Abstract
A 32-year-old Japanese woman was admitted to our hospital for the diagnosis and treatment of multiple liver tumors. She had been receiving 125 mg testosterone enanthate every 2 weeks following female-to-male gender identity disorder (GID) diagnosis at 20 years of age. Ultrasonography, computed tomography, and magnetic resonance imaging showed 11 hepatic nodular tumors with a maximum diameter of 28 mm. Liver tumors with hepatocellular adenoma (HCA) were diagnosed with needle biopsy. Segmentectomy of the left lateral lobe including two lesions, subsegmentectomy of S6 including two lesions, enucleation of each tumor in S5 and S7, and open surgical radiofrequency ablation for each tumor in S4 and S7 were performed. Immunohistochemical specimens showed that the tumor cells were diffusely and strongly positive for glutamine synthetase and that the nuclei were ectopically positive for β-catenin. Thus, the tumors were diagnosed as β-catenin-activated HCA (b-HCA). Transcatheter arterial chemoembolization plus subsequent radiofrequency ablation was performed for the 3 residual lesions in S4 and S8. Although testosterone enanthate was being continued for GID, no recurrence was observed until at least 22 months after the intensive treatments. HCA development in such patients receiving testosterone should be closely monitored using image inspection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular adenoma (HCA) is a rare hepatic tumor. In the United States, it is present in 3–4 out of every 100,000 people, and most of whom are young women using oral contraceptives [1]. In Japan, the HCA incidence appears to be lower than that in Europe and the United States. Women account for 53.8% of all Japanese patients and > 90% of Euro-American patients, indicating no sex difference in the HCA incidence in Japan [2]. In addition to contraceptive agents, glycogen storage disease types I and III as well as anabolic androgenic steroid therapy for Fanconi anemia are identified risk factors for HCA development [3, 4]. Some studies have also reported HCA development due to the administration of testosterone, an anabolic androgenic steroid, in transsexual men [5, 6].
Recently, HCA classification was originally proposed by multiple French groups using molecular and immunohistological techniques and was categorized into the following four subtypes; hepatocyte nuclear factor 1α inactivated HCA (H-HCA), inflammatory HCA (I-HCA), β-catenin-activated HCA (b-HCA), and unclassified HCA (u-HCA) [7,8,9]. These subtypes were specified in the 2010 WHO classification [10]. Currently, this classification is widely used, because routine immunohistochemistry facilitates the classification of HCA: H-HCA is diagnosed by a lack of immunoreactivity for liver fatty acid-binding protein (L-FABP), I-HCA by positive immunoreactivity for serum amyloid A (SAA) and C-reactive protein (CRP), and b-HCA by positive immunoreactivity for glutamine synthetase (GS) and nuclear β-catenin [7, 8, 11].
To the best of our knowledge, there are no case reports of HCA that developed due to testosterone treatment for gender identity disorder (GID) and subtyped according to the classification described above. Here, we report the first case of a woman in whom multiple HCA developed during the use of testosterone for female-to-male (FtM) GID, where the HCA subtype was determined using immunohistochemical findings.
Case report
A 32-year-old Japanese woman was admitted to our hospital for the diagnosis and treatment of multiple liver tumors. She had been regularly taking 125 mg testosterone enanthate once every 2 weeks, since she was diagnosed with FtM GID at 20 years of age. Nine months before she was admitted to our hospital, she had visited a nearby hospital because of epigastric pain. She had multiple liver tumors that were detected on abdominal ultrasonography (US); however, these were not evaluated further. Thereafter, she became worried about the liver tumors and visited a hepatologist in our hospital.
She had been smoking 10 cigarettes daily since the age of 13 years; however, she did not consume alcohol before that. She had a past history of epilepsy, renal infarction, and hypertension; however, she had never taken an oral contraceptive. She was tattooed and had postoperative scars owing to bilateral mastectomy on her chest. She had never received any blood products.
On admission, her body mass index was 30.2 kg/m2. The liver tumors were not palpable in the abdomen. Laboratory tests showed liver dysfunction and dyslipidemia. She tested negative for hepatitis B surface antigen and hepatitis C virus antibody. Liver dysfunction was believed to be caused by nonalcoholic fatty liver disease, because she was obese with dyslipidemia and high liver echogenicity. Serum alpha-fetoprotein levels were normal, whereas serum des-gamma-carboxy prothrombin (DCP) levels were high (935 mAu/ml; normal range < 40 mAu/ml). Indocyanine green retention rate at 15 min was 11.0% (normal range < 10%). The serum testosterone level was considerably high at 22.9 ng/ml (normal range 0.11–0.47 ng/ml) (Table 1).
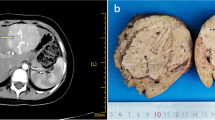
US examination revealed multiple hyperechoic and hypoechoic nodules in both the lobes of the liver (Fig. 1). The total number of nodules was 11. Plain computed tomography (CT) showed a low-density nodule in the left hepatic lobe, which was 28 mm in maximum diameter and the largest among all the nodules. A contrast medium enhanced the nodule in the dynamic arterial phase and was washed out in the portal venous phase and late phase (Fig. 2). The nodule expressed isointensity relative to the surrounding liver parenchyma on T1-weighted magnetic resonance imaging (MRI), and homogeneous enhancement in the dynamic arterial phase, isointensity in the portal venous phase, isointensity in the late dynamic phase, and slight hypointensity relative to the surrounding liver parenchyma in the hepatocyte phase at 20 min on gadolinium-ethoxybenzyl-diethylenetriaminepentaacetic acid (Gd-EOB-DTPA)-enhanced MRI. In contrast, the nodules in S6 and S8 were definitely hypointense in the hepatocyte phase (Fig. 3). US-guided needle biopsy was performed for these 2 nodules. Both these nodules were histopathologically diagnosed with HCA. However, well-differentiated hepatocellular carcinoma (HCC) could not be completely ruled out, including other nodules. Therefore, we considered that preoperative diagnosis was “well-differentiated HCC or HCA”, so segmentectomy of the left lateral lobe, subsegmentectomy of S6, enucleation of tumors in S5 and S7, and open surgical radiofrequency ablation (RFA) for S4 and S7 tumors was performed. Three months postoperatively, transcatheter arterial chemoembolization (TACE) using miriplatin (Miripla; Dainippon-Sumitomo Pharma, Osaka, Japan), iodized oil (Lipiodol Ultra-Fluid; Guerbet, Aulnay-sous-Bois, France), and gelatin sponge particles (Gelpart; Astellas Pharma, Tokyo, Japan) and subsequent RFA were performed for the 3 residual tumors. Serum DCP levels were decreased from 436 mAu/ml before surgery naturally to 43 mAu/ml after surgery. They were constantly around 100 (102–118) mAu/ml after TACE plus RFA (Fig. 4). Although testosterone enanthate was being continued for GID, no recurrence was observed at least until 22 months after the intensive treatments.
Ultrasonography (US) examination images. US reveals multiple hyperechoic and hypoechoic nodules with a clear margin in both the lobes of the liver. Nodules in the left hepatic lobe, S5, and S6 were hyperechoic and inhomogeneous (a–c; arrows). A nodule in S8 was hypoehoic and inhomogeneous (d; arrow)
T1-weighted magnetic resonance imaging (MRI) and gadolinium-ethoxybenzyl-diethylenetriaminepentaacetic acid enhanced MRI images. The nodule in the left hepatic lobe expresses isointensity relative to the surrounding liver parenchyma on T1-weighted MRI (a; arrow). The nodule expresses homogenous enhancement in the dynamic arterial phase (b; arrow), isointensity in the portal venous phase (c; arrow), isointensity in the late dynamic phase (d; arrow), and slight hypointensity relative to the surrounding liver parenchyma in the hepatocyte phase at 20 min (e). Nodules in S6 and S8 were definitely hypointense in the hepatocyte phase (f, g; arrows)
Changes in serum alpha-fetoprotein (AFP) and serum des-gamma-carboxy prothrombin (DCP) levels are shown. AFP levels were kept in normal range. DCP levels were 935 mAu/ml on admission, 436 mAu/ml before surgery, and 43 mAu/ml after surgery. They were kept in the range of 102–118 mAu/ml after transcatheter arterial chemoembolization (TACE) followed by radiofrequency ablation (RFA)
Pathological findings
In total, 6 tumors were found in the 4 resected liver tissues. The tumor sizes ranged from 9 to 28 mm in diameter, and all the tumors showed well-defined margins and whitish cut surfaces. Microscopically, the tumor cells were basically arranged in one or two-cell-thick cords and plates. A pseudoglandular pattern was predominant in some places. Although mild nuclear atypia were found such as slight enlargement and irregularity in size and shape, the nucleo–cytoplasmic ratio was low and mitosis was not observed (Fig. 5a, b). We used immunohistochemical antibodies to β-catenin (DAKO, Glostrup, Denmark), GS (Chemicon, Inc., Temecula, CA, USA), L-FABP (Abcam, Cambridge, UK), CRP (Abcam), SAA (Abcam), and Glypican 3 (Nichirei Biosciences Inc, Tokyo, Japan) for the classification of HCA. Immunohistochemistry was performed on a VENTANA DISCOVERY auto-immunostainer (Roche Diagnostics, Tokyo, Japan). Antigen retrieval was carried out with CC1 buffer (Roche Diagnostics). β-catenin was expressed in the nucleus as well as cell membrane of the tumor cells (Fig. 5c). Tumor cells were diffusely positive for GS (Fig. 5d), while negative for Glypican 3. As for L-FABP, SAA and CRP, there were no findings suggesting H-HCA and I-HCA. Therefore, the tumor was diagnosed as b-HCA, not HCC, based on the histological features and immunohistochemistry findings. Liver histology showed nonspecific reactive hepatitis in the non-neoplastic area with the well-preserved lobular structure (Fig. 5e). The portal areas were inflamed with mild lymphoid cell infiltration. Necrosis and steatosis were seldom seen in the parenchymal area (Fig. 5f).
Histological features in the tumor at low magnification for Hematoxylin and Eosin staining. Tumor cells basically arranged in cords and plates show a conspicuous glandular pattern in this area (a). High magnification for Hematoxylin and Eosin staining. The tumor nuclei showed slight enlargement with small nucleoli, but severe nuclear atypia and mitosis were not observed (b). Immunostaining for β-catenin. The nucleus (c; arrows) as well as cell membrane of the tumor cells showed positive (c). Immunostaining for glutamine synthetase. The tumor cells showed strong positivity in diffuse pattern [this area corresponding to a] (d). The lobular structure was maintained in the non-tumor area for Hematoxylin and Eosin staining (e). The portal areas were inflamed with mild lymphoid cell infiltration. Necrosis and steatosis were seldom seen in the parenchymal area (f)
Discussion
In the United States, HCA development has only been reported in young women who use oral contraceptives [1]. The HCA incidence in Asia, including Japan, is lower than that in Europe and North America because Asians use oral contraceptives less frequently than westerners [12]. HCA is classified into 4 subtypes, and the WHO classification is widely used [10]. The prevalence rates of HCA subtypes are 33–46% for H-HCA, 18–60% for I-HCA, 5–19% for b-HCA, and 5–23% for u-HCA in the world [7, 9, 10, 13, 14]. On the other hand, they are 7.1% (1 of 14 cases) for H-HCA, 14.3% (2 of 14 cases) for b-HCA, 50.0% (7 of 14 cases) for I-HCA, and 28.6% (4 of 14 cases) for u-HCA in Japan [15]. The rate of H-HCA in Japan is lower than that in the world. Because HCA associated with mutant HNF1A, a major type of HNF1α-inactivated HCA, occurs almost exclusively in women [7, 9, 10, 13, 14], a relatively high rate of male HCA patients may be related to the low rate in of H-HCA subgroup in Japan. The prevalence of multiple tumors in b-HCA is 32% (10 of 31 cases) worldwide; however, it is 11% (1 of 9 cases) in Japan [2, 9, 13, 16,17,18]. Alternatively, the use of anabolic androgenic steroid, including testosterone, increases the HCA incidence in athletes and bodybuilders [17,18,19,20]. In addition to patients treated with a 6-month high-dose course, many patients underwent long-term (2–15 years) administration of an anabolic androgenic steroid. The HCA incidence may be related to the duration of medication. Furthermore, HCA development could be correlated with obesity [21,22,23]. This patient was an obese woman who had been treated with testosterone for 12 years; therefore, in this case, HCA development may be attributable to the long-term use of testosterone and obesity.
A hepatocyte phase of Gd-EOB-DTPA-enhanced MRI is useful for the diagnosis of HCC. OATP1B3 is a sodium-independent organic anion transporter localized to the basolateral hepatocyte membrane [24] and contributes to the uptake of Gd-EOB-DTA by hepatocytes. The MRI findings are influenced by the OATP1B3 expression level [25]. Regarding the relationship between HCA and OATP1B3, OATP1B3 expression is decreased in most β-catenin-negative HCAs, whereas OATP1B3 expression is preserved or increased in β-catenin-positive HCAs. In addition, most β-catenin-negative HCAs are hypointense during the hepatocyte phase of Gd-EOB-DTPA-enhanced MRI, whereas most β-catenin-positive HCAs are isointense or hyperintense during the hepatocyte phase of Gd-EOB-DTPA-enhanced MRI. HCAs with nuclear staining for β-catenin reflect preserved or enhanced OATP1B3 expression levels [16]. However, the tumors in this case exhibited iso-hypointensity. This result suggests that b-HCA diagnosis is challenging when using only the findings of the hepatocyte phase of the Gd-EOB-DTPA-enhanced MRI. Therefore, immunostaining of the biopsy or resected specimens appears necessary for the accurate diagnosis of b-HCA.
Malignant transformation of HCA is associated with tumor size. In particular, the risk of malignant transformation is high when the tumor size is > 5 cm in diameter [26]. Furthermore, the risk rate in men is ten times more frequent than that in women [27]. The activation of the β-catenin pathway is observed in benign hepatocellular tumors, suggesting that the pathway-related genes play a role at an early stage of hepatocellular tumorigenesis. The same nucleotide mutation of β-catenin was identified in both HCA and a part of HCC [13]. In fact, β-catenin-activated mutations are present in 20–34% of HCCs [28,29,30,31]. The frequency of HCCs associated with b-HCA is 43–46%, which is higher than that with other subtypes (0–7%) [9, 13]. Thus, b-HCA is at a higher risk of malignant transformation. According to the European Association for the Study of the Liver guidelines, the treatment for tumors with a size > 5 cm in diameter and b-HCA based on the immunohistological classification is recommended [32]. Our literature review showed that 7 patients without Fanconi anemia had HCA that developed during the administration of anabolic androgenic steroids. All of the patients were men. HCA classification was performed in 2 patients, both of whom were diagnosed with b-HCA [17,18,19,20, 33, 34] (Table 2). This patient was the first case of a woman in whom multiple HCA developed during the use of testosterone for FtM GID. Although this case was woman and the maximum tumor size in this case was < 5 cm in diameter, it was difficult to completely rule out well-differentiated HCC even in the tumor biopsy specimens. Therefore, tumor resection and ablation were performed for multiple liver nodules. The tumors were surgically resected; therefore, we could diagnose them as b-HCA with high risk of malignant transformation on the basis of immunohistochemical staining for the resected specimens. Therefore, we performed TACE and subsequent RFA for the residual tumors as postoperative additional treatment. Some studies have reported that HCA tumors disappeared or contracted after the discontinuation of oral contraceptives and anabolic steroids as well as weight loss in obese patients [19, 35, 36]. It is important to reduce the risk of malignant transformation; therefore, the discontinuation of testosterone and weight loss should be considered in this case. However, it is challenging to discontinue testosterone administration in patients with FtM GID. Periodic imaging tests, such as US and CT/MRI, are necessary for such patients who are being administered hormones.
While the concept and definition of GID are widely accepted in the society, the number of patients with GID is rapidly increasing and continues to leap upward for some time in the future. Although the global prevalence of transsexualism is 4.6 in 100,000 individuals [37], it is estimated mainly based on hospital records. The real-world prevalence of GID is expected to be higher, because several such individuals do not seek medical attention or are not diagnosed with GID. Furthermore, some patients receive treatment irregularly and some personally purchase over-the-counter hormone drugs. When a liver nodular tumor is accidentally detected and the differential diagnosis includes HCA, it is important to carefully interview patients about GID and testosterone use. Image inspection should be used to closely monitor patients receiving testosterone for HCA development.
References
Rooks JB, Ory HW, Ishak KG, et al. Epidemiology of hepatocellular adenoma. The role of oral contraceptive use. JAMA. 1979;242:644–8.
Sasaki M, Nakanuma Y. Overview of hepatocellular adenoma in Japan. Int J Hepatol. 2012;2012:648131. https://doi.org/10.1155/2012/648131.
Labrune P, Trioche P, Duvaltier I, et al. Hepatocellular adenomas in glycogen storage disease type I and III: a series of 43 patients and review of the literature. J Pediatr Gastroenterol Nutr. 1997;24:276–9.
Velazquez I, Alter BP. Androgens and liver tumors: fanconi’s anemia and non-Fanconi’s conditions. Am J Hematol. 2004;77:257–67.
Bird D, Vowles K, Anthony PP. Spontaneous rupture of a liver cell adenoma after long term methyltestosterone: report of a case successfully treated by emergency right hepatic lobectomy. Br J Surg. 1979;66:212–3.
Coombes GB, Reiser J, Paradinas FJ, et al. An androgen-associated hepatic adenoma in a trans-sexual. Br J Surg. 1978;65:869–70.
Bioulac-Sage P, Rebouissou S, Thomas C, et al. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007;46:740–8.
Bioulac-Sage P, Cubel G, Balabaud C, et al. Revisiting the pathology of resected benign hepatocellular nodules using new immunohistochemical markers. Semin Liv Dis. 2011;31:91–103. https://doi.org/10.1055/s-0031-1272837.
Bioulac-Sage P, Laumonier H, Couchy G, et al. Hepatocellular adenoma management and phenotypic classification: the Bordeaux experience. Hepatology. 2009;50:481–9. https://doi.org/10.1002/hep.22995.
Bioulac-Sage P, Balabaud C, Wanless I. Focal nodular hyperplasia and hepatocellular adenoma. In: Bosman F, Carneiro F, Hruban H, Theise N, editors. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC; 2010. p. 198–204.
Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology. 2013;144:888–902. https://doi.org/10.1053/j.gastro.2013.02.032.
Balabaud C, Al-Rabih WR, Chen P, et al. Focal nodular hyperplasia and hepatocellular adenoma around the world viewed through the scope of the immunopathological classification. Int J Hepatol. 2013;2013:268625. https://doi.org/10.1155/2013/268625.
Zucman-Rossi J, Jeannot E, Nhieu JT, et al. Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology. 2006;43:515–24.
Rebouissou S, Bioulac-Sage P, Zucman-Rossi J. Molecular pathogenesis of focal nodular hyperplasia and hepatocellular adenoma. J Hepatol. 2008;48:163–70.
Sasaki M, Yoneda N, Kitamura S, Sato Y, et al. Characterization of hepatocellular adenoma based on the phenotypic classification: the Kanazawa experience. Hepatol Res. 2011;41:982–8. https://doi.org/10.1111/j.1872-034X.2011.00851.x.
Fukusato T, Soejima Y, Kondo F, et al. Preserved or enhanced OATP1B3 expression in hepatocellular adenoma subtypes with nuclear accumulation of β-catenin. Hepatol Res. 2015;45:E32–42. https://doi.org/10.1111/hepr.12453.
Hardt A, Stippel D, Odenthal M, et al. Development of hepatocellular carcinoma associated with anabolic androgenic steroid abuse in a young bodybuilder: a case report. Pathology. 2012;2012:195607. https://doi.org/10.1155/2012/195607.
Solbach P, Potthoff A, Raatschen HJ, et al. Testosterone-receptor positive hepatocellular carcinoma in a 29-year old bodybuilder with a history of anabolic androgenic steroid abuse: a case report. BMC Gastroenterol. 2015;15:60. https://doi.org/10.1186/s12876-015-0288-0.
Socas L, Zumbado M, Perez-Luzardo O, et al. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature. Br J Sports Med. 2005;39:e27. https://doi.org/10.1136/bjsm.2004.013599.
Creagh TM, Rubin A, Evans DJ. Hepatic tumours induced by anabolic steroids in an athlete. J Clin Pathol. 1988;41:441–3.
Paradis V, Champault A, Ronot M, et al. Telangiectatic adenoma: an entity associated with increased body mass index and inflammation. Hepatology. 2007;46:140–6.
Bunchorntavakul C, Bahirwani R, Drazek D, et al. Clinical features and natural history of hepatocellular adenomas: the impact of obesity. Aliment Pharmacol Ther. 2011;34:664–74. https://doi.org/10.1111/j.1365-2036.2011.04772.x.
Bioulac-Sage P, Taouji S, Possenti L, et al. Hepatocellular adenoma subtypes: the impact of overweight and obesity. Liver Int. 2012;32:1217–21. https://doi.org/10.1111/j.1478-3231.2012.02786.x.
Cui Y, Konig J, Nies AT, et al. Detection of the human organic anion transporters SLC21A6 (OATP2) and SLC21A8 (OATP8) in liver and hepatocellular carcinoma. Lab Invest. 2003;83:527–38.
Narita M, Hatano E, Arizono S, et al. Expression of OATP1B3 determines uptake of Gd-EOB-DTPA in hepatocellular carcinoma. J Gastroenterol. 2009;44:793–8. https://doi.org/10.1007/s00535-009-0056-4.
Dokmak S, Paradis V, Vilgrain V, et al. A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology. 2009;137:1698–705. https://doi.org/10.1053/j.gastro.2009.07.061.
Farges O, Ferreira N, Dokmak S, et al. Changing trends in malignant transformation of hepatocellular adenoma. Gut. 2011;60:85–9. https://doi.org/10.1136/gut.2010.222109.
de La Coste A, Romagnolo B, Billuart P, et al. Somatic mutations of the beta-catenin gene are frequent in mouse and human hepatocellular carcinomas. Proc Natl Acad Sci USA. 1998;95:8847–51.
Miyoshi Y, Iwao K, Nagasawa Y, et al. Activation of the beta-catenin gene in primary hepatocellular carcinomas by somatic alterations involving exon 3. Cancer Res. 1998;58:2524–7.
Nhieu JT, Renard CA, Wei Y, et al. Nuclear accumulation of mutated beta-catenin in hepatocellular carcinoma is associated with increased cell proliferation. Am J Pathol. 1999;155:703–10.
Laurent-Puig P, Legoix P, Bluteau O, et al. Genetic alterations associated with hepatocellular carcinomas define distinct pathways of hepatocarcinogenesis. Gastroenterology. 2001;120:1763–73.
European Association for the Study of the Liver. (EASL). EASL Clinical Practice Guidelines on the management of benign liver tumours. J Hepatol. 2016;65:386–98. https://doi.org/10.1016/j.jhep.2016.04.001.
Hernandez-Nieto L, Bruguera M, Bombi J, et al. Benign liver-cell adenoma associated with long-term administration of an androgenic-anabolic steroid (methandienone). Cancer. 1977;40:1761–4.
Gorayski P, Thompson CH, Subhash HS, et al. Hepatocellular carcinoma associated with recreational anabolic steroid use. Br J Sports Med. 2008;42:74–5. https://doi.org/10.1136/bjsm.2007.03932.
Aseni P, Sansalone CV, Sammartino C, et al. Rapid disappearance of hepatic adenoma after contraceptive withdrawal. J Clin Gastroenterol. 2001;33:234–6.
Dokmak S, Belghiti J. Will weight loss become a future treatment of hepatocellular adenoma in obese patients? Liv Int. 2015;35:2228–32. https://doi.org/10.1111/liv.12925.
Arcelus J, Bouman WP, Van Den Noortgate W, et al. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30:807–15. https://doi.org/10.1016/j.eurpsy.2015.04.005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Keizo Kato, Hiroshi Abe, Noriko Hanawa, Junya Fukuzawa, Ryota Matsuo, Takeshi Yonezawa, Sadahiro Ito, Yoshiyuki Sato, Makiko Ika, Shohei Shimizu, Shinji Endo, Hiroshi Hano, Asami Izu, Masahiko Sugitani, and Akihito Tsubota declare that they have no conflict of interest.
Human rights
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Kato, K., Abe, H., Hanawa, N. et al. Hepatocellular adenoma in a woman who was undergoing testosterone treatment for gender identity disorder. Clin J Gastroenterol 11, 401–410 (2018). https://doi.org/10.1007/s12328-018-0854-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-018-0854-4