Abstract
Spinocerebellar ataxias (SCA) constitute of a group of degenerative and progressive disorders that can be identified on a molecular and cellular basis. Along with histological changes, the clinical presentation of SCA differs between subtypes. In addition to basic cerebellar dysfunction symptoms, patients with SCA develop gait ataxia, dysphagia, dysarthria, oculomotor disturbances, pyramidal and extrapyramidal disease signs, rigidity, bradycardia, sensory deficits, and mild cognitive and executive function decline. MRI scans have confirmed reduction in mass of frontal, temporal, and parietal portions of the brain along with the cerebellar peduncles, brainstem, and cranial nerve III. Clinically, these damages manifest as decline in cognition and problems with speech, contemplation, and vision. This review article compares the most prevalent subtypes of SCA based on genetic background, pathogenesis, neurological manifestations, other presenting symptoms, and diagnostic workup. Further goals of research in this field should be directed towards a cure for SCA, which currently does not exist.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent discoveries regarding the diseases known as spinocerebellar ataxias (SCA) have opened gates to a wide variety of research opportunities, especially regarding SCA6. SCA, collectively, are progressive and degenerative genetic disorders that can be characterized by discordant gait, in association with poorly coordinated speech, hands, and eye movements. SCA1 was first identified in 1993 as a mutation of the ATXN1 gene encoding that ataxin-1 protein, with 44 total autosomal dominant SCA currently identified affecting gene loci on all chromosomes besides 8, 9, 10, 21, and 23 [1]. The primary mutation of SCA6 alters the transcription of a calcium channel gene located on chromosome 19p via CAG repeat expansions [2]. Histologically, Gierga et al. confirmed that in SCA6, there is an absence of layer V giant Betz pyramidal cells in the primary motor cortex and an expansive degeneration of brainstem nuclei, along with cerebellar damage, the common denominator in all subtypes of SCA [3] SCA6, which was once thought to be a disorder of purely cerebellar damage, has now been labeled as “primarily” cerebellar manifestations because of findings that showed marked neurodegeneration throughout the brain, rather than just in the cerebellum as previously thought, with in vivo brain MRI showing degeneration of the cerebellum, cerebral cortex, thalamus, midbrain, pons, and medulla [3, 4].
The most common genotypes of SCA are SCA1, SCA2, and SCA3, and SCA6. SCA1 and SCA3 are more similar to each other, and more severe than other forms of SCA, in terms of atrophy prominent in all brainstem regions in addition to the cerebellum, putamen, and caudate nucleus, with Schulz et al. revealing a direct correlation of clinical findings in SCA1 with atrophy of the pons and SCA3 clinical findings with total brainstem atrophy [4]. On the other hand, clinical manifestations of SCA6 (as rated on the Unified Huntington’s Disease Rating Scale) were correlated only with total cerebellar atrophy [4]. While the 44 various SCA subtypes arise through multiple types of mutation mechanisms, CAG (polyglutamine) repeats are responsible for SCA genotypes 1, 2, 3, 6, 7, and 17 [5]. The insulted proteins, which serve as biochemical markers, lead to repeated aggregates in the form of intranuclear or cytoplasmic inclusions. SCA genotypes 7, 11, 20, 31, and 32 have exhibited clear symptoms of the disease associated with these intracellular inclusions [5]. For example, SCA7 is associated with retinal degeneration, SCA11 with tau aggregation, SCA20 with dentate calcification, SCA31 with protein deposition in the Purkinje cell layer, and SCA32 with azoospermia [5]. Although the exact pathogenesis caused by the inclusions have yet to be distinguished, hindrance in axonal transport, appendage of transcription factors, and degraded protein quality have been linked to these inclusions [5]. In all cases of polyglutamine repeat ataxias, the length of the repeat can be proportionately correlated to the age of onset of symptoms. In addition, an anticipatory phenomenon is observed whereby additional expansion of trinucleotide repeat results in earlier onset of symptoms in the offspring of the affected individual. Although there is no established approach to halt this phenomenon, alleviation of symptoms and stopping the rapid progression of disease is possible through physical, occupational, and speech therapy. Further research on symptom onset and management of SCA6, along with continued exploration of the genetic, anatomic, and histological impacts of SCA6 can lead to improved patient outcomes in the future.
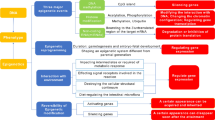
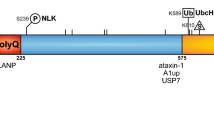
Genetics and Pathogenesis of SCA6
SCA6 can present as sporadic mutation or via autosomal dominant inheritance. Though the disease is characterized as a polyglutamine disorder (a gain of function mutation), the small number of repeats puts it in the normal range compared to other SCA genotypes, and SCA6 may be best categorized as a channelopathy [6, 7]. In symptomatic patients, SCA6 presents with 20–33 CAG repeats found on chromosome 19p13.2-p13.1 of the 3′ region (C-terminus) of the bicistronic CACNA1A gene, which encodes the α1A subunit of the P/Q type voltage-gated calcium channel [8,9,10]. The C-terminus has roles in channel function [10]. The P-type calcium channel affected in SCA6 has been found in the bifurcations of cerebellar Purkinje cell dendrites, molecular layer of cerebellar cortex, periglomerular cells of olfactory bulb, scattered neurons in deep layer of entorhinal and pyriform cortices, brainstem, habenula, nucleus of the trapezoid body and inferior olive, floor of fourth ventricle, layer II pyramidal cells of frontal cortex, CA1 cells of hippocampus, lateral nucleus of substantia nigra, lateral reticular nucleus, spinal fifth nucleus, and the striatum [11]. SCA6 is unique in that the P/Q type channel can be found in the cytoplasm and nucleus of Purkinje cells, whereas it is found in the nucleus of various neurons in most other polyglutamine diseases [7]. It has been shown that a piece of the C-terminal, containing polyglutamine tracts, translocates from the cytoplasm to the nucleus, with nuclear localization contributing to toxicity [12]. The exact pathogenesis of this mechanism is unclear: changes in the calcium channel may lead to collections of proteins with polyglutamine, mutations in the calcium channel may lead to cell death, or there may be proteins with both polyglutamine and calcium channel proteins causing dysfunction [7]. The main hypotheses for CAG repeat diseases are that proteins with polyglutamine sequences recruit others with similar repeats leading to toxic effects, or that collections of polyglutamine proteins inhibit the ubiquitin-proteasome pathway, preventing protein breakdown [13]. Molecular chaperones prevent protein misfolding and aggregation, and it is possible that polyglutamine expansions hinder interaction with chaperone proteins, leading to degeneration and loss [10, 13].
The CACNA1A gene has been also associated with other related movement disorders. Over 80 mutations in the CACNA1A gene have been linked to episodic ataxia type 2 (EA2), which presents with episodes of ataxia and nystagmus. In addition, familial hemiplegic migraine is associated over 20 mutations in the gene and commonly presents with migraines, ataxia and nystagmus. Sporadic hemiplegic migraine presents similarly to familiar hemiplegic migraine; however, patients present with no family history of the disease. Finally, 19p13.13 deletion syndrome is caused by a deletion in a section of chromosome 19 containing CACNA1A. Features associated with the disease include macrocephaly, intellectual disability, tall stature, seizures, and ataxia [14].
Neurological Manifestations of SCA6
Cerebellum
A summary of known anatomical findings associated with SCA6 can be found in Table 1. Within the cerebellum, affected locations include vermis, fastigial, globose emboliform, dentate nuclei, and white matter [3, 4]. A study by Schulz et al. showed loss of brain tissue in grey matter of the cerebellum on voxel-based morphometry and volumetry, while a study by Wang et al. showed atrophy in the superior vermis, reduced molecular layer of the cerebellar cortex, dentate nucleus, and inferior olivary complex, atrophic neurons with pyknotic cytoplasm in the dentate nuclei, and severely decreased number of Purkinje cells with reduced dendritic mass, spines, and branching complexity [4, 15]. Note that primary neurodegeneration occurs in the cerebellum and trans-synaptic degeneration in the precerebellar nuclei, with hypothesized retrograde trans-synaptic degeneration in the olivocerebellar connections [15]. Loss of Purkinje cells with Bergemann’s gliosis is evident in the superior vermis, inferior vermis, and cerebellar hemisphere, along with loss of granule cells [16]. Findings from Gomez et al. include atrophy of anterior and posterior vermis, gliotic fastigial and dentate nuclei, loss of Purkinje cells in flocculus and anterior cerebellar hemisphere, and involvement of the cerebellar tonsils [17]. T2-weighted and FLAIR MRI show high signals in middle cerebellar peduncles, possibly due to degeneration and demyelination of pontocerebellar tracts [18, 19]. Results of positron emission tomography (PET) have also shown hypometabolism in the cerebellar hemispheres, brainstem, basal ganglia, and frontal, temporal, and occipital cortices [2]. Atrophy of the vermis may impact blood flow via the fastigial nucleus (which connects the vermis to the cortex and brainstem), resulting in hypoperfusion and hypometabolism [2, 20]. Finally, the middle cerebellar peduncles have shown mildly reduced diameter on MRI [21].
Motor Cortex
Findings from Gierga et al. concluded that the primary motor cortex of studied SCA6 patients showed depletion/shrinkage of imperforate giant Betz pyramidal cells [3]. This explains the prolonged central motor conduction time and pyramidal signs (spasticity, increased stretch reflexes, and positive Babinski sign). More specifically, the allocortical transentorhinal and entorhinal regions in the prealpha layers showed neuronal loss in all three patients studied, yet this was attributed to early cortical Alzheimer’s disease–related cytoskeletal pathology [3]. Betz cells make up the largest portion of neurons in the central nervous system and are primarily responsible for sending information down via the corticospinal tract. In addition to their apical dendrite, they have multiple dendritic shafts, which branch out and relay information to a vast array of nearby cells and neurons. Therefore, it is not a surprise that SCA6 subtype presents with some of the earliest motor symptoms and has the longest disease duration of all types of SCA.
Thalamus
From Gierga et al., thalamic neuronal loss was noted in the somatosensory ventral posterior lateral nucleus (VPL) and visual lateral and inferior subnuclei of the pulvinar nucleus in the patient with the earliest onset of disease and longest duration of those included in the study [3]. The pulvinar nuclei are thought to have roles in visual attention as well as integrating visual and oculomotor signals [22,23,24]. Thalamic degeneration in SCA6 is significantly less severe than in SCA1, SCA2, and SCA3 [5].
Midbrain
From Gierga et al., the patient described above with thalamic neuronal loss also displayed neurodegenerative changes in the oculomotor nuclei, red nuclei, and anterolateral/anterointermediate subnuclei of the pars compacta [3]. Changes in the substantia nigra can help explain Parkinsonian symptoms seen in SCA6 patients. Gomez et al. showed gliosis in periaqueductal grey matter, midbrain tectum, dorsal tegmentum, and red nuclei, but no neuronal loss [17]. The dorsal motor nuclei of the vagus nerve were the only cranial nerve to show gliosis [17]. MRI studies have also shown decreased diameter of the red nuclei [21].
Pons and Medulla
The pons of SCA6 patients has shown mildly decreased anteroposterior diameter on MRI [21]. Neurodegenerative changes are seen in vestibular (superior, lateral, interstitial, medial), oculomotor abducens, auditory (lateral lemniscus and superior olive), ingestion-related (mesencephalic, motor and spinal trigeminal, facial, hypoglossal, ambiguus, parvocellular reticular and solitary), precerebellar inferior olive, external cuneate, and cuneate nuclei [3]. In reference to the inferior olivary nuclei, a study by Ishikawa et al. specifically exhibited loss in the dorsomedial region [16]. Wang et al. showed loss and gliosis of the inferior olivary nucleus distally [15]. Gomez et al. showed neuronal loss and astrocytosis of the accessory and inferior olivary nuclei and dense gliosis in the vestibular nuclei [17]. Changes to these nuclei in the pons and medulla are manifested in symptoms such as palsy of the abducens nerve and the lateral rectus muscle, optokinetic and horizontal gaze-evoked nystagmus, a history of easy falls, and incoordination of arm movements [3]. Study of SCA6 patients by Rüb et al. found defects in the ingestion and lingual phases of swallowing, likely due to degeneration within ingestion-related nuclei [8].
Spinal Cord
Wang et al. showed severe to moderate loss of motor neurons in the anterior horn (manifesting with muscle weakness) and intermediolateral nucleus (manifesting with autonomic signs) of the intumescentia lumbalis by immunohistochemical staining [15]. Patients examined by Gomez et al. showed degeneration of both corticospinal tracts with macrophage infiltrates, gliosis, and occasional axonal spheroids and myelin ovoids [17].
Presentation and Symptoms of SCA6
Although neuronal loss in SCA6 is not as severe as in subtypes SCA1-3 and 7, it still imposes discomposure in the life of an affected individual. The first symptoms of SCA6 are usually an unsteady gait, stumbling, and imbalance, which may present anywhere from 16 to 72 years old, with a mean age 45 years old [25]. Alternately, there are reported cases of diplopia, dysarthria, vertigo, and leg pain as being the earliest presenting symptoms [25, 26]. SCA6 progresses slowly, with all patients generally developing gait ataxia (rarely episodic ataxia), upper-limb incoordination, intention tremor, and dysarthria. Other symptoms include difficulties swallowing (dysphagia and choking), visual impairment (diplopia, difficulty fixating on moving objects, various types of nystagmus, impaired smooth pursuit, abnormal vestibulo-ocular reflex), hyperreflexia, extensor plantar responses, peripheral neuropathy, basal ganglia signs (dystonia and blepharospasm), Parkinsonism, cognitive impairment with preserved mentation, myoclonus, depression, and fatigue [17, 25,26,27]. The vestibulo-ocular reflex (VOR) is usually reduced or absent in autosomal dominant SCAs, yet it has been found to be hyperactive in SCA6 [17]. In patients with an older onset of SCA6, which is also associated with shorter triplet repeats, the onset and clinical course of dysphagia was noted to be more severe than those patients with an earlier, more insidious onset of SCA6 symptoms [28]. As the disease manifestations of SCA6 progress, videofluoroscopic examination of swallowing is recommended to prevent aspiration in these patients. Notably, among a cohort of 30 SCA patients, the neurological impairments associated with the disease led to a reduction in chewing movements, changes in the oral phase of swallowing, and in some patients, leftover food residue in the epiglottic vallecular on initial swallow, increasing the risk for aspiration [29]. While the challenges and dangerous implications of these extra-neurological manifestations of SCA are well known, on a recent systematic review, there have been no known randomized clinical trials of dysphagia interventions in hereditary ataxias, opening the door for further research on the medical management of these issues [30].
Diagnosis of SCA6
In the pregenetic era, autosomal dominant cerebellar ataxias (ADCA) were grouped into three subtypes, with SCA6 falling within Type III (originally categorized by purely cerebellar symptoms). The classification system is important because Type III generally have better prognosis and are easier to diagnose without genetic testing [25]. Of the ADCAs, SCA6 represents about 13% prevalence, varying by geographical area [25, 31]. Unfortunately, there is no cure for spinocerebellar ataxias, and management is supportive, including exercise, medications, computer devices, and mechanical aids [27]. Further research is being performed on the possible implementation of gene and stem cell therapy for treatment [25].
While there are no formal diagnostic criteria for the SCAs, the diagnosis of SCA6 is based on molecular genetic testing [25, 27]. Clinical and family histories, a thorough physical exam, and imaging (particularly with MRI) can aid in diagnosis, especially when ruling out ataxia due to another cause. Generally, if a patient presents with purely cerebellar symptoms in a population where prevalence of SCA6 is high (such as in Japan or USA), genetic testing for SCA6 should be done first. If the prevalence is low, a head MRI should be done. If the MRI shows pons atrophy, then genetic testing should be performed to elucidate the subtype of SCA present; if there is no pons atrophy, alternate testing for other subtypes should be done [25]. Genetic testing of the CACNA1A gene searches for CAG repeats with a sensitivity and specificity of 100% either as a single-gene test or as a multi-gene panel to look for similar conditions [32]. The test considers less than 18 CAG repeats to be normal and between 20 and 33 repeats to be full penetrance alleles with symptoms expected to develop sometime within one’s lifetime. 19 CAG repeats are of questionable significance as asymptomatic and symptomatic cases have been reported [32]. Predictive testing is available for at-risk asymptomatic individuals and prenatal diagnosis/preimplantation genetic diagnosis for at-risk pregnancies [27].
The advent of genetic testing has significantly altered the knowledge base on spinocerebellar ataxias and has rapidly increased the pace of research into this class of diseases. Further work in the field of SCA should be directed to the understanding the progression of neurological changes, either on the macroscopic scale through atrophy or through histological examination and additional ways to predict, prevent, and treat symptoms to lead to better patient quality of life.
Treatment
Currently, there are no specific treatments for spinal cerebellar ataxias, thus therapy is aimed at treating the symptoms. Reduction of ataxia can be accomplished with acetazolamide, while the issue of balance can be addressed with a combination of walkers, canes, assisted devices, and physical therapy exercises that target core strength. Efforts should be made to increase the patient’s independence and quality of life. It is important to encourage healthy eating and weight loss to prevent obesity and subsequent mobility issues. Vestibular symptoms may be managed with medications such as diphenhydramine, gabapentin, and baclofen. 4-aminopyridine may treat nystagmus as well as vestibular symptoms. Dysarthria may be improved with speech therapy and communication devices. Patients should follow up annually with physiatrists and physical therapy for continual review of need for walking aids or home adaptations. Referrals for nutrition evaluation or feeding assessments as well as video esophagography should be done as needed. Sedative hypnotics and alcohol should be avoided as they can further decrease coordination and increase risk of falls [27].
Research is ongoing on potential future treatment options involving RNAi. Using miRNA to knock out the CACNA1A gene in mice models has shown to cause death within weeks due to the loss of the calcium channel receptor required for cell nerve function. However, the CACNA1A gene has been shown to produce a second protein known as α1ACT, which enhances neuronal growth, while mutations lead to neuronal death. Using miRNA to knock out the mutated α1ACT gene has shown to prevent development of SCA6. This model maybe useful not only in curing SCA6 but other bicistronic genes in the future [33].
References
OMIM Phenotypic Series - PS164400 - Spinocerebellar Ataxias [Internet]. [cited 2019 Oct 29]. Available from: https://omim.org/phenotypicSeries/PS164400
Soong B, Liu R, Wu L, Lu Y, Lee H. Metabolic characterization of spinocerebellar ataxia type 6. Arch Neurol. 2001;58(2):300–4.
Gierga K, Schelhaas HJ, Brunt ER, Seidel K, Scherzed W, Egensperger R, et al. Spinocerebellar ataxia type 6 (SCA6): neurodegeneration goes beyond the known brain predilection sites. Neuropathol Appl Neurobiol. 2009;35(5):515–27.
Schulz JB, Borkert J, Wolf S, Schmitz-Hübsch T, Rakowicz M, Mariotti C, et al. Visualization, quantification and correlation of brain atrophy with clinical symptoms in spinocerebellar ataxia types 1, 3 and 6. NeuroImage. 2010;49(1):158–68.
Seidel K, Siswanto S, Brunt ERP, den Dunnen W, Korf H-W, Rüb U. Brain pathology of spinocerebellar ataxias. Acta Neuropathol (Berl). 2012;124(1):1–21.
Frontali M. Spinocerebellar ataxia type 6: channelopathy or glutamine repeat disorder? Brain Res Bull. 2001;56(3):227–31.
Ishikawa K, Owada K, Ishida K, Fujigasaki H, Shun Li M, Tsunemi T, et al. Cytoplasmic and nuclear polyglutamine aggregates in SCA6 Purkinje cells. Neurology. 2001;56(12):1753–6.
Rüb U, Brunt ER, Petrasch-Parwez E, Schöls L, Theegarten D, Auburger G, et al. Degeneration of ingestion-related brainstem nuclei in spinocerebellar ataxia type 2, 3, 6 and 7. Neuropathol Appl Neurobiol. 2006;32(6):635–49.
Tsou W-L, Qiblawi SH, Hosking RR, Gomez CM, Todi SV. Polyglutamine length-dependent toxicity from α1ACT in Drosophila models of spinocerebellar ataxia type 6. Biol Open. 2016;5(12):1770–5.
Orr HT, Zoghbi HY. Trinucleotide repeat disorders. Annu Rev Neurosci. 2007;30(1):575–621.
Hillman D, Chen S, Aung TT, Cherksey B, Sugimori M, Llinás RR. Localization of P-type calcium channels in the central nervous system. Proc Natl Acad Sci U S A. 1991;88(16):7076–80.
Kordasiewicz HB, Thompson RM, Clark HB, Gomez CM. C-termini of P/Q-type Ca 2+ channel α1A subunits translocate to nuclei and promote polyglutamine-mediated toxicity. Hum Mol Genet. 2006;15(10):1587–99.
Sakahira H, Breuer P, Hayer-Hartl MK, Hartl FU. Molecular chaperones as modulators of polyglutamine protein aggregation and toxicity. Proc Natl Acad Sci U S A. 2002;99(Suppl 4):16412–8.
Reference GH. CACNA1A gene [Internet]. Genetics Home Reference. [cited 2020 Jan 13]. Available from: https://ghr.nlm.nih.gov/gene/CACNA1A
Wang X, Wang H, Xia Y, Jiang H, Shen L, Wang S, et al. A neuropathological study at autopsy of early onset spinocerebellar ataxia 6. J Clin Neurosci. 2010;17(6):751–5.
Ishikawa K, Watanabe M, Yoshizawa K, Fujita T, Iwamoto H, Yoshizawa T, et al. Clinical, neuropathological, and molecular study in two families with spinocerebellar ataxia type 6 (SCA6). J Neurol Neurosurg Psychiatry. 1999;67(1):86–9.
Gomez CM, Thompson RM, Gammack JT, Perlman SL, Dobyns WB, Truwit CL, et al. Spinocerebellar ataxia type 6: gaze-evoked and vertical nystagmus, Purkinje cell degeneration, and variable age of onset. Ann Neurol. 1997;42(6):933–50.
Riva A, Bradac GB. Primary cerebellar and spino-cerebellar ataxia an MRI study on 63 cases. J Neuroradiol J Neuroradiol. 1995;22:71–6.
Nakagawa N, Katayama T, Makita Y, Kuroda K, Aizawa H, Kikuchi K. A case of spinocerebellar ataxia type 6 mimicking olivopontocerebellar atrophy. Neuroradiology. 1999;41(7):501–3.
Elliott MA, Peroutka SJ, Welch S, May EF. Familial hemiplegic migraine, nystagmus, and cerebellar atrophy. Ann Neurol. 1996;39(1):100–6.
Murata Y, Kawakami H, Yamaguchi S, Nishimura M, Kohriyama T, Ishizaki F, et al. Characteristic magnetic resonance imaging findings in spinocerebellar ataxia 6. Arch Neurol. 1998;55(10):1348–52.
Grieve KL, Acuña C, Cudeiro J. The primate pulvinar nuclei: vision and action. Trends Neurosci. 2000;23(1):35–9.
Shipp S. The functional logic of cortico-pulvinar connections. Philos Trans R Soc B Biol Sci. 2003;358(1438):1605–24.
Arend I, Machado L, Ward R, McGrath M, Ro T, Rafal RD. Chapter 5.15 - The role of the human pulvinar in visual attention and action: evidence from temporal-order judgment, saccade decision, and antisaccade tasks. In: Kennard C, Leigh RJ, editors. Progress in Brain Research [Internet]: Elsevier; 2008. [cited 2019 Oct 21]. p. 475–83. (Using Eye Movements as an Experimental Probe of Brain Function; vol. 171). Available from: http://www.sciencedirect.com/science/article/pii/S0079612308006699.
Fujioka S, Sundal C, Wszolek ZK. Autosomal dominant cerebellar ataxia type III: a review of the phenotypic and genotypic characteristics. Orphanet J Rare Dis. 2013;8:14.
Stevanin G, Dürr A, David G, Didierjean O, Cancel G, Rivaud S, et al. Clinical and molecular features of spinocerebellar ataxia type 6. Neurology. 1997;49(5):1243–6.
Casey HL, Gomez CM. Spinocerebellar ataxia type 6. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Stephens K, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington; 1993. [cited 2020 Jan 13]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK1140/.
Isono C, Hirano M, Sakamoto H, Ueno S, Kusunoki S, Nakamura Y. Progression of dysphagia in spinocerebellar ataxia type 6. Dysphagia. 2017;32(3):420–6.
Abdulmassih EM d S, Teive HAG, Santos RS. The evaluation of swallowing in patients with spinocerebellar ataxia and oropharyngeal dysphagia: a comparison study of videofluoroscopic and sonar doppler. Int Arch Otorhinolaryngol. 2013;17(1):66–73.
Vogel AP, Keage MJ, Johansson K, Schalling E. Treatment for dysphagia (swallowing difficulties) in hereditary ataxia. Cochrane Database Syst Rev [Internet]. 2015;11 [cited 2019 Oct 21] Available from: http://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010169.pub2/full.
Schöls L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004;3(5):291–304.
Comprehensive ataxia repeat expansion panel (SCA 1, 2, 3, 6, 7, 8, 10, 12, 17, 36, DRPLA & FRDA) - Tests - GTR - NCBI [Internet]. [cited 2020 Jan 13]. Available from: https://www.ncbi.nlm.nih.gov/gtr/tests/567650/overview/
Miyazaki Y, Du X, Muramatsu S, Gomez CM. An miRNA-mediated therapy for SCA6 blocks IRES-driven translation of the CACNA1A second cistron. Sci Transl Med. 2016;8(347):347ra94–4.
Author information
Authors and Affiliations
Contributions
Zubir Rentiya: Article idea, literature search, article draft
Robert Hutnik: Literature search, article critical revision
Yolunna Q Mekkam: Literature search, article critical revision
Junun Bae: Article idea, literature search, article draft
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rentiya, Z., Hutnik, R., Mekkam, Y.Q. et al. The Pathophysiology and Clinical Manifestations of Spinocerebellar Ataxia Type 6. Cerebellum 19, 459–464 (2020). https://doi.org/10.1007/s12311-020-01120-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-020-01120-y