Abstract
Purpose
Although non-pharmacological interventions have been shown to improve physical functioning in individuals with osteoarthritis (OA), the mechanisms by which this occurs are often unclear. This study assessed whether changes in arthritis self-efficacy, perceived pain control, and pain catastrophizing mediated changes in physical functioning following an osteoarthritis intervention involving weight management, physical activity, and cognitive-behavioral pain management.
Method
Three hundred Veteran patients of 30 primary care providers with knee and/or hip OA were cluster randomized to an OA intervention group or usual care. The OA intervention included a 12-month phone-based patient behavioral protocol (weight management, physical activity, and cognitive-behavioral pain management) plus patient-specific OA treatment recommendations delivered to primary care providers.
Results
Using linear mixed models adjusted for provider clustering, we observed that baseline to 6-month changes in arthritis self-efficacy and pain control partially mediated baseline to 12-month physical functioning improvements for the intervention group; catastrophizing did not.
Conclusion
Findings of a mediating role of arthritis self-efficacy and pain control in intervention-related functional changes are consistent with hypotheses and align with theoretical assertions of the role of cognitions in cognitive and behavioral interventions for chronic pain. However, contrary to hypotheses, catastrophizing was not found to be a mediator of these changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a widespread and debilitating condition, affecting 27 million Americans [1] with prevalence on the rise [2, 3]. Evidence-based guidelines for OA emphasize the importance of combining medical approaches with behavioral interventions, such as cognitive-behavioral therapy (CBT) for pain, weight management, and exercise, all of which have shown efficacy for improving symptom management [4,5,6,7,8]. With an eye toward maximizing benefit for patients, many interventions have combined multiple behavioral strategies. Although these programs have demonstrated improvements in pain and function [7, 9], few studies have explored the mechanisms for these changes. Gaining a better understanding of the processes by which these interventions exert effects can inform the design of more efficient and effective interventions. This study is a secondary mediation analysis exploring mechanisms of change in physical functioning in the context of a randomized controlled trial (RCT) of a multifaceted intervention for Veterans with OA.
Literature examining diverse behavioral interventions for pain suggests that changes in the ways individuals think about their arthritis are one key pathway for gains in functional outcomes [7, 10,11,12]. Of these behavioral treatments, CBT is unique in targeting cognitive change as the primary intervention strategy, as its underlying theory asserts that changing thoughts about pain can bring about decreased pain and improved function [13]. In CBT for pain, participants work to restructure maladaptive cognitions and patterns of thinking about their pain such as catastrophizing (i.e., magnification of the threat of chronic pain and helplessness in the face of pain) and increase adaptive pain cognitions such as self-efficacy (i.e., confidence in ability to manage chronic pain-related symptoms) and pain control (i.e., perceived ability to exert control over one’s pain). Changes in these cognitions have been shown to relate to improvements in functioning through CBT (e.g., [10]). Although cognitions may not be the primary or only intended process of change in other behavioral interventions, research on exercise, physical therapy, and weight loss interventions for chronic pain have also suggested a role for cognitions as mechanisms of change in functional outcomes [7, 11, 12, 14,15,16,17]. For example, in a randomized controlled trial, Smeets and colleagues (2006) compared active physical treatment, CBT, active physical treatment + CBT, and wait list control groups of individuals with chronic low back pain. Change in pain catastrophizing mediated improvements in disability for all groups except the wait list group, suggesting that cognitions may act as mechanisms of change even in treatments that do not explicitly target them. Changes in cognitions have also been demonstrated in observational studies of patients undergoing multidisciplinary treatments for chronic pain [18,19,20], accounting for 26% of the variance in improved physical functioning for participants completing one 4-week multidisciplinary pain program [19].
Despite strong suggestions for a key role of cognitions as mechanisms of change in interventions for chronic pain, the majority of this literature has serious methodological flaws, either utilizing synchronous (cross) correlations (e.g., [11]) or using lagged correlations without a treatment control group (e.g., [18]) [21]. Mediation analyses allow for the analysis of mechanisms of change over time. Principled methods of mediation (1) demonstrate temporal precedence between the mediator and the outcome and (2) include a control group that allows for causal interpretations about the role of therapy associated with the change in cognitions [22, 23].
The current study is the first to use temporal mediation to explore cognitive processes of change in a multifaceted OA intervention. Specifically, we explored whether changes in arthritis self-efficacy, catastrophizing, and perceived control over pain, measured at the midpoint of the intervention, predicted improvements in physical functioning following the intervention. In order to demonstrate that a factor is a mediator of treatment, the factor must (1) demonstrate change occurring during treatment; (2) be correlated with treatment group, thus potentially being the result of treatment; and (3) have an effect on the outcome [23]. Measuring changes in cognitions 6 months after the randomization and before physical functioning was measured following intervention completion allows for conclusions to be made about whether intervention-related changes in cognitions help to explain intervention-related changes in physical functioning measured 6 months later. Arthritis self-efficacy, catastrophizing, and perceived control over pain were selected because they have been the most commonly analyzed mechanisms of change in behavioral interventions for chronic pain [10,11,12, 15, 17, 24]. Based on this prior research, we expected that all three cognitions would partially explain treatment-related changes in functioning. Physical function was the outcome of interest because of its important role in OA and because there were significant, yet modest, changes in this outcome following the intervention [25]. The goal of this analysis was to determine whether changes in pain cognitions played a role in this effect, as hypothesized.
Methods
The institutional review board of the Department of Veterans Affairs HealthCare System in Durham, NC (DVAHCS), approved this study. All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all participants. Detailed methods and primary study results have been published previously [25, 26].
Study Design
This was a secondary analysis of a cluster-randomized controlled trial, with primary care providers (PCPs) randomized to OA intervention (nPCPs = 15; nVeterans = 151) or usual care control (nPCPs = 15; nVeterans = 149). We enrolled approximately 10 patient participants for each PCP. PCPs assigned to the OA intervention received the provider intervention, and their enrolled patient participants received the patient intervention. Patient participants in both arms continued with usual medical care recommended by their providers.
Participants and Recruitment
PCPs in the DVAHCS Ambulatory Care Service with patient panels large enough to likely enroll n = 10 participants were invited to participate. Patients were eligible if they had hip OA and/or knee OA, were overweight (body mass index (BMI) ≥ 25), and engaged in low physical activity (see Allen et al. [26] for details and exclusion criteria). Potential participants were identified from DVAHCS electronic medical records, mailed an introductory letter, and called for a screening interview. Potential patient participants were blinded to their PCP’s randomization until after baseline assessments.
Interventions
Patient Intervention
The intervention lasted 12 months and focused on physical activity, weight management, and cognitive-behavioral pain management strategies [26]. A counselor taught CBT skills alongside general exercise and dietary strategies via telephone. Cognitive restructuring was taught during months 9 and 10. Calls were scheduled twice per month for the first 6 months, then monthly for the last 6 months, and were delivered by one counselor with training in OA, health education, and behavior change, with oversight provided by study co-investigators. Goal setting, action planning, and motivational interviewing strategies were major components of the intervention. Participants were given written patient educational materials, an exercise video for patients with OA, and an audio CD of relaxation exercises.
Provider Intervention
This intervention involved delivery of patient-specific OA treatment recommendations to PCPs via the electronic medical record, based on published treatment guidelines (e.g., refer to physical therapist, recommended topical NSAID, or capsaicin [6, 8, 27]).
Measures
Baseline and 12-month follow-up measures were completed in-person with allowance for telephone-based assessments as needed. Six-month measures of cognitions were assessed via telephone. Outcome assessors were blind to randomization.
Outcome
The primary outcome measure was the physical function subscale of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), a self-report measure (17 items) referencing difficulty completing everyday physical tasks over the past 2 weeks [28,29,30]. All items are rated on a five-point Likert scale ranging from “none” to “extreme” (higher scores indicate worse function). The reliability and the validity of the WOMAC subscales have been confirmed [28, 31]. Cronbach’s alphas for the physical functioning subscale at both baseline and 12-month time points were 0.96. The outcome was the change score (12-month score minus baseline score); participants with missing baseline or follow-up WOMAC were not included.
Mediators
The Arthritis Self-Efficacy Scale examines perceived ability to cope with arthritis symptoms [32]. This scale includes eight items asking respondents how certain they are that they can perform specific activities or tasks. Items are scored on a Likert scale (1 = very uncertain to 10 = very certain). The scale has shown acceptable construct validity, internal reliability, and test-retest reliability [32]. Cronbach’s alphas for arthritis self-efficacy were 0.91 at baseline, 0.92 at 6 months, and 0.93 at 12 months. The mediator variable was the change score calculated as 6-month score minus baseline score (12-month score minus baseline score for sensitivity analyses); participant with missing baseline or follow-up data were not included.
Pain control was measured using two items from the Coping Strategies Questionnaire [33]. Participants were asked “Based on all the things you did to cope, or deal, with your arthritis pain during the last week, how much control do you feel you had over it?” and “Based on all the things you did to cope, or deal, with your arthritis pain during the last week, how much were you able to decrease it?” They rated responses on a 0–6 scale (0 = no control to 6 = complete control or can decrease it completely). These two items have been previously used as a measure of pain control related to pain intensity and coping [34, 35]. Cronbach’s alphas for pain control were 0.77 at baseline and 6 months and 0.81 at 12 months. The mediator variable was the change in score calculated as 6-month score minus baseline score (12-month score minus baseline score for sensitivity analyses); participants with missing baseline or follow-up data were not included.
Catastrophizing was measured using the Pain Catastrophizing Scale (PCS), a 13-item self-report scale asking participants to rate the degree to which they experience specific thoughts and feelings when experiencing pain on a five-point scale (0 = not at all to 4 = all the time). The PCS has demonstrated good reliability and validity [36,37,38]. Cronbach’s alphas for pain catastrophizing were 0.96 at baseline, 6 months, and 12 months. The mediator variable was the change score calculated as 6-month PCS minus baseline PCS (12-month PCS minus baseline PCS for sensitivity analyses); subjects with missing baseline or follow-up data were not included.
Covariates
Mirroring the main study analyses [25], all models included a dichotomous (white vs. non-white) self-reported race variable, which was used as a stratifying variable for randomization.
Data Analyses
First, descriptive analyses including intercorrelations among all mediation analysis variables were performed. Linear mixed models were then fit with WOMAC physical function change from baseline to 12 months as the outcome using the PROC MIXED procedure using SAS software, version 9.4 (SAS Institute Inc., 2014, Cary, NC). A random effect to account for clustering of PCPs was used. The intervention group indicator variable was dummy coded—½ vs. ½, and all mediator variables were centered at 0, in accordance with Kraemer and colleagues’ [22, 23] recommendations for assessing mediators of treatment effects in RCTs. All models included the interactions between the intervention group and mediators to account for any interactive effects [22, 23].
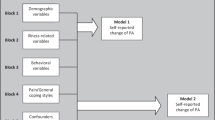
Mediation models were first fit separately for each individual mediator then fit together in a single model. We planned a priori to include all hypothesized mediators in the full model, whether or not they demonstrated significant mediation effects in the individual models. This decision was made to clarify the roles of each individual cognition, in the context of the others, as previous literature has demonstrated that pain cognitions tend to predict other, similar types of pain cognitions [39]. First, we confirmed the effect of the intervention on change in physical functioning outcome from baseline to 12 months (coefficient c in Fig. 1). We then tested for differences between the intervention and control groups in baseline to 6-month change in cognitions (catastrophizing, arthritis self-efficacy, and pain control; coefficient a in Fig. 1). Next, we examined whether the baseline to 6-month changes in the cognitive mediators predicted the outcome: baseline to 12-month change in physical functioning, with the intervention group variable in the model (coefficient b in Fig. 1). We calculated the product of the coefficients (a × b [40]) and used RMediation [41] to estimate the mediated effects and their associated asymmetric 95% confidence limits.
Finally, analyses were conducted to explore whether the mediation effect remained over and above variables that could also be considered potential mediators: depression (Patient Health Questionnaire-8 [42]) and physical activity (Community Health Activities Model Program for Seniors scale [43, 44]). These variables were n measured, only at baseline and 12 months. The same methods described in the primary analysis were used to explore the mediation effect of baseline to 12-month change in catastrophizing, arthritis self-efficacy, and pain control on baseline to 12-month change in physical functioning in the intervention group. Baseline to 12-month change in depression and physical activity were then added to the model to determine whether the mediation effects were maintained when adjusting for these effects.
Results
Descriptive Analysis
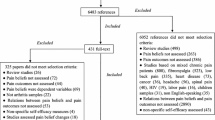
Demographic and baseline scores for all variables based on are presented in Table 1. Randomized participants were an average age of 61.1 (±9.2) years, predominantly male (90.7%), and obese (mean BMI 33.8 ± 5.8), most with osteoarthritis of the knee only (79.3%). There were no significant differences in outcome, mediator, or covariate variables between groups. Mean change scores for outcome, mediator, and covariate variables are presented in Table 2. Some data were missing due to participants who were excluded (due to developing a contraindicated/exclusionary health condition), were lost to follow-up (unable to be reached), scoring algorithms, and/or persons who declined to participate. N values for the number of participants per group included in the following analyses are presented in Table 2.
Evaluation of intercorrelations among mediation analysis variables revealed that they were all significantly related (r values 0.21–0.52, all ps ≤ 0.001). As expected, baseline to 6-month increases in arthritis self-efficacy and pain control were correlated with baseline to 12-month improvements in physical functioning. Baseline to 6-month changes in catastrophizing were negatively correlated with baseline to 12-month changes in physical functioning.
Mediation Analysis
First, we confirmed using our model that the intervention group showed a significantly greater improvement in physical functioning compared to the control group (c path in Fig. 2; c = − 3.39, SE = 1.54, p = 0.04). Next, we determined whether or not intervention group membership predicted differences in baseline to 6-month change in arthritis self-efficacy, catastrophizing, and pain control separately. Findings, depicted as paths a1 and a2 in Fig. 2, revealed that individuals in the intervention group showed greater increases in arthritis self-efficacy and pain control from baseline to 6 months than the control group, but not so for catastrophizing. Third, we examined whether increases in arthritis self-efficacy and pain control predicted baseline to 12-month improvements in physical functioning. When assessed in independent models, both arthritis self-efficacy (a1b1 = − 0.86, SE = 0.41, 95% CI [− 1.75, − 0.16]) and pain control (a1b1 = − 0.88, SE = 0.38, 95% CI [− 1.72, − 0.21]) significantly mediated the link between intervention group and baseline to 12-month change in physical functioning. When included together in the model, along with catastrophizing (presented in Fig. 2), baseline to 6-month changes in arthritis self-efficacy (b1 path) and pain control (b2 path) were still significantly related to baseline to 12-month changes in physical functioning, beyond the contributions of intervention group and all interaction terms (intervention group × change in cognitions). The indirect effects for both arthritis self-efficacy and pain control confirmed mediating roles (a1b1 = − 0.54, SE = 0.33, 95% CI [− 1.30, − 0.04]; a2b2 = − 0.59, SE = 0.33, 95% CI [− 1.33, − 0.08]). The direct effect of intervention group on change in physical functioning was no longer significant after including the mediators in the model (c′ = − 2.02, SE = 1.52, p = 0.20). Thus, the intervention group’s increases in arthritis self-efficacy and pain control cognitions (but not catastrophizing) from baseline to the intervention midpoint helped to explain their greater improvement in physical functioning from baseline to intervention completion compared to the control group.
In an additional analysis, we followed the same procedure to determine whether these mediating effects of cognitive changes in response to the intervention remained when controlling for baseline to 12-month intervention-related changes in depressive symptoms and physical activity. Baseline to 12-month change in arthritis self-efficacy was found to be the only significant mediator of the link between intervention group membership and baseline to 12-month change in physical functioning when baseline to 12-month changes in pain control, depression, and physical activity were included in the model (results available upon request). Thus, the intervention group’s increased arthritis self-efficacy over the course of the intervention predicted their greater intervention-related improvements in physical functioning compared to the control group. This impact was distinct from that of their intervention-related changes in depressive symptoms and physical activity.
Discussion
This secondary analysis of a large RCT of a multifaceted OA intervention demonstrated that changes in arthritis self-efficacy and perceived control over pain in the first 6 months of treatment partially explained intervention-related improvements in physical functioning. Contrary to our hypothesis, the intervention group did not report decreases in catastrophizing at the treatment midpoint compared to the control group, and thus, catastrophizing was not found to mediate improved physical functioning for the intervention group. The mediating effect of arthritis self-efficacy persisted even after adjusting for mediation effects of pain control and catastrophizing and intervention-related changes in physical activity and depression symptoms, two alternative potential intervention-related processes of change. These analyses are the first to demonstrate pain cognitions as mechanisms of change in a multifaceted intervention for chronic pain in a controlled design where the mediators precede the outcomes, improving upon past weaknesses in the literature [21]. The results are consistent with cognitive-behavioral and health behavior change theories, building an even stronger case for the importance of cognitions in functional improvements through behavioral means in OA and other chronic pain populations.
These findings reinforce a key role for self-efficacy as a mechanism of change in multifaceted interventions for chronic pain. Self-efficacy is a common thread in multiple health behavior change theories, e.g., social cognitive theory, health locus of control, and theory of self-regulation [16, 45,46,47,48,49]. The multifaceted intervention in the current study specifically targeted self-efficacy, using skills including mastery, modeling, persuasion, and reinterpretation of symptoms (cognitive restructuring). Goal setting was also a primary component of the intervention; counselors helped participants adjust goals when they reported low self-efficacy for accomplishing goals. Our findings are consistent with studies suggesting a mediating role for self-efficacy in predicting physical functioning improvements after exercise [14, 17] and CBT interventions [10].
While pain control/helplessness has been found to mediate change in disability in some trials of CBT and multidisciplinary treatment approaches (e.g., [10, 18, 50]), in at least one study of behavioral interventions for chronic low back pain, perceived pain control did not improve [11]. In Turner and colleagues’ [10] temporal mediation analysis of CBT, self-efficacy and pain control were both found to mediate CBT-related disability improvements in individual models. However, when included in the same model, self-efficacy predicted little variance in disability beyond perceived control. The authors interpreted these findings to indicate that these constructs might be related. In our study, both self-efficacy and pain control showed significant improvement, even when included together in the mediation model. However, only self-efficacy remained significant when additional possible mediators were included in the 12 month analysis. These findings suggest the need for further analysis regarding relations between pain cognition processes of change.
Contrary to our hypotheses, there were no differences in catastrophizing between the intervention and control groups at the midpoint or conclusion of the intervention. This finding is inconsistent with a number of past studies suggesting a mediating role for catastrophizing in functional improvements after multiple types of interventions (e.g., [10,11,12, 24, 51, 52]). Whereas there were a number of planned techniques to increase self-efficacy through the study, cognitive restructuring was the primary mechanism proposed to target catastrophizing, and it was a relatively small part of a large intervention (2/18 sessions) that occurred toward the end of treatment (after the midpoint mediation assessment). Thus, any change from baseline to midpoint was related to the physical activity, weight loss, and behavioral therapy (e.g., relaxation) aspects of the intervention covered in the first 6 months. However, we also did not find an intervention group difference in catastrophizing from baseline to 12 months. The dose of cognitive restructuring in the intervention may have been too low to effect a significant change in pain catastrophizing. Given past data showing links between decreased catastrophizing and improved pain-related outcomes, the current intervention may have demonstrated more markedly improved outcomes if it had resulted in decreases in catastrophizing. Future trials investigating mediating effects should consider additional measurement points throughout the intervention, at time points relevant to the timing of the intervention mechanism proposing to target the mediator, in order to better capture change in mediators while also maintaining temporal precedence.
Some limitations should be noted regarding these analyses. We focused on cognitions as mechanisms, but there are other potential processes of change for improving functioning in these types of interventions (e.g., increased strength and endurance through exercise, decreased weight resulting in less pain). Future studies should use a theory-based approach to identify and assess other potential mediators in order to understand relative impact on outcomes, in order to improve interventions. Additionally, as the intervention consisted of multiple components (physical activity, cognitive-behavioral), many of which could impact cognitions, it is not possible to determine the relative contribution of each component on the change in cognitions. Subjects with missing follow-up data were case deleted; however, results from our models for the physical function outcome were similar to those presented in the main study paper, which used all available subject data indicating that case deletion was not problematic. Furthermore, we found in the main study paper that results from a sensitivity analysis using multiply imputed data were very similar to the main study results [25]. As shown on the CONSORT diagram in the main outcomes paper [25], the numbers of individuals in the intervention and control groups were similar with respect to missed assessments/lost to follow-up/exclusions and withdrawals at 6 and 12 months. For WOMAC physical function, an additional subject in each arm is missing due to missing items in the survey at 12 months. For the mediators, with respect to missed assessments/lost to follow-up/exclusions and withdrawals at 6 months, 21 observations were missing from the intervention group and 16 observations were missing in usual care. For pain catastrophizing, there were an additional six subjects in control and seven subjects in the intervention group missing due to missing items in the survey at 6 months. Finally, the study population consisted of Veterans (primarily male); thus, these findings may not generalize across different populations.
In summary, this study’s temporal, controlled design allowed for a rigorous mediation analysis of intervention-related effects on outcomes in a large sample of patients with OA. This analysis was the first to our knowledge to demonstrate that arthritis self-efficacy and pain control serve as mechanisms of change through a multifaceted intervention for chronic pain involving physical activity, weight loss, and cognitive-behavioral components. These findings add to previous literature asserting the critical role of cognitions in improving functional outcomes for patients with chronic pain. Our findings suggest that behavioral interventions for chronic pain should emphasize techniques shown to increase self-efficacy, such as development and practice to relevant skills, observation of others, and personal accomplishments to increase experiences of mastery [45, 46, 53, 54]. Increased focus on cognitive restructuring, with the goal of increasing adaptive cognitions such as self-efficacy, may promote improved outcomes in future interventions. Ongoing work exploring how and why functional outcomes improve throughout the course of behavioral treatments for chronic pain will help inform the design of more effective and more efficient interventions.
References
Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. https://doi.org/10.1002/art.23176.
Barbour KE. Prevalence of doctor-diagnosed arthritis at state and county levels—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65.
Nguyen U-SD, Zhang Y, Zhu Y, Niu J, Zhang B, Felson DT. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155(11):725–32.
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4):465–74.
Zhang W, Moskowitz R, Nuki G, Abramson S, Altman R, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthr Cartil. 2007;15(9):981–1000.
Zhang W, Nuki G, Moskowitz R, Abramson S, Altman R, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil. 2010;18(4):476–99.
Somers TJ, Blumenthal JA, Guilak F, Kraus VB, Schmitt DO, Babyak MA, et al. Pain coping skills training and lifestyle behavioral weight management in patients with knee osteoarthritis: a randomized controlled study. Pain. 2012;153(6):1199–209.
Richmond J, Hunter D, Irrgang J, Jones MH, Snyder-Mackler L, Van Durme D, et al. American Academy of Orthopaedic surgeons clinical practice guideline on the treatment of osteoarthritis (OA) of the knee. J Bone Joint Surg. 2010;92(4):990–3.
Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–73. https://doi.org/10.1001/jama.2013.277669.
Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive–behavioral therapy for chronic pain. Pain. 2007;127(3):276–86.
Smeets RJ, Vlaeyen JW, Kester AD, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain. 2006;7(4):261–71.
Burns JW, Day MA, Thorn BEI. Reduction in pain catastrophizing a therapeutic mechanism specific to cognitive-behavioral therapy for chronic pain? Transl Behav Med. 2012;2(1):22–9.
Turk DC. A cognitive-behavioral perspective on treatment of chronic pain patients. Psychological approaches to pain management: a practitioner’s handbook. 2nd ed. New York: Guilford Press; 2002.
Focht BC, Rejeski WJ, Ambrosius WT, Katula JA, Messier SP. Exercise, self-efficacy, and mobility performance in overweight and obese older adults with knee osteoarthritis. Arthritis Care Res. 2005;53(5):659–65.
George SZ, Zeppieri G, Cere AL, Cere MR, Borut MS, Hodges MJ, et al. A randomized trial of behavioral physical therapy interventions for acute and sub-acute low back pain (NCT00373867). Pain. 2008;140(1):145–57.
Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: implications for health education practice (part I). Health Promot Pract. 2005;6(1):37–43. https://doi.org/10.1177/1524839904266790.
Rejeski WJ, Martin K, Ettinger WH, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Rheum. 1998;11(2):94–101.
Burns JW, Glenn B, Bruehl S, Harden R, Lofland K. Cognitive factors influence outcome following multidisciplinary chronic pain treatment: a replication and extension of a cross-lagged panel analysis. Behav Res Ther. 2003;41(10):1163–82.
Moss-Morris R, Humphrey K, Johnson MH, Petrie KJ. Patients’ perceptions of their pain condition across a multidisciplinary pain management program: do they change and if so does it matter? Clin J Pain. 2007;23(7):558–64.
Vowles KE, McCracken LM, Eccleston C. Processes of change in treatment for chronic pain: the contributions of pain, acceptance, and catastrophizing. Eur J Pain. 2007;11(7):779–87.
Morley S, Keefe FJ. Getting a handle on process and change in CBT for chronic pain. Pain. 2007;127(3):197–8.
Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychol. 2008;27(2S):S101.
Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59(10):877–83.
Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9(5):745–58. https://doi.org/10.1586/ERN.09.34.
Allen KD, Yancy WS, Bosworth HB, Coffman CJ, Jeffreys AS, Datta SK, et al. A combined patient and provider intervention for Management of Osteoarthritis in veterans: a randomized clinical trial. Ann Intern Med. 2016;164(2):73–83.
Allen KD, Bosworth HB, Brock DS, Chapman JG, Chatterjee R, Coffman CJ, et al. Patient and provider interventions for managing osteoarthritis in primary care: protocols for two randomized controlled trials. BMC Musculoskelet Disord. 2012;13(1):60.
ASo O. Recommendations for the medical management of osteoarthritis of the hip and knee. 2000 update. Arthritis Rheum. 2000;43(9):1905–15.
Bellamy N. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol. 1988;1:95–108.
Bellamy N. WOMAC: a 20-year experimental review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29(12):2473–6.
Bellamy N, Buchanan W. A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol. 1986;5(2):231–41.
McConnell S, Kolopack P, Davis AM. The western Ontario and McMaster universities osteoarthritis index (WOMAC): a review of its utility and measurement properties. Arthritis Care Res. 2001;45(5):453–61.
Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32(1):37–44.
Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17(1):33–44.
Keefe FJ, Affleck G, Lefebvre JC, Starr K, Caldwell DS, Tennen H. Pain coping strategies and coping efficacy in rheumatoid arthritis: a daily process analysis. Pain. 1997;69(1):35–42.
Affleck G, Urrows S, Tennen H, Higgins P. Daily coping with pain from rheumatoid arthritis: patterns and correlates. Pain. 1992;51(2):221–9.
Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524.
Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The pain catastrophizing scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23(4):351–65.
Osman A, Barrios FX, Kopper BA, Hauptmann W, Jones J, O’Neill E. Factor structure, reliability, and validity of the pain catastrophizing scale. J Behav Med. 1997;20(6):589–605.
Gil KM, Williams DA, Keefe FJ, Beckham JC. The relationship of negative thoughts to pain and psychological distress. Behav Ther. 1990;21(3):349–62. https://doi.org/10.1016/S0005-7894(05)80336-3.
Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivar Behav Res. 2001;36(2):249–77.
Tofighi D, MacKinnon DP. RMediation: an R package for mediation analysis confidence intervals. Behav Res Methods. 2011;43(3):692–700.
Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1):163–73.
Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–41.
Hekler EB, Buman MP, Haskell WL, Conway TL, Cain KL, Sallis JF, et al. Reliability and validity of CHAMPS self-reported sedentary-to-vigorous intensity physical activity in older adults. J Phys Act Health. 2012;9(2):225.
Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice-Hall series in social learning theory. Englewood Cliffs: Prentice-Hall, Inc; 1986.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191.
Leventhal H, Safer MA, Panagis DM. The impact of communications on the self-regulation of health beliefs, decisions, and behavior. Health Educ Behav. 1983;10(1):3–29.
Shortridge-Baggett LM. Self-efficacy: measurement and intervention in nursing. Scholarly Inquirty in Nursing Practice. 2001;15:183–8.
Strecher VJ, DeVellis BM, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Educ Behav. 1986;13(1):73–92.
Woby SR, Watson PJ, Roach NK, Urmston M. Are changes in fear-avoidance beliefs, catastrophizing, and appraisals of control, predictive of changes in chronic low back pain and disability? Eur J Pain. 2004;8(3):201–10.
Mansell G, Kamper SJ, Kent P. Why and how back pain interventions work: what can we do to find out? Best Pract Res Clin Rheumatol. 2013;27(5):685–97.
Wertli MM, Burgstaller JM, Weiser S, Steurer J, Kofmehl R, Held U. Influence of catastrophizing on treatment outcome in patients with nonspecific low back pain: a systematic review. Spine. 2014;39(3):263–73.
Schiaffino KM, Revenson TA, Gibofsky A. Assessing the impact of self-efficacy beliefs on adaptation to rheumatoid arthritis. Arthritis Rheum. 1991;4(4):150–7.
Shelby RA, Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Blumenthal JA. Domain specific self-efficacy mediates the impact of pain catastrophizing on pain and disability in overweight and obese osteoarthritis patients. J Pain. 2008;9(10):912–9.
Funding
This project was supported by the Department of Veterans Affairs, Health Services Research and Development Service (IIR 10-126). This work was also supported by the Center of Innovation for Health Services Research in Primary Care (CIN 13-410) at the Durham Veterans Affairs HealthCare System. Dr. Taylor is funded by a VA Office of Academic Affiliations, Health Services Research and Development Service postdoctoral fellowship (TPH 21-000). Dr. Bosworth is funded by a Veterans Affairs Career Scientist award (08-027).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Veterans Affairs.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Taylor, S.S., Oddone, E.Z., Coffman, C.J. et al. Cognitive Mediators of Change in Physical Functioning in Response to a Multifaceted Intervention for Managing Osteoarthritis. Int.J. Behav. Med. 25, 162–170 (2018). https://doi.org/10.1007/s12529-017-9689-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-017-9689-5