Abstract
Despite promising evidence that school-based health centers (SBHCs) and school mental health (SMH) services can reduce disparities in access to mental health care for underserved populations, little is known about what predicts retention of youth in SMH services. This study aimed to identify individual- and school-level factors associated with access and retention in mental health services provided in SBHCs. Existing data were analyzed for 17,348 students (2205 who received SMH services) who attended 17 middle and high schools in an urban school district. Student-level predictors included sex, race/ethnicity, and mental health need at intake. School-level predictors included grade level (middle vs. high school), student/teacher ratio, percent of white students, and percent of students receiving free or reduced lunch. Hierarchical generalized linear modeling was used to examine the association between student- and school-level variables and retention in care. White, Latino, and Asian students were less likely to access SMH services; multiracial and Native American students were more likely to access services, and African-American students were no more or less likely. Hierarchical models found that retention in services was more likely for female students, those who presented with social/educational problems, internalizing problems, and trauma/abuse/neglect, and less likely for Asian students. Retention was also more likely for students in middle schools, schools with a lower student/teacher ratio, and schools with a smaller percentage of students eligible for free or reduced lunch. While SMH services show promise in increasing access for underserved groups, ensuring equitable retention of students in care will likely require concerted effort focused on consistently engaging students and ensuring quality of care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children and adolescents’ underutilization of mental health services is a significant public health problem. Although over 18 million children and adolescents experience mental health problems, only a third of those youth receive treatment (Costello, Foley, & Angold, 2006; Merikangas et al., 2011). Youth of color are significantly less likely to access mental health care than their white peers despite similar levels of need for services (Cauce et al., 2002; Cook, Barry, & Busch, 2013; Garland et al., 2005; Snowden & Yamada, 2005). Further, research indicates that even when youth of color initiate mental health services, they are more likely to terminate prematurely (Haan, Boon, Jong, Geluk, & Vermeiren, 2014; Wolf, Dulmus, Maguin, & Perkins, 2014). These disparities are troubling given research has consistently indicated that unmet mental health needs contribute to negative outcomes for youth, including substance abuse and suicide, and a range of outcomes that occur disproportionately for low-income youth and youth of color, such as school dropout, youth violence, and juvenile justice involvement (Breslau, Kendler, Su, Gaxiola-Aguilar, & Kessler, 2005; Jane Costello et al., 2006; Kessler et al., 2012).
Schools provide convenient access points for health, mental health, and other services, reducing barriers to treatment that plague traditional outpatient settings, such as transportation, health insurance, and parental involvement (Pullmann, Bruns, Daly, & Sander, 2013; Pullmann, VanHooser, Hoffman, & Heflinger, 2010). Schools may be particularly effective in promoting access to care for historically underserved groups, such as youth from lower socioeconomic backgrounds and minority racial and ethnic groups (Allison et al., 2007; Juszczak, Melinkovich, & Kaplan, 2003; Lyon, Ludwig, VanderStoep, Gudmundsen, & McCauley, 2013; Soleimanpour, Geierstanger, Kaller, McCarter, & Brindis, 2010). A study of 12 school-based health centers (SBHCs) in northern California found SBHCs provided increased access to health care for ethnic and racial minority and uninsured or underinsured students and that a majority of SBHC users reported that the SBHC was their primary source of care for counseling services (Soleimanpour et al., 2010). Another study focused on school mental health (SMH) services found that Latino adolescents were four times more likely to be referred to services than Asian students (Guo et al., 2013).
Ecological theories for understanding mental health care help-seeking and utilization, especially among ethnic minority youth, highlight organizational and social influences, such as referral systems and peer networks, as well as individual influences on adolescents’ pathways into services (Cauce et al., 2002). Ecological frameworks are also applicable to access and retention in SMH services. Several factors at the organizational and individual levels influence disparities in mental health service use. Racial and ethnic disparities in mental health service use vary by the setting in which they are provided (e.g., schools) even when student need for services, socioeconomic status, and a range of other relevant variables are controlled (Anyon, Moore et al., 2013; Burns et al., 1995; Gudiño, Martinez, & Lau, 2012).
Access to SMH Services
School contextual factors such as school size, organization (e.g., student/teacher ratio), and student composition influence access to and utilization of SBMH services (Gottfredson & Gottfredson, 2001; Waters, Cross, & Runions, 2009; Wilson, Gottfredson, & Najaka, 2001). For example, several researchers have found an association between various aspects of school organizational and structural characteristics and the level of implementation of school-based prevention programs and associated outcomes (Bradshaw, Koth, Thornton, & Leaf, 2009; Payne, Gottfredson, & Gottfredson, 2006). Some important school characteristics include size and number of students in the school, instructional and management characteristics, and school level (e.g., elementary, secondary), which can lead to differential outcomes (Gottfredson & Gottfredson, 2001; Waters et al., 2009; Wilson et al., 2001). For example, elementary, middle, or high school levels may play an important role in expected outcomes (Eccles & Roeser, 2011; Stone et al., 2009). A recent study comparing differences in school-level characteristics found participants in elementary schools to rate characteristics of the learning environment higher than those in high schools, regardless of whether the school had a SBHC (Strolin-Goltzman et al., 2012).
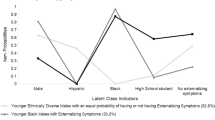
At the individual level, students’ racial/ethnic background influences the how school staff and clinicians refer students to SMH services as well as the diagnoses received. School staff members’ perceptions of students’ mental health concerns are often racially and culturally biased. School staff members tend to initiate referrals in response to disruptive behavior, learning difficulties, and truancy, not the full range of problems that constitute need for health services (Chang & Sue, 2003; Costello & Janiszewski, 1990; Zwaanswijk, Ende, Verhaak, Bensing, & Verhulst, 2007). This tendency may shape disparities in service use and retention. For example, only externalized behaviors predict the use of mental health services by youth of color in educational settings, and racial group differences in service use appear to be more pronounced among youth with internalized symptoms (Gudiño et al., 2012).
Retention in SMH Services
Despite promising evidence that both SBHCs and SMH can enhance access to care for underserved populations, the effectiveness of SMH services may be undermined by difficulties with retention in care (de Haan, Boon, de Jong, Hoeve, & Vermeiren, 2013; Kazdin & Mazurick, 1994; Miller, Southam-Gerow, & Allin, 2008). Across all mental health service settings, at least 20% of clients drop out of therapy prematurely (Swift & Greenberg, 2012), with some studies finding rates up to 75% (Aubuchon-Endsley & Callahan, 2009; Callahan et al., 2014; de Haan et al., 2013). In the current study, retention refers to individuals who attend at least one appointment after the initial visit (Lau & Weisz, 2003; Miller et al., 2008). Clients who terminate after only one session are particularly likely to have poor outcomes, with approximately one-third of these clients exhibiting worse symptoms at follow-up (Pekarik, 1983, 1992). This is particularly problematic for SMH, given previous research has found the modal number of sessions in one district’s SMH initiative was one (Walker, Kerns, Lyon, Bruns, & Cosgrove, 2010). Although little is known about retention in SMH, research has identified student factors that predict service retention in community and specialty mental health. Generally speaking, underserved populations (low socioeconomic status and ethnic minority groups) are most vulnerable to premature termination (de Haan et al., 2013; Fenger, Mortensen, Poulsen, & Lau, 2011). Among ethnic minority clients, African-American clients may be particularly likely to terminate prematurely (Miller et al., 2008). Children who have more severe diagnoses, a history of psychiatric hospitalization, and private health insurance tend to receive more services (Harpaz-Rotem, Leslie, & Rosenheck, 2004). Only one previous study has examined post-referral differences in utilization of SMH services. This study found that differences may occur between students who decide to enroll in services and continue treatment versus those who are referred to services but do not continue with treatment (Guo et al., 2013).
Much of the literature on treatment retention has focused on individual-level variables, but there is reason to suspect that organizational factors are also important. School contextual factors (e.g., grade level, size, racial/ethnic composition, and school climate) influence access to and use of SMH services (Billy et al., 2000; Glisson et al., 2007; Gottfredson & Gottfredson, 2001; Gottfredson, Jones, & Gore, 2002; Waters, Cross, & Runions, 2009; Wilson, Gottfredson, & Najaka, 2001). Research also shows that schools with high student mobility, discipline problems, high rates of suspensions, and low student attendance are more likely to have problems implementing evidence-based behavioral health programs (Gottfredson & Gottfredson, 2001; 2002).
The Current Study
Although research has determined that SMH improves access to mental health services, especially for underserved populations of youth (Allison et al., 2007; Brindis et al., 2003; Lyon et al., 2013; Soleimanpour et al., 2010), few studies have investigated retention in SMH. Moreover, research that has been conducted rarely controls for factors that may actually influence the need for services, such as diagnosis, relying instead on self-report surveys. Finally, there has been little research conducted in the last decade investigating school-level predictors of SMH access.
To improve mental health outcomes for vulnerable populations of youth, it is imperative to better operationalize and understand the reasons for disparities in access to and retention in SMH services. However, little is known about the relative contribution of organizational (e.g., school) and individual (i.e., student) factors and how they influence disparities in SMH access and retention. The current study sought to inform our understanding by analyzing school and service use data from a long-standing SBHC initiative that includes a well-developed SMH component. The objective of this study was to determine which factors contribute to disparities in access (i.e., entering treatment) and retention (attending at least one session of treatment beyond intake) of SMH services (Miller et al., 2008). Specifically, we sought to (1) identify racial disparities in access to SMH services, (2) identify racial disparities in retention of SMH services, and (3) determine which student and school characteristics are associated with disparities in retention in SMH services provided in these SBHCs. We hypothesize that access to and retention in SMH services will vary by race, diagnosis category, and school-level variables.
Method
Study Context
The context for the study was a SBHC initiative in a public school district in a large, western US city. SBHCs in this district provide integrated primary care and mental health services. Students are identified for mental health and medical services through routine risk assessment performed by healthcare providers, referrals from school intervention teams, targeted screening by school nurses, and self-referral. Staffing for the SBHCs typically consists of a full-time nurse practitioner, a full-time, masters-level mental health clinician, and a half-time administrative assistant. The current study focused on SMH services provided in SBHCs operating in the district’s 17 secondary schools.
Sample
The overall population includes 17,348 students who attended the 17 middle and high schools with SBHCs during the 2015–2016 school year (Table 1). Approximately 36% of these students received SBHC services. Of these, our primary sample of interest includes 2205 middle and high school students (13% of the total school population) who used SMH services in the SBHCs during this year. Nineteen of these students (0.8%) were excluded because race or diagnosis data were missing. As shown in Table 1, SMH service users were 21% African-American, 19% Asian/Pacific Islander, 33% Caucasian, 11% Hispanic/Latino, 15% multiracial, 1% American Indian. Females make up about 68% of the sample, and males include 31% of the sample.
Data Sources
This study analyzed data from two sources. First, we accessed publicly available aggregate school-level data (e.g., school student/teacher ratio, percent of white students at the school, and percent of students eligible for free and reduced lunch). The second data source is the SBHC service utilization database. This database houses the service records for all students that access the SBHC and includes information on student demographics, dates of services, intake data (e.g., initial diagnosis codes), and service use data (e.g., dates of service, procedure codes).
Measures
Dependent Variables
SMH service access Student-level SMH service use was based on provider-reported documentation in the SBHC service utilization database. Service access was measured at the student population level. Access was a dichotomous variable defined as using SMH services in the SBHC at least one time, as compared to no use.
SMH service retention Retention was computed only for students who accessed SMH services in the SBHC. Retention was a dichotomous variable defined as using SBHC mental health services two or more times (retained) versus a single visit (Lau & Weisz, 2003; Miller et al., 2008).
Independent Variables: Student-Level Measures
Demographics Sex was dichotomously coded (males = 1, females = 0). Race/ethnicity was coded into dichotomous variables (1 = yes, 0 = no) for each of seven categories: African-American, Latino, White, Asian/Pacific Islander, multiracial, and Native American.
Mental Health Need at Intake Each student was given a brief intake assessment at first service. Service records provided either a preliminary ICD-9 or 10 diagnosis code or a reason for seeking services. These codes were used to develop a proxy for problem type and severity of mental health need. Codes were categorized using DSM-5 diagnostic hierarchies (e.g., related codes were collapsed into “depressive disorders”), then using empirically established diagnostic clusters (e.g., depression and anxiety are both forms of internalizing distress) (Brown & Barlow, 2004; Brown, Chorpita, & Barlow, 1998). The first, fourth, sixth, and last authors reviewed the list of codes and developed a categorization scheme via a consensus process. This process resulted in the following five need categories: (1) social/educational problems (e.g., educational circumstances, family issues, social problems); (2) internalizing problems (e.g., depression, anxiety); (3) externalizing problems (e.g., ADHD, impulse disorders, behavioral acting out); (4) trauma/abuse/neglect (e.g., rape, abuse, post-traumatic stress); and (5) non-specific problems (e.g., general counseling, stress). The frequency of each of the diagnosis categories is shown in Table 2 with 36% presenting with social/educational needs, 26% presenting with internalizing needs, 2% presenting with externalizing needs, 3% presenting with trauma/abuse/neglect, and 34% presenting with non-specific needs.
Independent Variables: School-Level Measures
School characteristics included student/teacher ratio, % of students receiving free/reduced lunch, % white students, and school grade level (middle = 1, high school = 0). These variables were collected from school profile data which is publicly available on the district website.
Analytic Strategy
Statistical analyses were conducted using SPSS (SPSS, 2009), Stata (“Data Analysis and Statistical Software | Stata,” n.d.), and HLM software packages (Bryk & Raudenbush, 2011). To analyze disparities in access to SMH services, odds ratios were calculated comparing students who accessed SMH services to the total school population by race/ethnicity. This provided information about each group’s representation in SMH services compared to the group’s representation of the total student population.
To analyze disparities in retention in SBHC services, prior to any inferential statistics, univariate and bivariate descriptive statistics were computed to assess distributions and associations among student- and school-level variables. Variables which were not significant in the bivariate analysis were not included in the multilevel models. Subsequently, a series of two-level hierarchical generalized linear models (HLMs) to account for students nested within schools were computed with student factors at level 1 and school factors at level 2. Simple contrast coding was used for race and mental health need, with White and non-specific problems as the reference categories. Therefore, odds ratios in these models represent each racial/ethnic group’s representation in SBHC services as compared to White students and each mental health need category as compared to non-specific problems. To improve interpretability of the coefficients, all level 2 covariates were grand mean centered with the exception of school grade level. Because the dependent variable of retention was dichotomous, models applied a Bernoulli distribution at level 1 with a logit-link function. Results depict unit-specific models. Estimation was computed using full maximum likelihood via EM-Laplace 2 using HLM software (Bryk & Raudenbush, 2011).
Model building followed a standard approach (Bryk & Raudenbush, 1992). First, a null model was calculated. Level 1 predictors were added based on our research questions of interest and known associations. Level 2 variables were then added to this level 1 model. Goodness-of-fit statistics were calculated using χ2 deviance statistics between each model iteration.
Results
Patterns of Racial Disparity in Access to SMH Services
Of the 17,348 students in the 17 schools with SBHCs, 13% (n = 2205) accessed SMH services in the SBHC during the period examined (see Table 1). Of the students who accessed SMH services, 33% were White; this group comprised 38% of the total secondary school population. White students had 19% (OR = 0.81; p < .001) smaller odds of accessing SMH services than all other students. Similarly, Latino students and Asian students had 20% (OR = 0.80; p < .001) smaller odds of accessing SMH services than all other students. The odds of accessing services were 230% greater for multiracial students (OR = 3.3; p < .001) and 350% greater for Native American students (OR = 4.5; p < .001) than all other students.
Bivariate Associations of Retention in SMH Services
As shown in Table 2, of the 2205 students who accessed SMH services, bivariate analyses revealed that males (OR = 0.66; p < .001), Black students (OR = 0.76; p < .01), and Asian students (OR = 0.69; p < .01) had significantly lower odds of retention in SMH services (i.e., attending 2 or more sessions). Students presenting with social/educational (OR = 1.6; p < .001) and internalizing problems (OR = 2.9; p < .001) as well as trauma/abuse/neglect (OR = 3.5; p < .01) were significantly more likely to be retained in SMH services, while students with non-specific problems (OR = 0.28; p < .001) were significantly less likely to be retained.
Multilevel Predictors of Disparities in Retention of SMH Services
Table 3 presents results from multilevel models examining predictors of retention in SMH services. The final model revealed that the odds of retention in services were significantly lower for male students, compared to female students (OR = 0.67; p < .01) and Asian students, as compared to White students (OR = 0.72; p < .01). In addition, the odds of retention in services were significantly greater for those students who presented with social/educational problems (OR = 3.27; p < .01), internalizing problems (OR = 4.97; p < .01), and trauma/abuse/neglect (OR = 8.87; p < .01).
School-level variables that predicted retention in SMH services included being in middle school, as compared to high school (OR = 2.81; p < .05), being in school with a lower student/teacher ratio (OR = 0.76; p < .05), and being in a school with a smaller percentage of students eligible for free and reduced lunch (OR = 0.93; p < .05). The percentage of white students in the school was not significantly related to odds of retention.
Discussion
SBHCs and SMH services have both shown promise for increasing access to mental health care for underserved populations. However, relatively little is known about whether students from underserved groups are retained in services once they access care, and few studies have examined student- and school-level characteristics that predict access and retention. The current study found that, compared to the overall school population, there were significantly higher proportions of Native American and multiracial students who accessed SMH services, and significantly lower proportions of Hispanic, Asian, and White students accessed SMH services.
Once students accessed services, males and African-Americans were less likely to be retained. Students presenting with social/educational problems, internalizing problems, and trauma/abuse/neglect were more likely to be retained compared to students with non-specific problems. We also identified school-level characteristics that predicted retention. High school students were less likely to be retained in SMH services, as were students in schools with higher student/teacher ratios and a greater proportion of students eligible for free and reduced lunch.
Access in School Mental Health Services
Hispanic students in our sample were less likely to access SMH services, while African-American students were proportionally represented given their representation in the student body. These results are somewhat different from previous studies which have found Hispanic and African-American students overrepresented in SBHC services (Amaral, Geierstanger, Soleimanpour, & Brindis, 2011; Anyon, Moore et al., 2013; Anyon, Whitaker, Shields, & Franks, 2013; Walker et al., 2010). This finding may suggest that African-American students are adequately accessing SMH services in the study district. Perhaps the underutilization of services by Asian and Latino students is reflective other factors which have been associated with lower mental health care utilization among these populations such as lower levels of acculturation, lower levels of health literacy or knowledge of available services, or family factors such as less communication between parents and children (Alegria et al., 2004; Guo et al., 2013). Differences may also reflect that, unlike many of the studies cited above, the current study sought to control for students’ behavioral health needs at baseline. As presented above, over half of students presented for SMH services in these SBHCs without a specific mental health diagnosis, seeking more general counseling for stress or academic issues. Further examination of the presenting problems of different types of students is warranted to both explain this funding and tailor SMH services in SBHCs to different types of students.
Consistent with previous studies, we found that Asian students are underrepresented in SMH services (Anyon, Moore et al., 2013; Anyon, Whitaker et al., 2013; Whitaker, 2015). Some research suggests that this underutilization is at least partly accounted for by under-referral of Asian students by school staff. For instance, Guo et al. (2013) found that Asian Americans in their school-based sample tended to perform better academically and endorse fewer externalizing symptoms and that this mediated racial/ethnic differences in referral to SMH. Particularly in school settings, adults may be particularly attuned to acting out behaviors and academic concerns and less able to recognize internalizing symptoms. The underutilization of SMH by Asian American students may also be accounted for by student misperceptions of SBHC services. Interviews and focus groups with Asian American high school students found that some youth perceive SBHCs as primarily providing services to students engaging in risky behaviors requiring reproductive health services (e.g., early sexual activity) and services for youth with externalizing behaviors (i.e., student who got in trouble, substance use) (Anyon, Whitaker et al., 2013). More research is needed to understand the barriers to access to mental health care for Asian American youth and determine effective ways to engage and retain this underserved group in SMH services.
Retention in School Mental Health Services
One of the unique contributions of this study is moving beyond a focus on access, to understanding the factors that influence retention in SMH services. The current study contributes to the nascent literature on individual-level factors associated with retention in SMH. We found that males and African-American students were significantly less likely to be retained in services. Both of these findings are consistent with previous research in school-based and community settings (Adelman, Barker, & Nelson, 1993; Amaral et al., 2011; Miller et al., 2008; Pastore, Juszczak, Fisher, & Friedman, 1998; Soleimanpour et al., 2010). At least among adult recipients of health services, ethnic minority groups (African-American, Hispanic, and Asian) report lower service satisfaction, perceive poorer quality of care, and have less confidence in their providers (Institute of Medicine, 2003; Zane, Enomoto, & Chun, 1994). Although the evidence on the effects of ethnic matching on treatment retention and effectiveness is mixed, pointing to null or small but significant effects (Maramba & Nagayama Hall, 2002; Shin et al., 2005), it should be noted that the vast majority of mental health providers in our sample were White and female. More recently, researchers have conceptualized ethnic match as a proxy for client–therapist “cognitive match” on factors such as problem conceptualization and coping orientation, which are likely to lead to enhanced therapeutic alliance and improved treatment outcomes (Zane et al., 2005). A fuller understanding of the reasons for treatment dropout among male and African-American students in school-based settings is needed.
This study found that internalizing problems, social/educational functioning problems, and problems extending from trauma/abuse/neglect were all predictive of retention in services, even after controlling for individual and school-level characteristics. These findings are in line with community-based studies showing youth who have more serious problems tended to experience greater intensity of care. Given that mental health clinicians working in SBHCs tend to be able to serve youth with a broad range of problems (evidenced here with the large percentage of students presenting for general counseling and/or with no assigned mental health diagnosis), it makes sense that students with these more serious and/or specific types of presenting problems would be relatively more likely to be engaged past one session (Harpaz-Rotem et al., 2004).
Although mental health needs related to social/educational problems, internalizing problems, and trauma/abuse and neglect were associated with greater retention, we did not find externalizing behaviors predictive of retention in SMH services. In fact, students presenting with externalizing problems were less likely to receive more than one session. This may suggest students with these types of presenting problems are less likely to be retained in services due to perceptions of an involuntary nature of these types of referrals. Previous school-based research has found that school staff members tend to initiate referrals in response to disruptive behavior, learning difficulties, and truancy, not the full range of problems that constitute need for services (Chang & Sue, 2003; Costello & Janiszewski, 1990; Guo et al., 2013; Zwaanswijk et al., 2007). This tendency may shape disparities in service use. For example, one study found that only externalizing behaviors predict the use of mental health services by youth of color in educational settings, and racial group differences in service use appear to be more pronounced among youth with internalizing symptoms (Gudiño, Martinez, & Lau, 2012). Guo and colleagues (2013) found conduct problems mediated the relationship between ethnicity and referral to SMH services. Additional research using methods such as mediation and moderation is needed to better understand barriers to retention in SMH services and reduced disparities in mental health for underserved populations.
Contribution of School-Level Variables
Across a number of indicators, we found that lower-resource schools tended to have lower retention in services. Specifically, student/teacher ratio and percent of students eligible for free and reduced lunch were both negatively associated with retention in SMH services. Racial and ethnic disparities in mental health service use may vary by the setting in which they are provided (e.g., schools) even when student need for services, socioeconomic status, and a range of other relevant variables are controlled (Anyon, Moore et al., 2013; Burns et al., 1995; Gudiño et al., 2012; Lyon et al., 2013). In addition, similar types of school characteristics (e.g., characteristics of students in the school, instructional characteristics, school climate, and school level) have been found to contribute to differential outcomes related to school-based services (Gottfredson & Gottfredson, 2001; Waters et al., 2009; Wilson et al., 2001). These school-level characteristics point to organizational factors that may cause a more chaotic school environment where students may be less likely to receive individualized attention and follow-up from school staff. However, research has found that SBHCs are more likely to exist in schools with larger student populations that include high percentages of nonwhite students and students eligible for free or reduced price lunches (Bersamin, Fisher, Gaidus, & Gruenewald, 2016). Future research could address ways that SBHC staff successfully navigate potentially chaotic school environments and provide sufficient attention and follow-up to students. In addition, future research could include more malleable school-level factors, such as indicators of school climate, which could be addressed through school-level interventions.
Limitations and Future Directions
The current study extends the existing literature on SMH by identifying student and school predictors of access and retention in school-based mental health. Nonetheless, several limitations of the study should be noted. First, our sample was drawn from SBHCs serving one school district in an urban area. Generalizability of the findings to other districts may be impacted by initiatives, policies, and other contextual factors unique to this district. For instance, while many SMH practitioners can only see students who qualify for Medicaid and/or meet diagnostic eligibility criteria, SBHC services in this district are funded by sources that allow access by all students. Second, our indicator of mental health need relied on clinician diagnosis codes at first visit. Future research may benefit from including more sensitive indicators of mental health need such as standardized measure of symptoms and functioning. In addition, given the primary focus of schools on academic outcomes, it will be important to include indicators of academic performance (e.g., attendance, grades) to examine additional predictors and outcomes of services.
Conclusions
These limitations notwithstanding, the current study is among the first to identify student and school predictors of retention in SMH. Consistent with findings from other mental health service sectors, we found that African-American and male students and those in low-resource settings are less likely to return for a second mental health visit. These findings suggest that while SMH services show promise in increasing access to care for some underserved groups, there is significant work to be done to retain students in treatment in order to eliminate long-standing disparities in mental health status. System-level quality improvement initiatives that strive to consistently identify all students in need, engage all students, provide research-based treatment elements for all students, and use data to stay on track in these areas may support this cause.
In a finding that is somewhat inconsistent with previous research, results did not demonstrate disproportionately greater SMH service access for African-American and Hispanic students. This finding underscores the importance of ensuring that SBHCs and SMH initiatives not assume that their presence alone will address the vast disparities in mental health care access that exist in our society. Taken together, findings from this study reinforce that, to achieve broad effects, SBHCs and SMH services must be ever striving to achieve a “triple aim” of access, efficiency, and quality of care.
References
Adelman, H. S., Barker, L. A., & Nelson, P. (1993). A study of a school-based clinic: Who uses it and who doesn’t? Journal of Clinical Child Psychology, 22(1), 52.
Alegria, M., Takeuchi, D., Canino, G., Duan, N., Shrout, P., Meng, X.-L., et al. (2004). Considering context, place and culture: the National Latino and Asian American study. International Journal of Methods in Psychiatric Research, 13(4), 208–220. https://doi.org/10.1002/mpr.178.
Allison, M. A., Crane, L. A., Beaty, B. L., Davidson, A. J., Melinkovich, P., & Kempe, A. (2007). School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics, 120(4), e887–e894. https://doi.org/10.1542/peds.2006-2314.
Amaral, G., Geierstanger, S., Soleimanpour, S., & Brindis, C. (2011). Mental health characteristics and health-seeking behaviors of adolescent school-based health center users and nonusers. Journal of School Health, 81(3), 138–145. https://doi.org/10.1111/j.1746-1561.2010.00572.x.
Anyon, Y., Moore, M., Horevitz, E., Whitaker, K., Stone, S., & Shields, J. P. (2013). Health risks, race, and adolescents’ use of school-based health centers: Policy and service recommendations. The Journal of Behavioral Health Services & Research, 40(4), 457–468. https://doi.org/10.1007/s11414-013-9356-9.
Anyon, Y., Whitaker, K., Shields, J. P., & Franks, H. (2013). Help-seeking in the school context: understanding Chinese American adolescents’ underutilization of school health services. Journal of School Health, 83(8), 562–572. https://doi.org/10.1111/josh.12066.
Aubuchon-Endsley, N. L., & Callahan, J. L. (2009). The hour of departure: Predicting attrition in the training clinic from role expectancies. Training and Education in Professional Psychology, 3(2), 120–126. https://doi.org/10.1037/a0014455.
Bersamin, M. M., Fisher, D. A., Gaidus, A. J., & Gruenewald, P. J. (2016). School-based health centers’ presence: The role of school and community factors. American Journal of Preventive Medicine, 51(6), 926–932. https://doi.org/10.1016/j.amepre.2016.06.025.
Billy, J. O., Grady, W. R., Wenzlow, A. T., Brener, N. D., Collins, J. L., & Kann, L. (2000). Contextual influences on school provision of health services. The Journal of Adolescent Health, 27(1), 12–24.
Bradshaw, C. P., Koth, C. W., Thornton, L. A., & Leaf, P. J. (2009). Altering school climate through school-wide positive behavioral interventions and supports: Findings from a group-randomized effectiveness trial. Prevention Science, 10(2), 110–115.
Breslau, J., Kendler, K. S., Su, M., Gaxiola-Aguilar, S., & Kessler, R. C. (2005). Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine, 35(03), 317–327. https://doi.org/10.1017/S0033291704003514.
Brindis, C., Klein, J., Schlitt, J., Santelli, J., Juszczak, L., & Nystrom, R. J. (2003). School-based health centers: Accessibility and accountability. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 32(6 Suppl), 98–107.
Brown, T. A., & Barlow, D. H. (2004). Classification of anxiety and mood disorders. In D. H. Barlow (Ed.), Anxiety and its disorders: The nature and treatment of anxiety and panic. New York: Guilford Press.
Brown, T. A., Chorpita, B. F., & Barlow, D. H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107(2), 179–192. https://doi.org/10.1037/0021-843X.107.2.179.
Bryk, A. S., & Raudenbush, S. W. (1992). Hierarchical linear models for social and behavioral research: Applications and data analysis methods. Newbury Park, CA: SAGE Publications.
Bryk, A. S., & Raudenbush, S. W. (2011). HLM 7.0 for windows. Lincolnwood, IL: Scientific Software International, Inc.
Burns, B. J., Costello, E. J., Angold, A., Tweed, D., Stangl, D., Farmer, E. M., et al. (1995). Children’s mental health service use across service sectors. Health Affairs, 14(3), 147–159. https://doi.org/10.1377/hlthaff.14.3.147.
Callahan, J. L., Gustafson, S. A., Misner, J. B., Paprocki, C. M., Sauer, E. M., Saules, K. K., et al. (2014). Introducing the association of psychology training clinics’ collaborative research network: A study on client expectancies. Training and Education in Professional Psychology, 8(2), 95–104. https://doi.org/10.1037/tep0000047.
Cauce, A. M., Domenech-Rodríguez, M., Paradise, M., Cochran, B. N., Shea, J. M., Srebnik, D., et al. (2002). Cultural and contextual influences in mental health help seeking: A focus on ethnic minority youth. Journal of Consulting and Clinical Psychology, 70(1), 44–55. https://doi.org/10.1037/0022-006X.70.1.44.
Chang, D. F., & Sue, S. (2003). The effects of race and problem type on teachers’ assessments of student behavior. Journal of Consulting and Clinical Psychology, 71(2), 235–242. https://doi.org/10.1037/0022-006X.71.2.235.
Cook, B. L., Barry, C. L., & Busch, S. H. (2013). Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research, 48(1), 129–149. https://doi.org/10.1111/j.1475-6773.2012.01439.x.
Costello, E. J., Foley, D. L., & Angold, A. (2006). 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: II. developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry, 45(1), 8–25. https://doi.org/10.1097/01.chi.0000184929.41423.c0.
Costello, E. J., & Janiszewski, S. (1990). Who gets treated? Factors associated with referral in children with psychiatric disorders. Acta Psychiatrica Scandinavica, 81(6), 523–529. https://doi.org/10.1111/j.1600-0447.1990.tb05492.x.
Data Analysis and Statistical Software | Stata. (n.d.). Retrieved April 2, 2016. from http://www.stata.com/
de Haan, A. M., Boon, A. E., de Jong, J. T. V. M., Hoeve, M., & Vermeiren, R. R. J. M. (2013). A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review, 33(5), 698–711. https://doi.org/10.1016/j.cpr.2013.04.005.
Eccles, J. S., & Roeser, R. W. (2011). Schools as developmental contexts during adolescence. Journal of Research on Adolescence, 21(1), 225–241. https://doi.org/10.1111/j.1532-7795.2010.00725.x.
Fenger, M., Mortensen, E. L., Poulsen, S., & Lau, M. (2011). No-shows, drop-outs and completers in psychotherapeutic treatment: Demographic and clinical predictors in a large sample of non-psychotic patients. Nordic Journal of Psychiatry, 65(3), 183–191. https://doi.org/10.3109/08039488.2010.515687.
Garland, A. F., Lau, A. S., Yeh, M., McCabe, K. M., Hough, R. L., & Landsverk, J. A. (2005). Racial and ethnic differences in utilization of mental health services among high-risk youths. The American Journal of Psychiatry, 162(7), 1336–1343. https://doi.org/10.1176/appi.ajp.162.7.1336.
Glisson, C., Landsverk, J., Schoenwald, S., Kelleher, K., Hoagwood, K. E., & Mayberg, S. (2007). Assessing the organizational social context (OSC) of mental health services: Implications for research and practice. Administration and Policy in Mental Health and Mental Health Services Research, 35(1–2), 98–113. https://doi.org/10.1007/s10488-007-0148-5.
Gottfredson, G. D., & Gottfredson, D. C. (2001). What schools do to prevent problem behavior and promote safe environments. Journal of Educational and Psychological Consultation, 12(4), 313–344. https://doi.org/10.1207/S1532768XJEPC1204_02.
Gottfredson, D. C., & Gottfredson, G. D. (2002). Quality of school-based prevention programs: Results from a national survey. Journal of Research in Crime and Delinquency, 39(1), 3–35. https://doi.org/10.1177/002242780203900101.
Gottfredson, G. D., Jones, E. M., & Gore, T. W. (2002). Implementation and evaluation of a cognitive–behavioral intervention to prevent problem behavior in a disorganized school. Prevention Science, 3(1), 43–56. https://doi.org/10.1023/A:1014671310038.
Gudiño, O. G., Martinez, J. I., & Lau, A. S. (2012). Mental health service use for children in contact with child welfare: Racial disparities depend on problem type. Psychiatric Services, 63(10), 1004–1010. https://doi.org/10.1176/appi.ps.201100427.
Guo, S., Kataoka, S. H., Bear, L., & Lau, A. S. (2013). Differences in school-based referrals for mental health care: Understanding racial/ethnic disparities between Asian American and Latino youth. School Mental Health, 6(1), 27–39. https://doi.org/10.1007/s12310-013-9108-2.
Haan, A. M., Boon, A. E., Jong, J. T. V. M., Geluk, C. A., & Vermeiren, R. R. (2014). Therapeutic relationship and dropout in youth mental health care with ethnic minority children and adolescents. Clinical Psychologist, 18(1), 1–9. https://doi.org/10.1111/cp.12030.
Harpaz-Rotem, I., Leslie, D., & Rosenheck, R. A. (2004). Treatment retention among children entering a new episode of mental health care. Psychiatric Services, 55(9), 1022–1028. https://doi.org/10.1176/appi.ps.55.9.1022.
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. (2003). In B. D. Smedley, A. Y. Stith, & A. R. Nelson (Eds.), Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK220358/.
Juszczak, L., Melinkovich, P., & Kaplan, D. (2003). Use of health and mental health services by adolescents across multiple delivery sites. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 32(6 Suppl), 108–118.
Kazdin, A. E., & Mazurick, J. L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62(5), 1069–1074. https://doi.org/10.1037/0022-006X.62.5.1069.
Kessler, R. C., Avenevoli, S., Costello, E. J., Georgiades, K., Green, J. G., Gruber, M. J., et al. (2012). Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 69(4), 372–380. https://doi.org/10.1001/archgenpsychiatry.2011.160.
Lau, A. S., & Weisz, J. R. (2003). Reported maltreatment among clinic-referred children: Implications for presenting problems, treatment attrition, and long-term outcomes. Journal of the American Academy of Child and Adolescent Psychiatry, 42(11), 1327–1334. https://doi.org/10.1097/01.CHI.0000085754.71002.14.
Lyon, A. R., Ludwig, K. A., VanderStoep, A., Gudmundsen, G., & McCauley, E. (2013). Patterns and predictors of mental healthcare utilization in schools and other service sectors among adolescents at risk for depression. School Mental Health, 5(3), 155–165. https://doi.org/10.1007/s12310-012-9097-6.
Maramba, G. G., & Nagayama Hall, G. C. (2002). Meta-analyses of ethnic match as a predictor of dropout, utilization, and level of functioning. Cultural Diversity and Ethnic Minority Psychology, 8(3), 290–297. https://doi.org/10.1037/1099-9809.8.3.290.
Merikangas, K. R., He, J., Burstein, M., Swendsen, J., Avenevoli, S., Case, B., et al. (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the national comorbidity survey–adolescent supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50(1), 32–45. https://doi.org/10.1016/j.jaac.2010.10.006.
Miller, L. M., Southam-Gerow, M. A., & Allin, R. B. (2008). Who stays in treatment? Child and family predictors of youth client retention in a public mental health agency. Child & Youth Care Forum, 37(4), 153–170. https://doi.org/10.1007/s10566-008-9058-2.
Pastore, D. R., Juszczak, L., Fisher, M. M., & Friedman, S. B. (1998). School-based health center utilization: A survey of users and nonusers. Archives of Pediatrics and Adolescent Medicine, 152(8), 763–767. https://doi.org/10.1001/archpedi.152.8.763.
Payne, A. A., Gottfredson, D. C., & Gottfredson, G. D. (2006). School predictors of the intensity of implementation of school-based prevention programs: results from a national study. Prevention Science: The Official Journal of the Society for Prevention Research, 7(2), 225–237. https://doi.org/10.1007/s11121-006-0029-2.
Pekarik, G. (1983). Follow-up adjustment of outpatient dropouts. American Journal of Orthopsychiatry, 53(3), 501–511. https://doi.org/10.1111/j.1939-0025.1983.tb03394.x.
Pekarik, G. (1992). Posttreatment adjustment of clients who drop out early vs. late in treatment. Journal of Clinical Psychology, 48(3), 379–387. https://doi.org/10.1002/1097-4679(199205)48:3<379:AID-JCLP2270480317>3.0.CO;2-P.
Pullmann, M. D., Bruns, E. J., Daly, B. P., & Sander, M. A. (2013). Improving the evaluation and impact of mental health and other supportive school-based programmes on students’ academic outcomes. Advances in School Mental Health Promotion, 6(4), 226–230. https://doi.org/10.1080/1754730X.2013.835543.
Pullmann, M. D., VanHooser, S., Hoffman, C., & Heflinger, C. A. (2010). Barriers to and supports of family participation in a rural system of care for children with serious emotional problems. Community Mental Health Journal, 46(3), 211–220. https://doi.org/10.1007/s10597-009-9208-5.
Shin, S.-M., Chow, C., Camacho-Gonsalves, T., Levy, R. J., Elaine, I., & Stephen, H. (2005). A meta-analytic review of racial-ethnic matching for African American and Caucasian American clients and clinicians. Journal of Counseling Psychology, 52(1), 45–56. https://doi.org/10.1037/0022-0167.52.1.45.
Snowden, L. R., & Yamada, A.-M. (2005). Cultural differences in access to care. Annual Review of Clinical Psychology, 1(1), 143–166. https://doi.org/10.1146/annurev.clinpsy.1.102803.143846.
Soleimanpour, S., Geierstanger, S. P., Kaller, S., McCarter, V., & Brindis, C. D. (2010). The role of school health centers in health care access and client outcomes. American Journal of Public Health, 100(9), 1597–1603. https://doi.org/10.2105/AJPH.2009.186833.
SPSS, P. (2009). PASW complex samples 18. Chicago.
Stone, S., Astor, R., & Benbenishty, R. (2009). Teacher and principal perceptions of student victimization and the schools’ response to violence: The contributions of context on staff congruence. International Journal of Educational Research, 48(3), 194–213. https://doi.org/10.1016/j.ijer.2009.07.002.
Strolin-Goltzman, J., Sisselman, A., Auerbach, C., Sharon, L., Spolter, S., & Corn, T. B. (2012). The moderating effect of school type on the relationship between school-based health centers and the learning environment. Social Work in Public Health, 27(7), 699–709. https://doi.org/10.1080/19371910903323815.
Swift, J. K., & Greenberg, R. P. (2012). Premature discontinuation in adult psychotherapy: A meta-analysis. Journal of Consulting and Clinical Psychology, 80(4), 547–559. https://doi.org/10.1037/a0028226.
Walker, S. C., Kerns, S., Lyon, A. R., Bruns, E. J., & Cosgrove, T. J. (2010). Impact of school-based health center use on academic outcomes. Journal of Adolescent Health, 46(3), 251–257. https://doi.org/10.1016/j.jadohealth.2009.07.002.
Waters, S. K., Cross, D. S., & Runions, K. (2009). Social and ecological structures supporting adolescent connectedness to school: A theoretical model. Journal of School Health, 79(11), 516–524. https://doi.org/10.1111/j.1746-1561.2009.00443.x.
Whitaker, K. (2015). The relationship between school-based health center utilization, school connectedness, and academic outcomes—proQuest. Berkeley, CA: University of California, Berkeley. Retrieved from https://search.proquest.com/openview/d863eb11f41fc760a6b93dcc674f8d39/1?pq-origsite=gscholar&cbl=18750&diss=y.
Wilson, D. B., Gottfredson, D. C., & Najaka, S. S. (2001). School-based prevention of problem behaviors: A meta-analysis. Journal of Quantitative Criminology, 17(3), 247–272. https://doi.org/10.1023/A:1011050217296.
Wolf, D. A. P. S., Dulmus, C. N., Maguin, E., & Perkins, J. (2014). Differential outcomes in agency-based mental health care between minority and majority youth. Research on Social Work Practice. https://doi.org/10.1177/1049731514550208.
Zane, N., Enomoto, K., & Chun, C.-A. (1994). Treatment outcomes of Asian- and White-American clients in outpatient therapy. Journal of Community Psychology, 22(2), 177–191. https://doi.org/10.1002/1520-6629(199404)22:2<177:AID-JCOP2290220212>3.0.CO;2-7.
Zane, N., Sue, S., Chang, J., Huang, L., Huang, J., Lowe, S., et al. (2005). Beyond Ethnic match: Effects of client-therapist cognitive match in problem perception, coping orientation, and therapy goals on treatment outcomes. Journal of Community Psychology, 33(5), 569–585. https://doi.org/10.1002/jcop.20067.
Zwaanswijk, M., Ende, J. V. D., Verhaak, P. F. M., Bensing, J. M., & Verhulst, F. C. (2007). The different stages and actors involved in the process leading to the use of adolescent mental health services. Clinical Child Psychology and Psychiatry, 12(4), 567–582. https://doi.org/10.1177/1359104507080985.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no competing interests.
Ethical Approval
The data used in this article were de-identified existing data not eligible for Human Subjects review; therefore, this article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Whitaker, K., Nicodimos, S., Pullmann, M.D. et al. Predictors of Disparities in Access and Retention in School-Based Mental Health Services. School Mental Health 10, 111–121 (2018). https://doi.org/10.1007/s12310-017-9233-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12310-017-9233-4