Abstract
Purpose
Controversies exist on the relative contribution of sagittal spino-pelvic alignment on pathogenesis of lumbar disc herniation.
Methods
Spinopelvic alignment parameters, pelvic incidence, pelvic tilt, sacral slope, pelvic radius-S1 end-plate ratio and pelvic radius-S1 angle, in 52 patients with lumbar disc herniation were compared with the same measurements in 43 healthy adult volunteers.
Results
Statistical analysis revealed significant difference in pelvic incidence and sacral slope between patients with lumbar disc herniation and normal population.
Conclusion
Patients with lumbar disc herniation have a more vertical sacrum compared to the normal population which may result in higher intradiscal pressure in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
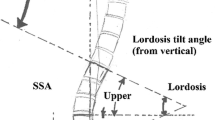
The sagittal balance is characterized by both pelvic and spinal parameters. Several studies have confirmed that the shape and the spatial orientation of the pelvis determines the organization of the lumbo-thoracic spine [1, 2]. Duval-Beaupère et al. [3] and then Legayeet al. [4] coined the term ‘pelvic incidence’ (PI) as a fundamental pelvic parameter that is specific and constant for each individual and determines pelvic orientation as well as lumbar lordosis (LL). Sacral slope (SS) and pelvic tilt (PT) are position-dependent parameters and vary according to the position of the pelvis in space. Pelvic radius technique as described by Jackson et al. [5] measures pelvic morphology by using the approximated center of the hip on the lateral radiograph and drawing a line to the posterior superior corner of S1 end-plate. Pelvic radius-S1 (PR-S1) angle is the angle formed by the line drawn from approximated center of hip to the posterior superior corner of S1 and the line parallel to superior end-plate of S1 vertebrae. Pelvic radius (PR) is also measured in millimetre, representing the distance from approximated hip center (also called bicoxofemoral hip axis) to the posterior superior corner of S1 (Fig. 1). We divided PR by S1 end-plate length (PR/S1) in this study to omit the magnification errors that might be encountered.
Pelvic morphology has been shown to substantially influence the biomechanical characteristics of the lumbar spine and plays a significant role in the pattern of load distribution and mechanical environment of the intervertebral disc. Several studies have been performed to determine any possible relationship between these parameters and degenerative disc and facet disease [5,6,7,8,9]. However, few studies have been carried out to determine the relationship between spino-pelvic morphology and lumbar disc herniation (LDH) in young adult patients [10,11,12,13].
In this study, we conducted a roentgenographic analysis of spino-pelvic sagittal parameters in 52 patients with acute lumbar disc herniation and compared the results with an asymptomatic control group.
Materials and methods
A total of 52 patients with documented lumbar disc herniation (LDH) in magnetic resonance imaging (MRI) who met the inclusion criteria and were aged between 20 and 50 years, were compared with a group of 43 healthy volunteers. LDH patients did not have any other pathology in spine such as spondylolysis, spondylolisthesis, or any history of spine tumour or infection. They had typical radicular pain in lower extremity with or without neurologic deficit and were symptomatic for no more than 6 months. Demographic data such as age, sex and body mass index (BMI), level of disc herniation, duration of symptoms, presence of neurologic deficit and any treatment received were recorded. Lumbar disc protrusion and extrusion were considered as disc herniation and disc bulging or annular tears were not included in the patients’ group.
Forty-three volunteers participated in the study. They aged 20–50 years and had no history of significant trauma, no history of significant back pain seeking medical intervention, no history of spine tumour or infection.
The radiographic protocol was standardized for all participants. For each subject, a standing right lateral radiograph including the lumbar spine and pelvis was obtained with the cassette placed at 72-in from the X-ray tube. Subjects were instructed to stand in a comfortable position with the hips and knees fully extended. Hands were positioned near the ear. All radiographs were acquired in digital format. Parameters of sacropelvic balance and morphology were then measured by two observers using INFINITT software (Optispine, Korea). All participants filled an informed consent form. Those with any contraindication for exposure to x-ray (e.g., pregnancy) were excluded. The study was approved by the University ethics committee.
Lumbopelvic alignment was measured in both groups as described in introduction. For each participant five parameters were measured including PI, SS, PT, PR-S1 and PR/S1.
The data were analysed using the SPSS 14.0 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics (mean and standard deviation) were provided for all subjects. The Kolmogorov–Smirnov test was used to assess if the measured parameters were normally distributed in the two groups. Comparisons between case and control groups were performed using bilateral independent Student’s t tests for those with normal distribution and Mann–Whitney test for the other. The relationship between two observers’ measurements was assessed using Pearson’s coefficient. Statistically significant correlation coefficients were considered clinically large if ≥ 0.8, moderate if ≥ 0.6, and small if ≥ 0.4. p value < 0.05 was considered significant.
Results
Standing Lateral lumbosacral radiographies of 43 healthy adult volunteers and 52 patients with lumbar disc herniation were analysed. Anthropometric data of all subjects is showed in Table 1. Pearson correlation test showed 0.899 correlation coefficient between measurements made by two observers; therefore, only data from the first observer was used for analysis. T test was used in order to calculate the difference between control and LDH groups. Measured spino-pelvic parameters and their respective values are demonstrated in Table 2 and Fig. 2. The mean pelvic incidence was 47.44° (SD = 6.0) in the LDH group and 51.81° (SD = 8.3) in the control group which was significant (p = 0.005). The sacral slope was significantly diminished in the LDH group (38.8° vs. 45.3°) compared to the control group (p = 0.0004). There was an increase in pelvic tilt value in the LDH group but it was weakly significant (p = 0.056).
Other parameters including PR-S1 angel and PR/S1 were analysed with Mann–Whitney test which showed no statistically significant difference between the two groups.
Discussion
Considering the spine as the pylon of a crane, the contact force on the lumbar intervertebral disc is the sum of gravity force (body weight) and the force of posterior paraspinal musculature. The more the lumbar lordosis, the more is the impact of contact force acting on the posterior elements. In low PI/low lordotic spine, the contact force shifts anteriorly towards the intervertebral discs (Fig. 3). In addition, because vertebral end-plates is close to the horizontal plane, the perpendicular component of the contact force increases (as opposed to sliding horizontal component) and the resultant intradiscal pressure increases significantly.

Adapted from: [15]
Position of the contact force (CF) vector relative to the spine in low and high lumbar lordosis.
Several studies have demonstrated loss of lumbar lordosis in patients with lumbar disc herniation. We decided not to include the lumbar lordosis values in the analysis because it is not clear whether this is a primary risk factor or, merely, a secondary response to disc herniation and muscle spasm. However, in the study carried out by Endo et al. lumbar lordosis improved to that of normal population after discectomy and pain relief [14].
We found that sacral slope and pelvic incidence were significantly lower in the LDH group. In these patients, orientation of the discs is almost horizontal which results in significant increase in intradiscal pressure. This may be an important risk factor for early disc degeneration and subsequent disc herniation.
This finding is in concordant with Barrey’s findings [10] who reported low pelvic incidence in young patients with lumbar disc disease. It seems that the risk of lumbar discopathy increases in patients with low PI and flat back. According to Roussouly and Pinheiro-Franco, “this back is not the one adapted for weight bearing, or sports or activities with high intradiscal pressure” [15].
Yang et al. [12] also discovered that the PI of the 80 patients with lumbar degeneration/herniation was lower compared to normal asymptomatic volunteers (40.0° vs. 48.7°). On the other hand, Fei et al. [13] reported there is no difference in PI between young adult (18–35 years old) patients with lumbar disc herniation and the normal population. However, considering long period of time which is probably needed for excessive pressure to influence on disc pathology, there may not be enough time to cause degeneration and LDH in these very young patient groups.
There are very few studies that have used pelvic radius techniques for better understanding of lumbar disc pathology. Therefore, for a more detailed investigation, we included these measurements in the analysis of spinopelvic alignment. The smaller PR-S1 angle appears to have a role in lumbar degenerative spondylolisthesis [16]; however, we could not find any correlation between these parameters and lumbar disc herniation.
Conclusion
We have found a significant association between lumbar disc herniation and pelvic parameters in this investigation and we hope it draws more attention to these kinds of studies in an effort to shed more light to the pathomechanics of degenerative disc disease and identification of individuals who have “high-risk anatomy” for lumbar disc herniation.
References
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar Spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353
Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P (2005) Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am 87-A:260–267
Duval-Beaupère G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Jackson RP, Peterson MD, McManus AC, Hales C (1998) Compensatory spinopelvic balance over the hip axis and better reliability in measuring lateral radiographs of adult volunteers and patients. Spine 23:1750–1767
Oh YM, Eun JP (2015) Clinical impact of sagittal spinopelvic parameters on disc degeneration in young adults. Medicine (Baltimore) 94:e1833. https://doi.org/10.1097/MD.0000000000001833
Wei X, Gengwu L, Chao C, Yifan L, Shang S, Ruixi H, Yunhan J, Xiaodong Z, Zhikun L (2018) Correlations between the sagittal plane parameters of the spine and pelvis and lumbar disc degeneration. J Orthop Surg Res 13:137. https://doi.org/10.1186/s13018-018-0838-6
Strube P, Pumberger M, Sonnow L, Zippelius T, Nowack D, Zahn RK, Putzier M (2018) Association between lumbar spinal degeneration and anatomic pelvic parameters. Clin Spine Surg 31:263–267. https://doi.org/10.1097/BSD.0000000000000660
Lv X, Liu Y, Zhou S, Wang Q, Gu H, Fu X, Ding Y, Zhang B, Dai M (2016) Correlations between the feature of sagittal spinopelvic alignment and facet joint degeneration: a retrospective study. BMC Musculoskelet Disord 17:341. https://doi.org/10.1186/s12891-016-1193-6
Barrey C, Jund J, Noseda O, Roussouly P (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J 16:1459–1467. https://doi.org/10.1007/s00586-006-0294-6
Rajnics P, Templier A, Skalli W, Lavaste F, Illes T (2002) The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop 26:104–108
Yang X, Kong Q, Song Y, Liu L, Zeng J, Xing R (2014) The characteristics of spinopelvic sagittal alignment in patients with lumbar disc degenerative diseases. Eur Spine J 23:569–575. https://doi.org/10.1007/s00586-013-3067-z
Fei H, Li WS, Sun ZR, Ma QW, Chen ZQ (2017) Analysis of spino-pelvic sagittal alignment in young chinese patients with lumbar disc herniation. Orthop Surg 9:271–276. https://doi.org/10.1111/os.12340
Endo K, Suzuki H, Tanaka H, Kang Y, Yamamoto K (2010) Sagittal spinal alignment in patients with lumbar disc herniation. Eur Spine J 19:435–438. https://doi.org/10.1007/s00586-009-1240-1
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20:609–618. https://doi.org/10.1007/s00586-011-1928-x
Zhou Z, Hou C, Li D, Si J (2018) The pelvic radius technique in the assessment of spinopelvic sagittal alignment of degenerative spondylolisthesis and lumbar spinal stenosis. J Orthop Sci 23:902–907. https://doi.org/10.1016/j.jos.2018.06.021
Acknowledgements
This article has been obtained from a thesis (Registered No. 93-01-01-8507) submitted to the Shiraz University of Medical Sciences in partial fulfillment of the requirement for the degree of specialty in orthopaedic surgery. The project is sponsored by Bone and Joint Diseases Research Center, Shiraz University of Medical Sciences.
Funding
This work was supported financially by the Grant No. 93-01-01-8507 from Vice Chancellor for Research of Shiraz University of Medical Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pourabbas Tahvildari, B., Masroori, Z., Erfani, M.A. et al. The impact of spino-pelvic parameters on pathogenesis of lumbar disc herniation. Musculoskelet Surg 106, 195–199 (2022). https://doi.org/10.1007/s12306-020-00693-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00693-5