Abstract
Background
The study of the COVID-19 disease consequences on healthcare professionals’ mental health has drawn a great interest in psychology and other behavioral sciences. Previous studies mainly focused on professionals’ health in terms of psychopathology, therefore, there is no research examining their positive mental health during both the first and the second wave. Also, there is no research studying healthcare professionals’ social recognition during the pandemic and the influence of this variable on professionals’ positive health.
Methods
Following the WHO’s recommendations, our objective was to measure pathology (i.e., anxiety and traumatic intensity), positive health (i.e., Hedonic, Psychological and Social Well-being) and social recognition in a sample of 200 healthcare professionals in the frontline care of Covid-19 patients.
Results
In both waves, participants showed high levels of anxiety and traumatic intensity, although, as expected, in the second (vs. the first) wave psychopathological symptoms decreased. Concerning positive health indicators, in the second wave, health professionals showed more hedonic and psychological well-being than in the first one. However, in the second wave social well-being was lower than in the first wave, an expected though apparently paradoxical result, linked to the decrease in healthcare professionals’ social recognition between the first and the second wave. In fact, bootstrapping procedures and Sobel Test confirm the mediating role of social recognition on the effect of Covid-19 wave on social well-being.
Conclusions
Public institutions, governments, and society in general, should recognize health professionals’ work, given that social recognition is a fundamental protection factor for social well-being.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The study of the COVID-19 disease consequences on mental health has drawn a great interest in psychology and other behavioral sciences. For example, according to different studies, COVID-19 has caused an increase in psychopathological symptoms in the general population, specifically problems related to anxiety disorders and trauma and stressor-related disorders [1,2,3,4]. However, the effect of the pandemic on general population’s positive mental health has been studied to a much lesser degree [5,6,7,8]. In this sense, results indicate that COVID-19 has reduced general population’s well-being, mainly during isolation. Moreover, quality of life of vulnerable people (e.g., people with physical or mental multimorbidity, people who live alone, etc.) was the most intensely affected [9].
Beyond the effects of COVID-19 on general population, health professionals are being particularly affected by COVID-19 for various reasons. For example, during the first wave of COVID-19, frontline healthcare professionals were living in a constant COVID-19 disease exposure without appropriate Personal Protection Equipment (PPE), showing high levels of anxiety and traumatic intensity [10]. In this sense, different studies have already examined the mental health of this specific population, although, as in the case of the general population, mainly from a pathological perspective [11,12,13,14,15,16]. These studies indicate a significant impact of the COVID-19 pandemic on healthcare professionals’ mental health, with an increase in anxiety, traumatic and depressive symptoms [15]. Despite the growing interest in studying healthcare professionals’ mental health, only a few empirical studies have evaluated their positive mental health, indicating a strong deterioration of their wellbeing [10, 17]. In sum, previous research conducted during the first wave indicates that COVID-19 has seriously affected healthcare professionals’ mental health, both from a psychopathology-based perspective and from a positive mental health perspective [10,11,12,13,14,15,16,17].
Since first wave, various aspects related to the pandemic that could affect health workers changed. For example, in countries like Spain, in the second wave, all frontline health workers had access to the appropriate PPE or to COVID-19 vaccines. Also, scientific knowledge related to COVID-19 increased, generating a greater sense of control in clinical practice. Moreover, in the second wave health authorities developed COVID-19 contingency plans, especially focused on human resources, to reduce work overload, although the number of professionals remained insufficient in some services, such as in Intensive Care Units. Finally, another important aspect related to the pandemic that changed in subsequent waves is the social recognition of health professionals. During the first wave, people, institutions, and governments showed signs of admiration and gratitude to health professionals’ work. As an example of this social recognition in Spain, people applauded, every day at 8:00 p.m. from March 14, 2020 to May 17, 2020, from their windows and balconies to show their gratitude to health professionals. Although a few stigmatizing behaviors appeared (e.g., health professionals’ neighbors forced them to change their residence due to fear of infection), these acts were infrequent. In the second wave, however, spontaneous gestures of gratitude disappeared, stigmatizing behaviors increased, and the Spanish population began to blame health workers for the collapse in medical care system caused by COVID-19, such as delays in appointments, inability to obtain face-to-face medical care or long waiting time for surgeries. These changes in health professionals’ social recognition are highly relevant to their wellbeing [18] because it is essential for workers to feel that they are an important part of society (a core factor of social integration) [19, 20] and vital members making a valuable contribution to the society (a core factor of social contribution) [21].
Thus, given that various conditions changed since the first wave, it is necessary to study health workers’ mental health in subsequent waves. However, the few studies that analyzed the effect of the COVID-19 s wave on health professionals used only a pathological perspective [22, 23]. That is, to the best of our knowledge, there is no study examining healthcare professionals’ positive mental health during the second wave. Also, there is no previous research examining the social recognition changes between the first and the second wave and the potential influence of this variable in professionals’ positive health.
The Present Study
Following the recommendations of the World Health Organization (WHO) [24], in our study we pretend to analyze health workers’ mental health during the first and second waves of the COVID-19 pandemic in Spain, not only from a psychopathological perspective, but also from a positive mental health perspective using well-being indicators [25]. Specifically, to evaluate well-being we used the Complete State Model of Health (CSMH) [26], according to which mental illness and positive mental health reflect distinct continua, instead of the extreme ends of a single dimension. To operationalize positive mental health, the CSMH proposes the constructs of Hedonic Well-being (HWB) (subjective evaluation of life via satisfaction and positive affect indicators), Psychological Well-being (PWB) (optimal psychological functioning and experience indicators), and Social Well-being (SoWB) (functioning in society indicators).
The purpose of the present study was to examine (1) health workers’ pathology (i.e., anxiety and traumatic intensity), positive mental health (i.e., well-being), and social recognition differences between first and second COVID-19 waves in Spain, (2) the relationships between pathology and positive mental health of these professionals in both waves, and (3) the role of perceived social recognition on health workers’ positive health. In relation to the first purpose, the present study hypothesized that (H1.1) according the forementioned changes that occurred in Spain between the two waves (e.g., guaranteed access to PPE, fully vaccinated health professionals, etc.), health workers will show lower levels of anxiety and traumatic intensity in the second wave compared to the first one. For the same reasons the present study also hypothesized that (H1.2) health workers’ levels of HWB and PWB will increase in the second wave. Finally, this study hypothesized that (H1.3) SoWB of Spanish professionals will be lower in the second wave compared to the first one. This seemingly paradoxical prediction is based on healthcare professionals’ social recognition decrease between the first and the second wave [27]. Regarding the second purpose, based on the CSMH, the present study hypothesizes that (H2.1) correlations between pathology and positive mental health indicators in both waves will be negative and significant except for SoWB in the first wave. Due to the high social recognition that professionals received in the first wave, we expected that (H2.2) in this wave more pathology does not imply less SoWB. Finally, concerning the third objective, and considering that social recognition is a key factor of SoWB [27], the present study hypothesized that (H3.1) social recognition will mediate the effect of the COVID-19 wave on health professionals’ SoWB.
Methods
Participants
In order to determine the sample size needed to detect the key main effects, we conducted an a priori power analysis using the statistical software G-Power, aiming to achieve a power of .80. In the absence of previous results in the literature, a conservative medium effect size was sought (f = .20) [28]. The results of this analysis suggested that a sample size of 199 participants was needed. Since the study has a two-group design (i.e., first wave vs. second wave), we set a sample size of 200 people (100 per condition). Therefore, two-hundred participants between 27 and 65 years old voluntarily participated in the study without compensation (M = 36.30; SD = 13.02). In the first wave condition participants were between 30 and 65 years old (M = 35.20; SD = 13.29), and in the second wave were between 27 and 62 years old (M = 37.40; SD = 12.88). There were no age differences between waves, F (1, 199) = .05, p = .83, ηp2 < .001. Participants were 134 women (67%) and 66 men (33%) (first wave: 62 women, 38 men; second wave: 72 women, 28 men). Also, there were no differences in gender between waves, χ2 = 2.26, p = .13. All participants were health professionals (total sample: doctors 110 (55%), nurses 90 (45%); first wave: doctors 52, nurses 48; second wave: doctors 58, nurses 42), in the frontline care of Covid-19 patients, who worked in public or private hospitals in the territories most affected by the first and second waves in Spain. Again, there were no differences in profession between waves, χ2 = .72, p = .39.
Procedure
Participants were recruited through letters of invitation explaining the project, the voluntary nature of participation and the strict anonymity of the results. The invitations were given to participants who met the study criteria: 1) Being health professionals; 2) Being in the frontline care of Covid-19 patients at the time of their participation in the study (i.e., having continued and direct contact with COVID-19 patients); 3) Working in a public or private hospital in Spanish regions that were more affected by the pandemic (i.e., Madrid, Castilla la Mancha, Castilla León and Catalonia). Considering that health authorities explicitly instructed healthcare professionals to avoid negative comments about the pandemic management, the perception of anonymity was essential to avoid correction bias in responses. For this reason, in the first wave participants were informed that all collected information was confidential and anonymous, and that there would be no traceability of their answers (not even by the researchers) because no identification numbers would be assigned. Consequently, a longitudinal study could not be conducted. To avoid duplications in participation, in the COVID-19 s wave condition, no invitations were sent to professionals who had already participated. In response to our invitations, in the first wave we received two hundred eighty-seven consents, and one hundred participants were selected through a simple random sampling method. In the second wave, two hundred forty-six consents were received and one hundred were selected through the same method. This study was part of a research project funded by the Spanish Ministry of Science and Innovation and was approved by the ethics committee of the “Hospital General Universitario de Ciudad Real—Universidad de Castilla La Mancha”. All participants signed an informed consent. To control possible effects due to the order of presentation, half the participants completed online first the State Trait Anxiety Inventory, followed by the Davidson Trauma Scale. Second, the Mental Health Continuum Short Form was fulfilled. The other half completed online the questionnaires in the reverse order. Finally, all participants completed the social recognition measure.
Measures
Covid Wave
In the COVID-19 first-wave condition, participants completed the study between March 27th and April 3rd, 2020, week with the greatest overload of the Spanish health system due to the number of new daily infections detected. During this period, confirmed COVID-19 cases in Spain were doubled from 64,059 to 117,710 and 2909 people with COVID-19 died [29]. In the COVID-19 s-wave condition, participants completed the study between January 20th and 27th, 2021, the week with the greatest overload in the second wave. During this second period, there were 257,027 new COVID-19 cases and 2646 deaths linked to COVID-19 [30].
Anxiety
The State Trait Anxiety Inventory (STAI) [31], validated in Spanish [32], was used to measure state anxiety. This instrument consists of two scales, trait anxiety and state anxiety, which include 20 items each (e.g., I am tense). Since the objective of the study was to analyze the effect of each COVID-19 wave on health professionals’ anxiety, we only used the state anxiety scale. Participants responded to the 20 items using a 4-point scale ranging from 0 (almost never) to 3 (almost always). As a consequence, STAI-S scores can range from 0 to 60, with higher scores indicating higher levels of anxiety. A score greater than 40 is the cut-off point that presents the highest efficiency to detect the possible presence of any anxiety disorders [33]. This scale has demonstrated good psychometric properties both in English and Spanish versions [33, 34]. In the present study, Cronbach’s α value for the STAI State scale was .93 (first wave Cronbach’s α was 92; second wave Cronbach’s α was 93).
Trauma Intensity
To measure trauma intensity during the last month previous to each COVID-19 wave, healthcare professionals answered the Davidson Trauma Scale (DTS) [35], Spanish version [36]. The instrument contains 17 self-report items linked to posttraumatic stress symptoms (e.g., Have you been avoiding any thoughts or feelings about the event?). All items correspond to the DSM-IV symptoms of Post-traumatic Stress Disorder (PTSD) (Criteria B: items 1–4 and 17; Criteria C: items 5–11, Criteria D: items 12–16). Participants rated each item in terms of both frequency and severity on 5-point (0–4) Likert scales. Total scores range from 0 to 136, with higher scores indicating higher levels of trauma intensity. A score greater than 35 is the highest efficiency cut point score, according to McDonald and colleagues criterium [37], to detect the presence of PTSD. In previous research, this instrument showed good psychometric properties [38,39,40]. In the current study, Cronbach’s α for the DTS-total score was .91 (first wave Cronbach’s α was .88; second wave Cronbach’s α was .92).
Well-being
Well-being was assessed using the Mental Health Continuum-Short Form (MHC-SF) [41, 42], Spanish version [43]. This instrument consists of 14 items designed to assess HWB, PWB, and SoWB. Items correspond to each one of the theory guided dimensions. For example, the items “In the past month, how often did you feel that you belonged to a community (like a social group, your neighborhood, your city)?” and “In the past month, how often did you feel that you had something important to contribute to society?” evaluate respectively social integration and social contribution of social well-being [18]. This period of one month is included between the beginning of the first wave in Spain (March 14th, 2020: national state of emergency and full confinement in Spain) and first wave data collection, and between the beginning of the second wave in Spain (October 25th, 2020: second national state of emergency) and second wave data collection. In previous research, the instrument demonstrated excellent internal consistency and factorial validity [41, 43]. Participants answered items using a 6-point Likert scale ranging from 1 (never) to 6 (every day). Consequently, total scores on the MHC-SF range from 14 to 84, with higher scores indicating higher levels of well-being. Moreover, we calculated the scores of the three sub-scales: HWB, PWB and SoWB. According to previous research [26], to obtain a categorical measure of the presence (vs. absence) of positive mental health, professionals should experience at least one of the three symptoms of HWB and at least six of the eleven symptoms of PWB and SoWB “every day” or “almost every day” in the past month. In the present study, Cronbach’s α for the MHC-SF was .90 (first wave Cronbach’s α was .86; second wave Cronbach’s α was .94), for the HWB was .85 (first wave Cronbach’s α was .81; second wave Cronbach’s α was .87), for the PWB was .85 (first wave Cronbach’s α was .82; second wave Cronbach’s α was .88), and for the SoWB was .85 (first wave Cronbach’s α was.76; second wave Cronbach’s α was .89).
Social Recognition
To measure macrosocial aspects of Social Recognition (SR), instead of individual reactions in one’s close or wider social environment, we used two items based on the Social Recognition Sub-scale of the Social Acknowledgement Questionnaire (SAQ) [27]. Specifically, participants answered to the following items: "to what extent have you felt positively appreciated and supported by society/community in the last month?" and “to what extent did you feel positively appreciated and supported by governments in the last month?” on a 4-point Likert scale (0 = not at all, 3 = totally). These two items were highly correlated (r = .45, p = .001), showing an adequate reliability according to Clark and Watson criterium (inter-item correlation within the range of .15 to .20 for scales that measure broad characteristics and between .40 to .50 for those tapping narrower ones) [44], therefore were averaged to make an overall index of perceived social recognition. Cronbach’s α for the composed two-item social recognition measure was acceptable (Cronbach’s α = .61; first wave Cronbach’s α = .59; second wave Cronbach’s α = .60) considering that α-coefficient is affected by the length of the scale and consequently underestimates true reliability in two-item scales [45].
Data Analysis
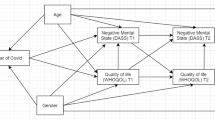
To analyze anxiety, traumatic intensity, well-being, and social recognition differences between the two COVID-19 waves we conducted several ANCOVAS with age, sex and profession as covariates. To examine the relationships between all scales in both waves we used Pearson Correlations. Specifically, to test our hypothesis regarding the moderating role of Covid-19 wave on the relationship between pathology symptoms and SoWB we subjected this last variable to a multiple regression analysis using the PROCESS add-on for SPSS (model 1) [46], and introduced Anxiety, Covid Wave (dichotomous variable: -1 = 1st wave; 1 = 2nd wave) and the interaction term as predictors. PROCESS is a computational procedure for SPSS and SAS that implements moderation or mediation analysis as well as their combination in an integrated conditional process model [46, 47]. Finally, to test our hypothesis regarding the mediating role of social recognition in the effect of COVID-19 waves on SoWB, we conducted a biased corrected bootstrapping procedure with 10,000 bootstrap re-samples using Hayes PROCESS macro (model 4; see Fig. 1). This approach includes procedures that compute a 95% confidence interval (CI) around the indirect effect and mediation is supported if CI does not include zero. COVID-19 Wave was the independent variable, SoWB was the dependent variable, and Social Recognition was the mediating variable. Some factors can produce spurious associations, particularly in studies such as the present one. Therefore, again age, sex and profession were introduced as covariates in mediation analysis. Also, a classical approach of mediation was used, and a Sobel Test was developed.
Results
Means and Standard Deviations of STAI-S, DTS, MHC-SF and SR are presented in Table 1. According to our hypothesis, in the first (vs. the second) wave the health professionals showed greater anxiety and greater traumatic intensity, although levels of anxiety and traumatic intensity were relatively high in both waves. In the first wave, 64 health professionals presented a STAI-S score greater than 40, indicating the possible presence of anxiety disorders. In the second wave, 40 health professionals reported a score greater than 40. In relation to trauma intensity levels, in the first wave, 48 health professionals reported a DTS score greater than 35, an indicator of the possible presence of PTSD. In the second wave, 44 health professionals reported a DTS score greater than 35.
Regarding the differences in health professionals’ global well-being (positive health) in both waves, the results were apparently surprising, since there were no differences in the total scores of the MHC-SF between the first and the second wave. However, when we examine the MHC-SF score for each one of the three subscales, we obtain the expected results. That is, health professionals showed lower HWB and PWB in the first wave compared to the second wave. However, and in accordance with our hypothesis, they showed greater SoWB in the first wave compared to the second one, an apparently counterintuitive result. In relation to the categorical diagnosis of the presence (vs. absence) of positive mental health, in the first wave 20 healthcare professionals showed a flourishing mental health diagnosis based on the criteria proposed by the CSMH. In the second wave, 40 professionals had a flourishing mental health diagnosis. Finally, as expected, health professionals perceived greater social recognition in the first wave of COVID-19 compared to the second one.
Regarding our second objective, Pearson correlation coefficients among STAI-S, DTS and MHC-SF, in the first wave, second wave and aggregated scores, are presented in Table 2. Concerning total scores, correlations between measures of pathology (i.e., STAI-S and DTS) and well-being (MHC-SF) were significant, although the amount of the correlation (all <|.55|) did not indicate overlap. In this sense, as suggested by the CSMH, this result seems to imply that mental illness and positive mental health reflect two distinct but interrelated domains, rather than the extreme ends of a single spectrum. Although correlations between pathology indicators (i.e., STAI-S and DTS) and well-being subscales were significant, the correlations of SoWB with anxiety and SoWB with traumatic intensity were weak. Precisely, in the first wave, correlations between psychopathology indicators and SoWB were not significant. However, in the second wave, both anxiety and traumatic intensity correlated significantly with SoWB. Subjecting SoWB to a multiple regression analysis introducing Anxiety, Covid Wave and the interaction term as predictor variables, we observed that the interaction between Anxiety and Covid Wave was significant, B = -.16, t(233) = -2.60, p = .01, 95% CI: -.29, -.04. As mentioned above, the results for Traumatic Intensity were similar in tendency, although the interaction between Traumatic Intensity and Covid Wave was not significant, B = -.08, t(236) = -1.19, p = .23, 95% CI: -.20, .05. This moderating effect of the COVID-19 wave did not occur for HWB, nor for PWB (all p > .32).
Finally, to examine the hypothesized mediating role of social recognition, we conducted a biased corrected bootstrapping procedure introducing COVID-19 Wave as the independent variable, SoWB as the dependent variable, and Social Recognition as the mediating variable. Age, sex, and profession were introduced as covariates in mediation analysis. According to our hypothesis, the data revealed that the 95% confidence interval of the indirect effect (i.e., the path through the mediator) did not include zero (Indirect Effect a x b = -.08, 95% CI [-14, -.03]). Also, Sobel Test was significant, Z = -2,83, p < .01, thus mediation by social recognition was supported (see Fig. 1). Although the two items of the Social Recognition measure were highly correlated, we also computed the mediating analyses for both items separately. The decomposition of the mediator in being appreciated by society and being appreciated by governments items showed similar results. For the first item the data revealed that the 95% confidence interval of the indirect effect did not include zero (Indirect Effect a x b = -.05, 95% CI [-11, -.02]) and Sobel Test was significant, Z = -2,17, p < .05. The same pattern emerged for being appreciated by governments (Indirect Effect a x b = -.07, 95% CI [-13, -.03]; Sobel Test, Z = -2,56, p = .01).
Discussion
Our study confirmed previous research about healthcare workers’ mental health in the COVID-19 first wave [47, 48], showing that professionals in the frontline care of Covid-19 patients informed high levels of anxiety and trauma intensity. Importantly, we extended these results to COVID-19 s wave. Nevertheless, in the second wave healthcare workers reported lower levels of anxiety and traumatic intensity (H1.1). As previously mentioned, there are various factors that could explain these results. First, although frontline professionals continued to be directly exposed to the virus, the availability of PPE in Spain was practically complete. Second, healthcare professionals received specific training for PPE correct use [49]. Third, in the beginning of the second wave in Spain, according to the Ministry of Health of Spain [50], practically all Spanish healthcare professionals were vaccinated with the complete dose. Fourth, although during the second wave there were also specific moments of healthcare overload, the Spanish strategic planning of human resources made it possible to increase the number of health workers to face the COVID-19 epidemic [51]. Finally, before the beginning of the second wave, notable advances in scientific knowledge about the disease were made and clinical protocols were established [52, 53]. All these aspects could lead to reduced fear of direct exposure, increased sense of control and partially reduced work overload, which in turn may decrease anxiety, trauma, and stress disorders symptoms [54]. Although health professionals recruited during the second wave showed lower levels of anxiety and trauma intensity than those in the first wave, as previously mentioned, the informed values were maintained high. In fact, in the second wave, approximately one out of three participants reported values that may indicate the presence of anxiety disorders and of PTSD. These results suggest that health authorities must continue to pay attention to healthcare professionals’ mental health. In this sense, protecting healthcare professionals’ mental health in the short, medium, and long term must be a central objective of governments of different countries [55].
Concerning front-line professionals’ positive health, their well-being was strongly affected by the COVID-19 pandemic in both waves. In the first wave, only one out of five health workers showed adequate positive mental health according to the criteria of the Complete State Model of Health. Regarding health workers’ well-being in the second wave, only two out of five showed positive mental health. According to out hypothesis (H1.2), health workers’ levels of HWB and PWB were greater during the second wave compared to the first one. Again, some of the factors previously mentioned could explain these results. For example, the reduction of work overload, better strategic planning of human resources, or lower mortality rates in the second wave (vs. the first wave), should act as protective factors of HWB and PWB levels. Specifically, HWB increase could be due to the decrease in negative emotionality produced by the reduction in communicating bad news to relatives, less patient suffering, fewer severe cases, and less mortality. Regarding PWB increment, in the second wave health professionals’ sense of subjective control probably increased, due to better knowledge of the disease and the availability of standardized clinical protocols, which could lead to greater Environmental Mastery (a core dimension of PWB). Although higher levels of all well-being indicators could be expected in the second wave (vs. the first wave), according to our hypothesis (H1.3), SoWB was lower in the second wave compared to the first one, an apparently paradoxical result. To better understand this paradox, we should consider that SoWB indicators are closely related to social integration, social recognition, and the sense of social contribution [18]. As already mentioned, in Spain during the first wave, there was a unanimous social recognition of health professionals, by society, governments and institutions. Also, the decisively contributions of health-care workers were made salient. Although fear of contagion was present among the population, there were practically no stigmatizing behaviors (e.g., people increasing physical distance with health professionals), and the few that did occur were rejected or condemned by both the population and governmental institutions. These aspects probably acted as protective factors for SoWB during the first wave. In fact, and according to our hypothesis, except for SoWB in the first wave, correlations between pathology and positive mental health indicators in both waves were negative and significant (H2.1), as predicted by the CSMH. However, as expected, in the first wave more pathology did not imply less SoWB (H2.2).
During the second wave in Spain, various of these elements changed. In this sense, and despite the increase in human resources, medical care services collapsed during the second wave. People experienced great difficulty in accessing medical care, both in primary care and hospitals. Medical appointment delays were in some cases very long, while people tended to attribute these delays to health professionals. Even governments, to avoid responsibility, blamed professionals for not further increase the length of their working hours. Also, stigmatizing behaviors began to increase in population. This lack of social support may have put health professionals’ social well-being at risk [56, 57]. In fact, as previously mentioned, health professionals reported less social recognition in the second (vs. the first) wave. How people are treated by their social environment, especially when facing traumatic events, such as working in front-line during the COVID-19 pandemic, may affect SoWB indicators [19, 40]. In this sense, we expected and found that social recognition mediated the effect of the COVID-19 wave on SoWB (H.3.1). In fact, this is not a novel idea; Durkheim already argued that when social structures are not able to integrate some individuals, by recognizing their work and effort, their social functioning is intensely affected [58]. These results have significant implications since they highlight the need to develop public policies designed to promote health professionals’ work recognition, with the aim of improving their positive mental health. We must not forget that “caring for those who care” must be an essential task of governments [59]. In this sense, interventions in the workplace to promote health workers’ mental health should be developed at primary, secondary, and tertiary levels. Positive mental health needs to become an inherent part of the organization, and mental health plans for health professionals should be developed in hospitals and healthcare centers. Also, creating protocols to identify workplace hazards to positive mental health could be useful. To facilitate early detection and early treatment of pathological mental health symptoms, rapid access of professionals to healthcare resources should be provided. A final objective is promoting reintegration in the workforce. At a legislative level, it is necessary to protect positive mental health in labor market legislation by including well-being and mental health protection as part of changes addressing employment conditions [60]. At a final comment, although working at an individual level is a tendency in positive psychology [61], the development of positive institutions is a challenge that needs to be addressed.
Despite the importance of the results, the present research has some limitations. The most important one has to do with the design of the study. As already mentioned, healthcare professionals were instructed by authorities to avoid negative comments about the pandemic management, so guarantee the anonymity perception was essential to avoid correction bias in responses. For this reason, due to the existing social climate, we decided to avoid traceability (not even for the researchers) between questionnaires and participants, and consequently participants were not assigned with identification numbers. Therefore, we could not employ a longitudinal study and we recruited two different samples of participants, one for each wave. The second limitation derives from the first one. Participants’ answers in the second wave could be affected by possible accumulation effects of both the first and the second wave. A longitudinal design would have helped to avoid this limitation. To minimize this possible accumulation effect, we selected instruments specifically designed to evaluate the effects produced by the COVID-19 during the last month. Importantly, the results of our study cannot be explained by this accumulation effect, because Covid-19 wave affected differently SoWB, HWB and PWB. That is, HWB and PWB improved in the second wave compared to the first one, while SoWB worsened. Moreover, psychopathological symptoms were greater in the first than in the second wave. As a final limitation, although we employed a simple random sampling method to select the participants in both waves, we selected them from an initial convenience pool. Therefore, we cannot guarantee that all variables of individual differences (e.g., professional experience or individual coping strategies to stressful events) were controlled. However, in the measured variables (i.e., age, gender, and profession) the first and second COVID-19 wave samples were equivalent.
Conclusions
Following the WHO recommendations, in the present study we evaluated healthcare professionals’ mental health during first and second COVID-19 waves using measures designed not only to evaluate psychopathology (i.e., state anxiety and post-traumatic stress) but also the presence of positive health.
In the second wave (vs. the first wave) our study detected some improvement in professionals’ mental health, specifically less psychopathological symptoms (although informed anxiety and traumatic intensity maintained high) and more HWB and PWB. However, not all changes were positive. Through COVID-19 pandemic, social recognition decreased. As a consequence, health professionals reported less SoWB in the second (vs. the first) wave. In this sense, due to the mediating role of social recognition, it is especially relevant that public institutions, governments, and society in general, should continue to recognize health professionals’ work, given that it is a fundamental protection factor for SoWB.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence Interval
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- DTS:
-
Davidson Trauma Scale
- HWB:
-
Hedonic Well-being
- MHC-SF:
-
Mental Health Continuum-Short Form
- PWB:
-
Psychological Well-being
- WHO:
-
World Health Organization
- SoWB:
-
Social Well-Being
- SR:
-
Social Recognition
- STAI:
-
State Trait Anxiety Inventory
References
Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Eng J Med. 2020;383(6):510–512. https://doi.org/10.1056/NEJMp2008017.
Hubbard G, den Daas C, Johnston M, Dixon D. Sociodemographic and psychological risk factors for anxiety and depression: Findings from the Covid-19 Health and Adherence Research in Scotland on Mental Health (CHARIS-MH) Cross-sectional survey. Int J Behav Med. 2021;28(6):788–800. https://doi.org/10.1007/s12529-021-09967-z.
Wang Y, Shi L, Que J, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. 2021;26(9):4813–22. https://doi.org/10.1038/s41380-021-01019-y.
Ye B, Wu D, Wang P, et al. COVID-19 stressors and poor sleep quality: The mediating role of rumination and the moderating role of emotion regulation strategies. Int J Behav Med. 2022;29(4):416–25. https://doi.org/10.1007/s12529-021-10026-w.
Heers M, Lipps O. Overwhelmed by learning in lockdown: Effects of Covid-19-enforced homeschooling on parents’ wellbeing. Soc Indic Res. 2022;164(1):323–43. https://doi.org/10.1007/s11205-022-02936-3.
Lewin AC, Shamai M, Novikov S. Surviving in Crisis Mode: The effect of material hardship and social support on emotional wellbeing among people in poverty during COVID-19. Soc Indic Res. 2023;165(1):245–65. https://doi.org/10.1007/s11205-022-03011-7.
van Zyl LE. Social study resources and social wellbeing before and during the intelligent COVID-19 lockdown in The Netherlands. Soc Indic Res. 2021;157(1):393–415. https://doi.org/10.1007/s11205-021-02654-2.
Zacher H, Rudolph CW. Individual differences and changes in subjective wellbeing during the early stages of the COVID-19 pandemic. Am Psychol. 2021;76(1):50–62. https://doi.org/10.1037/amp0000702.
Smith L, Jacob L, Yakkundi A, et al. Correlates of symptoms of anxiety and depression and mental wellbeing associated with COVID-19: A cross-sectional study of UK-based respondents. Psychiatry Res. 2020;291:113138. https://doi.org/10.1016/j.psychres.2020.113138
Bajo M, Gallego P, Stavraki M, Lamprinakos G, Luna P, Díaz D. Anxiety, trauma and well-being in health-care professionals during COVID-19 first wave in Spain: the moderating role of personal protection equipment availability. Health Qual Life Outcomes. 2021;19(1):207. https://doi.org/10.1186/s12955-021-01845-2.
Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976
Lu W, Wang H, Lin Y, Li L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:112936. https://doi.org/10.1016/j.psychres.2020.112936
Siddiqui I, Aurelio M, Gupta A, Blythe J, Khanji MY. COVID-19: Causes of anxiety and wellbeing support needs of healthcare professionals in the UK: A cross-sectional survey. Clin Med. 2021;21(1):66–72. https://doi.org/10.7861/clinmed.2020-0502.
Sobregrau-Sangrà P, Aguiló-Mir S, Castro-Ribeiro T, et al. Mental health assessment of Spanish healthcare workers during the SARS-CoV-2 pandemic. A cross-sectional study. Compr Psychiatry. 2022;112:152278. https://doi.org/10.1016/j.comppsych.2021.152278
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–7. https://doi.org/10.1016/j.bbi.2020.05.026.
Santabárbara J, Bueno-Notivol J, Lipnicki DM, et al. Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Prog Neuro Psychopharmacol Biol Psychiatry. 2021;107:110244. https://doi.org/10.1016/j.pnpbp.2021.110244
Bassi M, Negri L, Delle Fave A, Accardi R. The relationship between post-traumatic stress and positive mental health symptoms among health workers during COVID-19 pandemic in Lombardy. Italy J Affect Disord. 2021;280:1–6. https://doi.org/10.1016/j.jad.2020.11.065.
Keyes C. Social well-being Soc Psychol Q. 1998;61:121–40. https://doi.org/10.2307/2787065.
Blanco A, Blanco R, Díaz D. Social (dis)order and psychosocial trauma: Look earlier, look outside, and look beyond the persons. Am Psychol. 2016;71(3):187–98. https://doi.org/10.1037/a0040100.
Seeman M. Alienation motifs in contemporary theorizing: The hidden continuity of the classic themes. Soc Psychol Q. 1983;46(3):171–84. https://doi.org/10.2307/3033789.
Gecas V. The social psychology of self-efficacy. Annu Rev Sociol. 1989;15:291–316. https://doi.org/10.1146/annurev.so.15.080189.001451.
König J, Chung S, Ertl V, et al. The German translation of the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) scale: Results from healthcare workers during the second wave of COVID-19. Int J Environ Res Public Health. 2021;18(17):9377. https://doi.org/10.3390/ijerph18179377.
Roberts NJ, McAloney-Kocaman K, Lippiett K, Ray E, Welch L, Kelly CA. Factors influencing fatigue in UK nurses working in respiratory clinical areas during the second wave of the Covid-19 pandemic: An online survey. J Clin Nurs. 2022. https://doi.org/10.1111/jocn.16375.10.1111/jocn.16375.
World Health Organization. Official records of the world health organization, vol. 2. Geneva: World Health Organization. 1946.
Shek DTL. COVID-19 and quality of life: Twelve reflections. Appl Res Qual Life. 2021;16(1):1–11. https://doi.org/10.1007/s11482-020-09898-z.
Keyes CL. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol. 2005;73(3):539–48. https://doi.org/10.1037/0022-006X.73.3.539.
Maercker A, Müller J. Social acknowledgment as a victim or survivor: a scale to measure a recovery factor of PTSD. J Trauma Stress. 2004;17(4):345–51. https://doi.org/10.1023/B:JOTS.0000038484.15488.3d.
Cohen J. Statistical power analysis for the behavioural sciences. San Diego: Academic Press; 1969.
CNE ISCIII Red Nacional de Vigilancia Epidemiológica. Informe nº 20. Situación de COVID-19 en España a 3 de abril de 2020. Madrid: Instituto de Salud Carlos III. 2020.
CNE ISCIII Red Nacional de Vigilancia Epidemiológica. Informe nº 63. Situación de COVID-19 en España a 27 de enero de 2021. Madrid: Instituto de Salud Carlos III. 2021.
Spielberger CD, Gorsuch RL, Lushene RE. The state-trait anxiety inventory (test manual). Palo Alto: Consulting Psychologists Press. 1970.
Spielberger CD, Gonzalez-Reigosa F, Martinez-Urrutia A, Natalicio LF, Natalicio DS. Development of the Spanish edition of the State-Trait Anxiety Inventory. Interam J Psychol. 1971:5(3–4):145–158.
Spielberger CD. State-Trait Anxiety Inventory: Bibliography. 2nd ed. Palo Alto: Consulting Psychologists Press; 1989.
Guillén-Riquelme A, Buela-Casal G. Actualización psicométrica y funcionamiento diferencial de los ítems en el State Trait Anxiety Inventory (STAI). Psicothema. 2011:23(3), 510–515.
Davidson JR, Book SW, Colket JT, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27(1):153–60. https://doi.org/10.1017/s0033291796004229.
Bobes J, Calcedo-Barba A, García M, et al. Evaluation of the psychometric properties of the Spanish version of 5 questionnaires for the evaluation of post-traumatic stress syndrome. Actas Esp Psiquiatr. 2000:28(4), 207–218.
McDonald SD, Beckham JC, Morey RA, Calhoun PS. The validity and diagnostic efficiency of the Davidson Trauma Scale in military veterans who have served since September 11th, 2001. J Anxiety Disord. 2009;23(2):247–55. https://doi.org/10.1016/j.janxdis.2008.07.007.
Elhai JD, Lindsay BM, Gray MJ, Grubaugh AL, North TC, Frueh BC. Examining the uniqueness of frequency and intensity symptom ratings in posttraumatic stress disorder assessment. J Nerv Ment Dis. 2006;194(12):940–4. https://doi.org/10.1097/01.nmd.0000243011.76105.4b.
McDonald SD, Beckham JC, Morey R, Marx C, Tupler LA, Calhoun PS. Factorial invariance of posttraumatic stress disorder symptoms across three veteran samples. J Trauma Stress. 2008;21(3):309–17. https://doi.org/10.1002/jts.20344.
Díaz D, Stavraki M, Blanco A, Bajo M. 11-M victims 3 years after Madrid terrorist attacks: looking for health beyond trauma. J Happiness Stud. 2018;19:663–75. https://doi.org/10.1007/s10902-016-9842-x.
Lamers SM, Westerhof GJ, Bohlmeijer ET, ten Klooster PM, Keyes CL. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J Clin Psychol. 2011;67(1):99–110. https://doi.org/10.1002/jclp.20741.
Luijten CC, Kuppens S, van de Bongardt D, Nieboer AP. Evaluating the psychometric properties of the mental health continuum-short form (MHC-SF) in Dutch adolescents. Health Qual Life Outcomes. 2019;17(1):157. https://doi.org/10.1186/s12955-019-1221-y.
Echeverría G, Torres M, Pedrals N, Padilla O, Rigotti A, Bitran M. Validation of a spanish version of the Mental Health Continuum-Short Form Questionnaire. Psicothema. 2017;29(1):96–102.
Clark LA, Watson D. Constructing validity: Basic issues in objective scale development. Psychol Assess. 1995;7:309–19. https://doi.org/10.1037/1040-3590.7.3.309.
Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80(1):99–103. https://doi.org/10.1207/S15327752JPA8001_18.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York: Guilford Press; 2013.
Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3):e0246454. https://doi.org/10.1371/journal.pone.0246454.
Moitra M, Rahman M, Collins PY, et al. Mental health consequences for healthcare workers during the covid-19 pandemic: a scoping review to draw lessons for LMICs. Front Psychiatry. 2021;12:602614. https://doi.org/10.3389/fpsyt.2021.602614.
Romero CS, Delgado C, Catalá J, et al. COVID-19 psychological impact in 3109 healthcare workers in Spain: The PSIMCOV group. Psychol Med. 2022;52(1):188–94. https://doi.org/10.1017/S0033291720001671.
Ministry of Health of Spain. Covid-19 vaccination strategy in Spain. Ministry of Health of Spain. 2021. Accessed April 16, 2023. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/vacunaCovid19.htm.
Ministry of Health of Spain. Informe Anual del Sistema Nacional de Salud 2020–2021. Ministry of Health of Spain. Madrid: Centro de Publicaciones del Ministerio de Sanidad. 2022.
Del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA. 2020;324(17):1723–4. https://doi.org/10.1001/jama.2020.19719.
Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S. Neuropathogenesis and neurologic manifestations of the coronaviruses in the age of coronavirus disease 2019: A review. JAMA Neurol. 2020;77(8):1018–27. https://doi.org/10.1001/jamaneurol.2020.2065.
Tyra AT, Ginty AT, John-Henderson NA. Emotion Regulation Strategies Predict PTSS During the COVID-19 Pandemic in an American Indian Population. Int J Behav Med. 2021;28(6):808–12. https://doi.org/10.1007/s12529-021-09964-2.
Muller AE, Hafstad EV, Himmels JPW, et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020;293:113441. https://doi.org/10.1016/j.psychres.2020.113441.
van der Velden PG, Oudejans M, Das M, Bosmans MWG, Maercker A. The longitudinal effect of social recognition on PTSD symptomatology and vice versa: Evidence from a population-based study. Psychiatry Res. 2019;279:287–94. https://doi.org/10.1016/j.psychres.2019.05.044.
Holt-Lunstad J. Why social relationships are important for physical health: A systems spproach to understanding and modifying risk and protection. Annu Rev Psychol. 2018;69:437–58. https://doi.org/10.1146/annurev-psych-122216-011902.
Durkheim E. Suicide, a study in sociology. London: Routledge; 1951.
World Health Organization. Caring for those who care: guide for the development and implementation of occupational health and safety programs for health workers. Geneva World Health Org. 2022.
Commission E. Directorate-General for Health and Food Safety. Supporting mental health of health workforce and other essential workers. Lux Publ Off Eur Union. 2021.
Gable SL, Haidt J. What (and why) is positive psychology? Rev Gen Psychol. 2005;9(2):103–110. https://doi.org/10.1037/1089-2680.9.2.103.
Funding
This research was supported by Ministry of Science and Innovation—Government of Spain (PID2020-116651 GB-C32).
Author information
Authors and Affiliations
Contributions
MB and DD conceived the study design. MB, MS and GMGJ collected the data and drafted the manuscript. DD, MB and GMGJ performed the data analysis. Critical revisions were contributed by DD. All authors discussed the results, implications, and literature, and approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Statement Regarding Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement Regarding Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest Declaration
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bajo, M., García-Jiménez, G.M., Stavraki, M. et al. Positive Mental Health of Frontline Healthcare Professionals during COVID-19 First Wave and Second Wave in Spain: The Protective Role of Social Recognition. Int.J. Behav. Med. 31, 527–537 (2024). https://doi.org/10.1007/s12529-023-10190-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-023-10190-1