFDGNSM-ion conjugates is easier and more spontaneous than the presented Aβ-ion+ ones.
β-Sheet breakers
The structure of the Aβ42 fibril was first experimentally resolved by Lührs et al. (2005) (Fig. 4a). This structure provides important information about the identification of interacting regions, which might be targeted by inhibitor compounds (Lührs et al. 2005). There are at least four important sites with specific structural properties which either promote interaction or destabilize Aβ self-assembly: (a) hydrophilic region formed by electrostatic interaction between Asp23-Lys28; (b) Glu22 ladder formed between Glu22 residue side chains of adjacent β-sheets; (c) central cleft in the interior of the U-shaped turn; and (d) hydrophobic regions by Leu17-Ala21 and Ala30-Val36 residues of the N- and C-terminal β-strands, respectively.
The salt-bridge formed between Asp23 and Lys28 residues has a vital role in stabilizing the β-sheet conformations. It is believed that the salt-bridge can stimulate the oligomerization of Aβ by stabilizing the Val24-Asn27 turn (Reddy et al. 2009). The hydrophobic residues in the C-terminus moiety (saddle form) especially Met35 play an important role in fibril stabilization due to modulating Aβ aggregation via hydrophobic interactions. The met35 binding site is therefore considered a potential site to prevent protein–protein interactions and inhibit amyloid fibril formation (Friedemann et al. 2015). However, the central hydrophobic region (17–21) can inhibit fibrillation formation by reducing elongation along the major fibril axis.
Overall, the central hydrophobic core (K16LVFF20), hydrophobic C-terminal residues (29–36), and turn segment are critical regions on Aβ42 which are able to initiate nucleation, enhance conformational transition of Aβ, and promote fibril formation. Therefore, compounds with the potential to act as β-sheet breakers tend to interact with these binding regions responsible for the formation of stable β-conformation and long growth of fibrils. Also, they interfere with hydrophobic contacts within the monomeric structure required for polypeptide collapse and dense conformation by electrostatic, hydrophobic, and π–π interactions (Eskici and Gur 2013). In the following section, we classify them into three main groups, focusing on new achievements in each class separately.
Nanoparticles
Nanostructures are not employed as a carrier for transporting active agents across the BBB in the treatment of AD. Moreover, many studies have focused on designing brain-specific nanostructures capable of protecting neurons from aggregated Aβ toxicity by inhibiting Aβ fibrillation and delaying the accumulation of Aβ oligomeric species (Table 2). Such nanomaterials can directly interact with the Aβ peptides or the aggregated amyloid, thereby overcoming peptide self-assembly into fibrillar plaques or toxic oligomers. Aβ fibril formation is a nucleated self-assembly process that has three phases which include the lag phase (critical oligomer cores formation), the elongation phase (oligomers polymerization), and a pseudo equilibrium/fibril saturation phase (Fig. 3) (Gillam and MacPhee 2013). Nanotechnology-based agents can influence both the lag, elongation, and saturation phases by efficient adsorption of monomers, oligomers, and protofibrils, features enhanced by their unique properties such as large surface-to-volume ratio (Cabaleiro-Lago et al. 2008).
Kumaraswamy et al. (2012) obtained liposomes by the thin-film hydration procedure. Thermal studies revealed that β-sheet breaker agents inserted into the hydrophobic core, where it presented a lower surface tension. This characteristic enabled these liposomes to act as potential therapeutic agents for the inhibition of amyloid aggregation. In another study, Aβ proteins were inserted into amphipathic nanogels composed of cholesterol-bearing pullulan (CHP). The amphipathic properties of these CHP gels afforded them properties similar to natural chaperones (Ikeda et al. 2006). Recently, Boridy et al. (2009) indicated a great reduction in Aβ42-associated toxicity in primary cortical and microglial cell culture after using CHP nanogels. PEGylated phospholipid nanomicelles have also been reported capable of inhibiting Aβ self-assembly (Joshi et al. 2010) by promoting the interaction between the micellar interfaces and the Aβ peptide. Podolski et al. (2007) illustrated an anti-assembly effect of C60 hydrated fullerene (C60HyFn) on the fibrillation of Aβ25–35 fragment. They demonstrated that injection of 3.6 nM of C60HyFn to each of the brain ventricles could prevent and improve the cognitive impairment in AD-affected rats. Kogan et al., in order to destroy amyloid aggregations, utilized local thermal energy that was generated by a mixture of gold nanoparticles (AuNPs) and weak microwave fields (Kogan et al. 2006). The AuNPs are targeted to Aβ plaques, and when enveloped in a weak microwave field, thermal energy was produced, helping to destroy the plaque. Each AuNP provided thermal energy of approximately 10–14 J/s, whereas the required energy for breaking a fibril non-covalent bond is about 10–20 J per bond per μs. It is found that gold NPs of 23 nm can be used as a probe to detect the formation of Aβ fibrils and oligomers (Elbassal et al. 2017). It is shown that this simple, low-cost AuNP-based assay is sensitive to the quantity and oligomeric structures of both Aβ40 and the Aβ40-K16Nle mutant.
Recent studies have exhibited that curcumin may help to delay or inhibit amyloid-beta aggregation due to neuroprotective and cognitive-enhancing properties. However, poor solubility and bioavailability of curcumin have limited its clinical applications (Anand et al. 2007). Polyvinylpyrrolidone conjugated with curcumin coated on the surfaces of gold nanoparticles (PVP–C–AuNP) can increase the bioavailability and solubility of curcumin (Brahmkhatri et al. 2018). In this study, the inhibitory effect of curcumin nanoconjugates was evaluated using TEM analysis of fibers formed from the short Aβ1–16 fragment. It was found that this fragment promotes aggregate formation in the healthy brain. The results showed that curcumin nanoconjugates could stop Aβ1–16 fibrillation and decompose formed aggregations (Anand et al. 2007).
NPs can show dual effects of inhibition or acceleration on the nucleation process according to their physical and chemical features such as size, shape, surface modification, charge, composition, and concentration (Cabaleiro-Lago et al. 2008; Yoo et al. 2011; Sudhakar et al. 2017; John et al. 2018). They show different binding affinity to Aβ monomers and oligomers in various conditions and are therefore also capable of having different effects on the fibrillation process. NP diameter and surface chemistry can modulate the extent of aggregation, while NP electric charge influences the aggregation morphology (Moore et al. 2017). Recently, much attention has been paid to the study of the effect of nanoparticles on the folding and aggregation of peptides.
Size effects of gold nanoparticles (AuNPs) and nanoclusters (AuNCs) stabilized with l-glutathione were reported to play a role in inhibiting protein amyloidosis (Gao et al. 2017). It is described that large AuNPs accelerate Aβ fibrillation, whereas small AuNPs significantly suppress fibrillation process. More interestingly, AuNCs with smaller sizes can completely inhibit the nucleation and amyloidosis. In another study, the effects of gold nanoparticles (AuNPs) with different shapes (nanospheres and cubes) and the same size on the aggregation of an Aβ40 peptide were evaluated (Wang et al. 2019); the results demonstrated that nanospheres show a significant acceleration effect on nucleation and fibrillation process in comparison with nanocubes. This effect may be due to factors such as higher degree of the gold NP surface availability and greater affinity of nanospheres to Aβ40. In another report, it was demonstrated that small, spherical AuNPs have higher anti-fibrillation effects than large, nanocube ones (Liao et al. 2012). In addition, negatively charged gold NPs can delay aggregation processing via more absorption of Aβ monomers rather than positively charged ones (Liao et al. 2012).
The inhibitory ability of gold nanospheres can also change with different surface coatings. PAA (polyacrylic acid)-coated NPs of 18 nm and smaller (8 nm) are superior inhibitors as they can inhibit aggregation at substoichiometric ratios as low as 1:2,000,000 with in relation to Aβ (Moore et al. 2017). Previous reports showed that small iron oxide NPs, with negative charge, presented higher inhibitory activity than their large, positively charged ones (Pansieri et al. 2018). Other investigations illustrated that negatively charged inorganic CdTe (Yoo et al. 2011) and graphene oxide (Mahmoudi et al. 2012) grab Aβ monomers and oligomers to postpone fibrillation phase, while positively self-assembled chitosan-hyaluronic acid composite (CH) NPs exhibited higher inhibitory effect than did the negatively charged ones (with regard to Aβ aggregation) (Jiang et al. 2018). The concentration of nanoparticles can be a decisive factor. Polystyrene NPs present at a high concentration present a large surface area that can capture free Aβ peptides and inhibit fibrillation, while a low concentration can play a role similar to preformed seeds that improve the fibrillation rate (Cabaleiro-Lago et al. 2010).
Organic molecules
In this section, we review the different groups of natural and synthetic small molecules which are able to block the initial stages of Aβ peptide aggregation and toxicity. They may be described as unique pharmacological agents in Alzheimer’s diseases (Table 3).
A large number of small molecules such as polyphenols, inositols, organofluorines, and quinones and their derivatives were trialed and introduced as potential inhibitors of amyloid formation (Brahmachari et al. 2017). These compounds present significant antioxidant and anti-inflammatory properties and as such may play a principal role in diminishing age-dependent oxidative stress and inflammation. Thus, they can obstruct the start of neurodegenerative disorders. Second to this is that these compounds may competitively interact with aromatic amino acids such as phenylalanine in Aβ peptide and impose barriers between aromatic groups, hereby limiting the π–π interactions and preventing the self-assembly process by enhancing the stability of amyloid peptides in the native state (Ahmad et al. 2011). Third, they may inhibit toxic Aβ oligomer interaction with the cell membrane by selective neutralization of the toxic Aβ structural conformation. Also, they may reduce Aβ production via stimulation of the α-secretase pathway and hindering of the β- and γ-secretase pathways (Jayasena et al. 2013).
Overall, these molecules contain two aromatic or inositol groups separated through a backbone of the suitable length (Porat et al. 2006). It can be inferred that the two terminal groups interact with Aβ peptide residues to determine the binding affinity, whereas the linker promotes binding of compounds to specific subregions. It was seen that the polyphenols activity was reduced following the lack of the phenolic functional groups on the aromatic rings (Porat et al. 2006).
It was also established that the linker segment seems to be one of the significant features in amyloid inhibition and the ideal linker region is limited to a fixed length in particular for curcumin, 8–16 Å. The polar functional groups (and often, hydroxyls) commonly exist in inhibitor molecules (Reinke and Gestwicki 2007). Studies have demonstrated that curcumin as a natural polyphenolic antioxidant can decrease Aβ peptide formation from APP and inhibit the Aβ fibrillation into pleated sheets. Yamada and coworkers evaluated the inhibitory activity of curcumin on Aβ peptide (Ono et al. 2004). These in vitro findings showed that curcumin could inhibit Aβ40/42 aggregation and destabilize preformed fibrils. Cole et al. showed in vivo (Yang et al. 2005) that curcumin hinders the formation of oligomers and aggregates through its ability to bind to plaques and decrease fibril-derived Aβ toxicity. In order to determine curcumin permeability through the BBB, its ability to bind to Aβ plaques and persuade rapid decomposition of Aβ plaques in brain tissue and the cerebral vasculature, in vivo multiphoton microscopy studies, was applied in mutated mice model of APPs/PS1dE9 which were treated with curcumin for 7 days. The study revealed reduction of existing plaques. In other studies, it was found that curcumin could diminish inflammatory cytokine levels such as interleukin-1b and isoprostanes in the central nervous system (CNS) as well as reduce amyloid plaque burden in transgenic mice (Ringman et al. 2012).
Modeling studies such as molecular dynamics (MD) simulation showed that curcumin plays an important role in the inhibition of Aβ aggregation (Martin et al. 2018). Curcumin has a dual-inhibitor effect on aggregation process; it can serve as a valuable β-sheet breaker agent and as a chelator able to bind to free ions of Cu2+ and Fe2+. Epigallocatechin gallate (EGCG) is a natural polyphenolic compound which effectively inhibits conformational transition from a random coil to a β-sheet structure and the formation of Aβ and α-synuclein fibrils (Rezai-Zadeh et al. 2005). This agent can pass through the BBB and may be effective as a prophylaxis agent for AD. In vivo findings showed that it improved spatial cognition learning ability in rats and converted Aβ fibrils and toxic oligomers into smaller nontoxic aggregations (Bieschke et al. 2010).
Natural phytoalexin compounds like resveratrol have beneficial properties such as antioxidative, anti-inflammatory, antimutagenic, and anticarcinogenic (Marambaud et al. 2005). Experimental results indicated that resveratrol exhibited inhibitory activity and neuroprotective effects on Aβ fibrillation and neuronal cells, respectively, and produced nontoxic aggregate species instead of toxic oligomers. This compound reduced secreted and intracellular Aβ peptide by BACE-1 inhibition and also decreased Aβ-associated inflammatory mediators like NF-kappa B by overexpressing and activating the SIRT-1pathway. This agent can degrade intracellular Aβ and reduce extracellular Aβ accumulation through action on the proteasome and stimulating AMPK activity. It was recognized that compounds like resveratrol directly join the natively unfolded polypeptides via effective interactions with the existing aromatic groups, break the π–π contacts, and consequently inhibit their conversion into toxic intermediates.
As noted, EGCG and resveratrol (and their analogs) have undergone phase II clinical trials (Belluti et al. 2013). Recently, 3-morpholinosydnonimine hydrochloride (SIN-1), a synthetic FDA-approved drug in inhibition of platelet aggregation in cardiovascular disease (CVD), has undergone testing for its ability to inhibit amyloid formation (Ren et al. 2017). The in vitro and computational results showed that this drug can effectively inhibit Aβ misfolding and aggregation at different steps of aggregation, prolonging the lag phase, slowing the aggregation rate, and reducing the total amount of fibril formation as well as decreasing Aβ-induced cell toxicity in a dose-dependent manner. It exhibited a remarkable tendency for binding hydrophobic residues I31−M35 and interrupting the formation of the C-terminal β-sheet of Aβ peptide and Aβ−Aβ association (Ren et al. 2017).
Matrine (Mat) is a new natural compound, which is obtained from traditional Chinese herbs to treat dementia. Cui et al. (2017) introduced this compound for inhibition of the Aβ aggregation and blocking the RAGE/Aβ pathway. They discovered that it could inhibit Aβ42-induced cytotoxicity and stop the Aβ/RAGE signaling pathway in an AD mouse model. Also, it was observed that it reduced the levels of pro-inflammatory cytokines and Aβ deposition as well as modulated the memory impairment in AD transgenic mice. Norepinephrine (NE) is a natural neurotransmitter in the body. In vitro and computational results suggest that this compound (Zou et al. 2019) inhibited formation of Aβ aggregation and destabilized Aβ protofibril via formation of H-bonds with residues D1, A2, D23, and A42 in Aβ peptide. In addition, it can reduce inter-peptide β-sheet content and suppress formation of the β-hairpin structure, which leads to a more disordered coil-rich Aβ dimer.
HP-β-Cyclodextrin (HP-β-CD) is a synthetic sugar derivative that is used in drug delivery, genetic vector, environmental protection, and Niemann–Pick disease type C1 (NPC1) treatment. Its efficiency has been investigated as a sugar-based Aβ inhibitor (Ren et al. 2016). In vitro results indicated that it prevented Aβ42 aggregation and Aβ-induced toxicity in a concentration-dependent method as well showing no intrinsic cellular toxicity. Simulation studies showed that it has a high tendency to interact with hydrophobic residues of Aβ at two β-strands and N-terminal domain. It was also reported that carbenoxolone (Cbx), as a natural glycyrrhetinic acid–based compound and FDA-approved drug for the treatment of peptic and esophageal inflammation, has a neuroprotective effect and can stop the aggregation of Aβ42 peptide and destabilize the formed fibrillations (Sharma et al. 2017). This agent forms strong interactions with the available residues in the amyloidogenic regions of Aβ42 monomers.
Peptides and antibodies
Due to their crucial ability to regulate biological functions, peptides represent another important pharmaceutical choice instead of small organic compound–based drugs. Nowadays, peptides constitute a large fraction of the global drug market due to their unique properties such as high selectivity, low side effects and toxicity, low accumulation in tissues, good tolerance, synthetic viability and practicality, and diversity of chemical and biological synthesis routes, along with a possibility for rational design compared with other therapeutic compounds (Danho et al. 2009). A large number of therapeutic peptides have been proposed as Aβ aggregation inhibitors for treatment of AD (Table 4). Peptides are well-known as β-sheet breakers. Peptide candidates are typically assessed based on their capacity to inhibit Aβ toxicity and self-assembly, prevent conformational transitions, and increase alternative nontoxic fibrillation pathways.
As previously reported, various regions of the Aβ peptide are responsible for the process of Aβ fibrillation. This knowledge is essential for the rational design and development of peptide inhibitors. According to these vital regions the Aβ peptide sequence, the peptide-based inhibitors are divided into two main categories: (1) Aβ sequence-derived peptides and (2) non-Aβ-derived peptide sequences.
Aβ sequence-derived peptides
Peptide inhibitors are principally derived from the Aβ peptide based on regions of the central hydrophobic core (CHC) sequence and C-terminal fragments (CTFs). These peptides are homologous to Aβ peptide and hydrophobic feature but have a low tendency to form β-sheets as well as a good binding affinity to Aβ peptide. The central hydrophobic core (CHC) region (residues K16LVFFA21) of Aβ is also known as a key self-recognition sequence or the nucleation site within the Aβ peptide which is responsible for aggregation (Petkova et al. 2002). It was suggested that residues of Ile41 and Ala42 from Aβ42 peptide could strongly support stabilization of a new conformation (Li et al., 2011a). Designed short peptides related to the hydrophobic core residues have been widely investigated as potential inhibitors based on their ability to interact with the full-length Aβ peptide. The CTFs on Aβ42 peptide is an important domain with strong rigidity for targeting of Aβ oligomerization. CTFs are able to adjust intermolecular interactions for controlling of Aβ42 oligomer formation. The CTF domain reacts with several sites on Aβ42 such as C-terminus and N-terminus (Urbanc et al. 2004). Although the natural amino acid–containing peptides are effective inhibitor agents against Aβ aggregation, they suffer from rapid proteolytic degradation in plasma and tend to self-assemble into fibrils during administration and delivery. To overcome these problems and improve their binding affinity to the Aβ peptide, modified peptides with different approaches were utilized (Bruno et al. 2013). These approaches include fluorination, use of d-amino acids, and also the use of retro-inverso cyclization and N-methylation of the ester bond (Goyal et al. 2017; Yan et al. 2013).
Fluorination of the hydrophobic amino acids valine or phenylalanine in the KLVFF sequence can increase the peptide inhibitor activity. Fluorinated amino acids bind to hydrophobic residues of Aβ peptide and interfere with the hydrophobic contacts between Aβ peptide monomers and inhibit their aggregation (Loureiro et al. 2014). d-Amino acid–containing peptides have higher stability against proteolytic enzymes and demonstrate greater affinity when binding to Aβ peptide than their l-isomers. Using animal models, d-peptides were shown to have inhibitor activity against Aβ aggregation (Jagota and Rajadas 2013). Retro-inverso peptides, produced using d-amino acids and flipping the NH and CO groups in the peptide bonds, maintain the same spatial position of the side chain residues and protect the favorable 3D structure in comparison with unmodified l-peptides (Chorev and Goodman 1995). These peptides show advantages with respect to inhibition, higher enzymatic stability, reduced self-assembly, and an improved BBB permeability in an animal model in comparison to l-peptides. Cyclic peptides show strong and specific inhibitor effects towards the formation of amyloid aggregation compared with their noncyclic ones (Luo and Abrahams 2014). Due to their high protease resistance, they are degraded slowly. Methyl group addition to amide groups is a powerful approach in the development of new inhibitors. N-methyl groups can both improve the solubility in aqueous solution and reduce the Aβ toxicity.
Reported N-methylated proprietary peptides such as D-NH2 (SEN304) (Larbanoix et al. 2011) and SEN1576 can inhibit Aβ-associated toxicity in in vivo studies (Kokkoni et al. 2006; Amijee et al. 2012). Importantly, the SEN304 peptide has been not derived from Aβ sequence and yet is a more potent inhibitor than customized versions of the KLVFF peptide. These peptides can promote Aβ nucleation into nontoxic forms, thereby eliminating toxic oligomers. There are important other factors which can be used in the rational design of peptide inhibitor. Solvent tension is a crucial factor in Aβ aggregation (Ghanta et al. 1996).
Glutamic acid and lysine residues have been recognized as potential enhancing and stabilizing agents (kosmotropes) of Aβ fibrillation through improving the surface tension, while arginine residues have been recognized as inhibitions of aggregation through their action as destabilizing agents (chaotropes) without associating the solvent feature. Tjernberg et al. (1996) demonstrated that Aβ16–20 (KLVFF) plays an important role in disrupting the aggregation of Aβ by binding to full-length Aβ peptides and preventing fibril formation in vitro (Tjernberg et al. 1996). Subsequently, peptides derived from this short sequence were reported for their ability to inhibit the aggregation process. Also, this fragment has been modified using different delivery platforms, such as a dendrimer, polymer, or a few residues of hydrophilic amino acids, in order to improve their physicochemical properties and inhibitory effect on the β-sheet formation.
As previously described, the proline amino acid is a proper β-sheet breaker (Wood et al. 1995). Soto and coworkers rationally entered proline and aspartic acid residues in place of valine and alanine, respectively, to obtain a proline-containing peptide (the LPFFD 5-mer iAβ5) (Soto et al. 1998). This derived peptide from the KLVFF sequence is a β-sheet breaker which can inhibit Aβ aggregation and reduce plaque burden, and neurotoxicity (Soto et al. 1998). Proline prevents the formation of hydrogen bonds in fibrils due to lack of a proton on the secondary substituted nitrogen in the peptide bond. These reported short peptides suffer from rapid degradation by proteolytic enzymes and poor BBB permeability in vivo study (although they showed a significant in vitro efficacy). In order to improve their stability in mice brain and a greater half-life after intravenous (IV) administration, iAβ5p derivate was introduced which had been modified by N-methylation between Pro and Phe residues (Cruz et al. 2004).
The in vitro/in vivo results showed that it has a similar inhibitory effect to the iAb5 peptide against amyloid fibril formation and neurotoxicity but its resistance to protease degradation is greater than shown by the iAb5 peptide. In addition, MD simulations indicate that this peptide has stronger binding and enhanced activity against Aβ40 aggregation when compared with the iAβ5 peptide. The KLVFWAK motif was derived from the KLVFF sequence, and a mutation was introduced at the glutamic acid (E22) residue (to lysine (K)) to improve solubility and disrupt self-assembly by electrostatic repulsion (Aoraha et al. 2015). This designed motif targets only C-terminal domain in Aβ oligomers. Results indicated that this motif showed the smallest self-aggregation potential and highest binding affinity to Aβ aggregates and fibrils compared with other peptide candidate. On the other hand, it should have more specificity for reliable detection of Aβ oligomer and fibrils in vivo and ex vivo studies. Towards this aim, d-GRKKRRQRRR-GGGG-DVEFRH (Aβ1−6A2V-TAT) peptide was designed and evaluated in vivo (Di Fede et al. 2009; Cimini et al. 2016).
The N-terminal fragment of DAEFRH (Aβ1−6) was modified by mutation of alanine 2 to valine and conjugation with the HIV protein transduction domain GRKKRRQRRR (TAT). The TAT motif improves permeability of peptides into/across cell membranes and assists in crossing the BBB. This designed peptide showed great proteolytic stability and higher binding affinity towards Aβ40 fibrils than Aβ1−6 and inhibited fibrillation formation and elongation in the brain. In order to maximize electrostatic interactions for disrupting in aggregation process and reduce the tendency for self-assembly of the KLVFF segment, RIVFF sequence was designed and modified based on KLVFF sequence using residue mutations of lysine16 (K) to arginine (R) and leucine17 (L) to isoleucine (I) (Ramaswamy et al. 2014).
The results demonstrated that this peptide exhibits reduced surface tension upon self-aggregating into β-sheet structures and may practically enhance cytotoxicity. The two peptides RGKLVFFGR (OR1) and RGKLVFFGR-NH (OR2) are known as retro-inverso peptides (Austen et al. 2008). These peptides derived from the KLVFF sequence were modified via addition of an arginine (R) and glycine (G) residues to enhance their solubility, to prevent self-aggregation, and to act as spacers, respectively. These peptides showed high solubility and stability against proteases while only OR2 peptide demonstrated effective inhibitory effects on Aβ oligomer formation and cytotoxicity. In order to further improve these characteristics, OR2 peptide was modified as HN-rGklvffGr-Ac (RI-OR2) using acetylation of the C-terminal residue (Taylor et al. 2010). The resulting peptide showed high resistance against proteolysis with the same previous inhibitory activity demonstrated in vivo. In another study, the RI-OR2 peptide was conjugated to the TAT peptide to enhance cell membranes and BBB permeability (Parthsarathy et al. 2013). The findings showed that it decreased Aβ aggregation, Aβ plaque levels, and oxidative damages while it enhanced the number of young neurons in the brain.
Ac-LVFFARK-NH2 (LK7) is a peptide derived from the KLVFF sequence via incorporation of two positively charged residues arginine and lysine (R and K) (Xiong et al. 2015). It has been shown to have a dose-dependent inhibitory effect on Aβ42 fibrillation process, but due to a high self-assembly properties, it can actually increase cytotoxicity. To reduce this self-aggregation feature and improve inhibitory activity, the LK7 peptide was added to polymers, nanoparticles, and chelators. The LK7 peptide was conjugated onto poly(lactic-co-glycolic acid) NPs. The obtained LK7-PLGA-NPs complex eliminated LK7 self-assembly while also inhibiting Aβ42 fibrillation (Xiong et al. 2015). Binding β-cyclodextrin to LK7 (Zhang et al., 2018a) enhanced solubility of LK7 peptide, suppressed its self-aggregation tendency, and improved its binding and inhibitory abilities against Aβ aggregation. Head-to-tail cyclization of LK7 peptide also led to a decrease of the self-assembly propensity of the LK7, an increase of proteolytic stability and binding affinity to the Aβ40 peptide. This derivative also can stabilize the Aβ40 secondary structure and prevent Aβ40-related cytotoxicity. Another derivative of LK7 peptide is Ac-LVFFARKHH-NH2 (LK7-HH) in which LK7 has been attached to the HH ligand as a chelator for capturing free and complexed ions of Cu2+ and reducing reactive oxygen species (ROS) production (Zhang et al., 2018a, b, c). This chelator also improved anti-aggregative effects of LK7 against Aβ peptide and reduced its self-aggregation propensity.
Sequences derived from the C-terminal fragments of Aβ42, including IIGLMGGVVIA (Aβ31−42) and VVIA (Aβ39−42), have also been shown to act as inhibitors of Aβ aggregation (Fradinger et al. 2008). It has been shown that the tetrameric Aβ39−42 peptide interacts with small oligomers and Aβ42 monomers and locates at several positions, specifically at the N-terminal region in MD simulations. Also, the results illustrated that VVIA-NH2 peptide inhibits Aβ42 aggregation and Aβ42-related toxicity preserving synaptic activity at micromolar levels. However, the acetylated Ac-VVIA sequence did not show these effects (Zheng et al. 2015). The non-acetylated VVIA-NH2 sequence interacts particularly with the C-terminal region while the Ac-VVIA peptide showed a dispersed binding distribution (Zheng et al. 2015). Recently, the Ac-IGLMVG-NH2 sequence (Aβ32–37), a hexapeptide derived from the C-terminal fragment, has been evaluated as an inhibitor of Aβ toxicity in vitro. It revealed a mild efficiency against Aβ-related toxicity (Bansal et al. 2016).
A different class of Aβ aggregation inhibitor was reported that might help the development and improvement of new therapeutics. O-acyl isopeptide (1) and NMe-b-Ala26 (2) (Aβ42 derivatives) were introduced as inhibitors (Kawashima et al. 2013). They were derived from the full-length Aβ sequence with modification of an ester bond at the Gly25-Ser26 moiety and an N-methyl amide-β-Ala26, respectively. In vitro results showed that derivative (1) inhibited the formation of Aβ42 fibrillation at an equimolar ratio with an inhibitory mechanism different from any other peptidic inhibitors reported so far. Also, this derivative showed more aqueous solubility rather than Aβ42 peptides and rapidly decomposed to Aβ42 monomers under physiological conditions through an O-to-N acyl rearrangement reaction while derivative (2) exhibited higher chemical stability at physiological conditions.
A novel metalloporphyrin-peptide conjugate based on the KLVFF motif was applied as a fluorescent sensor for detection and visualization of soluble Aβ oligomers in biological fluids (Villari et al. 2017). The zinc-porphyrin compound was covalently attached to the KLVFF motif, and the resulting structure targets histidine residues and hydrophobic region of Aβ42. This conjugated compound can enhance amyloid suppression properties and photodynamic therapy as well as inhibition of the cytotoxic effects of Aβ42 through the formation of supramolecular bodies with the protein. Gordon et al. (2001) described Apan or PPI1019 (D-(H-((Me-L)-VFFL)-NH2)) as an N-methylated peptide inhibitor for Aβ aggregation and neurotoxicity. This peptide is currently at phase II clinical trial (Sun et al. 2012).
Non-Aβ sequence-derived peptides
The peptide QSHYRHISPAQV (D1) was reported as a peptide inhibitor not derived from the Aβ sequence (Wiesehan et al. 2003). This peptide was selected using a randomized mirror-image phage display technique. Results showed that it interacts with all forms of Aβ peptide (oligomers and fibrils and monomers) and binds specifically to Aβ plaques in the tissue of human brain. It also reduces Aβ aggregation formation and Aβ-associated cytotoxicity at high concentrations. A related peptide D-RPRTRLHTHRNR (D3) was also proposed for inhibition of Aβ aggregation and Aβ-related toxicity (Van Groen et al. 2008). This peptide was not taken from the Aβ sequence and was identified by the mirror-image phage display method. It exhibited great enzymatic stability, good BBB permeability, and efficient bioavailability in oral administration. Moreover, it can bind to Aβ oligomers and convert resulting aggregations to nontoxic amorphous forms via changing of their morphology (Van Groen et al. 2008). In vivo results showed that this peptide decreased Aβ plaque levels and Aβ-related inflammations and improved cognitive impairment in an AD mouse model. Presently, D3 and its derivatives are being tested in phase III clinical trials and are currently at the stage of safety analysis.
Carnosine is a natural imidazole dipeptide molecule which is in muscle and brain tissues. This natural compound was not taken from Aβ sequence, and like a chelator, it can coordinate divalent metal ions (Aloisi et al. 2013). The in vitro and in vivo results showed that it has inhibitory activity against fibrillation process of amyloidogenic species such as Aβ peptide, natural and glycated α-crystallin, and prion protein and reduces their associated toxicity on rat brain endothelial and PC12 cells. This peptide blocks the formation of the intermolecular salt bridge, which is important in stability, and elongation of fibrillation (Aloisi et al. 2013).
Polyclonal antibodies, due to their intrinsic heterogeneity, show inferior biological function to monoclonal antibodies (Dodel et al. 2004). Research has revealed that a monoclonal antibody directed against a single epitope can identify Aβ peptide and suppress its aggregation and cytotoxicity (Du et al. 2003). Previous results have shown that the bapineuzumab monoclonal antibody acts effectively as an Aβ aggregation inhibitor. Other mABs have entered in phase III clinical trial (Nie et al. 2011). These include the solanezumab (LY2062430) monoclonal antibody which was designed as a humanized anti-Aβ peptide immunoglobulin (IgG1). Solanezumab was shown to reduce cognitive and functional decline in AD by lowering Aβ production. Currently, it has completed the phase III clinical trial (Han and He 2018).
Associated challenges with inhibitors of Aβ aggregation
Inhibitor compounds of Aβ aggregation such as metal chelators, nanostructure-based strategies, organic molecules, peptides, and antibodies that interact and bind to specific domains of Aβ highlight new developments of amyloid hypothesis-based therapeutics. These compounds also face challenges and problems that prevent their entrance to clinical uses. For this reason, to date, none of these compounds have proven successful in clinical trials.
It is well that when NPs come into a physiological environment, their surfaces will be immediately covered by biomolecules such as proteins to produce protein crown-like halos, and the effect of these structures on Aβ fibrillation is currently being evaluated (Salvati et al. 2013). Another important issue with nano-based compounds is their potential toxicity although relatively few studies have reported about long-term toxicity after NP use. It is also known that small molecules produce inadequate steric hindrance effects and are therefore usually unable to inhibit Aβ aggregation (Wells and McClendon 2007). Other important challenges around peptide therapeutic use are BBB permeability, serum stability, and their self-assembly dring storage. In recent years, a tremendous effort has been employed on combatting these limitations.
Conclusion
According to the World Alzheimer Report 2016, nearly 46.8 million people worldwide are currently affected by AD. This number is expected to increase to 131.5 million by 2050 Prince (2015). Yet, there is no cure for AD nor any sensitive clinical tools for the detection and diagnosis of early onset AD. As discussed in this Review, one of the main challenges is that AD is a multifactorial disease that may have different pathologies and etiologies. Specifically, AD can manifest in a molecular sense as Aβ aggregation and fibrillation, tau phosphorylating kinases ROS, and cell cycle proteins. A large body of research suggests that production and aggregation of Aβ peptide causes AD. Therefore, developing methods and tools to inhibit Aβ aggregation will represent a great step forward for AD therapy.
References
Adlard PA, Cherny RA, Finkelstein DI, Gautier E, Robb E, Cortes M, Volitakis I, Liu X, Smith JP, Perez K (2008) Rapid restoration of cognition in Alzheimer’s transgenic mice with 8-hydroxy quinoline analogs is associated with decreased interstitial Aβ. Neuron 59(1):43–55
Ahmad E, Ahmad A, Singh S, Arshad M, Khan AH, Khan RH (2011) A mechanistic approach for islet amyloid polypeptide aggregation to develop anti-amyloidogenic agents for type-2 diabetes. Biochimie 93(5):793–805
Ahmad Fazili N, Naeem A, Hua Gan S, Kamal MA (2015) Therapeutic interventions for the suppression of Alzheimer’s disease: quest for a remedy. Curr Drug Metab 16(5):346–353
Aloisi A, Barca A, Romano A, Guerrieri S, Storelli C, Rinaldi R, Verri T (2013) Anti-aggregating effect of the naturally occurring dipeptide carnosine on aβ1-42 fibril formation. PLoS One 8(7):e68159
Amijee H, Bate C, Williams A, Virdee J, Jeggo R, Spanswick D, Scopes DI, Treherne JM, Mazzitelli S, Chawner R (2012) The N-methylated peptide SEN304 powerfully inhibits Aβ (1–42) toxicity by perturbing oligomer formation. Biochemistry 51(42):8338–8352
Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB (2007) Bioavailability of curcumin: problems and promises. Mol Pharm 4(6):807–818
Anguiano M, Nowak RJ, Lansbury PT (2002) Protofibrillar islet amyloid polypeptide permeabilizes synthetic vesicles by a pore-like mechanism that may be relevant to type II diabetes. Biochemistry 41(38):11338–11343
Ansari MA, Abdul HM, Joshi G, Opii WO, Butterfield DA (2009) Protective effect of quercetin in primary neurons against Aβ (1–42): relevance to Alzheimer’s disease. J Nutr Biochem 20(4):269–275
Aoraha E, Candreva J, Kim JR (2015) Engineering of a peptide probe for β-amyloid aggregates. Mol BioSyst 11(8):2281–2289
Ashur-Fabian O, Segal-Ruder Y, Skutelsky E, Brenneman DE, Steingart RA, Giladi E, Gozes I (2003) The neuroprotective peptide NAP inhibits the aggregation of the beta-amyloid peptide. Peptides 24(9):1413–1423
Association A s (2016) 2016 Alzheimer’s disease facts and figures. Alzheimers Dement 12(4):459–509
Atwood CS, Moir RD, Huang X, Scarpa RC, Bacarra NME, Romano DM, Hartshorn MA, Tanzi RE, Bush AI (1998) Dramatic aggregation of Alzheimer Aβ by Cu (II) is induced by conditions representing physiological acidosis. J Biol Chem 273(21):12817–12826
Atwood CS, Scarpa RC, Huang X, Moir RD, Jones WD, Fairlie DP, Tanzi RE, Bush AI (2000) Characterization of copper interactions with Alzheimer amyloid β peptides: identification of an attomolar-affinity copper binding site on amyloid β1-42. J Neurochem 75(3):1219–1233
Austen BM, Paleologou KE, Ali SA, Qureshi MM, Allsop D, El-Agnaf OM (2008) Designing peptide inhibitors for oligomerization and toxicity of Alzheimer’s β-amyloid peptide. Biochemistry 47(7):1984–1992
Bansal S, Maurya IK, Yadav N, Thota CK, Kumar V, Tikoo K, Chauhan VS, Jain R (2016) C-terminal fragment, Aβ32–37, analogues protect against aβ aggregation-induced toxicity. ACS Chem Neurosci 7(5):615–623
Bartus RT, Emerich DF (1999) Cholinergic markers in Alzheimer disease. Jama 282(23):2208–2209
Bekris LM, Yu C-E, Bird TD, Tsuang DW (2010) Genetics of Alzheimer disease. J Geriatr Psychiatry Neurol 23(4):213–227
Belluti F, Rampa A, Gobbi S, Bisi A (2013) Small-molecule inhibitors/modulators of amyloid-β peptide aggregation and toxicity for the treatment of Alzheimer’s disease: a patent review (2010–2012). Expert Opin Ther Patents 23(5):581–596
Bieschke J, Russ J, Friedrich RP, Ehrnhoefer DE, Wobst H, Neugebauer K, Wanker EE (2010) EGCG remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity. Proc Natl Acad Sci 107(17):7710–7715
Boridy S, Takahashi H, Akiyoshi K, Maysinger D (2009) The binding of pullulan modified cholesteryl nanogels to Aβ oligomers and their suppression of cytotoxicity. Biomaterials 30(29):5583–5591
Brahmachari S, Paul A, Segal D, Gazit E (2017) Inhibition of amyloid oligomerization into different supramolecular architectures by small molecules: mechanistic insights and design rules. Future Med Chem 9(8):797–810
Brahmkhatri VP, Sharma N, Sunanda P, D’Souza A, Raghothama S, Atreya HS (2018) Curcumin nanoconjugate inhibits aggregation of N-terminal region (Aβ-16) of an amyloid beta peptide. New J Chem 42(24):19881–19892
Brener O, Dunkelmann T, Gremer L, Van Groen T, Mirecka EA, Kadish I, Willuweit A, Kutzsche J, Jürgens D, Rudolph S (2015) QIAD assay for quantitating a compound’s efficacy in elimination of toxic Aβ oligomers. Sci Rep 5:13222
Bruce NJ, Chen D, Dastidar SG, Marks GE, Schein CH, Bryce RA (2010) Molecular dynamics simulations of Aβ fibril interactions with β-sheet breaker peptides. Peptides 31(11):2100–2108
Bruno BJ, Miller GD, Lim CS (2013) Basics and recent advances in peptide and protein drug delivery. Ther Deliv 4(11):1443–1467
Cabaleiro-Lago C, Quinlan-Pluck F, Lynch I, Dawson KA, Linse S (2010) Dual effect of amino modified polystyrene nanoparticles on amyloid β protein fibrillation. ACS Chem Neurosci 1(4):279–287
Cabaleiro-Lago C, Quinlan-Pluck F, Lynch I, Lindman S, Minogue AM, Thulin E, Walsh DM, Dawson KA, Linse S (2008) Inhibition of amyloid β protein fibrillation by polymeric nanoparticles. J Am Chem Soc 130(46):15437–15443
Casdorph H (1981) EDTA chelation therapy II, efficacy in brain disorders. J Holist Med 3:101–117
Chauhan NB, Siegel GJ (2007) Antisense inhibition at the β-secretase-site of β-amyloid precursor protein reduces cerebral amyloid and acetyl cholinesterase activity in Tg2576. Neuroscience 146(1):143–151
Chen T, Zhang Y, Shang Y, Gu X, Zhu Y, Zhu L (2018) NBD-BPEA regulates Zn2+-or Cu2+-induced Aβ40 aggregation and cytotoxicity. Food Chem Toxicol 119:260–267
Cherny RA, Atwood CS, Xilinas ME, Gray DN, Jones WD, McLean CA, Barnham KJ, Volitakis I, Fraser FW, Kim Y-S (2001) Treatment with a copper-zinc chelator markedly and rapidly inhibits β-amyloid accumulation in Alzheimer’s disease transgenic mice. Neuron 30(3):665–676
Chorev M, Goodman M (1995) Recent developments in retro peptides and proteins—an ongoing topochemical exploration. Trends Biotechnol 13(10):438–445
Churches QI, Caine J, Cavanagh K, Epa VC, Waddington L, Tranberg CE, Meyer AG, Varghese JN, Streltsov V, Duggan PJ (2014) Naturally occurring polyphenolic inhibitors of amyloid beta aggregation. Bioorg Med Chem Lett 24(14):3108–3112
Cimini S, Sclip A, Mancini S, Colombo L, Messa M, Cagnotto A, Di Fede G, Tagliavini F, Salmona M, Borsello T (2016) The cell-permeable Aβ1-6A2VTAT (D) peptide reverts synaptopathy induced by Aβ1-42wt. Neurobiol Dis 89:101–111
Civitelli L, Sandin L, Nelson E, Khattak SI, Brorsson A-C, Kågedal K (2016) The luminescent oligothiophene p-FTAA converts toxic Aβ1–42 species into nontoxic amyloid fibers with altered properties. J Biol Chem 291(17):9233–9243
Colovic MB, Krstic DZ, Lazarevic-Pasti TD, Bondzic AM, Vasic VM (2013) Acetylcholinesterase inhibitors: pharmacology and toxicology. Curr Neuropharmacol 11(3):315–335
Conte-Daban A, Boff B, Candido Matias A, Aparicio CNM, Gateau C, Lebrun C, Cerchiaro G, Kieffer I, Sayen S, Guillon E (2017) A trishistidine pseudopeptide with ability to remove both CuΙ and CuΙΙ from the amyloid-β peptide and to stop the associated ROS formation. Chem Eur J 23(67):17078–17088
Corder E, Saunders AM, Risch N, Strittmatter W, Schmechel D, Gaskell P, Rimmler J, Locke P, Conneally P, Schmader K (1994) Protective effect of apolipoprotein E type 2 allele for late onset Alzheimer disease. Nat Genet 7(2):180
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small G, Roses AD, Haines J, Pericak-Vance MA (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261(5123):921–923
Crouch PJ, Barnham KJ (2012) Therapeutic redistribution of metal ions to treat Alzheimer’s disease. Acc Chem Res 45(9):1604–1611
Cruz M, Tusell J, Grillo-Bosch D, Albericio F, Serratosa J, Rabanal F, Giralt E (2004) Inhibition of β-amyloid toxicity by short peptides containing N-methyl amino acids. J Pept Res 63(3):324–328
Cui L, Cai Y, Cheng W, Liu G, Zhao J, Cao H, Tao H, Wang Y, Yin M, Liu T (2017) A novel, multi-target natural drug candidate, matrine, improves cognitive deficits in Alzheimer’s disease transgenic mice by inhibiting Aβ aggregation and blocking the RAGE/Aβ Axis. Mol Neurobiol 54(3):1939–1952
Cui Z, Lockman PR, Atwood CS, Hsu C-H, Gupte A, Allen DD, Mumper RJ (2005) Novel D-penicillamine carrying nanoparticles for metal chelation therapy in Alzheimer’s and other CNS diseases. Eur J Pharm Biopharm 59(2):263–272
Danho, W., J. Swistok, W. Khan, X.-J. Chu, A. Cheung, D. Fry, H. Sun, G. Kurylko, L. Rumennik and J. Cefalu (2009). Opportunities and challenges of developing peptide drugs in the pharmaceutical industry. Peptides for Youth, Springer, pp 467–469
Datki Z, Papp R, Zádori D, Soós K, Fülöp L, Juhász A, Laskay G, Hetényi C, Mihalik E, Zarándi M (2004) In vitro model of neurotoxicity of Aβ 1–42 and neuroprotection by a pentapeptide: irreversible events during the first hour. Neurobiol Dis 17(3):507–515
Deane R, Bell RD, Sagare A, Zlokovic BV (2009) Clearance of amyloid-β peptide across the blood-brain barrier: implication for therapies in Alzheimers Disease. CNS Neurol Disord-Dr Targets 8:16. https://doi.org/10.2174/187152709787601867
Deane R, Du Yan S, Submamaryan RK, LaRue B, Jovanovic S, Hogg E, Welch D, Manness L, Lin C, Yu J (2003) RAGE mediates amyloid-β peptide transport across the blood-brain barrier and accumulation in brain. Nat Med 9(7):907
Di Fede G, Catania M, Morbin M, Rossi G, Suardi S, Mazzoleni G, Merlin M, Giovagnoli AR, Prioni S, Erbetta A (2009) A recessive mutation in the APP gene with dominant-negative effect on amyloidogenesis. Science 323(5920):1473–1477
Dodel R, Du Y, Depboylu C, Hampel H, Frölich L, Haag A, Hemmeter U, Paulsen S, Teipel S, Brettschneider S (2004) Intravenous immunoglobulins containing antibodies against β-amyloid for the treatment of Alzheimer’s disease. J Neurol Neurosurg Psychiatry 75(10):1472–1474
Dong M, Li H, Hu D, Zhao W, Zhu X, Ai H (2016) Molecular dynamics study on the inhibition mechanisms of drugs CQ1–3 for Alzheimer amyloid-β40 aggregation induced by Cu2+. ACS Chem Neurosci 7(5):599–614
Du Y, Wei X, Dodel R, Sommer N, Hampel H, Gao F, Ma Z, Zhao L, Oertel WH, Farlow M (2003) Human anti-β-amyloid antibodies block β-amyloid fibril formation and prevent β-amyloid-induced neurotoxicity. Brain 126(9):1935–1939
Elbassal EA, Morris C, Kent TW, Lantz R, Ojha B, Wojcikiewicz EP, Du D (2017) Gold nanoparticles as a probe for amyloid-β oligomer and amyloid formation. J Phys Chem C 121(36):20007–20015
Emi M, Wu LL, Robertson MA, Myers RL, Hegele RA, Williams RR, White R, Lalouel J-M (1988) Genotyping and sequence analysis of apolipoprotein E isoforms. Genomics 3(4):373–379
Eskici G, Gur M (2013) Computational design of new peptide inhibitors for amyloid beta (Aβ) aggregation in Alzheimer’s disease: application of a novel methodology. PLoS One 8(6):e66178
Finder VH, Glockshuber R (2007) Amyloid-β aggregation. Neurodegener Dis 4(1):13–27
Fradinger EA, Monien BH, Urbanc B, Lomakin A, Tan M, Li H, Spring SM, Condron MM, Cruz L, Xie C-W (2008) C-terminal peptides coassemble into Aβ42 oligomers and protect neurons against Aβ42-induced neurotoxicity. Proc Natl Acad Sci 105(37):14175–14180
Friedemann M, Helk E, Tiiman A, Zovo K, Palumaa P, Tõugu V (2015) Effect of methionine-35 oxidation on the aggregation of amyloid-β peptide. Biochem Biophys Rep 3:94–99
Fu Z, Luo Y, Derreumaux P, Wei G (2009) Induced β-barrel formation of the Alzheimer’s Aβ25–35 oligomers on carbon nanotube surfaces: implication for amyloid fibril inhibition. Biophys J 97(6):1795–1803
Gao G, Zhang M, Gong D, Chen R, Hu X, Sun T (2017) The size-effect of gold nanoparticles and nanoclusters in the inhibition of amyloid-β fibrillation. Nanoscale 9(12):4107–4113
Geng J, Li M, Wu L, Ren J, Qu X (2012) Liberation of copper from amyloid plaques: making a risk factor useful for Alzheimer’s disease treatment. J Med Chem 55(21):9146–9155
Ghanta J, Shen C-L, Kiessling LL, Murphy RM (1996) A strategy for designing inhibitors of β-amyloid toxicity. J Biol Chem 271(47):29525–29528
Giedraitis V, Sundelöf J, Irizarry MC, Gårevik N, Hyman BT, Wahlund L-O, Ingelsson M, Lannfelt L (2007) The normal equilibrium between CSF and plasma amyloid beta levels is disrupted in Alzheimer’s disease. Neurosci Lett 427(3):127–131
Gillam J, MacPhee C (2013) Modelling amyloid fibril formation kinetics: mechanisms of nucleation and growth. J Phys Condens Matter 25(37):373101
Glabe CC (2005) Amyloid accumulation and pathogenesis of Alzheimer’s disease: significance of monomeric, oligomeric and fibrillar Aβ. Alzheimer’s Disease, Springer, pp 167–177
Gordon DJ, Sciarretta KL, Meredith SC (2001) Inhibition of β-amyloid (40) fibrillogenesis and disassembly of β-amyloid (40) fibrils by short β-amyloid congeners containing N-methyl amino acids at alternate residues. Biochemistry 40(28):8237–8245
Goyal D, Shuaib S, Mann S, Goyal B (2017) Rationally designed peptides and peptidomimetics as inhibitors of amyloid-β (Aβ) aggregation: potential therapeutics of Alzheimer’s disease. ACS Comb Sci 19(2):55–80
Graeber M, Kösel S, Egensperger R, Banati R, Müller U, Bise K, Hoff P, Möller H, Fujisawa K, Mehraein P (1997) Rediscovery of the case described by Alois Alzheimer in 1911: historical, histological and molecular genetic analysis. Neurogenetics 1(1):73–80
Granic I, Masman MF, Nijholt IM, Naude PJ, de Haan A, Borbély E, Penke B, Luiten PG, Eisel UL (2010) LPYFDa neutralizes amyloid-β-induced memory impairment and toxicity. J Alzheimers Dis 19(3):991–1005
Guo J, Sun W, Liu F (2017) Brazilin inhibits the Zn2+-mediated aggregation of amyloid β-protein and alleviates cytotoxicity. J Inorg Biochem 177:183–189
Haass C, Selkoe DJ (1993) Cellular processing of β-amyloid precursor protein and the genesis of amyloid β-peptide. Cell 75(6):1039–1042
Habchi J, Arosio P, Perni M, Costa AR, Yagi-Utsumi M, Joshi P, Chia S, Cohen SI, Müller MB, Linse S (2016) An anticancer drug suppresses the primary nucleation reaction that initiates the production of the toxic Aβ42 aggregates linked with Alzheimer’s disease. Sci Adv 2(2):e1501244
Hajipour MJ, Santoso MR, Rezaee F, Aghaverdi H, Mahmoudi M, Perry G (2017) Advances in Alzheimer’s diagnosis and therapy: the implications of nanotechnology. Trends Biotechnol 35(10):937–953
Hall D, Edskes H (2012) Computational modeling of the relationship between amyloid and disease. Biophys Rev 4(3):205–222
Hall D, Edskes H (2009) A model of amyloid’s role in disease based on fibril fracture. Biophys Chem 145(1):17–28
Han F, Wang W, Chen C (2015) Research progress in animal models and stem cell therapy for Alzheimer’s disease. J Neuro-Oncol 3:11–22
Han X, He G (2018) Toward a rational design to regulate β-amyloid fibrillation for Alzheimer’s disease treatment. ACS Chem Neurosci 9(2):198–210
Handattu SP, Garber DW, Monroe CE, van Groen T, Kadish I, Nayyar G, Cao D, Palgunachari MN, Li L, Anantharamaiah G (2009) Oral apolipoprotein AI mimetic peptide improves cognitive function and reduces amyloid burden in a mouse model of Alzheimer’s disease. Neurobiol Dis 34(3):525–534
Hardy J, Selkoe DJ (2002) The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 297(5580):353–356
Henke H, Lang W (1983) Cholinergic enzymes in neocortex, hippocampus and basal forebrain of non-neurological and senile dementia of Alzheimer-type patients. Brain Res 267(2):281–291
Hochdörffer K, März-Berberich J, Nagel-Steger L, Epple M, Meyer-Zaika W, Horn AH, Sticht H, Sinha S, Bitan G, Schrader T (2011) Rational design of β-sheet ligands against Aβ42-induced toxicity. J Am Chem Soc 133(12):4348–4358
Hu X, Zhang Q, Wang W, Yuan Z, Zhu X, Chen B, Chen X (2016) Tripeptide GGH as the inhibitor of copper-amyloid-β-mediated redox reaction and toxicity. ACS Chem Neurosci 7(9):1255–1263
Ignatius MJ, Gebicke-Härter PJ, Skene J, Schilling JW, Weisgraber KH, Mahley RW, Shooter EM (1986) Expression of apolipoprotein E during nerve degeneration and regeneration. Proc Natl Acad Sci 83(4):1125–1129
Ikeda K, Okada T, Sawada S-i, Akiyoshi K, Matsuzaki K (2006) Inhibition of the formation of amyloid β-protein fibrils using biocompatible nanogels as artificial chaperones. FEBS Lett 580(28-29):6587–6595
Jagota S, Rajadas J (2013) Synthesis of d-amino acid peptides and their effect on beta-amyloid aggregation and toxicity in transgenic Caenorhabditis elegans. Med Chem Res 22(8):3991–4000
Jaruszewski KM, Omtri RS, Kandimalla KK (2012) Role of nanotechnology in the diagnosis and treatment of Alzheimer’s. Curr Adv Med Appl Nanotechnol 107
Jayasena T, Poljak A, Smythe G, Braidy N, Muench G, Sachdev P (2013) The role of polyphenols in the modulation of sirtuins and other pathways involved in Alzheimer’s disease. Ageing Res Rev 12(4):867–883
Ji Y, Lee HJ, Kim M, Nam G, Lee SJC, Cho J, Park C-M, Lim MH (2017) Strategic design of 2, 2′-bipyridine derivatives to modulate metal–amyloid-β aggregation. Inorg Chem 56(11):6695–6705
Jiang Z, Dong X, Liu H, Wang Y, Zhang L, Sun Y (2016) Multifunctionality of self-assembled nanogels of curcumin-hyaluronic acid conjugates on inhibiting amyloid β-protein fibrillation and cytotoxicity. React Funct Polym 104:22–29
Jiang Z, Dong X, Sun Y (2018) Charge effects of self-assembled chitosan-hyaluronic acid nanoparticles on inhibiting amyloid β-protein aggregation. Carbohydr Res 461:11–18
John T, Gladytz A, Kubeil C, Martin LL, Risselada HJ, Abel B (2018) Impact of nanoparticles on amyloid peptide and protein aggregation: a review with a focus on gold nanoparticles. Nanoscale 10(45):20894–20913
Joshi SA, Chavhan SS, Sawant KK (2010) Rivastigmine-loaded PLGA and PBCA nanoparticles: preparation, optimization, characterization, in vitro and pharmacodynamic studies. Eur J Pharm Biopharm 76(2):189–199
Kawashima H, Sohma Y, Nakanishi T, Kitamura H, Mukai H, Yamashita M, Akaji K, Kiso Y (2013) A new class of aggregation inhibitor of amyloid-β peptide based on an O-acyl isopeptide. Bioorg Med Chem 21(21):6323–6327
Kino R, Araya T, Arai T, Sohma Y, Kanai M (2015) Covalent modifier-type aggregation inhibitor of amyloid-β based on a cyclo-KLVFF motif. Bioorg Med Chem Lett 25(15):2972–2975
Klein AN, Ziehm T, Tusche M, Buitenhuis J, Bartnik D, Boeddrich A, Wiglenda T, Wanker E, Funke SA, Brener O (2016) Optimization of the all-D peptide D3 for Aβ oligomer elimination. PLoS One 11(4):e0153035
Knopman DS (2016) Alzheimer disease: preclinical Alzheimer disease—the new frontier. Nat Rev Neurol 12(11):620
Kogan MJ, Bastus NG, Amigo R, Grillo-Bosch D, Araya E, Turiel A, Labarta A, Giralt E, Puntes VF (2006) Nanoparticle-mediated local and remote manipulation of protein aggregation. Nano Lett 6(1):110–115
Kokkoni N, Stott K, Amijee H, Mason JM, Doig AJ (2006) N-Methylated peptide inhibitors of β-amyloid aggregation and toxicity. Optimization of the inhibitor structure. Biochemistry 45(32):9906–9918
Kumaraswamy P, Sethuraman S, Krishnan UM (2012) Liposomal delivery of a beta sheet blocker peptide for the treatment of Alzheimer’s disease. Alzheimer’s Dement: J Alzheimer’s Assoc 8(4):P705
Laganowsky A, Liu C, Sawaya MR, Whitelegge JP, Park J, Zhao M, Pensalfini A, Soriaga AB, Landau M, Teng PK (2012) Atomic view of a toxic amyloid small oligomer. Science 335(6073):1228–1231
Larbanoix L, Burtea C, Ansciaux E, Laurent S, Mahieu I, Vander Elst L, Muller RN (2011) Design and evaluation of a 6-mer amyloid-beta protein derived phage display library for molecular targeting of amyloid plaques in Alzheimer’s disease: comparison with two cyclic heptapeptides derived from a randomized phage display library. Peptides 32(6):1232–1243
Leithold LH, Jiang N, Post J, Niemietz N, Schartmann E, Ziehm T, Kutzsche J, Shah NJ, Breitkreutz J, Langen K-J (2016) Pharmacokinetic properties of tandem d-peptides designed for treatment of Alzheimer’s disease. Eur J Pharm Sci 89:31–38
Lemkul JA, Bevan DR (2012) The role of molecular simulations in the development of inhibitors of amyloid β-peptide aggregation for the treatment of Alzheimer’s disease. ACS Chem Neurosci 3(11):845–856
Li H, Du Z, Lopes DH, Fradinger EA, Wang C, Bitan G (2011a) C-terminal tetrapeptides inhibit Aβ42-induced neurotoxicity primarily through specific interaction at the N-terminus of Aβ42. J Med Chem 54(24):8451–8460
Li H, Luo Y, Derreumaux P, Wei G (2011b) Carbon nanotube inhibits the formation of β-sheet-rich oligomers of the Alzheimer’s amyloid-β (16-22) peptide. Biophys J 101(9):2267–2276
Li M, Guan Y, Ding C, Chen Z, Ren J, Qu X (2016) An ultrathin graphitic carbon nitride nanosheet: a novel inhibitor of metal-induced amyloid aggregation associated with Alzheimer’s disease. J Mater Chem B 4(23):4072–4075
Li X, Xie B, Dong X, Sun Y (2018) Bifunctionality of iminodiacetic acid-modified lysozyme on inhibiting Zn2+-mediated amyloid β-protein aggregation. Langmuir 34(17):5106–5115
Liao YH, Chang YJ, Yoshiike Y, Chang YC, Chen YR (2012) Negatively charged gold nanoparticles inhibit Alzheimer’s amyloid-β fibrillization, induce fibril dissociation, and mitigate neurotoxicity. Small 8(23):3631–3639
Liu, F., W. Wang, J. Sang, L. Jia and F. Lu (2018). Hydroxylated single-walled carbon nanotubes inhibit Aβ42 fibrillogenesis, disaggregate mature fibrils, and protect against Aβ42-induced cytotoxicity. ACS Chem Neurosci
Liu G, Men P, Harris PL, Rolston RK, Perry G, Smith MA (2006) Nanoparticle iron chelators: a new therapeutic approach in Alzheimer disease and other neurologic disorders associated with trace metal imbalance. Neurosci Lett 406(3):189–193
Liu H, Dong X, Liu F, Zheng J, Sun Y (2017a) Iminodiacetic acid-conjugated nanoparticles as a bifunctional modulator against Zn2+-mediated amyloid β-protein aggregation and cytotoxicity. J Colloid Interface Sci 505:973–982
Liu H, Xie B, Dong X, Zhang L, Wang Y, Liu F, Sun Y (2016) Negatively charged hydrophobic nanoparticles inhibit amyloid β-protein fibrillation: the presence of an optimal charge density. React Funct Polym 103:108–116
Liu H, Yu L, Dong X, Sun Y (2017b) Synergistic effects of negatively charged hydrophobic nanoparticles and (−)-epigallocatechin-3-gallate on inhibiting amyloid β-protein aggregation. J Colloid Interface Sci 491:305–312
Liu J, Wang W, Zhang Q, Zhang S, Yuan Z (2014) Study on the efficiency and interaction mechanism of a decapeptide inhibitor of β-amyloid aggregation. Biomacromolecules 15(3):931–939
Liu S, Zhao J, Li K, Wan K, Sun T, Zheng N, Zhu F, Ma J, Jiao J, Li T, Ni J (2019a) Organoplatinum-substituted polyoxometalate inhibits β-amyloid aggregation for Alzheimer’s therapy. Angew Chem
Liu, W., X. Dong and Y. Sun (2019b). D-Enantiomeric RTHLVFFARK-NH2: a potent multifunctional decapeptide inhibiting Cu2+-mediated amyloid β-protein aggregation and remodeling Cu2+-mediated amyloid β aggregates. ACS Chem Neurosci
Liu Z, Li X, Wu X, Zhu C (2019c) A dual-inhibitor system for the effective antifibrillation of Aβ40 peptides by biodegradable EGCG–Fe (iii)/PVP nanoparticles. J Mater Chem B 7(8):1292–1299
Lott IT, Dierssen M (2010) Cognitive deficits and associated neurological complications in individuals with Down’s syndrome. Lancet Neurol 9(6):623–633
Loureiro JA, Crespo R, Börner H, Martins PM, Rocha FA, Coelho M, Pereira MC, Rocha S (2014) Fluorinated beta-sheet breaker peptides. J Mater Chem B 2(16):2259–2264
Luheshi LM, Hoyer W, de Barros TP, van Dijk Härd I, Brorsson A-C, Macao B, Persson C, Crowther DC, Lomas DA, Ståhl S (2010) Sequestration of the Aβ peptide prevents toxicity and promotes degradation in vivo. PLoS Biol 8(3):e1000334
Lührs T, Ritter C, Adrian M, Riek-Loher D, Bohrmann B, Döbeli H, Schubert D, Riek R (2005) 3D structure of Alzheimer’s amyloid-β (1–42) fibrils. Proc Natl Acad Sci 102(48):17342–17347
Luo J, Abrahams JP (2014) Cyclic peptides as inhibitors of amyloid fibrillation. Chem Eur J 20(9):2410–2419
Mahmoudi M, Akhavan O, Ghavami M, Rezaee F, Ghiasi SMA (2012) Graphene oxide strongly inhibits amyloid beta fibrillation. Nanoscale 4(23):7322–7325
Mandel S, Amit T, Bar-Am O, Youdim MB (2007) Iron dysregulation in Alzheimer’s disease: multimodal brain permeable iron chelating drugs, possessing neuroprotective-neurorescue and amyloid precursor protein-processing regulatory activities as therapeutic agents. Prog Neurobiol 82(6):348–360
Mandelkow E-M, Mandelkow E (1998) Tau in Alzheimer’s disease. Trends Cell Biol 8(11):425–427
Marambaud P, Zhao H, Davies P (2005) Resveratrol promotes clearance of Alzheimer’s disease amyloid-β peptides. J Biol Chem 280(45):37377–37382
Martin TD, Malagodi AJ, Chi EY, Evans DG (2018) Computational study of the driving forces and dynamics of curcumin binding to amyloid-β protofibrils. J Phys Chem B 123(3):551–560
Martínez A, Alcendor R, Rahman T, Podgorny M, Sanogo I, McCurdy R (2016) Ionophoric polyphenols selectively bind Cu2+, display potent antioxidant and anti-amyloidogenic properties, and are non-toxic toward Tetrahymena thermophila. Bioorg Med Chem 24(16):3657–3670
Matsuoka Y, Jouroukhin Y, Gray AJ, Ma L, Hirata-Fukae C, Li H-F, Feng L, Lecanu L, Walker BR, Planel E (2008) A neuronal microtubule-interacting agent, NAPVSIPQ, reduces tau pathology and enhances cognitive function in a mouse model of Alzheimer’s disease. J Pharmacol Exp Ther 325(1):146–153
Mattson MP (2004) Pathways towards and away from Alzheimer’s disease. Nature 430(7000):631
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34(7):939–939
Mehrazma B, Opare S, Petoyan A, Rauk A (2018) D-Amino acid pseudopeptides as potential amyloid-beta aggregation inhibitors. Molecules 23(9):2387
Mehta, M., A. Adem and M. Sabbagh (2012) New acetylcholinesterase inhibitors for Alzheimer’s disease. Int J Alzheimers Dis
Meng J, Zhang H, Dong X, Liu F, Sun Y (2018) RTHLVFFARK-NH2: a potent and selective modulator on Cu2+-mediated amyloid-β protein aggregation and cytotoxicity. J Inorg Biochem 181:56–64
Minicozzi V, Chiaraluce R, Consalvi V, Giordano C, Narcisi C, Punzi P, Rossi GC, Morante S (2014) Computational and experimental studies on β-sheet breakers targeting Aβ1–40 fibrils. J Biol Chem 289(16):11242–11252
Moore KA, Pate KM, Soto-Ortega DD, Lohse S, van der Munnik N, Lim M, Jackson KS, Lyles VD, Jones L, Glassgow N (2017) Influence of gold nanoparticle surface chemistry and diameter upon Alzheimer’s disease amyloid-β protein aggregation. J Biol Eng 11(1):5
Necula M, Kayed R, Milton S, Glabe CG (2007) Small molecule inhibitors of aggregation indicate that amyloid β oligomerization and fibrillization pathways are independent and distinct. J Biol Chem 282(14):10311–10324
Nie Q, Du X-g, Geng M-y (2011) Small molecule inhibitors of amyloid β peptide aggregation as a potential therapeutic strategy for Alzheimer’s disease. Acta Pharmacol Sin 32(5):545
Ono K, Hasegawa K, Naiki H, Yamada M (2004) Curcumin has potent anti-amyloidogenic effects for Alzheimer’s β-amyloid fibrils in vitro. J Neurosci Res 75(6):742–750
Oliveri V, Francesco B, Graziella V (2017) Structural isomers of cyclodextrin-bearing IOX1 compound as inhibitors of Aβ aggregation. Chem Select 2(2):655–659
Pansieri J, Gerstenmayer M, Lux F, Mériaux S, Tillement O, Forge V, Larrat B, Marquette C (2018) Magnetic nanoparticles applications for amyloidosis study and detection: a review. Nanomaterials 8(9):740
Parthsarathy V, McClean PL, Hölscher C, Taylor M, Tinker C, Jones G, Kolosov O, Salvati E, Gregori M, Masserini M (2013) A novel retro-inverso peptide inhibitor reduces amyloid deposition, oxidation and inflammation and stimulates neurogenesis in the APPswe/PS1ΔE9 mouse model of Alzheimer’s disease. PLoS One 8(1):e54769
Pedersen JT, Borg CB, Michaels TC, Knowles TP, Faller P, Teilum K, Hemmingsen L (2015) Aggregation-prone amyloid-β· CuII species formed on the millisecond timescale under mildly acidic conditions. ChemBioChem 16(9):1293–1297
Petkova AT, Ishii Y, Balbach JJ, Antzutkin ON, Leapman RD, Delaglio F, Tycko R (2002) A structural model for Alzheimer’s β-amyloid fibrils based on experimental constraints from solid state NMR. Proc Natl Acad Sci 99(26):16742–16747
Podolski IY, Podlubnaya Z, Kosenko E, Mugantseva E, Makarova E, Marsagishvili L, Shpagina M, Kaminsky YG, Andrievsky G, Klochkov V (2007) Effects of hydrated forms of C60 fullerene on amyloid β-peptide fibrillization in vitro and performance of the cognitive task. J Nanosci Nanotechnol 7(4-5):1479–1485
Porat Y, Abramowitz A, Gazit E (2006) Inhibition of amyloid fibril formation by polyphenols: structural similarity and aromatic interactions as a common inhibition mechanism. Chem Biol Drug Des 67(1):27–37
Prince, MJ (2015) World Alzheimer Report 2015: the global impact of dementia: an analysis of prevalence, incidence, cost and trends. Alzheimer's Disease International 2015. https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf
Prince M, Comas-Herrera A, Knapp M, Guerchet M and Karagiannidou M (2016). World Alzheimer report 2016: improving healthcare for people living with dementia: coverage, quality and costs now and in the future
Ramaswamy K, Kumaraswamy P, Sethuraman S, Krishnan UM (2014) Self-assembly characteristics of a structural analogue of Tjernberg peptide. RSC Adv 4(32):16517–16523
Rana M, Cho H-J, Roy TK, Mirica LM, Sharma AK (2018) Azo-dyes based small bifunctional molecules for metal chelation and controlling amyloid formation. Inorg Chim Acta 471:419–429
Rao PP, Mohamed T, Teckwani K, Tin G (2015) Curcumin binding to beta amyloid: a computational study. Chem Biol Drug Des 86(4):813–820
Reddy G, Straub JE, Thirumalai D (2009) Influence of preformed asp23− lys28 salt bridge on the conformational fluctuations of monomers and dimers of Aβ peptides with implications for rates of fibril formation. J Phys Chem B 113(4):1162–1172
Reiman EM (2016) Alzheimer’s disease: attack on amyloid-β protein. Nature 537(7618):36
Reinke AA, Gestwicki JE (2007) Structure–activity relationships of amyloid beta-aggregation inhibitors based on curcumin: influence of linker length and flexibility. Chem Biol Drug Des 70(3):206–215
Ren B, Jiang B, Hu R, Zhang M, Chen H, Ma J, Sun Y, Jia L, Zheng J (2016) HP-β-cyclodextrin as an inhibitor of amyloid-β aggregation and toxicity. Phys Chem Chem Phys 18(30):20476–20485
Ren B, Zhang M, Hu R, Chen H, Wang M, Lin Y, Sun Y, Jia L, Liang G, Zheng J (2017) Identification of a new function of cardiovascular disease drug 3-morpholinosydnonimine hydrochloride as an amyloid-β aggregation inhibitor. ACS Omega 2(1):243–250
Rezai-Zadeh K, Shytle D, Sun N, Mori T, Hou H, Jeanniton D, Ehrhart J, Townsend K, Zeng J, Morgan D (2005) Green tea epigallocatechin-3-gallate (EGCG) modulates amyloid precursor protein cleavage and reduces cerebral amyloidosis in Alzheimer transgenic mice. J Neurosci 25(38):8807–8814
Richman M, Wilk S, Chemerovski M, Wärmländer SK, Wahlström A, Gräslund A, Rahimipour S (2013) In vitro and mechanistic studies of an antiamyloidogenic self-assembled cyclic d, l-α-peptide architecture. J Am Chem Soc 135(9):3474–3484
Rigacci S, Guidotti V, Bucciantini M, Nichino D, Relini A, Berti A, Stefani M (2011) Aβ (1-42) aggregates into non-toxic amyloid assemblies in the presence of the natural polyphenol oleuropein aglycon. Curr Alzheimer Res 8(8):841–852
Ringman JM, Frautschy SA, Teng E, Begum AN, Bardens J, Beigi M, Gylys KH, Badmaev V, Heath DD, Apostolova LG (2012) Oral curcumin for Alzheimer’s disease: tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimers Res Ther 4(5):43
Ritchie CW, Bush AI, Mackinnon A, Macfarlane S, Mastwyk M, MacGregor L, Kiers L, Cherny R, Li Q-X, Tammer A (2003) Metal-protein attenuation with iodochlorhydroxyquin (clioquinol) targeting Aβ amyloid deposition and toxicity in Alzheimer disease: a pilot phase 2 clinical trial. Arch Neurol 60(12):1685–1691
Rossor M, Emson P, Mountjoy C, Roth M, Iversen L (1980) Reduced amounts of immunoreactive somatostatin in the temporal cortex in senile dementia of Alzheimer type. Neurosci Lett 20(3):373–377
Rossor M, Revesz T, Lantos P, Warrington EK (2000) Semantic dementia with ubiquitin-positive tau-negative inclusion bodies. Brain 123(2):267–276
Sahni JK, Doggui S, Ali J, Baboota S, Dao L, Ramassamy C (2011) Neurotherapeutic applications of nanoparticles in Alzheimer’s disease. J Control Release 152(2):208–231
Salvati A, Pitek AS, Monopoli MP, Prapainop K, Bombelli FB, Hristov DR, Kelly PM, Åberg C, Mahon E, Dawson KA (2013) Transferrin-functionalized nanoparticles lose their targeting capabilities when a biomolecule corona adsorbs on the surface. Nat Nanotechnol 8(2):137
Sastre M, Ritchie CW, Hajji N (2015) Metal ions in Alzheimer’s disease brain. JSM Alzheimer’s Dis Relat Dement 2:1014
Savelieff MG, Nam G, Kang J, Lee HJ, Lee M, Lim MH (2018) Development of multifunctional molecules as potential therapeutic candidates for Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis in the last decade. Chem Rev 119(2):1221–1322
Scherzer-Attali R, Pellarin R, Convertino M, Frydman-Marom A, Egoz-Matia N, Peled S, Levy-Sakin M, Shalev DE, Caflisch A, Gazit E (2010) Complete phenotypic recovery of an Alzheimer’s disease model by a quinone-tryptophan hybrid aggregation inhibitor. PLoS One 5(6):e11101
Schöneich C, Williams TD (2002) Cu (II)-catalyzed oxidation of β-amyloid peptide targets His13 and His14 over His6: detection of 2-Oxo-histidine by HPLC-MS/MS. Chem Res Toxicol 15(5):717–722
Selkoe DJ (2001) Alzheimer’s disease: genes, proteins, and therapy. Physiol Rev 81(2):741–766
Shamloo A, Asadbegi M, Khandan V, Amanzadi A (2018) Designing a new multifunctional peptide for metal chelation and Aβ inhibition. Arch Biochem Biophys 653:1–9
Sharma S, Nehru B, Saini A (2017) Inhibition of Alzheimer’s amyloid-beta aggregation in-vitro by carbenoxolone: insight into mechanism of action. Neurochem Int 108:481–493
Shuaib S, Goyal B (2018) Scrutiny of the mechanism of small molecule inhibitor preventing conformational transition of amyloid-β42 monomer: insights from molecular dynamics simulations. J Biomol Struct Dyn 36(3):663–678
Singer O, Marr RA, Rockenstein E, Crews L, Coufal NG, Gage FH, Verma IM, Masliah E (2005) Targeting BACE1 with siRNAs ameliorates Alzheimer disease neuropathology in a transgenic model. Nat Neurosci 8(10):1343
Sloane PD, Zimmerman S, Suchindran C, Reed P, Wang L, Boustani M, Sudha S (2002) The public health impact of Alzheimer’s disease, 2000–2050: potential implication of treatment advances. Annu Rev Public Health 23
Sohma Y (2016) Medicinal chemistry focusing on aggregation of amyloid-β. Chem Pharm Bull 64(1):1–7
Soininen H, Kosunen O, Helisalmi S, Mannermaa A, Paljärvi L, Talasniemi S, Ryynänen M, Riekkinen P Sr (1995) A severe loss of choline acetyltransferase in the frontal cortex of Alzheimer patients carrying apolipoprotein ε4 allele. Neurosci Lett 187(2):79–82
Soltani N, Gholami MR (2017) Increase in the β-sheet character of an amyloidogenic peptide upon adsorption onto gold and silver surfaces. ChemPhysChem 18(5):526–536
Sood S, Jain K, Gowthamarajan K (2014) Intranasal therapeutic strategies for management of Alzheimer’s disease. J Drug Target 22(4):279–294
Soto C, Kindy MS, Baumann M, Frangione B (1996) Inhibition of Alzheimer’s amyloidosis by peptides that prevent β-sheet conformation. Biochem Biophys Res Commun 226(3):672–680
Soto C, Sigurdsson EM, Morelli L, Kumar RA, Castaño EM, Frangione B (1998) β-Sheet breaker peptides inhibit fibrillogenesis in a rat brain model of amyloidosis: implications for Alzheimer’s therapy. Nat Med 4(7):822–826
Su T, Zhang T, Xie S, Yan J, Wu Y, Li X, Huang L, Luo H-B (2016) Discovery of novel PDE9 inhibitors capable of inhibiting Aβ aggregation as potential candidates for the treatment of Alzheimer’s disease. Sci Rep 6:21826
Sudhakar S, Kalipillai P, Santhosh PB, Mani E (2017) Role of surface charge of inhibitors on amyloid beta fibrillation. J Phys Chem C 121(11):6339–6348
Sun N, Funke AS, Willbold D (2012) A survey of peptides with effective therapeutic potential in Alzheimer’s disease rodent models or in human clinical studies. Mini-Rev Med Chem 12(5):388–398
Tamaoka A, Sawamura N, Fukushima T, Shoji S, Matsubara E, Shoji M, Hirai S, Furiya Y, Endoh R, Mori H (1997) Amyloid β protein 42 (43) in cerebrospinal fluid of patients with Alzheimer’s disease. J Neurol Sci 148(1):41–45
Taylor M, Moore S, Mayes J, Parkin E, Beeg M, Canovi M, Gobbi M, Mann DM, Allsop D (2010) Development of a proteolytically stable retro-inverso peptide inhibitor of β-amyloid oligomerization as a potential novel treatment for Alzheimer’s disease. Biochemistry 49(15):3261–3272
Tjernberg LO, Näslund J, Lindqvist F, Johansson J, Karlström AR, Thyberg J, Terenius L, Nordstedt C (1996) Arrest of-amyloid fibril formation by a pentapeptide ligand. J Biol Chem 271(15):8545–8548
Török M, Abid M, Mhadgut SC, Török B (2006) Organofluorine inhibitors of amyloid fibrillogenesis. Biochemistry 45(16):5377–5383
Urbanc B, Cruz L, Yun S, Buldyrev SV, Bitan G, Teplow DB, Stanley HE (2004) In silico study of amyloid β-protein folding and oligomerization. Proc Natl Acad Sci 101(50):17345–17350
Van Groen T, Wiesehan K, Funke SA, Kadish I, Nagel-Steger L, Willbold D (2008) Reduction of Alzheimer’s disease amyloid plaque load in transgenic mice by D3, ad-enantiomeric peptide identified by mirror image phage display. ChemMedChem: Chem Enabling Drug Discov 3(12):1848–1852
Villari V, Tosto R, Di Natale G, Sinopoli A, Tomasello MF, Lazzaro S, Micali N, Pappalardo G (2017) A metalloporphyrin-peptide conjugate as an effective inhibitor of amyloid-β peptide fibrillation and cytotoxicity. ChemistrySelect 2(28):9122–9129
Walsh DM, Selkoe DJ (2007) Aβ oligomers–a decade of discovery. J Neurochem 101(5):1172–1184
Wang D, Zhang Q, Hu X, Wang W, Zhu X, Yuan Z (2018) Pharmacodynamics in Alzheimer’s disease model rats of a bifunctional peptide with the potential to accelerate the degradation and reduce the toxicity of amyloid β-Cu fibrils. Acta Biomater 65:327–338
Wang L, Zeng R, Pang X, Gu Q, Tan W (2015) The mechanisms of flavonoids inhibiting conformational transition of amyloid-β 42 monomer: a comparative molecular dynamics simulation study. RSC Adv 5(81):66391–66402
Wang W, Han Y, Fan Y, Wang Y (2019) Effects of gold nanospheres and nanocubes on amyloid-β peptide fibrillation. Langmuir.
Wells JA, McClendon CL (2007) Reaching for high-hanging fruit in drug discovery at protein–protein interfaces. Nature 450(7172):1001
Wiesehan K, Buder K, Linke RP, Patt S, Stoldt M, Unger E, Schmitt B, Bucci E, Willbold D (2003) Selection of D-amino-acid peptides that bind to Alzheimer’s disease amyloid peptide Aβ1–42 by mirror image phage display. Chembiochem 4(8):748–753
Wimo A, Jönsson L, Bond J, Prince M, Winblad B, A. D. International (2013) The worldwide economic impact of dementia 2010. Alzheimers Dement 9(1):1–11. e13
Wisniewski H, Wegiel J (1995) The neuropathology of Alzheimer’s disease. Neuroimaging Clin N Am 5(1):45–57
Wood SJ, Wetzel R, Martin JD, Hurle MR (1995) Prolines and aamyloidogenicity in fragments of the Alzheimer’s peptide. beta./A4. Biochemistry 34(3):724–730
Xiong N, Dong X-Y, Zheng J, Liu F-F, Sun Y (2015) Design of LVFFARK and LVFFARK-functionalized nanoparticles for inhibiting amyloid β-protein fibrillation and cytotoxicity. ACS Appl Mater Interfaces 7(10):5650–5662
Xiong N, Zhao Y, Dong X, Zheng J, Sun Y (2017) Design of a molecular hybrid of dual peptide inhibitors coupled on AuNPs for enhanced inhibition of amyloid β-protein aggregation and cytotoxicity. Small 13(13):1601666
Yan LM, Velkova A, Tatarek-Nossol M, Rammes G, Sibaev A, Andreetto E, Kracklauer M, Bakou M, Malideli E, Göke B (2013) Selectively N-methylated soluble IAPP mimics as potent IAPP receptor agonists and nanomolar inhibitors of cytotoxic self-assembly of both IAPP and Aβ40. Angew Chem Int Ed 52(39):10378–10383
Yang F, Lim GP, Begum AN, Ubeda OJ, Simmons MR, Ambegaokar SS, Chen PP, Kayed R, Glabe CG, Frautschy SA (2005) Curcumin inhibits formation of amyloid β oligomers and fibrils, binds plaques, and reduces amyloid in vivo. J Biol Chem 280(7):5892–5901
Yang X, Cai P, Liu Q, Wu J, Yin Y, Wang X, Kong L (2018) Novel 8-hydroxyquinoline derivatives targeting β-amyloid aggregation, metal chelation and oxidative stress against Alzheimer’s disease. Bioorg Med Chem 26(12):3191–3201
Yang Y, Chen T, Zhu S, Gu X, Jia X, Lu Y, Zhu L (2015) Two macrocyclic polyamines as modulators of metal-mediated Aβ40 aggregation. Integr Biol 7(6):655–662
Yang W, Wong Y, Ng OT, Bai LP, Kwong DW, Ke Y, Jiang ZH, Li HW, Yung KK, Wong MS (2012) Inhibition of beta-amyloid peptide aggregation by multifunctional carbazole-based fluorophores. Angew Chem Int Ed 51(8):1804–1810
Yoo SI, Yang M, Vivekanandan Subramanian D, Brender JR, Sun K, Joo NE, Jeong S-H, Ramamoorthy A, Kotov NA (2011) Mechanism of fibrillation inhibition of amyloid peptides by inorganic nanoparticles reveal functional similarities with proteins. Angew Chem Int Ed Eng 50(22):5110
Zhang H, Dong X, Liu F, Zheng J, Sun Y (2018a) Ac-LVFFARK-NH2 conjugation to β-cyclodextrin exhibits significantly enhanced performance on inhibiting amyloid β-protein fibrillogenesis and cytotoxicity. Biophys Chem 235:40–47
Zhang H, Dong X, Sun Y (2018b) Carnosine-LVFFARK-NH2 conjugate: a moderate chelator but potent inhibitor of Cu2+-mediated amyloid β-protein aggregation. ACS Chem Neurosci 9(11):2689–2700
Zhang H, Zhang C, Dong XY, Zheng J, Sun Y (2018c) Design of nonapeptide LVFFARKHH: a bifunctional agent against Cu2+-mediated amyloid β-protein aggregation and cytotoxicity. J Mol Recognit 31(6):e2697
Zhang J, Zhou X, Yu Q, Yang L, Sun D, Zhou Y, Liu J (2014) Epigallocatechin-3-gallate (EGCG)-stabilized selenium nanoparticles coated with Tet-1 peptide to reduce amyloid-β aggregation and cytotoxicity. ACS Appl Mater Interfaces 6(11):8475–8487
Zhang Q, Hu X, Wang W, Yuan Z (2016) Study of a bifunctional Aβ aggregation inhibitor with the abilities of antiamyloid-β and copper chelation. Biomacromolecules 17(2):661–668
Zhang Y x, Wang SW, Lu S, Zhang LX, Liu DQ, Ji M, Wang WY, Liu RT (2017) A mimotope of Aβ oligomers may also behave as a β-sheet inhibitor. FEBS Lett 591(21):3615–3624
Zhao G, Dong X, Sun Y (2018) Self-assembled curcumin–poly (carboxybetaine methacrylate) conjugates: potent nano-inhibitors against amyloid β-protein fibrillogenesis and cytotoxicity. Langmuir.
Zheng X, Wu C, Liu D, Li H, Bitan G, Shea J-E, Bowers MT (2015) Mechanism of C-terminal fragments of amyloid β-protein as Aβ inhibitors: do C-terminal interactions play a key role in their inhibitory activity? J Phys Chem B 120(8):1615–1623
Zhu L, Han Y, He C, Huang X, Wang Y (2014) Disaggregation ability of different chelating molecules on copper ion-triggered amyloid fibers. J Phys Chem B 118(31):9298–9305
Zou Y, Qian Z, Chen Y, Qian H, Wei G, Zhang Q (2019) Norepinephrine inhibits Alzheimer’s amyloid-β peptide aggregation and destabilizes amyloid-β protofibrils: a molecular dynamics simulation study. ACS Chem Neurosci
Acknowledgments
We would like to thank the Editorial Board Members of the Biophysical Reviews journal for their help in improving the clarity of expression of our manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jokar, S., Khazaei, S., Behnammanesh, H. et al. Recent advances in the design and applications of amyloid-β peptide aggregation inhibitors for Alzheimer’s disease therapy. Biophys Rev 11, 901–925 (2019). https://doi.org/10.1007/s12551-019-00606-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12551-019-00606-2