Abstract
Although there is limited knowledge about early signs of ADHD, deviations in motor development are suggested as a possible indicator of such early signs. The purpose of the present systematic review was to gather knowledge about motor development before three years of age in children later diagnosed with ADHD. A systematic search was completed in four research databases, and the quality of the identified studies was systematically assessed. Of 440 initial search results, only five studies met the inclusion criteria and were fully abstracted. Major methodological heterogeneity was found between the studies, and the results are pointing in various directions. One study found an association between delay in gross motor development and ADHD, while another did not. However, associations between both good early motor development as well as delayed were also found in one study. A study of premature infants showed no association between early motor development and attention problems at school age, and a study of high-risk children from a neonatal care unit found no association between abnormal general movements and later ADHD without comorbidity. The results of the studies are pointing in various directions. No firm conclusion can be drawn on early motor development in children with ADHD due to the very different results of the studies and the methodological heterogeneity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD) may appear already during early childhood, and the disorder has major consequences for both the child and the family (Rappley 2005). Recent studies have shown that early intervention may improve the development and behaviour in children with ADHD (Charach et al. 2013). Accordingly, it is important to be able to diagnose and initiate proper treatment at an early age. However, the average age of diagnosis is 8–10 years (Atladottir et al. 2015) and studies of the very early signs of ADHD are sparse, implying that it is problematic to diagnose children at an early age. An early marker of ADHD would assist in making an early clinical diagnosis possible, leading to early intervention and thus the possibility of improving the development of children with ADHD (Charach et al. 2013). Impaired early motor development might be an early indicator of ADHD (Lemcke et al. 2016).
School-age children with ADHD often have other comorbid disorders. A Swedish cohort study of 409 children found that 87% of the children with diagnosed ADHD had one comorbid disorder, and 67% had two or more (Kadesjo and Gillberg 2001). Likewise, a large Danish register-based study showed that 52% of the children with ADHD had at least one comorbid disorder, and 26% had two or more (Jensen and Steinhausen 2015). In addition, among the most common comorbid disorders identified were specific developmental disorders including delayed motor development. Several studies have shown that more than half of children aged 6–16 years diagnosed with ADHD have difficulties with gross and fine motor skills (Kaiser et al. 2014). Furthermore, in a case–control study of 486 children aged 5 years or more with ADHD, Fliers et al. (2008) found that 34% of the boys and 29% of the girls met the diagnostic criteria for Development Coordination Disorder (DCD). In the literature, it is discussed whether motor problems may be inherent in ADHD or mediated by comorbid DCD. However, there is very limited knowledge about the motor development below school age in children with ADHD.
Definition of the term motor development and related terminology is discussed in the literature with no clear consensus. In this review, motor development is defined as motor skills that build on postural control, depending on reflex adjustment of tone in a large number of muscles in response to visual and proprioceptive feedback. It develops in a cephalocaudal (head to tail) direction starting with head control, and then progressing with sitting, standing, walking and running (McIntosh et al. 2008). In addition, it is important to notice that in this review the term motor development does not include the activity level in infants.
Very early movements present in foetal life and until 3–4 months of age are referred to as general movements (GMs) (Hitzert et al. 2014). It is discussed whether GMs are part of the child’s motor development, or if it should be understood as early movements in the infant (Einspieler and Prechtl 2005). GMs are spontaneous movements endogenously generated, i.e. not triggered by specific sensory inputs. They are seen as complex motor patterns involving the complete infant body (Einspieler and Prechtl 2005). Already in the eighties, Professor Heinz Prechtl et al. described how measures of the quality of GMs worked as a powerful predictor of development of neurological disorders especially for cerebral palsy (Einspieler and Prechtl 2005). Since, it has been discussed if GMs can be used as a predictor for other psychiatric disorders including ADHD (Hadders-Algra and Groothuis 1999).
So far, the research concerning children with ADHD and motor development has mainly been on school-age children. The aim of this study is to critically review published research studies investigating the motor development before three years of age in children later diagnosed with ADHD.
Materials and methods
The guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA 2009) were followed as standard for producing and reporting findings in this review.
The population included in the review was children diagnosed with ADHD. Inclusion criteria for the ADHD diagnosis were either a clinical diagnosis, according to DSM-IV diagnostic criteria for Attention Deficit Hyperactivity Disorder (ADHD), including Attention Deficit Disorder (ADD) [“American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th ed. American Psychiatric Association. Washington”,] or the equivalent IDC-10 diagnosis for Hyperkinetic Disorders (F90.0), including other specified behavioural and emotional disorders without hyperactivity (F98.8) [“World HO (1993) The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. World Health Organisation, Geneva”,]. Or an ADHD diagnosis based on a validated questionnaire answered by a parent, teacher or by youth self-report, e.g. children behaviour check List (CBCL). Studies including children with congenital disorder (syndromes or genetic diseases), cerebral palsy or prenatal exposure to abuse were excluded. No restrictions were made to preterm or low weight children.
Selected for inclusion were studies assessing motor development with an age-appropriate validated measurement (e.g. Denver developmental screening test) and studies measuring motor development as a result of motor milestone achievements (e.g. walk independently). In this study, GMs are understood as a component of motor development, for which reason studies measuring GMs were included. In continuation, to insure that only early motor development was measured inclusion required that motor development was assessed in children aged three years or younger, which correspond to children in nursery care.
Information sources and search strategy
A systematic search of existing literature was performed in PubMed, Embase, PEDro and PsycInfo, using a block-searching strategy that included a free text search performed by the first author. The blocks were created based on the aim of the study. In the searches the following subject-headings assigned by the databases were used: (“Attention Deficit Disorders with Hyperactivity” OR “Attention Deficit Disorder”) AND (“Infant” OR “Toddler” OR “Early childhood”) AND (“Motor skills” OR “Motor skills disorders” OR “Motor disorders” OR “Development disabilities” OR “Child development” OR “Childhood development” OR “Motor development” OR “General movements”). In addition, further records were identified via Web Of Science by cross-checking references in selected articles (Gurevitz et al. 2014; Hadders-Algra et al. 2009a, b; Jaspers et al. 2013; Lemcke et al. 2016). The searches were restricted to human studies published in English, Danish, Swedish and Norwegian. Only original papers published in peer-reviewed journals were included. To ensure a high standard for the search result, case-rapports were excluded. No restrictions on date of publication were applied, and the final search was conducted on 8 February 2018.
Data collection process
From the systematic search, articles were exported to Endnote, where duplications were removed. Publication titles and abstracts were assessed, and irrelevant studies were excluded by the first author (SH). For the remaining studies (n = 43), the full text was independently evaluated by the two authors (SH and SL) with focus on inclusion and exclusion criteria, and disagreement was discussed to achieve consensus.
Risk of bias in individual studies
Modified editions of Critical Appraisal Skills Program Checklists (CASP 2018) were used to identify risk of bias for the included cohort and case–control studies. The tools contain 12 questions and for each question there are three response ratings: “Yes”, “No” or “Cannot tell”. Question 7 “What are the results of the study” is reported in Table 1. Questions 11 and 12 were not used as too few studies have previously been done in the field to answer the questions “Do the results of this study fit with other available evidence” and “What are the implications of the study for practice”. The study appraisal was conducted independently by two authors (SH and SL). Any disagreements in scoring were resolved through discussion.
Results
Study selection and characteristics
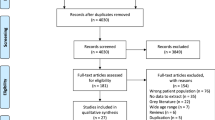
The literature search identified a total of 440 studies after removal of duplicates. Screening of title and abstract revealed 43 potential studies in which full text were assessed for eligibility. Finally, five studies were included in the review. A flowchart of the literature search is shown in Fig. 1.
Motor development was assessed by milestone achievement in four studies (Table 1), and one study was included due to GMs as a measurement of motor development (Table 1). Two studies (Gurevitz et al. 2014; Lemcke et al. 2016) included children with a clinical ADHD diagnosis, and in the three other studies the ADHD diagnosis was based on parent-rated questionnaires (Hadders-Algra et al. 2009a, b; Jaspers et al. 2013; Jeyaseelan et al. 2006).
Risk of bias within studies
The assessment of bias in the case–control and the cohort studies is shown in Tables 2 and 3. Overall, the appraisal of the included studies was good, but the following factors that could lead to bias were identified. The mean age at follow-up was only around 8 years in the case–control study by Gurevitz et al., and in the control group, no screening for ADHD was made which can lead to uncertainty about possible ADHD. Likewise, the study by Jeyaseelan et al. made follow-up on ADHD in the children at a mean age of 8.3 years. The studies by Hadders-Algra et al. and Jeyaseelan et al. included children with perinatal complications, consequently the children were “high risk” children for ADHD and the generalisability of the results can be discussed.
Association between early motor development and later ADHD
Four studies evaluated the early motor development with regard to milestones. A summary of the results is shown in Table 1. In a population of 58 children, Gurevitz et al. found a significant association between delay in gross motor development at 3, 9 and 18 months of age and later clinically diagnosed ADHD (3 months: OR = 0.31, p = 0.009. 9 months: OR = 0.254, p = 0.014. 18 months: OR = 0.043, p = 0.008) (Gurevitz et al. 2014). Gross motor development was assessed as achieved milestones, with no further subspecification. As secondary findings, they reported that significantly more children with later ADHD at 3 months of age were either hypotonic with lax ligaments (21%), hypertonic (7%) or had deformational plagiocephaly (7%). In the discussion part, but not as a result, it is mentioned that “Although most children of the ADHD group developed within the acceptable wide range of the motor milestone achievement rate, they performed at the ‘extremes’, being either early or late achievers” (Gurevitz et al. 2014, p. 6).
In a longitudinal study, including 419 children with ADHD, Jaspers et al. (2013) showed an association between good motor skills in the first year of life and later ADHD [Gross motor skills OR: 0.60, 95% CI (0.42–0.87)]. Another longitudinal birth cohort study including 2034 children with ADHD by Lemcke and co-workers found an association between a later diagnosis of ADHD and children who walked independently before 11 months [HR = 1.24 95% CI (1.08,1.44)], or after 15 months [HR = 1.66 95% CI (1.42, 1.94)]. However, most children with ADHD showed no deviations in the development of motor function (Lemcke et al. 2016). Follow-up in a cohort of 45 extreme low weight or premature infants showed no association between motor development and clinical tests of attention problems at school age, but a significant relationship between attention problems rated by parents and teachers and deviation in motor development at 24 months (Jeyaseelan et al. 2006). None of the papers included in this review describes associations between deviations in development of fine motor skills and ADHD.
In a study by Hadders-Algra et al., the association between GMs and ADHD was assessed in a small group of high-risk children (Table 1) (Hadders-Algra et al. 2009a, b). The study showed no significant association between abnormal GMs and later ADHD without comorbidity. However, children with ADHD and comorbidity had a significantly higher risk of having had abnormal GMs from birth to 4 months of age.
The influence of subtypes, sex and comorbidity
In general, the studies included in this paper reported weakly about topics like subtype, sex and comorbidity. As the only study, Gurevitz et al. (2014) divided the study cases into ADHD subtypes, ADHD and ADD. However, all results in the paper are reported for the total group, hence not specified in subtypes. All the papers identified report the gender distribution among the participants with a majority of boys, but the association with motor development is not reported.
Hadders-Algra et al. (2009a, b) found an association between abnormal GMs and children with ADHD and comorbidity. As mentioned earlier, in the study by Gurevitz et al. (2014) significantly more children showed deviations in tonus at 3 months, which might be interpreted as a comorbidity. Jaspers et al. adjusted for autism spectrum disorders, but no for other comorbidities in their analysis. However, it did not make any difference for the estimate of the association between early motor development and ADHD.
Discussion
In the systematic search, only five studies were identified that met the inclusion criteria and evaluated early motor development in children with later ADHD. The studies showed different results, from delayed motor development to good gross motor skills in the first year. The studies agreed that most children with ADHD develop as expected, however with a bipartite distribution of development of motor function to be either early or late (Gurevitz et al. 2014; Jaspers et al. 2013; Lemcke et al. 2016). No studies reported associations between minor motor difficulties and ADHD.
The association between ADHD and motor deficits in school-age children has been shown multiple times (Kaiser et al. 2014). However, the impact of comorbidity should be considered as suggested in the study by Hadders-Algra (2009a, b) and as Kaiser et al. (2014) hypothesise in a review from 2014. The influence of comorbidity was reported or discussed in three papers (Gurevitz et al. 2014; Hadders-Algra et al. 2009a, b; Lemcke et al. 2016). Hadders-Algra et al. (2009a, b) investigated it further and found, in a population consisting of 41 high-risk children, that an association between GMs and later ADHD only was present in children suffering from other psychiatric disorders. This result might suggest comorbidity as a confounder for the association between early motor development and later ADHD. But, it has to be taken into account that the study only identified four children with ADHD and comorbidity, and the result must therefore be taken with reservation. In addition, Gurevitz et al. (2014) found that significantly more children at 3 months showed deviations in tonus, which also might be interpreted as a comorbidity.
An ongoing discussion about ADHD subtypes and whether they represent one or three different diseases is taking place (Biederman and Faraone 2005; Vasserman et al. 2014). As the only study, Gurevitz et al. took this subdivision into account, but with no influence on the results. Future studies investigating the motor development with focus on the subtypes could bring important knowledge about the influence of the subtypes to the field. Likewise, no studies have investigated the impact of gender on the early motor development. This could also be of great interest in future studies.
A substantial methodological heterogeneity was found between the studies. The studies by Gurevitz and Hadders-Algra included small populations, which might influence the outcome and result in low statistical power. In contrast, the studies by Lemcke and Jaspers included large numbers of cases, which provides the studies with a high statistical power (Table 1). Population-based, the average age of an ADHD diagnosis is around 8–10 years (Atladottir et al. 2015). It can be discussed if an age at follow-up of 7–9 years, as in the studies by Gurevitz et al. and Jeyaseelan et al. provides sufficient follow-up time to identify children with ADHD diagnosis. The somewhat low age of follow-up can have influenced the results of the studies in different ways. If children diagnosed with ADHD at an older age also are the children without motor delays, an overestimation of the connection can be reported. Or if particular children, e.g. with comorbidity are diagnosed early, a considerable number of this group of children will be included as cases in the studies. This will bias the results towards an association between developmental deviations and ADHD with comorbidity. The rest of the studies identified in the report used a longer follow-up time, and the risk of that the above-mentioned bias should interfere the results are low (Hadders-Algra et al. 2009a, b; Jaspers et al. 2013; Lemcke et al. 2016).
In the studies by Gurevitz et al. and Hadders-Algra et al., assessors of motor development were unaware of the children’s ADHD scores or diagnosis. In the prospective studies, the study design makes the assessors of the early motor development unaware of later psychiatric diagnoses among the children, thus avoiding influences on the evaluation of the motor skills and increasing the generalisation of the results. The study by Lemcke et al. incorporates interviews were the questions were not specifically designed for assessment of the association between motor development and ADHD. The reliability of the findings from that study can be debated.
Two diagnostic systems, IDC-10 and DSM-IV, are used worldwide to diagnose ADHD. The IDC-10 system uses the term Hyperkinetic Disorder (HKD), while the term ADHD derives from the DMS-IV system. HKD is more narrowly defined than ADHD, and it has been shown that children diagnosed with HKD also meet the criteria for ADHD, however not vice versa (Lahey et al. 2006). Two studies (Gurevitz et al. 2014; Lemcke et al. 2016) included children with clinical diagnosis but based on separate diagnostic systems, where the remaining studies (Hadders-Algra et al. 2009a, b; Jaspers et al. 2013; Jeyaseelan et al. 2006) used information from validated questionnaires completed by parents to diagnose children with ADHD. This difference might have an impact on the classification of the diagnosed children found in this review and influence the comparability across the studies.
A number of papers were excluded, despite their use of CBCL as a standardised assessment tool as the inclusion criteria (Butcher et al. 2009; Hitzert et al. 2014). These studies did not evaluate ADHD as a disorder consisting of more components (inattention, hyperactivity, behaviour), but instead as a disorder of either attention or behaviour. The results of the full CBCL assessment would have been of major interest for this review. The activity level of infants as a predictor for later ADHD has previously been studied but was not included in this review (Johnson et al. 2015). A distinct definition of motor development excluding activity level was made, though it can be problematic to distinguish whether motor activities have an influence on motor development.
Some further limitations deserve consideration in the interpretation of the findings. The exclusion of other databases may have left out relevant studies. Moreover, applicable studies may have been missed by the exclusion of papers in other than English or Scandinavian languages. Furthermore, only one author conducted the literature search, including the first screening of the papers, which may have reduced the reliability and validity of the first step of the selection process.
In conclusion, a very limited number of studies have been performed to evaluate early motor development in children with later ADHD. The findings are pointing in various directions and due to methodological heterogeneity and other limitations, no firm conclusion regarding the correlation can be drawn. Before motor development as an early indicator of ADHD can be implemented in the clinical work, more knowledge is required. Ideally, prospective studies, including large study populations with clinically diagnosed children, should be performed with the emphasis on subtypes of ADHD, gender and comorbidity.
References
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington
Atladottir HO, Gyllenberg D, Langridge A, Sandin S, Hansen SN, Leonard H et al (2015) The increasing prevalence of reported diagnoses of childhood psychiatric disorders: a descriptive multinational comparison. Eur Child Adolesc Psychiatry 24(2):173–183. https://doi.org/10.1007/s00787-014-0553-8
Biederman J, Faraone SV (2005) Attention-deficit hyperactivity disorder. Lancet 366(9481):237–248. https://doi.org/10.1016/s0140-6736(05)66915-2
Butcher PR, van Braeckel K, Bouma A, Einspieler C, Stremmelaar EF, Bos AF (2009) The quality of preterm infants spontaneous movements: an early indicator of intelligence and behaviour at school age. J Child Psychol Psychiatry 50(8):920–930. https://doi.org/10.1111/j.1469-7610.2009.02066.x
Charach A, Carson P, Fox S, Ali MU, Beckett J, Lim CG (2013) Interventions for preschool children at high risk for ADHD: a comparative effectiveness review. Pediatrics 131(5):e1584–e1604. https://doi.org/10.1542/peds.2012-0974
Einspieler C, Prechtl HF (2005) Prechtl’s assessment of general movements: a diagnostic tool for the functional assessment of the young nervous system. Ment Retard Dev Disabil Res Rev 11(1):61–67. https://doi.org/10.1002/mrdd.20051
Fliers E, Rommelse N, Vermeulen SH, Altink M, Buschgens CJ, Faraone SV, Buitelaar JK (2008) Motor coordination problems in children and adolescents with ADHD rated by parents and teachers: effects of age and gender. J Neural Transm (Vienna) 115(2):211–220. https://doi.org/10.1007/s00702-007-0827-0
Gurevitz M, Geva R, Varon M, Leitner Y (2014) Early markers in infants and toddlers for development of ADHD. J Atten Disord 18(1):14–22. https://doi.org/10.1177/1087054712447858
Hadders-Algra M, Groothuis AMC (1999) Quality of general movements in infancy is related to neurological dysfunction, ADHD, and aggressive behaviour. Dev Med Child Neurol 41(6):381–391. https://doi.org/10.1017/S0012162299000845
Hadders-Algra M, Bouwstra H, Groen SE (2009a) Quality of general movements and psychiatric morbidity at 9 to 12 years. Early Hum Dev 85(1):1–6. https://doi.org/10.1016/j.earlhumdev.2008.05.005
Hadders-Algra M, Bouwstra H, Groen SE (2009b) Quality of general movements and psychiatric morbidity at 9 to 12 years. Early Human Dev 85(1):1–6. https://doi.org/10.1016/j.earlhumdev.2008.05.005
Hitzert MM, Roze E, Van Braeckel KN, Bos AF (2014) Motor development in 3-month-old healthy term-born infants is associated with cognitive and behavioural outcomes at early school age. Dev Med Child Neurol 56(9):869–876. https://doi.org/10.1111/dmcn.12468
Jaspers M, de Winter AF, Buitelaar JK, Verhulst FC, Reijneveld SA, Hartman CA (2013) Early childhood assessments of community pediatric professionals predict autism spectrum and attention deficit hyperactivity problems. J Abnorm Child Psychol 41(1):71–80. https://doi.org/10.1007/s10802-012-9653-4
Jensen CM, Steinhausen HC (2015) Comorbid mental disorders in children and adolescents with attention-deficit/hyperactivity disorder in a large nationwide study. Atten Defic Hyperact Disord 7(1):27–38. https://doi.org/10.1007/s12402-014-0142-1
Jeyaseelan D, O’Callaghan M, Neulinger K, Shum D, Burns Y (2006) The association between early minor motor difficulties in extreme low birth weight infants and school age attentional difficulties. Early Human Dev 82(4):249–255. https://doi.org/10.1016/j.earlhumdev.2005.10.012
Johnson MH, Gliga T, Jones E, Charman T (2015) Annual research review: infant development, autism, and ADHD—early pathways to emerging disorders. J Child Psychol Psychiatry 56(3):228–247. https://doi.org/10.1111/jcpp.12328
Kadesjo B, Gillberg C (2001) The comorbidity of ADHD in the general population of Swedish school-age children. J Child Psychol Psychiatry 42(4):487–492
Kaiser ML, Schoemaker MM, Albaret JM, Geuze RH (2014) What is the evidence of impaired motor skills and motor control among children with attention deficit hyperactivity disorder (ADHD)? Systematic review of the literature. Res Dev Disabil 36C:338–357. https://doi.org/10.1016/j.ridd.2014.09.023
Lahey BB, Pelham WE, Chronis A, Massetti G, Kipp H, Ehrhardt A, Lee SS (2006) Predictive validity of ICD-10 hyperkinetic disorder relative to DSM-IV attention-deficit/hyperactivity disorder among younger children. J Child Psychol Psychiatry 47(5):472–479. https://doi.org/10.1111/j.1469-7610.2005.01590.x
Lemcke S, Parner ET, Bjerrum M, Thomsen PH, Lauritsen MB (2016) Early development in children that are later diagnosed with disorders of attention and activity: a longitudinal study in the Danish National Birth Cohort. Eur Child Adolesc Psychiatry 25(10):1055–1066. https://doi.org/10.1007/s00787-016-0825-6
McIntosh N, Helms P, Smyth R, Logan S (2008) Forfar and Arneil’s textbook of pediatrics, 7th edn. Churchill Livingstone Elsevier
Rappley MD (2005) Attention deficit-hyperactivity disorder. N Engl J Med 352(2):165–173. https://doi.org/10.1056/NEJMcp032387
Vasserman M, Bender HA, Macallister WS (2014) Motor skills development in children with inattentive versus combined subtypes of ADHD. Appl Neuropsychol Child 3(2):145–151. https://doi.org/10.1080/21622965.2012.759466
World HO (1993) The ICD-10 classification of mental and behavioural disorders. Diagnostic criteria for research. World Health Organisation, Geneva
Acknowledgements
The project was funded by a Grant from The Central Denmark Region, Psychiatry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Per Hove Thomsen has received speaker’s honoraria from Shire, Novartis, and HB-Pharma within the last 3 years. He is not a member of any advisory boards nor does he hold any stocks. The other authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Havmoeller, S.R., Thomsen, P.H. & Lemcke, S. The early motor development in children diagnosed with ADHD: a systematic review. ADHD Atten Def Hyp Disord 11, 233–240 (2019). https://doi.org/10.1007/s12402-018-0280-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-018-0280-y