Abstract
We describe a case of chylous ascites with strangulated ileus, and review all 22 cases (including our case) of chylous ascites with strangulated ileus reported in the English and Japanese literature. The patient we describe was a 51-year-old woman with medical history of radiotherapy for cervical cancer of the uterus 15 months prior to being admitted to our hospital with abdominal pain after consuming a meal. A computed tomography (CT) scan revealed ascites, expansion of the small intestine, and whirl sign. Laparotomy revealed chylous ascites with an incarcerated internal hernia of the small intestine, which was released without intestinal resection. In our case the postoperative phase was uneventful, and as in the other 21 literature cases reviewed, treatment by either detorsion, release of the incarcerated internal hernia, or incision of the adhesion band without intestinal resection resulted in rapid improvement in the color of the intestine. It is considered that minimally invasive laparoscopic laparotomy should be selected as the treatment of first choice, because the degree of strangulation is slight in cases where chylous ascites is associated with strangulated ileus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chylous ascites is defined as extravasation of milky or creamy peritoneal fluid rich in triglycerides, caused by the presence of thoracic or intestinal lymph in the abdominal cavity. There are multiple causes of chylous ascites [1], the most common in Western countries being abdominal malignancy and cirrhosis, which account for over two-thirds of all cases. In contrast, infectious etiologies, such as tuberculosis and filariasis, account for the majority of cases of chylous ascites in Eastern and developing countries [2]. Other causes of chylous ascites include congenital, inflammatory, postoperative, traumatic, and miscellaneous disorders.
We describe herein a case of chylous ascites with strangulated ileus, and review all 22 reported cases (including our case) of chylous ascites with strangulated ileus in the English and Japanese literature.
Case report
Case 51 years old, female.
Chief complaint Epigastric pain after consuming a meal.
Past history In February 2013, the patient underwent radiochemotherapy for cervical cancer of the uterus and metastasis of lymph nodes (stage 1b2).
Operative history Nil.
Present illness In May 2013, epigastric pain appeared a few hours after consuming a meal. The pain disappeared spontaneously during 3 months of meal restriction. In May 2014 she again experienced epigastric pain after consuming a meal, and a few days following this episode she experienced sudden epigastric pain after eating her evening meal. This pain gradually increased, resulting in her being transferred to our hospital by ambulance.
Physical examination On examination the patient’s blood pressure was 104/66 mmHg, pulse 65 beats/minute, and temperature 36.0 °C. Her abdomen was mildly bulging, but soft. Severe tenderness was observed in the epigastric region, but rebound tenderness was not remarkable. There was pain that resonated in the epigastric region when pressure was applied in the lower right quadrant of the abdomen, similar to the referred pain with appendicitis.
Laboratory studies (Table 1) The leukocyte count was 6460/mm3, NEUT 76 %, CRP 0.00 mg/dl. Only slight leukocytosis was observed, and no inflammatory signs were seen. Serum protein and creatinine values were mildly abnormal, and the other tests were within the normal ranges of biochemistry tests.
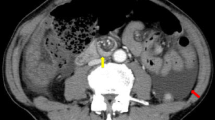
Plain and contrast-enhanced CT scans The retention of the stomach content was outstanding when examined 6 h after ingestion of the meal, and retention of a little ascites was seen around the liver and spleen. At that time the entire small intestine had a feeling of expansion and the liquid content was noticeable in the intestinal lumen. There was also thickening of the wall of the small intestine in the left abdomen but niveau (air–fluid level) formation was not evident. Changes to the small intestine were also noticeable in the pelvic region, but the running of its contents was difficult to follow. The colon was slightly collapsed, and its wall was slightly thick and edematous. The transverse plane revealed a “whirl-like sign” (Fig. 1).
An internal hernia forming something like a cord in the small intestine was suspected from these findings as there was a slight drop in the contrasting effect of nutritional blood vessels of the small intestine in the internal hernia, and ischemia was doubted.
Although there was no history of surgery, from these findings it was suspected that the strangulated ileus was caused by an incarcerated internal hernia due to the formation of something like a cord made after radiation for cervical cancer of the uterus.
Operative finding Laparoscopic laparotomy (LL) revealed a moderate amount of dirty yellowish white fluid in the lower abdomen and around the liver. Peritonitis due to perforation of the intestine was suspected, so the LL was converted to open laparotomy. The site of the perforation could not be discovered. Although the fluid found was yellowish white fluid, there was not a bad smell of pus present. Analysis of the fluid using Gram staining of a smear of the fluid during surgery failed to recognize the presence of any bacteria. At this point, the yellowish white fluid in the abdominal cavity was suspected as chyle, not pus.
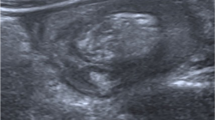
The small intestine on the 50-cm oral side and on the 90-cm oral side from the ileocecal region were adhered with funicular fiber, and about 30 cm of the small intestine was incarcerated into the narrow portion as an internal hernia (Fig. 2). The incarcerated intestine was edematous, but there were no changes observed to the color of the intestines. Therefore, only the funicular fiber band was divided, and this released the incarceration without intestinal resection.
A closed-suction tube was placed in the Douglas space, and the abdominal wall was sutured and closed by layer.
Ascites finding The fluid was yellowish white in color and cloudy in appearance. A positive stain of fat globules when Sudan Black B was applied was observed. Ascites was sterile on culture, and cytology showed class II. Unfortunately, biochemical examination of the ascites was not done. The ascites contained Sudan Black B stain-positive particles, which led to a diagnosis of chylous ascites.
Postoperative course Fluid in the drain tube postoperatively was serous in nature. Movement of the intestinal tract postoperatively was poor, so oral intake was delayed. Oral intake was commenced on postoperative day five (POD5). The drain was removed on POD6 after confirmation that there was no white fluid in the drain after the patient had eaten a meal. After that the postoperative course was uneventful, and the patient was discharged from the hospital on POD9.
Discussion
Chylous ascites is defined as extravasation of milky- or creamy-appearing peritoneal fluid rich in triglycerides, caused by the presence of thoracic or intestinal lymph in the abdominal cavity [1].
Typically, chyle has a white cloudy and turbid appearance, in contrast to the straw-colored and transparent appearance of ascites caused by cirrhosis and portal hypertension. The triglyceride levels in ascetic fluid are very important in defining chylous ascites. Triglyceride values are typically above 200 mg/dl. A positive stain of fat globules with Sudan Red, and disappearance of the color of ascitic fluid on addition of ether are characteristic [2].
Chylous ascites is an uncommon finding with reported incidence of approximately one in 20,000 admissions at a large university-based hospital over a 20-year period [3]. Nonetheless, it is believed that the incidence has increased because of more aggressive cardiothoracic and abdominal surgery and because of longer survival rates of patients with cancer.
Development of chylous ascites is usually associated with trauma, iatrogenic or otherwise. It can be a result of direct injury to the lymphatics during surgery and is more commonly seen if retroperitoneal, esophageal or gastric surgery is performed, particularly in oncological resections. External trauma can lead to chylous ascites through hyperextension and hyperflexion during blunt abdominal trauma which caused rupture of lymphatic vessels. It can also result from indirect injury to lymphatics through radiotherapy. Radiation therapy was the most common “inflammatory” cause of chylous ascites in Oliver’s review [1]. All cases involved abdominal or pelvic radiation. In a review of 207 patients who received whole-abdomen irradiation for gynecologic malignancies at the Mayo Clinic, 3 % incidence of chylous ascites was observed [4]. Abdominal radiation causes radiation-induced fibrous substance of the lymphatic vessels within the small bowel and/or mesentery. Obstruction of the lymphatic vessels results in the extravasation of chylous fluid. Clinically, chylous ascites is typically observed a mean time of 12 months after radiation therapy [5, 6]. At first our case of chylous ascites was considered to be due to a lymphatic disorder caused by radiation therapy, because the patient had undergone radiation therapy for cervical cancer of the uterus 15 months before. However, during surgery, the lymph vessels of the mesentery in the incarcerated intestine were dilated edematously, and the fluid from the postoperative drain positioned in the abdominal cavity did not become cloudy white after the patient had consumed a meal. So the cause of chylous ascites was not a lymphatic disorder by radiation therapy, and was considered to be due to stasis of the lymph flow of the mesentery by strangulation of the intestine.
Strangulated ileus is classified according to cause as follows:
-
1.
Fastening by postsurgical, postradiation adhesion
-
2.
Incarceration of hernia (inguinal, femoral, internal)
-
3.
Intussusception of the intestine
-
4.
Volvulus or torsion of the intestine.
Our case did not have a surgical history, but radiation therapy for cervical cancer of the uterus 15 months before. Radiation-induced injury of the small and large bowel have been recognized. The frequency of gastrointestinal complications following radiation therapy was 2–20 %. Side-effects of radiation on the intestine, such as ileus and hemorrhagic colitis, are more frequent after pelvic radiation [7–9].
Therefore, the mechanism of occurrence of chylous ascites in our case was considered to be that, at first, adhesion of the small intestine after radiation therapy appeared; then the internal hernia was formed; followed by the small intestine being incarcerated into the narrow part; then, although the mesenteric arteries and veins with high-pressure flow were not occluded, the lymph vessels with low-pressure flow were occulted by loose strangulation; and finally stasis and leakage of lymph occurred into the abdominal cavity.
A search of English and Japanese literature concerning case reports of chylous ascites with strangulated ileus revealed 22 cases, including our case. Of these, 16 cases were male and six were female, ranging in age from 13 to 88 years (mean age 56.2 ± 19.8 years).
Fourteen of the 22 cases had surgical history. The diseases and operative procedures are presented in Table 2.
Surgical procedures performed included segmental resection of the pharyngo-esophagus and reconstruction with free jejunum for one case of hypopharyngeal cancer [11], subtotal esophagectomy and gastric tube reconstruction for two cases of esophageal cancer [10, 19], total gastrectomy and Roux-en-Y reconstruction for five cases of gastric cancer [12–15, 21], distal subtotal gastrectomy and B-I reconstruction for one case of gastric cancer [18], and distal subtotal gastrectomy and B-II reconstruction for gastric ulcer and duodenal ulcer [20, 22]. One case of small intestine cancer had surgical history involving three operations, namely right hemicolectomy, sigmoidostomy, and partial resection of small intestine for perforated ileus due to recurrence [16]. One case had undergone laparoscopic cholecystectomy [17]. One case had undergone laparoscopic sigmoidectomy for volvulus [23]. Chylous ascites with strangulated ileus was frequent after surgery of the upper abdomen from the esophagus.
Eight of the 22 cases did not have history of surgery, and seven of those eight cases had volvulus, or torsion of the small intestine [24–30], while our case had incarcerated internal hernia of the small intestine by band formation after radiation therapy for cervical cancer of the uterus (Table 3).
Preoperative abdominal CT scan showed characteristically expansion of the small intestine, ascites, whirl sign, and edema of the concerned mesentery.
Fourteen cases with history of surgery had a diagnosis of strangulated ileus due to intestinal volvulus, incarcerated internal hernia, fasting by band formation with adhesion, or adhesion of a loop of the ileum to the colon by a band which twisted itself. Seven of the eight cases without history of surgery had strangulated ileus by intestinal volvulus, and one had an incarcerated internal hernia due to adhesions after pelvic radiation.
After treatment, the color tone of the intestine improved quickly by detorsion, release of incarcerated internal hernia, or incision of the adhesion band in all cases. There were no cases where intestinal resection was performed. The degree of strangulation was mild based on these operative findings and managed in all cases. It seems, therefore, that a laparoscopic operation could very possibly be sufficient treatment in these cases.
In two cases, including our case, LL was performed at first, but was converted to open laparotomy after confirmation of white ascites. At this point, we should accept these findings for what they are worth, and continue our research into laparoscopic operations and their outcome.
In only one case was chylous ascites confirmed preoperatively by abdominal paracentesis using an echo guide for a large amount of ascites on CT examination. In spite of the diagnosis of chylous ascites, open laparotomy was performed as emergency following the diagnosis of strangulated ileus with chylous ascites.
It was considered that abdominal paracentesis should be performed using an echo guide even if at first there was no diagnosis of strangulated ileus with ascites, no obvious expansion of the small intestine or whirl sign on a CT scan, poor rebound tenderness, and no significant laboratory data were found and the patient’s general condition was not serious. Also, after verifying chylous ascites, it was considered that minimally invasive LL should be selected as the first choice, because the degree of strangulation was slight in cases with chylous ascites associated with strangulated ileus.
Abbreviations
- CT:
-
Computed tomography
- NEUT:
-
Nitrophilic leukocyte
- CRP:
-
C-reactive protein
- LL:
-
Laparoscopic laparotomy
- POD:
-
Postoperative day
References
Aalami OO, Allen DB, Organ CH. Chylous ascites: a collective review. Surgery. 2000;128:761–78.
Cardenas A, Chopra S. Chylous ascites. Am J Gastroenterol. 2002;97:1896–900.
Press OW, Press NO, Kaufman SD. Evaluation and management of chylous ascites. Ann Intern Med. 1982;96:358–64.
Lentz S, Schray M, Wilson T. Chylous ascites after whole-abdomen irradiation for gynecologic malignancy. Int J Radiat Oncol Biol Phys. 1990;19:435–8.
Hurst P, Edwards J. Chylous ascites and obstructive lymphedema of the small bowel following abdominal radiotherapy. Br J Surg. 1979;66:780–1.
Todd TF. Rectal ulceration following irradiation treatment of carcinoma of the cervix uteri. Surg Gynecol Obstet. 1938;67:617–31.
Chino A, Suganuma T, Uragami N, et al. Radiation induced enterocolitis. Gastroenterol Endosc. 2010;52:1381–92 (in Japanese with English abstract).
Keung Y, Whitehead R, Cobos E. Chemotherapy treatment of chyloperitoneum and peritoneal carcinomatosis due to cervical cancer-review of literature. Gynecol Oncol. 1996;61:448–50.
Asahi H, Sasaki J, Isshiki M, et al. Five cases of the intestinal obstruction by radiation injury. Jpn J Gastroenterol Surg. 1981;14:117–22 (in Japanese with English abstract).
Kimura Y, Ikeda K, Fujita M, et al. A case of strangulated ileus with chylous ascite. J Jpn Colle Surg. 2004;29:254–7 (in Japanese with English abstract).
Taruno K, Miyashiro M, Matsushima K, et al. A case of strangulated ileus accompanied with chylous ascites. J Okinawa Med Assoc (in Japanese). 2007;45:46–8.
Shindo Y, Tenma K, Yoshino T, et al. A case of intestinal volvulus with chylous ascites after total gastrectomy. Surgery. 2007;69:711–4 (Geka, in Japanese).
Kamei N, Sakurai J, Katayama M, et al. A case of strangulated ileus accompanied with chyle-like ascites. J Jpn Surg Assoc. 2008;69:1683–6 (in Japanese with English abstract).
Sugawara H, Miyazaki S. A case of volvulus-caused acute chylous peritonitis. J Jpn Surg Assoc. 2009;70:895–8 (in Japanese with English Abstract).
Umemura A, Hida K, Kimura Y. A case of strangulated ileus with chylous ascites. J Abdom Emerg Med. 2010;30:847–50 (in Japanese with English abstract).
Kato K, Otsuka K, Itabashi T, et al. A case strangulated ileus with chylous ascites. J Jpn Surg Assoc. 2011;72:2056–60 (in Japanese with English Abstract).
Pengelly S, Potiszil K, Feldman M. Spontaneous midgut volvulus causing chylous ascites in an octogenarian. BMJ Case Rep. 2012;10:1136.
Shima H, Sugiura H, Shimizu Y, et al. A case of strangulated ileus with chylous ascites. J Jpn Surg Assoc. 2013;74:1281–5 (in Japanese with English Abstract).
Uji Y, Tokunaga M, Shingami K, et al. A case of strangulated ileus with chylous ascites. J Jpn Surg Assoc. 2013;74:92–5 (in Japanese with English Abstract).
Ishiba T, Enjoji M, Hiraoka Y, et al. A case of strangulated ileus with chylous ascites. J Abdom Emerg Med. 2014;34:911–4 (in Japanese with English Abstract).
Matsunaga T, Nakata K, Nagai E, et al. A case of chylous ascites associated with an internal hernia of the small bowel after total gastrectomy. J Jpn Surg Assoc. 2014;75:1261–4 (in Japanese with English Abstract).
Ishii W, Sato N, Iiduka, et al. A case of volvulus of the intestine with chylous ascites. J Abdom Emerg Med. 2014;25:233–7 (in Japanese with English Abstract).
Pai A, Park JJ, Marecik SJ, et al. Midgut volvulus presenting with acute chylous peritonitis. Clin Case Rep. 2014;2:159–61.
Yonezawa K, Yokoo N, Shiroko T, et al. A case of intestinal volvulus with chylous ascites in child. J Jpn Surg Assoc. 1997;58:2880–3 (in Japanese with English abstract).
Honda H, Tsuzawa T, Kawada T, et al. A case of primary small bowel volvulus in adult. J Jpn Surg Assoc. 2004;65:112–6 (in Japanese with English Abstract).
Kobe D, Watanabe A, Nakagawa K, et al. A case of primary small bowel volvulus. J Nara Med Assoc. 2008;12:65–7 (in Japanese with English abstract).
Maki A, Fujiki T, Matsuo K, et al. A case of primary volvulus of the small intestine in adult. J Jpn Surg Assoc. 2008;69:567–71 (in Japanese with English abstract).
Hanawa H, ogasawara Y, Kanoh T, et al. A case of volvulus of the small intestine in adult with chylous ascites and mesenteric edema. J Jpn Surg Assoc. 2012;73:603–7 (in Japanese with English abstract).
Koh YX, Chung JK, Tan HC, et al. Intestinal torsion causing chylous ascites: a rare occurrence. Singapore Med J. 2013;54:e88–90.
Tewari N, Bhalla A, Iftikhar S. Chylous ascites: why exercise is bad for you. Int J Surg Rep. 2013;4:118–20.
Disclosures
Conflict of interest: Yukari Harino and other co-authors have no conflict of interest.
Human/Animal Rights: This study does not contain any data about human or animal subjects.
Informed Consent: This study does not involve human subjects.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harino, Y., Kamo, H., Yoshioka, Y. et al. Case report of chylous ascites with strangulated ileus and review of the literature. Clin J Gastroenterol 8, 186–192 (2015). https://doi.org/10.1007/s12328-015-0573-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12328-015-0573-z