Abstract
Spinocerebellar ataxias (SCAs) are characterized by autosomal dominantly inherited progressive ataxia but are clinically heterogeneous due to variable involvement of non-cerebellar parts of the nervous system. Non-cerebellar symptoms contribute significantly to the burden of SCAs, may guide the clinician to the underlying genetic subtype, and might be useful markers to monitor disease. Peripheral neuropathy is frequently observed in SCA, but subtype-specific features and subclinical manifestations have rarely been evaluated. We performed a multicenter nerve conduction study with 162 patients with genetically confirmed SCA1, SCA2, SCA3, and SCA6. The study proved peripheral nerves to be involved in the neurodegenerative process in 82 % of SCA1, 63 % of SCA2, 55 % of SCA3, and 22 % of SCA6 patients. Most patients of all subtypes revealed affection of both sensory and motor fibers. Neuropathy was most frequently of mixed type with axonal and demyelinating characteristics in all SCA subtypes. However, nerve conduction velocities of SCA1 patients were slower compared to other genotypes. SCA6 patients revealed less axonal damage than patients with other subtypes. No influence of CAG repeat length or biometric determinants on peripheral neuropathy could be identified in SCA1, SCA3, and SCA6. In SCA2, earlier onset and more severe ataxia were associated with peripheral neuropathy. We proved peripheral neuropathy to be a frequent site of the neurodegenerative process in all common SCA subtypes. Since damage to peripheral nerves is readily assessable by electrophysiological means, nerve conduction studies should be performed in a longitudinal approach to assess these parameters as potential progression markers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinocerebellar ataxias (SCAs) comprise a group of hereditary neurodegenerative disorders with progressive ataxia as key symptom (for review see [1]). Beside this hallmark of the disease, SCA presents with variable phenotypes due to differential involvement of non-cerebellar parts of the nervous system. Hereby, phenotypic differences have been observed between as well as within specific genotypes.
Spinocerebellar ataxias type 1, 2, 3, and 6 are the worldwide most prevalent subtypes and share CAG repeat expansions in coding regions of the respective genes as a common disease mechanism [1, 2]. Although the genetic basis is known for more than a decade, no cure is available for these slowly progressive and severely disabling diseases. Substantial progress has been made to assess the severity of ataxia, non-cerebellar involvement, and progression rate of SCAs using semi-quantitative clinical rating scales, yet quantitative measures and progression markers are widely missing [3–7].
Peripheral nerves are readily assessable by nerve conduction studies in an objective and quantitative manner. Additionally, peripheral neuropathy is reported to be a frequent non-cerebellar affection in SCA, although large series are scarce. In a joint European project on spinocerebellar ataxias (EUROSCA), we set out to determine the frequency and neurophysiological characteristics of peripheral neuropathy in these four most common SCA subtypes and to analyze nerve conduction parameters as potential biomarkers in SCA.
Patients and Methods
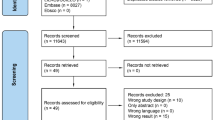
A total of 162 patients with a mutation in the SCA1, 2, 3, or 6 genes (aged 48 ± 14 years, range 18–81) and 79 healthy controls (aged 44 ± 14 years, range 20–77) were recruited in seven centers (Departments of Neurology of University Clinics in Bochum, Bonn, Brussels, Nijmegen, Santander, Tuebingen, and Warsaw) participating in the EUROSCA project (http://www.eurosca.org). All patients and controls gave their written informed consent prior to inclusion. The study was approved by the Ethics Committees of the participating centers. Patients underwent a clinical and electrophysiological examination.
Clinical examination assessed disease severity by the Scale for the Assessment and Rating of Ataxia (SARA; [3]) and the Inventory of Non-Ataxia Symptoms (INAS; [6]). SARA is a semi-quantitative assessment of the impairment level including eight items (gait, stance, sitting, speech disturbance, finger chase, nose-finger test, fast alternating hand movement; and heel-shin slide). The semi-quantitative INAS consists of 30 items, related to areflexia, hyperreflexia, extensor plantar response, spasticity, paresis, amyotrophy, fasciculations, myoclonus, rigidity, chorea, dystonia, resting tremor, sensory symptoms, brainstem oculomotor signs (horizontal and vertical ophthalmoparesis, slowing of saccades), urinary dysfunction, and cognitive impairment. Detailed demographic and clinical characteristics of the SCA population are shown in Table 1.
Neuropathy by clinical means was assumed by the presence of areflexia, atrophy, fasciculation, and/or impaired vibration sense (≤5/8).
Nerve conduction studies included ulnar and tibial nerves for motor assessment and radial and sural nerves for sensory fibers. Nerve conduction studies were performed according to a standardized protocol throughout centers. As a measure of quality control, recordings of 10 healthy controls (2 per decade, age 20–70 years) were performed by each participant and compared between centers. To assure comparability of neurophysiological procedures further, centers with major discrepancies from the reference center in Tuebingen were visited by the coordinator to perform exemplary measurements together with the local neurophysiologist.
Stimulation and recording were performed by surface electrodes. In motor nerves, stimulus intensity was increased in 5-mA steps to maximum response starting with a standard stimulus duration of 0.2 ms. If supramaximal stimulation could not be reached by maximum current, stimulus duration was increased by steps of 0.1 ms. For the tibial nerve, recordings were performed from the abductor hallucis muscle with distal stimulation 7 cm proximal to recording electrodes and proximal stimulation at the hollow of the knee. Minimal F-wave latency was assessed from 20 recordings. The ulnar nerve was recorded from the abductor digiti minimi muscle. Distal stimulation was performed 5 cm proximal to recording electrodes at the wrist. Proximal stimulations were performed at the elbow (1) distal and (2) proximal of the sulcus ulnaris. Distal motor latency (DL), compound muscle action potential (CMAP), motor nerve conduction velocity (MNCV), and minimal F-wave latency (F) were assessed. CMAP amplitudes were measured peak to peak.
Sensory recordings from the sural and radial nerve were performed in antidromic technique. For the sural nerve, the active electrode was placed above the nerve at the external malleolus with the reference electrode 3 cm distally at the lateral side of the foot. Stimulation was performed with standard intensity of 20 mA at the mid-calf, 14 cm proximal to recording electrodes. Skin temperature was controlled and adjusted to 34 °C using heating. For recordings of the radial nerve, the active electrode was placed over the first dorsal spatium interosseum with the indifferent electrode 3 cm distally in direction to the index finger. Stimulation was performed at the radial forearm, 15 cm proximally to the recording electrode with a stimulus intensity of 20 mA. Sensory nerve action potential (SNAP) and sensory nerve conduction velocity (SNCV) were assessed. SNAP amplitudes were measured from baseline to peak. In general, right-sided nerves were recorded; in case of trauma, nerve biopsy, or pitting edema, the less affected side was chosen.
Each electrophysiological parameter was modeled in a group of healthy controls to determine thresholds from which abnormal values can be defined, taking into account center and physiological age effects. It is well known that nerve conduction parameters are dependent on age. Mixed effect models were used with “age” as fixed effect, “center” as fixed covariate, and random effects for all parameters. Z-scores were calculated for each parameter for every patient as the subtraction between the observed and the expected parameter divided by the standard error of the residuals of the models. In the control patient group, 95 % of the Z-scores were expected between −1.96 and +1.96, with a mean of 0 and a standard deviation of 1. Z-scores were considered abnormal if lower than −1.96 for CMAP amplitudes, SNAP amplitudes, MNCV, and SNCV and higher than 1.96 for DL and F. Tibial and ulnar nerves were considered abnormal if CMAP, MNCV, DL, or F was abnormal. Sural and radial nerves were considered abnormal if SNAP or SNCV was abnormal. A patient was diagnosed with neuropathy if parameters were abnormal for at least two nerves.
Neuropathy was defined as axonal if CMAP and SNAP were abnormal. Neuropathy was considered demyelinating if DML, MNCV, SNCV. or F was abnormal. Mixed neuropathy was diagnosed as a mixture of the preceding.
Electrophysiologically defined motor (respectively sensory) neuropathy was diagnosed if both motor nerves (respectively both sensory nerves) were abnormal but sensory (respectively motor) recordings presented normal results. Sensorimotor neuropathy was defined if at least one motor and one sensory nerve were abnormal.
Fisher exact test was used to compare differences of qualitative variables between SCA subtypes. Occurrence of electrophysiologically defined neuropathy was modeled using a logistic regression with gender, age, age at onset of the disease, duration of the disease, INAS count, SARA score, disease stage, and shorter CAG repeat length or longer CAG repeat length as explanatory covariates. Complete data were extracted in each SCA group, and the covariates were first studied in univariate logistic regression models. When effect sizes were sufficient (SCA2 and 3), the covariates with a p value <0.30 (Wald test for associated parameter) were proposed in a multivariate logistic regression model forward selection procedure.
Group (SCA1, 2, 3, and 6) comparisons of Z-scores (differences of least squares means) were performed with analysis of variance and Tukey-Kramer adjustment of p values.
Results
Clinically defined neuropathy was most abundant in SCA2 patients (92 %) followed by SCA3 (84 %) and SCA1 (77 %) and less frequent in SCA6 patients (69 %). Differences between genotypes failed to reach significance (Fisher exact test, p = 0.064).
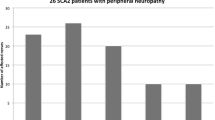
Electrophysiologically defined neuropathy was most frequent in SCA1 patients (82 %) followed by SCA2 (63 %) and SCA3 (55 %). Only 22 % of the SCA6 patients fulfilled electrophysiological criteria of peripheral neuropathy (Fisher exact test, p < 0.001, Fig. 1). The proportion of neuropathy was significantly lower in SCA6 patients than in SCA1 (p < 0.001), SCA2 (p = 0.0016), and SCA3 (p = 0.005) patients and was significantly higher in SCA1 than in SCA3 patients (p = 0.0076). These comparisons lead to the same conclusion after Bonferroni correction. Agreement between clinically and electrophysiologically defined neuropathy was reached in 57 % of patients.
Frequency of neuropathy by electrophysiological means in different SCA subtypes. Data are shown as percent. For criteria of electrophysiologically defined neuropathy, see the “Patients and Methods” section
Electrophysiologically defined neuropathies were further classified as axonal, demyelinating, and mixed neuropathy. Frequency of these types of neuropathy differed between genotypes (Fig. 2).
Distribution of neuropathies (axonal, demyelinating, and mixed) by electrophysiological means in different SCA subtypes. For criteria of different forms of neuropathy, see the “Patients and Methods” section
Analysis of sensory and motor nerve affection revealed sensorimotor neuropathy as the by far most common form in all SCA genotypes, ranging from 94 % in SCA1 to 69 % in SCA3 patients (Fig. 3) with no statistical differences between SCA type (Fisher exact test, p = 0.10).
Distribution of motor, sensory, and sensorimotor neuropathy by electrophysiological means in different SCA subtypes. For criteria of different forms of neuropathy, see the “Patients and Methods” section
Potential determinants of the appearance of electrophysiologically defined neuropathy were investigated by employing a logistic regression analysis. The only significant determinants in univariate analyses were the SARA score in SCA2 patients with an odds ratio of 1.17 [1.03; 1.34] per each additional point for the SARA score and age of onset with an odds ratio of 0.94 [0.88; 0.99] (Table 2). Multivariate analysis for SCA2 and SCA3 data did not pinpoint any additional statistically significant explanatory covariates. In order to avoid unreliable results due to overfitting, a multivariate analysis could not be performed for SCA1 and SCA6 patients due to the small number of SCA1 patients without neuropathy and SCA6 patients with neuropathy.
Table 3 summarizes the Z-scores of nerve conduction parameters for SCA1, 2, 3, and 6. Group comparisons of Z-scores with ANOVA followed by Tukey-Kramer adjustment of p values for significant post hoc comparisons revealed slower nerve conduction velocities of SCA1 patients compared to patients with other genotypes (Fig. 4). As expected from slower nerve conduction velocities, F wave latencies were longer in SCA1 than in other subtypes in the ulnar nerve (p < 0.0001 for all genotypes) as well as the tibial nerve (SCA1 vs SCA2, p < 0001; SCA1 vs SCA3, p = 0.0002; SCA1 vs SCA6, not significant). Interestingly, distal latencies did not differ between genotypes neither in the ulnar nor in the tibial nerve. Moreover, SCA6 patients revealed less axonal neuropathy in lower extremities than patients with other subtypes (p ≤ 0.01 for sural SNAP and tibial CMAP in comparison of SCA6 versus SCA1, SCA2, and SCA3; Table 3).
Z-scores of nerve conduction velocities (mean and standard deviation) in SCA1, 2, 3, and 6. For abbreviations, see the “Patients and Methods” section. Group (SCA1, 2, 3, and 6) comparisons of Z-scores (differences of least squares means) were performed with analysis of variance and Tukey-Kramer adjustment of p values (*** adjusted p < 0.005 and * adjusted p < 0.05). Error bars indicate standard deviation
Discussion
Peripheral neuropathy is frequent in all common subtypes of spinocerebellar ataxias. In this large European study, we found electrophysiological evidence for the affection of the peripheral nervous system in the majority of SCA patients. This is consistent with earlier studies in several substantially smaller cohorts published for single genotypes [8–19]. A strength of our multicenter approach is that we were able to recruit representative cohorts of all common SCA genotypes and to compare neurophysiological parameters across genotypes. However, the involvement of centers in several European countries required specific analyses including Z-score statistics to consider center effects.
We found nerve conduction velocities of SCA1 patients to be slower compared to those of the other genotypes. This was especially prominent in motor nerves (Table 3 and Fig. 4). Second, SCA6 patients revealed less axonal neuropathy than patients with other subtypes especially in sensory and motor nerves of lower extremities. This matches with earlier studies [20] and the notion that SCA6 is rather a “pure” type of cerebellar degeneration [16, 19] classified as ADCA type III according to Harding [21] whereas SCA1, 2, and 3 frequently present with non-cerebellar affection qualifying for ADCA type I.
Nerve conduction studies allow quantification of peripheral nerve involvement in a non-invasive, readily available, and repeatable test. This suggests nerve conduction studies as quantitative parameters for the assessment of disease severity and disease progression in SCA. In this respect, it is of importance that in accordance with the literature [22], not only a small subgroup but also the majority of SCA patients presented with electrophysiological abnormalities. It may be speculated that even patients with normal values in the present evaluation may develop abnormalities when the disease progresses.
At the first glance, the rather poor agreement of clinical and electrophysiological diagnoses of peripheral nervous system involvement is unexpected. However, given the multisystem involvement in SCA1, 2, and 3, clinical signs of peripheral neuropathy may find alternative explanations. For example, sensory loss may be caused by dorsal column pathology rather than peripheral nerve affection. Similarly, muscle atrophy may be secondary to inactivity or lower motor neuron affection rather than affection of the peripheral nerves [1, 23]. Additionally, nerve conduction studies do not necessarily depict the fibers of peripheral nerves that are responsible for clinical symptoms and especially sensory deficits. While nerve conduction studies primarily assess the largest, myelinated fibers, sensory symptoms may derive from thin or unmyelinated fibers that escape standard nerve conduction studies. Histopathological studies of peripheral nerves in genetically defined SCA cases are scarce and depicted reduction in density of myelinated and unmyelinated fibers and loss of large myelinated fibers and distal axonopathy with relative hypomyelination in SCA3 but with substantial interindividual variability [24–27].
One shortcoming of this study is that it did not look for neuronopathy in discrimination to distal peripheral neuropathy [20]. Such differentiation would have required needle EMG that is even more difficult to standardize in a multicenter setting than nerve conduction studies and is likely to reduce compliance of patients due to pain associated with the procedure.
Apart from an association of disease severity and age at onset in SCA2, we largely failed to identify significant determinants of peripheral nerve involvement in univariate logistic regression analysis taking into account CAG repeat length, gender, age at onset, disease duration, age, and disease severity. In this multicenter approach, we could not confirm a study in German SCA3 patients that found CMAP and SNAP amplitudes to be determined by age [28] and a study in Cuban SCA2 patients describing SNAP amplitudes of sural nerve to correlate with disease duration and disease severity as assessed by the International Cooperative Ataxia Rating Scale (ICARS) [29]. This may be explained by larger variability in our study due to multiple centers involved and a broad ethnical background. Our findings are in agreement with a Dutch study that did not observe an influence of age, disease duration, or ataxia severity as well [20]. This study and our findings establish peripheral neuropathy as an independent manifestation of the disease process in SCA. Whether electrophysiological parameters in nerve conduction studies are suitable surrogate markers to monitor disease progression is questionable given the poor correlation with severity of ataxia as assessed by SARA. This issue requires prospective data from longitudinal electrophysiological assessment for a definitive answer.
Conclusion
Our study proves peripheral neuropathy as a frequent manifestation in spinocerebellar ataxias type 1, type 2, and type 3. In contrast, neuropathy is less prominent in SCA6. Furthermore, neuropathy is different in SCA1 compared to other genotypes in that it goes along with substantially slowed nerve conduction. Longitudinal studies are needed to further evaluate electrophysiological parameters as biomarkers for disease progression that may be assessable in interventional trials in SCA in the future.
References
Schols L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004;3(5):291–304.
Durr A. Autosomal dominant cerebellar ataxias: polyglutamine expansions and beyond. Lancet Neurol. 2010;9(9):885–94.
Schmitz-Hubsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006;66(11):1717–20.
Schmitz-Hubsch T, Fimmers R, Rakowicz M, Rola R, Zdzienicka E, Fancellu R, et al. Responsiveness of different rating instruments in spinocerebellar ataxia patients. Neurology. 2010;74(8):678–84.
Schmitz-Hubsch T, Giunti P, Stephenson DA, Globas C, Baliko L, Sacca F, et al. SCA functional index: a useful compound performance measure for spinocerebellar ataxia. Neurology. 2008;71(7):486–92.
Schmitz-Hubsch T, Coudert M, Bauer P, Giunti P, Globas C, Baliko L, et al. Spinocerebellar ataxia types 1, 2, 3, and 6: disease severity and nonataxia symptoms. Neurology. 2008;71(13):982–9.
Jacobi H, Bauer P, Giunti P, Labrum R, Sweeney MG, Charles P, et al. The natural history of spinocerebellar ataxia type 1, 2, 3, and 6: a 2-year follow-up study. Neurology. 2011;77(11):1035–41.
Burk K, Stevanin G, Didierjean O, Cancel G, Trottier Y, Skalej M, et al. Clinical and genetic analysis of three German kindreds with autosomal dominant cerebellar ataxia type I linked to the SCA2 locus. J Neurol. 1997;244(4):256–61.
Crum BA, Josephs KA. Varied electrophysiologic patterns in spinocerebellar ataxia type 2. Eur J Neurol. 2006;13(2):194–7.
Kubis N, Durr A, Gugenheim M, Chneiweiss H, Mazzetti P, Brice A, et al. Polyneuropathy in autosomal dominant cerebellar ataxias: phenotype-genotype correlation. Muscle Nerve. 1999;22(6):712–7.
Kumagai R, Kaseda Y, Kawakami H, Nakamura S. Electrophysiological studies in spinocerebellar ataxia type 6: a statistical approach. Neuroreport. 2000;11(5):969–72.
Malandrini A, Galli L, Villanova M, Palmeri S, Parrotta E, DeFalco D, et al. CAG repeat expansion in an italian family with spinocerebellar ataxia type 2 (SCA2): a clinical and genetic study. Eur Neurol. 1998;40(3):164–8.
Nagai Y, Azuma T, Funauchi M, Fujita M, Umi M, Hirano M, et al. Clinical and molecular genetic study in seven Japanese families with spinocerebellar ataxia type 6. J Neurol Sci. 1998;157(1):52–9.
Perretti A, Santoro L, Lanzillo B, Filla A, De Michele G, Barbieri F, et al. Autosomal dominant cerebellar ataxia type I: multimodal electrophysiological study and comparison between SCA1 and SCA2 patients. J Neurol Sci. 1996;142(1–2):45–53.
Ueyama H, Kumamoto T, Nagao S, Mita S, Uchino M, Tsuda T. Clinical and genetic studies of spinocerebellar ataxia type 2 in Japanese kindreds. Acta Neurol Scand. 1998;98(6):427–32.
Schols L, Kruger R, Amoiridis G, Przuntek H, Epplen JT, Riess O. Spinocerebellar ataxia type 6: genotype and phenotype in German kindreds. J Neurol Neurosur Ps. 1998;64(1):67–73.
Schols L, Riess O, Schols S, Zeck S, Amoiridis G, Langkafel M, et al. Spinocerebellar ataxia type 1: clinical and neurophysiological characteristics in German kindreds. Acta Neurol Scand. 1995;92(6):478–85.
Abele M, Burk K, Andres F, Topka H, Laccone F, Bosch S, et al. Autosomal dominant cerebellar ataxia type I. Nerve conduction and evoked potential studies in families with SCA1, SCA2 and SCA3. Brain. 1997;120(12):2141–8.
Schols L, Amoiridis G, Buttner T, Przuntek H, Epplen JT, Riess O. Autosomal dominant cerebellar ataxia: phenotypic differences in genetically defined subtypes? Ann Neurol. 1997;42(6):924–32.
van de Warrenburg BP, Notermans NC, Schelhaas HJ, van Alfen N, Sinke RJ, Knoers NV, et al. Peripheral nerve involvement in spinocerebellar ataxias. Arch Neurol Chic. 2004;61(2):257–61.
Harding AE. Classification of the hereditary ataxias and paraplegias. Lancet. 1983;1(8334):1151–5.
Yadav R, Pal PK, Krishna N, Amar BR, Jain S, Purushottam M. Electrophysiological evaluation of spinocerebellar ataxias 1, 2 and 3. J Neurol Sci. 2012;312(1–2):142–5.
Durr A, Stevanin G, Cancel G, Duyckaerts C, Abbas N, Didierjean O, et al. Spinocerebellar ataxia 3 and Machado-Joseph disease: clinical, molecular, and neuropathological features. Ann Neurol. 1996;39(4):490–9.
Nakano KK, Dawson DM, Spence A. Machado disease. A hereditary ataxia in Portuguese emigrants to Massachusetts. Neurology. 1972;22(1):49–55.
Coutinho P, Guimaraes A, Pires MM, Scaravilli F. The peripheral neuropathy in Machado-Joseph disease. Acta Neuropathol. 1986;71(1–2):119–24.
Kinoshita A, Hayashi M, Oda M, Tanabe H. Clinicopathological study of the peripheral nervous system in Machado-Joseph disease. J Neurol Sci. 1995;130(1):48–58.
Lin KP, Soong BW. Peripheral neuropathy of Machado-Joseph disease in Taiwan: a morphometric and genetic study. Eur Neurol. 2002;48(4):210–7.
Klockgether T, Schols L, Abele M, Burk K, Topka H, Andres F, et al. Age related axonal neuropathy in spinocerebellar ataxia type 3/Machado-Joseph disease (SCA3/MJD). J Neurol Neurosurg Psychiatry. 1999;66(2):222–4.
Velazquez Perez L, Sanchez Cruz G, Canales Ochoa N, Rodriguez Labrada R, Rodriguez Diaz J, Almaguer Mederos L, et al. Electrophysiological features in patients and presymptomatic relatives with spinocerebellar ataxia type 2. J Neurol Sci. 2007;263(1–2):158–64.
Acknowledgments
The study was supported by a grant from the European Union (LSHM-CT-2004-503304) to EUROSCA.
Conflict of Interest
Dr. Linnemann reports no disclosures. Dr. Tezenas du Montcel received research support from the European Union (EU) EUROSCA. Dr. Rakowicz received research support from the EU EUROSCA and from the Polish Ministry of Science. Dr. Schmitz-Hübsch received research support from the EU EUROSCA. Dr. Szymanski received research support from the EU EUROSCA. Dr. Berciano received research support from the EU EUROSCA. Dr. van de Warrenburg received research support from the EU EUROSCA, from the Gossweiler Foundation, from the Radboud University Medical Center, and from BBMRI-NL. Dr. Depondt served on a scientific advisory board for UCB; has received funding for travel from Pfizer Inc; and received research support from the EU EUROSCA and from the Fonds National de la Recherche Scientifique (FNRS, Belgium). Dr. Rola received research support from the EU EUROSCA and from the Polish Ministry of Science. Dr. Klockgether received/receives research support from the EU EUROSCA, the German Research Foundation (DFG), and the German Federal Ministry of Education and Research (BMBF). Dr. Garcia received research support from the EU EUROSCA. Dr. Mutlu reports no disclosures. Dr. Schöls received research grants of the DFG, BMBF, EU to EUROSCA, and HSP-Selbsthilfegruppe Deutschland e.V.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linnemann, C., Tezenas du Montcel, S., Rakowicz, M. et al. Peripheral Neuropathy in Spinocerebellar Ataxia Type 1, 2, 3, and 6. Cerebellum 15, 165–173 (2016). https://doi.org/10.1007/s12311-015-0684-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-015-0684-6