Abstract
Cholangiolocellular carcinoma (CoCC) is a rare malignant liver tumor derived from hepatic progenitor cells, which exist in the canals of Hering. We encountered a case of CoCC with an extremely poor clinical course, initially showing abnormally elevated serum alfa-fetoprotein (AFP). A 72-year-old male presented with a liver tumor and abnormally elevated serum AFP levels (16,399 ng/ml). We preoperatively diagnosed hepatocellular carcinoma and performed extended right hepatectomy, after which the serum AFP levels remarkably decreased to 97 ng/ml. Postoperatively, the disease was pathologically diagnosed as CoCC. Furthermore, immunohistochemical pathological findings were alcian blue negative, cytokeratin (CK) 7 partially positive, CK19 positive, hepatocyte paraffin-1 negative, membranous negative for epithelial membrane antigen, and AFP negative. Fifty-five days later, intra- and extrahepatic recurrence developed, and the patient died 65 days after surgery. Although CoCCs show favorable outcomes, these characteristics of our case were not previously reported. It is necessary to accumulate more information on CoCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholangiolocellular carcinoma (CoCC) is a rare malignant primary liver tumor which derives from the cholangioles or the canals of Hering [1]. Steiner and Higginson first described the distinct pathological characteristics of CoCC. Given the results of recent advancements in the study and knowledge of hepatic progenitor or stem cells, CoCC is currently considered to originate from hepatic progenitor cells (HPCs) [2–4].
Recently, Ariizumi et al. [5] demonstrated favorable outcomes for CoCC, regardless of tumor progression. Nevertheless, we encountered a case of CoCC presenting with an extremely poor clinical course. Moreover, the clinical features of this case initially included abnormally elevated serum alfa-fetoprotein (AFP) levels. Here, we report a case of a CoCC with rapid progression that initially presented with abnormally elevated serum AFP levels.
Case report
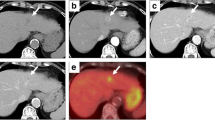
A 72-year-old male with chronic hepatitis C was referred for an evaluation of elevated levels of serum AFP and protein induced by vitamin K absence-II (PIVKA-II) as well as an asymptomatic liver mass that was detected on abdominal ultrasonography. Serum levels at the time of admission to our hospital were AFP 16,399 ng/ml (normal <10.0) and PIVKA-II 377 mAU/ml (normal <40). Liver function test results and levels of serum total bilirubin and albumin were within the normal range. The retention rate of indocyanine green at 15 min was 13.0 % (normal range 0–10 %) and prothrombin time was 88.8 % (normal >70). Abdominal computed tomography (CT) revealed a low-density mass (Fig. 1a) with lobular growth in segments V and VIII of the liver. The arterial phase of CT showed marked enhancement of the tumor (Fig. 1b), with homogeneous enhancement in the portal phase (Fig. 1c). The enhancement of the lesion was washed out in the late phase (Fig. 1d). The tumor invaded the middle hepatic vein and the diaphragm. CT did not reveal ascites or enlarged lymph nodes at the hepatoduodenal ligament.
Preoperative abdominal computed tomography (CT). CT shows a low-density mass, measuring 5 cm, in segments 6 and 8 of the liver (a). The tumor showed enhancement during the arterial phase (b), and the central area of the tumor showed mosaic enhancement during the portal phase (c). The enhancement of the lesion is washed out in the late phase (d)
Preoperatively, the tumor was diagnosed as hepatocellar carcinoma (HCC) on imaging studies and considering the tumor marker levels. With the aim of macroscopic curative resection, an extended right hepatectomy was planned. To obtain sufficient future liver remnant for functional hepatic volume, percutaneous transhepatic portal vein embolization (PTPE) was performed. Following PTPE, we performed an extended right hepatectomy. After surgery, the serum AFP level remarkably reduced to 97.0 ng/ml. The patient was categorized as having grade B post-hepatectomy liver failure using the International Study Group of Liver Surgery classification system [6]. The total bilirubin level improved without invasive treatment. However, 55 days after surgery, the patient complained of dyspnea and developed a pleural infusion with positive malignant cytology. Concurrently, CT showed intrahepatic recurrence, and peritoneal and pleural metastases (Fig. 2) without an increase in tumor marker levels; the serum AFP level was 4.6 ng/ml. The patient’s general condition worsened, and he died 65 days after surgery.
Macroscopically, three tumors were found—the main tumor was whitish and hard (8.0 × 7.5 × 6.0 cm) with an indistinct border (Fig. 3). For microscopic study, hematoxylin and eosin (H&E) staining and immunohistochemical staining using antibodies against alcian blue, cytokeratin (CK) 7 and 19, epithelial membrane antigen (EMA), hepatocyte paraffin (HepPar) 1, and AFP were performed for tumor sections. A pathological examination was performed for each tumor. Histological analysis revealed small ductules in an anastomosing pattern with a moniliform structure (Fig. 4a). On immunohistochemical staining, cancer cells exhibited negative staining for alcian blue (Fig. 4b), partially positive staining for CK7 (Fig. 4c), diffusely positive staining for CK19 (Fig. 4d), membranous negative staining for EMA (Fig. 4e), negative staining for HepPar-1 (Fig. 4f), and negative staining for AFP (Fig. 4g).
Microscopic findings: H&E staining (a): magnification ×40). Small ductules show an anastomosing pattern, and comprise a moniliform structure. In focal areas of the tumor, relatively large ductules are detected and resemble cholangiolocellular carcinoma. Immunohistochemical staining for alcian blue (b), CK7 (c), CK19 (d), EMA (e), HepPar-1 (f), and AFP (g): magnification ×200. The tumor cells tested diffusely positive for CK19, slightly positive for CK7, and negative for alcian blue, HepPar-1, and AFP, and membranous negative staining for EMA
Discussion
CoCC is a rare malignant primary liver tumor that is thought to originate from HPCs considering the recent advances in the knowledge of HPCs. Although patients with CoCC usually present with a relatively favorable clinical course [5], we encountered a rare case of CoCC with an extremely poor clinical course in which levels of serum AFP were initially abnormally high. Our case may highlight a mechanism for the development of CoCC involving an ability to produce AFP through the process of carcinogenesis.
The prognosis of CoCC remains unclear because of its rarity. Recently, Ariizumi et al. [5] demonstrated a favorable prognosis and reported that the presence of CoCC was an independent favorable prognostic factor regardless of tumor progression. However, the present case did not have a favorable clinical course, suggesting that an unusual carcinogenesis process may have occurred and influenced the poor outcome. Moreover, a clinical feature of this unusual case was the initially abnormally high serum AFP level.
AFP is recognized as a representative marker for HPCs. Evidence indicates that HPCs express AFP mRNA at high levels [7]. CoCC is thought to originate from HPCs and occasionally has small components of HCC [4, 5], which may contribute to elevated levels of serum AFP. Ariizumi et al. demonstrated that CoCC presented with levels of serum AFP that are higher than the normal level. However, this finding, in which patients presented with abnormally elevated serum levels of AFP (>1,000 ng/ml), was not described in detail. Therefore, we performed a systematic search of the PubMed database for English-language literature up to January 2016, using the search term ‘cholangiolocellular cholangiocarcinoma’. Only one case [4] of CoCC with an abnormally elevated level of serum AFP (>1,000 ng/ml) was reported in detail with an unfavorable clinical course (Table 1). The level of serum AFP in that case was lower than it was in our case. Unfortunately, we were unable to detect an immunohistochemically AFP-positive area in the resected specimens. Possible reasons for this include detectability of antigen, tumor characteristics (poor differentiation), or the number of resected specimens examined. Considering that the serum AFP level decreased after surgery, it is possible that the tumor did initially have the ability to produce AFP. Recurrent disease did not occur with an elevated serum AFP level, suggesting that, in this case, CoCC might differentiate into cholangiocarcinoma (CCC) [8]. Although we were unable to detect components of HCC or CCC, owing to the limited analysis, we cannot conclude that the primary tumor had no HCC or CCC component, i.e., possibility of diagnosis as combined HCC–CCC. Perhaps, the original components differentiated. Although the mechanism of AFP production and whether AFP production contributed to the poor outcome were unclear, it may be that a portion of CoCCs, including the case reported here, has the ability to produce AFP.
Conclusion
We reported a case of CoCC that had rapid progression and a poor outcome. The clinicopathological features of CoCC remain controversial. Our data indicate that CoCC with a poor prognosis exists, and that additional data are needed to gain a greater understanding of this disease.
References
Steiner PE, Higginson J. Cholangiolocellular carcinoma of the liver. Cancer. 1959;12:753–9.
Shiota K, Taguchi J, Nakashima O, et al. Clinicopathologic study on cholangiolocellular carcinoma. Oncol Rep. 2001;8:263–8.
Kozaka K, Sasaki M, Fujii T, et al. A subgroup of intrahepatic cholangiocarcinoma with an infiltrating replacement growth pattern and a resemblance to reactive proliferating bile ductules: ‘‘bile ductular carcinoma’’. Histopathology. 2007;51:390–400.
Komuta M, Spee B, Vander Borght S, et al. Clinicopathological study on cholangiolocellular carcinoma suggesting hepatic progenitor cell origin. Hepatology. 2008;4:1544–56.
Ariizumi S, Kotera Y, Katagiri S, et al. Long-term survival of patients with cholangiolocellular carcinoma after curative hepatectomy. Ann Surg Oncol. 2014;21:S451–8.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
DabevaMD S. Activation, proliferation, anddifferentiationof progenitor cells into hepatocytes in the d-galactosamine model of liver regeneration. Am J Pathol. 1993;143:1606–20.
Kadono M, Kimura K, Imamura J, et al. A case of a large cholangiolocellular carcinoma. Clin J Gastroenterol. 2011;4:340–6.
Acknowledgments
I would like to gratefully and sincerely thank Dr. Tsutumi in Saiseikai Chuwa Hospital for suggesting the pathological assessment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
All authors declare no conflict of interest.
Human Rights:
All procedures followed have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent:
Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Yoh, T., Kato, T., Hirohata, Y. et al. Cholangiolocellular carcinoma with rapid progression initially showing abnormally elevated serum alfa-fetoprotein . Clin J Gastroenterol 9, 257–260 (2016). https://doi.org/10.1007/s12328-016-0667-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-016-0667-2