Abstract
Although there is a growing body of evidence that health is the presence of well-being and not just the absence of a disease, research related to victims of terrorists attacks is mostly focused on the presence/absence of pathology (e.g. PTSD). The present study aims to apply the Complete State Model of Health to evaluate the mental health status of 69 direct victims of 11-M terrorist attack three years after the event. The results of Horn’s Parallel Analysis and CFA confirmed that the measures of positive mental health (well-being indicators) and illness (PTSD) loaded on separate but correlated factors. This is to say, the absence of PTSD in our sample was not equivalent to the presence of health. However, although positive health and illness indicators should be considered as two different factors, they were closely related. In fact, three well-being indicators were strongly associated with PTSD: positive affect, self-acceptance and positive relations. These findings suggest the need to work to ensure victims’ positive health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Almost seventy years ago, the World Health Organization (WHO 1946) defined health as a complete physical, mental, and social well-being, and not merely as the absence of disease. Despite the widely theoretical agreement with this approach, “the de facto conception of mental health is psychiatric: Individuals are either mentally ill or presumed mentally healthy” (Keyes 2005, p. 539). This is the base on which most psychiatrists and clinical psychologists develop their professional practice: the patient is mentally healthy when there is absence of pathology. Clinical care for victims of terrorist attacks is not an exception, even though only a low percentage of people exposed to terrorist attacks develop clinically significant disorders (e.g., Galea et al. 2003; Vázquez and Hervás 2010). Although consequences of trauma may include a wide range of psychopathology (e.g. Neria et al. 2008), post-traumatic stress disorder (PTSD) is the most common disorder caused by intentional violence (e.g. Neria et al. 2011). As a result of this theoretical approach, most studies on trauma caused by violence have focused on the presence/absence of PTSD (e.g. Galea et al. 2003) and have underestimated aspects, such as the after-effects on social and community relationships (e.g. Bracken et al. 1995; Luttrell et al. 2016; Martín-Baró 1998). Therefore, there is little research on the influence of trauma on victims’ well-being and quality of life, with an exception of studies on positive effects of traumas (e.g. posttraumatic growth; Helgeson et al. 2006).
Nowadays, there is the widely held belief that pathology is not the only after-effect of collective violence. Therefore, some authors consider health as a continuum, ranging from states of optimal well-being to complete disease (e.g., Antonovsky 1979). Consistent with this notion, Keyes (2005) developed the Complete State Model of Health (CSMH) which included social, interpersonal and intergroup relationships as a factor of health. According to this model, health is not a state characterized merely by the absence of disease, but also by the presence of a set of 13 indicators of hedonia (i.e. positive affect, avowed life satisfaction) and positive functioning (i.e. autonomy, self-acceptance, positive relations, control of the environment, purpose in life, personal growth, social integration, social acceptance, social contribution, social actualization and social coherence). To operationalize hedonia, the CSMH proposes to use the construct of Subjective Well-being and to employ Satisfaction With Life Scale (Diener et al. 1985) and Positive Affect Scale (Keyes et al. 2002) to measure it. To operationalize positive functioning, the CSMH proposes the constructs of Psychological Well-being and Social Well-being, and the use of Psychological Well-being Scales (Ryff 1989) and Social Well-being Scales (Keyes 1998). In this sense, the CSMH allows a continuous assessment and a categorical diagnosis of the presence and absence of mental health. The categorical diagnosis requires meeting the criteria of hedonia (high level on positive affect or/and avowed life satisfaction) and positive function (high level on six or more of the other well-being indicators).
Although the CSMH can be applied to most common mental disorders (Keyes 2005; e.g., major depression; Díaz et al. 2007), to the best of our knowledge up-to-date no study has applied this model to PTSD. However, there are several reasons why the CSMH should also apply to PTSD. First, PTSD severely compromises victims’ well-being (Nawijn et al. 2015). Second, anhedonia, referring to the inability to experience positive emotions and pleasure from normally pleasant stimuli and life events, and the existence of a persistent negative emotional state are two key features of PTSD (DSM-V D4-D7 criteria; American Psychiatric Association 2013), while hedonia is a main criterion of CSMH. Anhedonic symptoms, as inability to experience positive emotions, are present in about two-thirds of PTSD patients, independently of comorbid major depressive disorder (MDD) (Carmassi et al. 2014; for a review on the possible mechanisms underlying anhedonia in PTSD see Nawijn et al. 2015). Third, from a cognitive perspective, PTSD is often characterized by persistent negative beliefs and expectations about oneself, the others or the world (DSM-V D2 criterion; American Psychiatric Association 2013). These beliefs are closely related with some positive functioning indicators, particularly with self-acceptance and positive relations.
For these reasons, this study is aimed to apply the CSMH to a sample of direct victims of the terrorist attacks on March 11, 2004, in Madrid (Spain). These attacks were nearly simultaneous, coordinated bombings against the train system of Madrid and resulted in the deaths of 191 people and the injuries of more than 1800.
We believe that the application of the CSMH for the assessment of trauma caused by intentional violence can have interesting implications. First, according to the Psychosocial Trauma Model (Blanco et al. 2016), it is necessary to measure the after-effects of trauma not only in terms of absence/presence of psychopathology but also in terms of social injury (e.g., group polarization, isolation from social life, lack of confidence in social relationships, loss of social capital, etc.). The CSMH allows us to accurately assess these effects. Second, the CSMH argues that rather than forming a single bipolar dimension, health and illness are correlated unipolar dimensions. Therefore, the absence of PTSD does not guarantee the presence of health. This is especially important given that social support and protection programs for terrorist victims in many countries, like Spain, require the diagnosis of a mental disorder. When the diagnostic criteria are no longer fulfilled, victims stop receiving public aid from the government.
As we intend to analyze the medium/long-term effects of trauma and resilience of victims beyond PTSD, the research was conducted three years after the attacks. This time period was chosen for being the most common in previous studies on the effects of the terrorist attacks in the medium/long-term (e.g., 2–3 years after 11-S: DiGrande et al. 2011; 2–3 years after 1995–1996 bombings in France: Verger et al. 2004). Moreover, we have chosen victims with a high-intensity direct exposure to trauma, because most existing studies on the effects of the terrorist attacks have focused on victims of indirect exposure or on the general population (e.g., Rimé et al. 2009; Silver et al. 2002; Vázquez et al. 2008). In fact, to the best of our knowledge, this is the first research with 11-M victims in which all participants were traveling in one of the four trains where bombs were placed. Following the CSMH, our main hypothesis (1) is that two different unipolar dimensions will emerge from the measures used to assess positive health (i.e. well-being indicators) and illness (i.e. PTSD). In addition, our second hypothesis (2) is that positive health and illness will be correlated. Therefore, our last goal will be the study of the relationship between PTSD and well-being indicators as different but related constructs.
2 Method
2.1 Participants
Sixty-nine direct victims of 11-M terrorist attacks voluntarily participated without compensation. All participants were traveling in one of the four trains where bombs were placed on the morning of 11 March 2004. Participants were recruited via letter of invitation explaining the project and the voluntary nature of participation. Ninety-eight applications to participate were received. Participants were selected to meet the study criteria of (1) an initial PTSD diagnosis; (2) no diagnosis of other mental disorder or another medical condition (except minor injuries that did not require hospitalization); (3) no diagnosis of other mental disorders or general medical condition (except PTSD) at the time the study was conducted (three years after the attack). Participants who fulfilled the criteria were 30 men (43.5%) and 39 women (56.5%) between 20 and 68 years old. The mean age was 42.27 years (SD = 11.98).
2.2 Procedure
Participants completed the study within the psychological care protocol of 11-M Association of Victims, three years after the attacks. This study was part of a research project funded by the Spanish Ministry of Education and Science and was approved by the ethics committee of the coordinating university (SEJ2006-14894; Universidad Autónoma de Madrid). First, participants were placed in individual lab cubicles. Then, after being told that all collected information was confidential and anonymous, all participants signed an informed consent. To avoid possible order effects of the two sets of scales, half of the participants completed the Davidson Trauma Scale first followed by (in order of appearance) the Social Well-being Scales, the Psychological Well-being Scales, the Satisfaction with Life Scale and the Positive Affect Scale. By contrast, the other half first completed the Social Well-being Scales, the Psychological Well-being Scales, the Satisfaction with Life Scale and the Positive Affect Scale and, then, proceeded to complete the Davidson Trauma Scale.
2.3 Measures
2.3.1 Post-Traumatic Stress Disorder
Dimensional Measure The Davidson Trauma Scale (DTS; Davidson et al. 1997; validated in Spanish by Bobes et al. 2000) is a 17-item self-report questionnaire of posttraumatic stress symptoms, developed for use with trauma survivors. Each of the 17 items correspond to the 17 DSM-IV symptoms of PTSD and can be categorized as follows: items 1–4 and 17 (criteria B, intrusive re-experiencing); items 5–11 (criteria C, avoidance and numbness); and items 12–16 (criteria D, hyperarousal). For each item, the victims rate both frequency and severity using 5-point (0–4), Likert-type scales. The DTS total score and the three DTS subscales (re-experiencing, avoidance and numbness, and hyperarousal) were calculated.
Categorical Measure In order to obtain a categorical measure of the presence/absence of PTSD we employed as a threshold score a punctuation of 40 (the highest efficiency −.83—according to Davidson et al. 1997). Additionally, clinical diagnoses made by professionals who treated the victims during the study were used. These diagnoses were made using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I) (First et al. 2002). Both criteria (DTS threshold score and Clinical Diagnosis) converged for 68 victims (98.6%). In the only divergence found, we used the criterion based on the application of SCID-I.
2.3.2 Positive Health
Dimensional Measures Following CSMH, we measured hedonia (positive affect and avowed life satisfaction indicators) by having participants complete the Satisfaction With Life Scale (Diener et al. 1985) and Positive Affect Scale (Keyes et al. 2002). The Satisfaction With Life Scale (validated in Spanish by Cabañero et al. 2004) consists of five items that have shown good psychometric properties in different studies (e.g., Rodríguez-Carvajal et al. 2010 Participants responded to each item on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Participants also completed Positive Affect Scale (Keyes et al. 2002; Spanish version: Díaz et al. 2007) indicating how long, for the past 30 days, they have been experiencing the following six indicators of positive affect: cheerful, in good spirits, extremely happy, calm and peaceful, satisfied, and full of life. Participants responded using a response format with scores ranging from 1 (never) to 5 (all the time). Due to the strong correlation between the indicators (r = .76), and previous research indicating the existence of a higher order factor (e.g., Diener et al. 1999), a global subjective well-being score was also calculated. To measure positive function participants responded to Psychological Well-being Scales (Ryff 1989) and Social Well-being Scales (Keyes 1998). Participants filled the version of Psychological Well-being Scales validated into Spanish by Díaz et al. (2006). This instrument consists of six scales that measure six indicators of positive functioning (autonomy, self-acceptance, positive relations, control of the environment, purpose in life and personal growth). This measure has 33 total items (4–6 items per scale) to which participants responded using a response format with scores ranging from 1 (strongly disagree) to 6 (strongly agree). The proposed six-dimensional structure with second order general factor has been tested using confirmatory factor analysis including Spanish samples (Díaz et al. 2006; Van Dierendonck et al. 2008). Also, participants completed Keyes’ Social Well-being Scales (Keyes 1998) validated and translated to Spanish (Blanco and Díaz 2005). This instrument consists of five scales that measure five indicators of positive functioning (social integration, social acceptance, social contribution, social actualization and social coherence), which has shown good internal consistency in previous studies, with Cronbach’s α values ranging between .69 and .83. (e.g., Keyes 1998). The proposed five-dimensional structure with second order general factor has been tested using confirmatory factor analysis in Spanish samples (Keyes 1998; Blanco and Díaz 2005). Participants responded to items using a response format with response options ranging from 1 (strongly disagree) to 7 (strongly agree).
Categorical Measures Following Keyes (2005), in order to obtain a categorical measure of presence/absence of positive health, the presence of an indicator (flourishing) was taken into consideration when the subject’s score in the scale was equal to or greater than the mean of the general Spanish population according to the samples of Blanco and Díaz (2005), and Díaz et al. (2006, 2007). Using the categorical diagnosis of mental health provided by the CSMH, the presence of health required both criteria of hedonia (high level on at least one indicator scale—indicators 1 or 2) and positive functioning (high level on six or more indicator scales—indicators 3–13). Additionally, each subject participated in a semi-structured interview based on the descriptions of indicators proposed by Keyes (2005) where the professionals who treated the victims during the study codified the presence or absence of each of the criteria. Subsequently, the presence/absence of health was examined using the same criteria (CSMH categorical diagnosis). Both evaluations (well-being scales and semi-structured interviews) were converging for the 68 victims (98.6%). In the only divergence found, the result of the semi-structured interview was chosen.
2.3.3 Data Analysis
In order to check whether two different dimensions emerge from the measures used to assess positive health (well-being indicators scales) and illness (PTSD; DTS) (hypothesis i), we conducted an exploratory factor analysis (EFA). According to our first hypothesis, one of the most critical methodological decisions regarding EFA is the number of factors to retain. Following various authors’ recommendations (e.g., Glorfeld 1995; Hayton et al. 2004), in order to estimate the number of factors to maintain we used parallel analysis (PA), which is one of the most accurate factor retention methods. To do so, we used SPSS syntax developed by O’Connor (2000) to calculate the mean and the 95th percentile for each of the eigenvalues of the 100 randomly generated data sets. The random data eigenvalues were compare to the real-data eigenvalues obtained from a Principal Component Analysis (PCA) in which the number of factors extracted equals the number of scales entered into the analysis. Following the criterion established by the PA of the number of factors to be extracted, an EFA was conducted. We employed principal axis as factor extraction method, as Fabrigar et al. (1999) suggest. Also, we used direct oblimin as rotation method because, according to our second hypothesis, the emerged dimensions were expected to be correlated. To study the relationship between PTSD and well-being indicators, we used a contingency table, a Fisher’s exact test, Pearson’s correlations and different ANCOVAS (introducing as covariates age, sex and the train in which the victims were traveling).
3 Results
Descriptive statistics (means and standard deviations) and Cronbach alpha coefficients (α) of DTS and well-being scales are displayed in Table 1. The results of PA are shown in Table 2. Only the first and second eigenvalues of the real dataset exceeded random values. Using this information, an EFA was conducted. To reduce the number of variables entered into the analysis, global scores of subjective well-being, psychological well-being and social well-being were computed. As a result, six variables were introduced. The N:p ratio was 11.5, higher than those generally recommended in the literature to yield factors’ good recovery (e.g., Gorsuch 1983). Most importantly, communalities were consistently high (all greater than .60 with the exception of SWB that was .50), indicating a good factor recovery (Hogarty et al. 2005; MacCallum et al. 1999). As shown in Table 3, all the sub-scales of DTS essentially loaded on the first factor, explaining 54% of variance. All well-being indicators loaded on the second factor, explaining 22% of the variance. These results support the existence of two different unipolar dimensions: Illness (PTSD; factor 1) and positive health (well-being; factor 2). Correlation between the two factors was −.48, which is a first indicator of the strong existing relationship between illness and positive health.
Having confirmed the existence of the two-dimensionality hypothesis, we expect some victims no longer presenting PTSD may not be assessed as healthy by not meeting the criteria for the presence of positive health (categorical diagnostic approach). The categorical diagnosis requires the criteria of hedonia (high level on positive affect or/and avowed life satisfaction) and positive function (high level on six or more of the other well-being indicators) to be met. To test this affirmation, we computed a contingency table of positive health (presence-absence) X PTSD (presence–absence) (Table 4). Notably, 46 victims (69.7%) had PTSD 3 years after the 11-M terrorist attacks. Of the remaining 23 victims who did not have PTSD (31.3%) only 3 (4%) had a categorical diagnosis of mental health. To test the relationship between positive health and PTSD, we computed a Fisher’s exact test because the expected values in two cells of the contingency table were below 5. According to the CSMH, the results indicated that positive health and PTSD were related (Fisher’s exact test, p = .03).
To explore in more detail this relationship, we calculated the Pearson’s correlations of well-being scales and DTS Total Score, DTS-B Score, DTS-C Score and DTS-D Score (Table 5). Global indicators of subjective well-being, psychological well-being and social well-being were all significantly correlated with DTS Total Score, DTS-B Score, DTS-C Score and DTS-D Score. Concretely, positive affect and self-acceptance scales showed stronger relation to DTS Total Score, DTS-B Score, DTS-C Score and DTS-D Score than the rest of the scales.
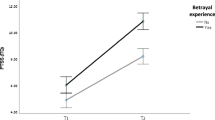
Finally, to analyze the differences between victims with and without PTSD (at the time the study was conducted, which was three years after the attack) in the well-being indicators scales we performed different ANCOVAS introducing as covariates age, sex and the train in which the victims were traveling. The results are shown in Table 6. None of the covariates were significant (p > .08). Concerning well-being global indicators, there were significant differences in subjective and psychological well-being, but not in social well-being. The most significant differences occurred in the indicators of life satisfaction, self-acceptance, positive relations with others, and positive affect. Delving into the relationship between PTSD and positive affect, victims who met the criteria of the presence of positive affect showed lower DTS Total Score (M = 31.42, SD = 16.34) than those who did not meet them (M = 55.42, SD = 18.91), F (1, 67) = 7.18, p = .03, η 2p = .07.
4 Discussion
The definition of health as the presence of well-being and not merely the absence of disease, has an important consensus in the scientific community, nevertheless its impact on clinical practice has been limited. Although there are different models and instruments to assess the “presence of well-being” (e.g., DSM-IV-TR Axis V GAF Scale), the CSMH is especially interesting because it proposes that rather than forming a single bipolar dimension, health and illness are correlated unipolar dimensions.
The main objective of the present research was to test whether this axiom of CSMH could be applied in the study of health of terrorist attacks’ victims. According to our hypothesis, the results of Horn’s PA and CFA confirmed that the measures of illness (PTSD) and mental health (well-being indicators) loaded on separate (hypothesis i) but correlated factors (hypothesis ii). This finding seems especially significant since it is in line with the argument that the absence of PTSD is not equivalent to the presence of health. In fact, of the 23 victims who did not have PTSD, only three had a diagnosis of presence of health. These results are relevant because in various countries, the maintenance of the main public economic aid and even free assistance (health care) to the victims of terrorist attacks depends on the presence of a mental disorder or another medical condition.
Therefore, it is important to continue working for victims’ positive health, even if they no longer meet diagnostic criteria for PTSD. Moreover, taking steps toward using this approach is important because, according to the psycho-social model of trauma (Blanco et al. 2016), the effects of terrorist attacks are long-lasting as well as severe. In fact, traumas caused by terrorist attacks tend to affect victims differently than traumas caused by natural disasters (Santiago et al. 2013). This happens because terrorist attacks have the intention to harm innocent people and spread terror among the civilian population (e.g., De la Corte et al. 2007). Also, terrorist attacks have emotional, social, and political consequences that accumulate and endure over time (Neria et al. 2011). For all these reasons, it is more difficult for victims to recover (Norris et al. 2002). In fact, in our sample, the majority of victims still had PTSD three years after the terrorist attacks of 11-M and only 3 victims (4%) had a categorical diagnosis of mental health, suggesting limited victim recovery.
Our results indicate that three well-being indicators appear to be strongly related to PTSD. The first is positive affect. In the analyses performed on continuous measures of PTSD and health, the positive affect scale had the strongest correlation with DTS Total Score. Furthermore, the victims who still had PTSD showed significantly lower levels of positive affect. These results converge with other studies that link trauma with difficulty in experiencing positive emotions (e.g., Rimé et al. 2009). In fact, anhedonia (i.e. inability to experience positive emotions) and persistent negative emotions are two main features of PTSD. For example, according to Carmassi et al. (2014), 53–61% of PTSD patients showed inability to experience positive emotions and 77–95% showed persistent negative emotional state. Also, in line with previous research, our results indicate that those who experienced positive emotions, faced trauma much better than the ones who didn’t (Fredrickson et al. 2003). That is, victims who met the criteria of the presence of positive affect showed lower scores on the DTS Total Score than those who did not meet them. Additionally, self-acceptance and positive relations were also strongly correlated to PTSD in our sample. Previous research suggests that trauma produces negative cognitions about the self and others (e.g., Blanco et al. 2010; Foa et al. 1999) and, in turn, that these negative cognitions subsequently increase PTSD in a vicious downward cycle (Shahar et al. 2013), diminishing well-being over time. Our results are consistent with this standpoint, since victims with PTSD showed significantly lower levels of self-acceptance and positive relations with others.
Apart from the findings described above, the present study has some limitations. The first is related to the sample size. This size was limited by the difficulty in accessing to direct victims of 11-M terrorist attacks. In addition, the strict criteria for participants’ inclusion and exclusion—although necessary to increase the validity of the results—also limited sample size. Although the sample size could affect the methodological analyses employed in this research, we can say that it has not significantly influenced the results. Concerning factor analyses, the N:p ratio is 11.5, which is higher than the ones generally recommended in the literature to yield good recovery of factors (e.g., Gorsuch 1983), and communalities are greater than .60 (with the exception of SWB .50). Both components are indicators of good factor recovery (Hogarty et al. 2005; MacCallum et al. 1999). Regarding the relationship between positive health and PTSD, and given the sample size, we computed a Fisher’s exact test because we expected low values in the cells of the contingency table. Concerning correlational analyses, we have included confidence intervals to assess the impact of sample size on results (Altman and Gardner 1988). Finally in all conducted ANCOVA there is an adequate N per group (>30). In regard to external validity, different studies have found similar results showing that two different but related factors emerge out of positive health measures (i.e. well-being) and pathology (e.g., Keyes 2005).
In closing, these findings suggest that assessments of health in terrorist attack victims must go beyond establishing the absence of disease (e.g., PTSD) to also establish the existence of high levels of physical, mental and social well-being. The implementation of the CSMH on the study of the health of victims has demonstrated that the symptoms of illness (PTSD) and health (well-being) compose two different but related factors. Based on these results, it is essential to work to ensure victims’ positive health by looking beyond the absence of disorders, directly at people’s well-being.
References
Altman, D. G., & Gardner, M. J. (1988). Statistics in Medicine: Calculating confidence intervals for regression and correlation. British Medical Journal, 296, 1238–1242.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Antonovsky, A. (1979). Health, stress and coping. San Francisco: Jossey-Bass.
Blanco, A., Blanco, R., & Díaz, D. (2016). Social (dis)order and psychosocial trauma: Look earlier, look outside, and look beyond the persons. American Psychologist, 71, 187–198.
Blanco, A., & Díaz, D. (2005). Social well-being: Theoretical structure and measurement. Psicothema, 17, 582–589.
Blanco, A., Díaz, D., Gaborit, M., & Amaris, M. C. (2010). World schema and self schema: The posttraumatic cognitions inventory (PTCI) in hispanic population. Revista Latinoamericana de Psicología, 42, 97–110.
Bobes, J., Calcedo-Barba, A., García, M., Francois, M., Rico-Villademoros, F., González, M., et al. (2000). Evaluación de las propiedades psicométricas de la versión española de cinco cuestionarios para la evaluación del trastorno de estrés postraumático. [Evaluation of the psychometric properties of the Spanish version of five questionnaires for the assessment of post-traumatic stress disorders]. Actas Españolas de Psiquiatría, 28, 207–218.
Bracken, P. J., Giller, J. E., & Summerfield, D. (1995). Psychological responses to war and atrocity: The limitations of current concepts. Social Science and Medicine, 40, 1073–1082.
Cabañero, M. J., Richart, M., Cabrero, J., Orts, M. I., Reig, A., & Tosal, B. (2004). Reliability and validity of the satisfaction with life scale of Diener in pregnant and puerperium women. Psicothema, 16, 448–455.
Carmassi, C., Akiskal, H. S., Bessonov, D., Massimetti, G., Calderani, E., Stratta, P., et al. (2014). Gender differences in DSM-5 versus DSM-IV-TR PTSD prevalence and criteria comparison among 512 survivors to the L’Aquila earthquake. Journal of Affective Disorders, 160, 55–61.
Davidson, J. R. T., Book, S. W., Colket, J. T., Tupler, L. A., Roth, S., David, D., et al. (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological Medicine, 27, 153–160.
De la Corte, L., Kruglanski, A., De Miguel, J. M., Sabucedo, J. M., & Díaz, D. (2007). Seven psychosocial principles for explaining terrorism. Psicothema, 19, 367–374.
Díaz, D., Blanco, A., Horcajo, J., & Valle, C. (2007). Depression and the complete state model of health. Psicothema, 19, 286–294.
Díaz, D., Rodríguez-Carvajal, R., Blanco, A., Moreno-Jiménez, B., Gallardo, I., Valle, C., et al. (2006). Spanish adaptation of the Psychological Well-Being Scales (PWBS). Psicothema, 18, 572–577.
Diener, E., Emmons, R., Larsen, R., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49, 71–75.
Diener, E., Suh, E., Lucas, R., & Smith, H. (1999). Subjective well-being: Three decades of progress. Psychological Bulletin, 125, 276–302.
DiGrande, L., Neria, Y., Brackbill, R. M., Pulliam, P., & Galea, S. (2011). Long-term posttraumatic stress symptoms among 3271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. American Journal of Epidemiology, 173, 271–281.
Fabrigar, L. R., Wegener, D. T., MacCallum, R. C., & Strahan, E. J. (1999). Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods, 3, 272–299.
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. W. (2002). Structured clinical interview for DSM-IV-TR Axis I Disorders (SCID-I). New York: Biometrics Research.
Foa, E. B., Dancu, C. V., Hembree, E. A., Jaycox, L. H., Meadows, E. A., & Street, G. P. (1999). A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology, 67, 194–200.
Fredrickson, B. L., Tugade, M. M., Waugh, C. E., & Larkin, G. (2003). What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology, 84, 365–376.
Galea, S., Vlahov, D., Resnick, H., Ahern, J., Susser, E., Gold, J., et al. (2003). Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. American Journal of Epidemiology, 158, 514–524.
Glorfeld, L. W. (1995). An improvement on Horn’s parallel analysis methodology for selecting the correct number of factors to retain. Educational and Psychological Measurement, 55, 377–393.
Gorsuch, R. L. (1983). Factor analysis (2nd ed.). Hillsdale, NJ: Erlbaum.
Hayton, J. C., Allen, D. G., & Scarpello, V. (2004). Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational Research Methods, 7, 191–205.
Helgeson, V. S., Reynolds, K. A., & Tomich, P. L. (2006). A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology, 74, 797–816.
Hogarty, K. Y., Hines, C. V., Kromrey, J. D., Ferron, J. M., & Mumford, K. R. (2005). The quality factor solutions in exploratory factor analysis: The influence of sample size, communality, and overdetermination. Educational and Psychological Measurement, 65, 202–226.
Keyes, C. (1998). Social well-being. Social Psychology Quarterly, 61, 121–140.
Keyes, C. (2005). Mental illness and/or mental health? Investigating axioms of the complete state model of health. Journal of Consulting and Clinical Psychology, 73, 539–548.
Keyes, C., Shmotkin, D., & Ryff, C. (2002). Optimizing well-being: The empirical encounter of two traditions. Journal of Personality and Social Psychology, 82, 1007–1022.
Luttrell, A., Petty, R. E., Briñol, P., & Wagner, B. C. (2016). Making it moral: Merely labeling an attitude as moral increases its strength. Journal of Experimental Social Psychology, 65, 82–93.
MacCallum, R. C., Widaman, K. F., Zhang, S., & Hong, S. (1999). Sample size in factor analysis. Psychological Methods, 4, 84–99.
Martín-Baró, I. (1998). Political violence and war as causes of psychosocial trauma in El Salvador. International Journal of Mental Health, 18, 3–20.
Nawijn, L., van Zuiden, M., Frijling, J. L., Koch, S. B., Veltman, D. J., & Olff, M. (2015). Reward functioning in PTSD: a systematic review exploring the mechanisms underlying anhedonia. Neuroscience and Biobehavioral Reviews, 51, 189–204.
Neria, Y., DiGrande, L., & Adams, B. G. (2011). Posttraumatic stress disorder following the September 11, 2001, terror attacks: A review of the literature among highly exposed populations. American Psychologist, 66, 429–446.
Neria, Y., Nandi, A., & Galea, S. (2008). Post-traumatic stress disorder following disasters: A systematic review. Psychological Medicine, 38, 467–480.
Norris, F. H., Friedman, M. J., Watson, P. J., Byrne, C. M., Diaz, E., & Kaniasty, K. (2002). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry, 65, 207–239.
O’Connor, B. P. (2000). SPSS and SAS programs for determining the number of components using parallel analysis and Velicer’s MAP test. Behaviour Research Methods, Instruments, & Computers, 32, 396–402.
Rimé, B., Páez, D., Basabe, N., & Martínez, F. (2009). Social sharing of emotion, post-traumatic growth, and emotional climate: Follow-up of Spanish citizen’s response to the collective trauma of March 11th terrorist attacks in Madrid. European Journal of Social Psychology, 40, 1029–1045.
Rodríguez-Carvajal, R., Díaz-Méndez, D., Moreno-Jiménez, B., Blanco-Abarca, A., & van Dierendonck, D. (2010). Vitality and inner resources as relevant components of psychological well-being. Psicothema, 22, 63–70.
Ryff, C. (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57, 1069–1081.
Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., et al. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS ONE, 8, e59236.
Shahar, G., Noyman, G., Schnidel-Allon, I., & Gilboa-Schechtman, E. (2013). Do PTSD symptoms and trauma-related cognitions about the self constitute a vicious cycle? Evidence for both cognitive vulnerability and scarring models. Psychiatry Research, 205, 79–84.
Silver, R. C., Holman, E. A., McIntosh, D. N., Poulin, M., & Gil-Rivas, V. (2002). Nationwide longitudinal study of psychological responses to September 11. JAMA, 288, 1235–1244.
Van Dierendonck, D., Díaz, D., Rodríguez-Carvajal, R., Blanco, A., & Moreno-Jiménez, B. (2008). Ryff’s six-factor model of psychological well-being, a Spanish exploration. Social Indicators Research, 87, 473–479.
Vázquez, C., & Hervás, G. (2010). Terrorist attacks and benefit finding: The role of positive and negative emotions. Journal of Positive Psychology, 5, 154–163.
Vázquez, C., Hervás, G., & Pérez-Sales, P. (2008). Chronic thought suppression as a vulnerability factor to posttraumatic symptoms: data from the Madrid March 11, 2004 terrorist attack. Journal of Anxiety Disorders, 22, 1226–1236.
Verger, P., Dab, W., Lamping, D. L., Loze, J. Y., Deschaseaux-Voinet, C., Abenhaim, L., et al. (2004). The psychological impact of terrorism: an epidemiologic study of posttraumatic stress disorder and associated factors in victims of the 1995–1996 bombings in France. American Journal of Psychiatry, 161, 1384–1389.
World Health Organization. (1946). Constitution of the World Health Organization. American Journal of Public Health and the Nation’s Health, 36, 1315–1323.
Acknowledgements
This research was supported by Ministry of Economy and Competitiveness—Government of Spain (PSI2012-37808; SEJ2006-14894).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Díaz, D., Stavraki, M., Blanco, A. et al. 11-M Victims 3 Years After Madrid Terrorist Attacks: Looking for Health Beyond Trauma. J Happiness Stud 19, 663–675 (2018). https://doi.org/10.1007/s10902-016-9842-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10902-016-9842-x