Abstract
Background
To assess the functional relevance of a coronary artery stenosis, corrected coronary opacification (CCO) decrease derived from coronary computed tomography angiography (CCTA) has been proposed. The present study aims at validating CCO decrease with quantitative 13N-ammonia positron emission tomography (PET) myocardial perfusion imaging (MPI).
Methods and Results
This retrospective study consists of 39 patients who underwent hybrid CCTA/PET-MPI. From CCTA, attenuation in the coronary lumen was measured before and after a stenosis and corrected to the aorta to calculate CCO and its decrease. Relative flow reserve (RFR) was calculated by dividing the stress myocardial blood flow (MBF) of a vessel territory subtended by a stenotic coronary by the stress MBF of the reference territories without stenoses. RFR was abnormal in 11 vessel territories (27%). CCO decrease yielded a sensitivity, specificity, negative predictive value, positive predictive value, and accuracy for prediction of an abnormal RFR of 73%, 70%, 88%, 47%, and 70%, respectively.
Conclusions
CCTA-derived CCO decrease has moderate diagnostic accuracy to predict an abnormal RFR in PET-MPI. However, its high negative predictive value to rule out functional relevance of a given lesion may confer clinical implications in the diagnostic work-up of patients with a coronary stenosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Low-dose coronary computed tomography angiography (CCTA) is a valuable non-invasive tool to assess coronary artery disease (CAD) with high negative predictive value1 and to guide subsequent treatment strategies.2,3 A limitation of CCTA is its moderate performance in assessing the functional relevance of a coronary stenosis as is inherently true for any anatomic test.4 However, proof of functional relevance of a stenosis prior to any revascularization procedure is mandatory to improve outcome.5,6,–7 Consequently, combining anatomic information on the coronary arteries derived from CCTA with functional information from single photon emission computed tomography (SPECT) or positron emission tomography (PET) myocardial perfusion imaging (MPI) either side-by-side or fused as hybrid imaging was established and has been shown to offer added clinical and prognostic value.8,9,–10 Concurrently, there is growing interest in parameters derived directly from CCTA to assess the functional relevance of a coronary lesion. Fractional flow reserve from CCTA (FFRCT) has been introduced recently and several prospective trials have lent support to suggest a clinical role.11,12 Calculation of FFRCT, however, currently remains a complex and cumbersome process with limited availability, but easily and quickly derivable parameters such as the transluminal attenuation gradient (TAG)13,14 and the decrease in corrected coronary opacification (CCO)15,16,–17 have emerged as promising alternatives. While TAG may be more related to vessel diameter than to stenosis severity,18 CCO decrease has consistently yielded high diagnostic accuracy (79 to 89%) to predict functional relevance of a coronary stenosis.15,16,–17 It has, nevertheless, not yet been investigated in comparison to quantitative PET-MPI which is considered the gold standard for myocardial perfusion assessment.19,20,–21 Moreover, the calculation of relative flow reserve (RFR) from PET-MPI has not only served as the standard of reference for the validation of invasive FFR,22 but has also been shown in some patient populations to yield significantly higher diagnostic accuracy than stress myocardial blood flow (MBF) or coronary flow reserve (CFR).23 The aim of the present study was to validate CCO decrease with stress MBF in PET-MPI and to assess the accuracy of CCO decrease to predict an abnormal RFR as derived from the gold standard PET-MPI.
Methods
Study Population
We retrospectively identified 67 patients who underwent hybrid CCTA/PET-MPI at our institution due to known or suspected CAD. Exclusion criteria were history of coronary artery bypass surgery and patients who suffered any events between the CCTA and the PET scan. The study protocol was approved by the institutional review board (cantonal ethics committee, BASEC-Nr. 2016-00177) and informed consent was waived for all patients scanned before 2014. For all patients scanned afterwards, written informed consent was obtained. No funding was obtained for performing this study.
CCTA Acquisition and Assessment of CCO Decrease
Patients underwent contrast-enhanced CCTA on either a 64-slice scanner (n = 39; LightSpeed VCT or Discovery HD 750, both GE Healthcare, Waukesha, WI, USA) or a 256-slice scanner (n = 28; Revolution CT, GE Healthcare) using helical (n = 4) or axial scanning with prospective ECG-triggering (n = 63) as previously described.24,25 Bolus tracking was performed and image acquisition was started 4 seconds after the signal density reached a predefined (i.e. 120 Hounsfield units) or a visually detectable threshold in the ascending aorta. In order to achieve a target heart rate <65 bpm, intravenous metoprolol (5-30 mg) was administered prior to scanning if necessary. Furthermore, all patients received 2.5 mg sublingual isosorbide dinitrate 2 minutes prior to the scan.
CCO decrease was measured for each coronary stenosis (i.e. luminal diameter narrowing ≥50%) as previously described.15 In brief, a region of interest (ROI) with a diameter of 1 mm was placed in the center of the coronary lumen and a ROI with a diameter of 10 mm was placed in the descending aorta on the same axial slice. CCO was calculated as the ratio of mean attenuation in the coronary ROI over the aortic ROI. CCO was measured twice as close as possible to the stenosis and due care was taken to avoid calcifications and streak artifacts in the measurements and the lower values were used to calculate CCO decrease as the difference of proximal minus distal value.
PET Acquisition and RFR Calculation
Patients underwent 13N-ammonia PET at rest and during adenosine stress at a standard rate (0.14 mg/min/kg) over 7 minutes with 700-900 MBq of 13N-ammonia administered intravenously into a peripheral vein after 3 minutes into stress. Images were acquired either on a Discovery (LS/RX) PET/CT scanner or on an Advance PET scanner (both GE Healthcare), as previously reported in detail.19
Quantitative MBF and CFR were calculated using the commercially available PMOD software (version 3.7; PMOD Technologies Ltd., Zurich, Switzerland) developed and validated at our institution.26 In brief, a volume of interest (VOI) encompassing the left ventricular myocardium was drawn and two more VOIs were put into the blood pool of the left and right ventricle. Myocardial and blood-pool time-activity curves (TAC) were obtained from dynamic frames corrected for radioisotope decay. Stress and rest MBF was estimated by model fitting of the blood pool and myocardial TACs corrected for spill-over and partial volume.19 CFR was calculated as the ratio of stress MBF over rest MBF.
Considering that standard vascular territory distribution in myocardial perfusion interpretation may be subject to a substantial morphologic variability of the coronary tree,27 quantitative PET datasets (using a 17-segment model) were fused with CCTA using a commercially available software (CardIQ Fusion, GE Healthcare) in order to assure true co-registration. For each coronary artery, mean MBF of the two myocardial PET segments subtended by the most distal vessel section was recorded and allocated to this coronary artery.10 Subsequently, in a subgroup of patients with 1- or 2-vessel-disease, relative flow reserve (RFR) was calculated by dividing the MBF of a coronary artery with a stenosis by the mean MBF in the reference vessel(s) without a coronary stenosis. An RFR below 0.69 was considered abnormal.28
Statistical Analysis
Continuous variables were expressed as mean ± standard deviation (SD) or as median with interquartile range (IQR) if data was not normally distributed, and categorical variables as percentages. Kolmogorov–Smirnov test was applied to assess normal distribution. Comparison of continuous variables with non-normal distributions between groups was performed with Mann–Whitney U and Kruskal–Wallis test. Spearman’s correlation was used to measure the association between CCO decrease and stress MBF. Receiver-operating characteristics (ROC) curve analysis was plotted to illustrate the performance of CCO decrease to diagnose an abnormal RFR. Youden’s index was calculated to define the optimal threshold. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of CCO decrease were calculated on a per-vessel basis, whereby an abnormal RFR served as the standard of reference for hemodynamic relevance. A P value <.05 was considered statistically significant. SPSS version 20.0 (IBM Corporation, Armonk, NY, USA) was used for analysis.
Results
Study Population
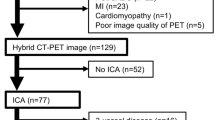
The baseline characteristics of the study population (n = 67) are summarized in Table 1. Twenty-seven patients (40%) were referred for exclusion of CAD and 40 (60%) for evaluation of known CAD. Twenty-one patients (53%) had a stent and 16 (40%) a history of prior myocardial infarction. Figure 1 depicts screening, inclusion, and eligibility for analysis of the study population in a flow chart.
CCTA Findings
CCTA ruled out CAD in 26 patients (39%). In 41 patients (61%), 99 stenoses were documented in a total of 73 vessels resulting in 18 patients with one-vessel, 14 patients with two-vessel, and 9 patients with three-vessel-disease. CCO decrease was successfully measured across each stenosis and varied significantly by stenosis severity (P < .001) as illustrated in Figure 2.
Box-and-whisker plot showing corrected coronary opacification (CCO) decrease of all lesions for subsets of anatomic stenosis severity (50% to 69%, 70% to 89%, 90% to 99%, and 100% diameter narrowing). The red horizontal line corresponds to the cut-off value for an abnormal CCO decrease as defined in the present study (CCO decrease >0.166). The boxes represent the interquartile range (IQR) and the dark line within each box indicates the median. The whiskers are defined as 1.5 times the IQR
PET Findings
Rest and stress MBF as well as CFR differed significantly across different stenosis severities (P < .05; Table 2). Among the vessels with a coronary stenosis, median stress MBF was 1.41 mL/min/g (IQR, 0.87 to 1.75 mL/min/g). In the subgroup of patients with 1- or 2-vessel-disease, RFR was calculated in 41 vessels with a coronary stenosis and resulted in a median of 0.84 (IQR, 0.66 to 1.13). RFR was abnormal in 11 patients (27%).
Diagnostic Accuracy of CCO Decrease
Stress MBF correlated significantly with CCO decrease (r = −0.480; P < .001; Figure 3).
The ROC curve analysis for CCO decrease to diagnose an abnormal RFR resulted in an AUC of 0.712 (P < .05; Figure 4). Youden’s index was calculated and identified the optimal cut-off of CCO decrease at 0.166. Implementing the latter, median RFR was significantly lower in vessels with an abnormal CCO decrease compared to vessels with a normal CCO decrease (0.69 vs. 1.02; P < .05; Figure 5). An abnormal CCO decrease correctly detected an abnormal RFR in 8 of 11 vessels and correctly ruled out an abnormal RFR in 21 of 30 vessels. This resulted in a sensitivity, specificity, negative predictive value, positive predictive value, and accuracy of 73% (95% CI: 39% to 94%), 70% (95% CI: 51% to 85%), 88% (95% CI: 68% to 97%), and 47% (95% CI: 23% to 72%) and 70%, respectively (Table 3).
Box-and-whisker plot showing relative flow reserve (RFR) in vessels with either a normal or an abnormal CCO decrease. The red horizontal line corresponds to the cut-off value for an abnormal RFR as previously defined (RFR < 0.69).28
Implementing a threshold of 0.166 for an abnormal CCO decrease, stress MBF was significantly lower in vessels with an abnormal CCO decrease compared to vessels with a normal CCO decrease (1.04 mL/min/g vs. 1.70 mL/min/g; P < .001).
Discussion
The present study is the first to compare CCO decrease with stress MBF and to report on its ability to predict abnormal RFR in vessels with a coronary stenosis. Our results demonstrate that CCO decrease correlates with stress MBF and that the presence of an abnormal CCO decrease is associated with significantly lower RFR. Although the assessment of functional relevance of coronary stenoses by CCTA-derived CCO decrease has only moderate diagnostic accuracy, it excludes an abnormal RFR with high negative predictive value. Thus, assessment of CCO decrease from CCTA may confer clinical implications in the diagnostic work-up of patients with a coronary stenosis. While some studies have previously reported high diagnostic accuracy of CCO decrease in comparison to TIMI flow, magnetic resonance MPI, or invasive FFR,15,16,–17 it has not yet been compared to PET-MPI, the current gold standard for quantitative MBF assessment. Compared to previous reports,15,16,–17 the lower diagnostic accuracy in the present study is most likely linked to the different standard of reference since the number of patients as well as the disease prevalence was comparable. Nonetheless, the results are consistent with these reports with regard to the high negative predictive value of CCO decrease.
It is well known that morphological stenosis severity poorly predicts functional relevance4 although assessment of functional relevance is the key to appropriate clinical decision-making. In fact, deferral from revascularization in case of functionally relevant stenoses29 as well as revascularization of non-relevant stenoses5,30 both have been associated with less favorable outcomes in randomized trials. Consequently, current guidelines mandate complementing pure anatomical characterization of a coronary stenosis with functional assessment for evidence-based target lesion revascularization. Despite increasing evidence and the current guidelines, both non-invasive stress testing before invasive coronary angiography (ICA) and FFR before percutaneous coronary intervention (PCI) are underused in daily practice.31,32 Furthermore, although it has been demonstrated that multimodality imaging successfully identifies patients at increased risk for adverse cardiovascular outcome and substantially reduces downstream resource utilization,9,33,34,35,–36 SPECT/CCTA and PET/CCTA are not yet widely adopted in clinical routine. The clinical implications of the present study lie in the ease of use of CCO decrease at no additional costs. The potential application of CCO decrease to predict abnormal RFR and thus offering functional assessment of a coronary stenosis may pave the way to individualize clinical workflow. Due to its moderate diagnostic accuracy CCO decrease may not replace MPI. However, thanks to the high negative predictive value to exclude functional relevance in intermediate stenoses, CCO decrease could potentially be endorsed as a gatekeeper after CCTA for additional non-invasive diagnostic work-up. If CCO decrease is normal, patients might be safely deferred from further testing such as MPI. On the contrary, if CCO decrease is abnormal, further non-invasive testing with SPECT or PET-MPI should be added and patient with ischemic burden above 10% of the left ventricle myocardium should be considered for revascularization.7 Through this approach, downstream resource utilization may be influenced in a cost-effective manner and the probability for a comprehensive anatomic and functional non-invasive assessment before the patient is referred to invasive coronary angiography is increased.
We acknowledge the following limitations. First, our study design was retrospective and the patient population was rather small. Future studies should prospectively assess the role of CCO decrease in the clinical workflow. Second, MBF can be impaired in a variety of cardiovascular diseases and reduced stress MBF values by PET-MPI cannot discriminate between epicardial coronary obstruction or microcirculatory dysfunction. While a pathologic RFR may suggest epicardial CAD23,28 a normal RFR in combination with a homogenous stress MBF reduction may result from either balanced ischemia due to epicardial multi-vessel CAD or microvascular disease. If the latter also interacts with CCO decrease values remains to be determined. However, since the CCO measurements are performed at low flow conditions and therefore do not depend on the vasodilatory capacity of the microvascular tree, this seems less likely. Third, although previous studies have demonstrated that intraluminal attenuation decreases with diminution of vessel diameter,18 CCO decrease is not commonly corrected for vessel diameter. However, since CCO decrease is measured within 2 cm proximal and distal of a stenosis, a relevant impact of vessel diameter seems rather unlikely. Finally, due to the relative small sample size and due to the single-center retrospective nature of this study, any extrapolation of the CCO cut-off point to distinguish between stenoses with and without hemodynamic significance to any patient population substantially differing from the one studied here should be made only with caution.
In conclusion, CCTA-derived CCO decrease has moderate diagnostic accuracy to predict an abnormal RFR in PET-MPI. However, its high negative predictive value to rule out functional relevance of a given lesion may confer clinical implications in the diagnostic work-up of patients with a coronary stenosis.
New Knowledge Gained
Due to the moderate diagnostic accuracy of CCO decrease, the use of more advanced imaging techniques to assess myocardial perfusion is indispensable. However, thanks to the high negative predictive value of CCO decrease it may be endorsed as a gatekeeper for implementation of a patient-tailored non-invasive further diagnostic work-up.
Abbreviations
- CCO:
-
Corrected coronary opacification
- CCTA:
-
Coronary computed tomography angiography
- SPECT:
-
Single photon emission computed tomography
- PET:
-
Positron emission tomography
- RFR:
-
Relative flow reserve
- MBF:
-
Myocardial blood flow
- CFR:
-
Coronary flow reserve
- TAC:
-
Time-activity curves
- ICA:
-
Invasive coronary angiography
- PCI:
-
Percutaneous coronary intervention
References
Herzog BA, Husmann L, Burkhard N, Gaemperli O, Valenta I, Tatsugami F, et al. Accuracy of low-dose computed tomography coronary angiography using prospective electrocardiogram-triggering: First clinical experience. Eur Heart J. 2008;29:3037-42.
Investigators S-H. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): An open-label, parallel-group, multicentre trial. Lancet. 2015;385:2383-91.
Douglas PS, Hoffmann U, Patel MR, Mark DB, Al-Khalidi HR, Cavanaugh B, et al. Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med. 2015;372:1291-300.
Tonino PA, Fearon WF, De Bruyne B, Oldroyd KG, Leesar MA, Ver Lee PN, et al. Angiographic versus functional severity of coronary artery stenoses in the FAME study fractional flow reserve versus angiography in multivessel evaluation. J Am Coll Cardiol. 2010;55:2816-21.
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’t Veer M, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-24.
Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: Results from the clinical outcomes utilizing revascularization and aggressive drug evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283-91.
Windecker S, Kolh P, Alfonso F, Collet JP, Cremer J, Falk V, et al. ESC/EACTS guidelines on myocardial revascularization: The task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35:2541-619.
Gaemperli O, Schepis T, Valenta I, Husmann L, Scheffel H, Duerst V, et al. Cardiac image fusion from stand-alone SPECT and CT: Clinical experience. J Nucl Med. 2007;48:696-703.
Pazhenkottil AP, Nkoulou RN, Ghadri JR, Herzog BA, Buechel RR, Kuest SM, et al. Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J. 2011;32:1465-71.
Danad I, Raijmakers PG, Appelman YE, Harms HJ, de Haan S, van den Oever ML, et al. Hybrid imaging using quantitative H215O PET and CT-based coronary angiography for the detection of coronary artery disease. J Nucl Med. 2013;54:55-63.
Norgaard BL, Leipsic J, Gaur S, Seneviratne S, Ko BS, Ito H, et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (analysis of coronary blood flow using CT angiography: Next steps). J Am Coll Cardiol. 2014;63:1145-55.
Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: The prospective longitudinal trial of FFRCT: Outcome and resource impacts study. Eur Heart J. 2015;36:3359-67.
Steigner ML, Mitsouras D, Whitmore AG, Otero HJ, Wang C, Buckley O, et al. Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging. 2010;3:179-86.
Choi JH, Min JK, Labounty TM, Lin FY, Mendoza DD, Shin DH, et al. Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging. 2011;4:1149-57.
Chow BJ, Kass M, Gagne O, Chen L, Yam Y, Dick A, et al. Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol. 2011;57:1280-8.
den Dekker MA, Pelgrim GJ, Pundziute G, van den Heuvel ER, Oudkerk M, Vliegenthart R. Hemodynamic significance of coronary stenosis by vessel attenuation measurement on CT compared with adenosine perfusion MRI. Eur J Radiol. 2015;84:92-9.
Wang R, Renker M, Schoepf UJ, Wichmann JL, Fuller SR, Rier JD, et al. Diagnostic value of quantitative stenosis predictors with coronary CT angiography compared to invasive fractional flow reserve. Eur J Radiol. 2015;84:1509-15.
Park EA, Lee W, Park SJ, Kim YK, Hwang HY. Influence of coronary artery diameter on intracoronary transluminal attenuation gradient during CT angiography. JACC Cardiovasc Imaging. 2016;9:1074-83.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150-6.
Fiechter M, Ghadri JR, Gebhard C, Fuchs TA, Pazhenkottil AP, Nkoulou RN, et al. Diagnostic value of 13N-ammonia myocardial perfusion PET: Added value of myocardial flow reserve. J Nucl Med. 2012;53:1230-4.
Gould KL, Johnson NP, Bateman TM, Beanlands RS, Bengel FM, Bober R, et al. Anatomic versus physiologic assessment of coronary artery disease. Role of coronary flow reserve, fractional flow reserve, and positron emission tomography imaging in revascularization decision-making. J Am Coll Cardiol. 2013;62:1639-53.
De Bruyne B, Baudhuin T, Melin JA, Pijls NH, Sys SU, Bol A, et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation. 1994;89:1013-22.
Lee JM, Kim CH, Koo BK, Hwang D, Park J, Zhang J, et al. Integrated myocardial perfusion imaging diagnostics improve detection of functionally significant coronary artery stenosis by 13N-ammonia positron emission tomography. Circ Cardiovasc Imaging. 2016;9:e004768.
Benz DC, Grani C, Hirt Moch B, Mikulicic F, Vontobel J, Fuchs TA, et al. Minimized radiation and contrast agent exposure for coronary computed tomography angiography: First clinical experience on a latest generation 256-slice scanner. Acad Radiol. 2016;23:1008-14.
Husmann L, Valenta I, Gaemperli O, Adda O, Treyer V, Wyss CA, et al. Feasibility of low-dose coronary CT angiography: First experience with prospective ECG-gating. Eur Heart J. 2008;29:191-7.
Siegrist PT, Gaemperli O, Koepfli P, Schepis T, Namdar M, Valenta I, et al. Repeatability of cold pressor test-induced flow increase assessed with H(2)(15)O and PET. J Nucl Med. 2006;47:1420-6.
Liga R, Vontobel J, Rovai D, Marinelli M, Caselli C, Pietila M, et al. Multicentre multi-device hybrid imaging study of coronary artery disease: Results from the evaluation of integrated cardiac imaging for the detection and characterization of ischaemic heart disease (EVINCI) hybrid imaging population. Eur Heart J Cardiovasc Imaging. 2016;17:951-60.
Stuijfzand WJ, Uusitalo V, Kero T, Danad I, Rijnierse MT, Saraste A, et al. Relative flow reserve derived from quantitative perfusion imaging may not outperform stress myocardial blood flow for identification of hemodynamically significant coronary artery disease. Circ Cardiovasc Imaging. 2015;8:e002400.
De Bruyne B, Fearon WF, Pijls NH, Barbato E, Tonino P, Piroth Z, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208-17.
Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-Year follow-up of the FAME (fractional flow reserve versus angiography for multivessel evaluation) study. J Am Coll Cardiol. 2010;56:177-84.
Buechel RR, Kaufmann BA, Tobler D, Wild D, Zellweger MJ. Non-invasive nuclear myocardial perfusion imaging improves the diagnostic yield of invasive coronary angiography. Eur Heart J Cardiovasc Imaging. 2015;16:842-7.
Härle T, Zeymer U, Hochadel M, Zahn R, Kerber S, Zrenner B, et al. Real-world use of fractional flow reserve in Germany: Results of the prospective ALKK coronary angiography and PCI registry. Clin Res Cardiol. 2016;106:140-50.
Fiechter M, Ghadri JR, Wolfrum M, Kuest SM, Pazhenkottil AP, Nkoulou RN, et al. Downstream resource utilization following hybrid cardiac imaging with an integrated cadmium-zinc-telluride/64-slice CT device. Eur J Nucl Med Mol Imaging. 2012;39:430-6.
Benz DC, Templin C, Kaufmann PA, Buechel RR. Ultra-low-dose hybrid single photon emission computed tomography and coronary computed tomography angiography: A comprehensive and non-invasive diagnostic workup of suspected coronary artery disease. Eur Heart J. 2015;36:3345.
Pazhenkottil AP, Herzog BA, Husmann L, Buechel RR, Burger IA, Valenta I, et al. Non-invasive assessment of coronary artery disease with CT coronary angiography and SPECT: A novel dose-saving fast-track algorithm. Eur J Nucl Med Mol Imaging. 2010;37:522-7.
Kajander SA, Joutsiniemi E, Saraste M, Pietila M, Ukkonen H, Saraste A, et al. Clinical value of absolute quantification of myocardial perfusion with (15)O-water in coronary artery disease. Circ Cardiovasc Imaging. 2011;4:678-84.
Acknowledgments
We thank Verena Weichselbaumer, Martina Vogt, Tania Lagrange, Lasien Vojo, and Kevin Frei for their excellent technical support.
Disclosure
The authors do not have any personal conflicts of interest to declare. However, the University Hospital Zurich holds a research agreement with GE Healthcare.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Dominik C. Benz and Christoph Gräni share first authorship; Philipp A. Kaufmann and Ronny R. Buechel share last authorship
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Benz, D.C., Gräni, C., Ferro, P. et al. Corrected coronary opacification decrease from coronary computed tomography angiography: Validation with quantitative 13N-ammonia positron emission tomography. J. Nucl. Cardiol. 26, 561–568 (2019). https://doi.org/10.1007/s12350-017-0980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-017-0980-2