Abstract
Background
Treatment of complex proximal humeral fractures in the elderly is a challenge and reverse shoulder arthroplasty (RTSA) is now an important alternative to open reduction internal fixation (ORIF) with angular stable plate. The purpose of this study is to compare clinical and radiological outcomes of RTSA and ORIF in the elderly.
Methods
We retrospectively analyzed patients treated for three- or four-part displaced fractures of the proximal humerus. Range of motion, disabilities of the arm, shoulder and hand (DASH) and Constant scores were recorded. X-ray exam in three projections completed the clinical observation at follow-up.
Results
Forty-eight patients were enrolled after a mean follow-up of 37 months: 22 RTSA and 26 ORIF. Mean age at trauma was 74 years. Compared with RTSA patients, ORIF patients had significantly higher mean external rotation (28° vs. 14°) and better results in modal internal rotation (hand at D7 vs. hand at L5-S1). No significant differences were seen in DASH and Constant scores. Avascular necrosis and loss of reduction with varus dislocation of the humeral head were the most frequent causes of revision surgery in ORIF (34.6%) while the revision rate of the RTSA was 9.1%.
Conclusion
In this study, both treatments showed good clinical outcomes, but RTSA resulted in lower revision rate than ORIF. Even if external and internal rotation in RTSA patients were worse than ORIF, they did not affect the patient’s quality of life. So, the reverse arthroplasty seems to be a more reliable treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures represent 6–8% of all fractures [1]. The incidence is steadily increasing due to an ever older population and changes in lifestyle [2, 3].
In elderly patient, these fractures represent a big problem because of pain, loss of function, and high mortality rate [4, 5].
The treatment is still under doubt, especially for 3- and 4-part fractures [6]: complexity of proximal humeral anatomy, surgery complications, and lack of scientific evidences, lead surgeons to make a choice relying on their experience and confidence with a surgical technique.
Three- and four-part fractures usually require a surgical approach, even though some studies suggest that conservative treatment should be considered in ultra-elderly people and in patients with a lot of comorbidities [7].
RTSA was initially recommended in elderly patients with rotator cuff pathology [8]. Subsequently, the use of RTSA has increased a lot during the last decade [9], and it is an optimal alternative to locking plates for the treatment of 3- and 4-part displaced fractures [10].
ORIF offers a reconstruction that respects the shoulder anatomy, but it presents several complications like avascular necrosis of the humeral head, screws cutout, loss of reduction, nonunion, and impingement syndrome [11].
RTSA is less dependent on rotator cuff status and synthesis of tuberosities than hemiarthroplasty, and it is characterized by a faster recovery after surgery [12]. Nevertheless, RTSA may presents complications like scapular notching, instability of the shoulder and the abolition of rotation [13]. Preservation of the tuberosities in anatomic position improves active forward elevation and external rotation as well as patient satisfaction with less complications [14].
We designed this retrospective study in order to compare clinical and radiological outcomes in patients older than 65, who were treated with ORIF or RTSA for 3- or 4-part proximal humeral fractures.
Materials and methods
We selected patients between 65 and 85 years old that were treated with a surgical approach (ORIF or RTSA) between January 2009 and June 2017 for 3- or 4-part proximal humeral fracture (AO-OTA type 11-B2 or 11-C2).
Fracture patterns were evaluated by two independent operators using X-rays (true AP view and Y-view) that were performed when the patient arrived at the hospital after trauma.
A CT-scan exam with 3D reconstruction was performed before surgery to characterize fracture patterns.
We excluded patients that presented a follow-up shorter than 12 months, cases of bifocal humeral fractures, patients with neurologic diseases or systemic comorbidities that could compromise clinical results. We also excluded patients who previously underwent surgery to the same shoulder in the past, and the ones who were treated after 10 days from their trauma.
We selected 63 patients operated at Clinical Orthopedics, University Politecnica delle Marche (AN).
Out of these 63 patients, 10 dropped out of the study due to death, together with 5 more patients who did not accept the clinical-radiological follow-up.
In the end, our retrospective comparative study was based on 48 patients.
We filled in a demographic form for each patient, in which we reported: date of birth, gender, weight, height, date of trauma, age at surgery time, total months of follow-up, and injured side.
Functional results were assessed using the Constant–Murley score (0–100 points). Overall subjective patient’s satisfaction was evaluated using the disabilities of the arm, shoulder and hand (DASH) score (100–0 points).
Besides, we took X-rays in three projections (true AP view, Y-view and axillary-view) just before the clinical evaluation.
An expert orthopedic evaluated each patient and two independent observers evaluated the X-rays exams during the follow-up.
Scapular notching was graded according to Sirveaux et al. [12] classification.
The 48 patients were divided into two groups depending on the kind of treatment.
The first group was composed of patients who were treated with PHILOS plate (Synthes, Paoli, PA, USA).
The second group was composed of patients who were treated with reverse total shoulder arthroplasty (Lima Corporate, San Daniele Del Friuli, Italy).
The choice of the treatment depended on the type of fracture, the presence of head splitting, bone stock quality, the presence of rotator cuff tear arthropathy, glenohumeral osteoarthritis, and function of the deltoid muscle.
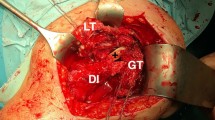
An upper-limb specialist operated all patients. The patient, after regional anesthesia, was placed in beach chair position. A deltoid-pectoral approach was used for reducing the fracture and positioning the plate. The upper part of the plate was positioned at least 1 cm far from the great tuberosity apex and lateral from the bicipital groove in order to avoid interferences with the anterior branch of the anterior circumflex humeral artery. We were also really careful about positioning inferior screws in order to give a medial support to the surgical humeral neck [15].
Humeral tuberosities, when possible, were fixed in their anatomical position using an intraosseous suture with non-absorbable wires (2/0 Ethibond Suture, Ethicon Inc., USA).
We employed a deltoid-pectoral approach in patients treated by RTSA and then, after removing humeral head fragments, we passed non-absorbable wires (2/0 Ethibond Suture, Ethicon Inc., USA) between tendon-bone junctions of the great and less tuberosity.
The glenoid component (36 or 40 mm of diameter) was implanted with an inferior tilt of 10°, and it was fixated to the scapula using two screws. Humeral component was positioned with a version of 0°, and we adjusted the height after taking some articular stability tests. The humeral component was never cemented.
Humeral tuberosities were sutured one to the other and then to the prothesis neck, respecting their anatomical position. It was impossible to fix tuberosities in 5 cases due to the poor bone stock or to the excessive bone fragmentation.
The rehabilitation program, in patient treated with plate, required a sling immobilization of the limb for 4 weeks. Passive shoulder exercises without gravity and active elbow movements were allowed on the very first postoperative day. After 4 weeks, progression to active assisted motion was started avoiding internal and external rotation until 40 days after surgery.
The rehabilitation program in patient treated with RTSA required a sling immobilization for 2 weeks, allowing passive movements of the shoulders and active elbow movements from the first postoperative day. After 2 weeks, progression to active assisted shoulder movements were allowed avoiding internal and external rotation until 40 days after surgery.
Data were collected and organized using Excel (Microsoft, Redmond, WA, USA).
Categorical variabilities were expressed in numbers and percentages. Continuous variabilities were expressed by averages and standard deviation (DS).
Data from two groups were compared using Mann–Whitney test, t test, and Fisher exact test when appropriate.
Statistical analyses were made using SPSS (version 21.0; IBM, Armonk, NY, USA). A p < 0.05 was considered as significant.
Results
The patient demographics are reviewed in Table 1. The mean ages of patients and the follow-up periods were similar with no significant difference between groups (p > 0.05).
In the group treated with locking plate, 3-part fractures were present in 9 patients, 15 patients had a 4-part fracture, and the remaining 2 patients had fracture with dislocation.
In the group treated with RTSA, 5 patients had a 3-part fracture, 14 patients had 4-part fracture, and the rest 3 cases had fracture with dislocation.
The mean DASH score in patients treated with ORIF was 18.99 ± 14.13, and the mean Constant–Murley score was 65.85 ± 15.73. The ORIF group average values were: abduction 105.5° ± 21.02°, forward flexion 125.75° ± 33.13°, external rotation 28° ± 14.18°, and modal internal rotation was D7.
The patients treated with RTSA had a mean DASH score of 25.1 ± 11.66 and a mean Constant–Murley score of 63.65 ± 12.14. The average values were: abduction 109.75° ± 20.09°, forward flexion 124.5° ± 20.45°, external rotation 14.25° ± 13.69°, and modal internal rotation was L5-S1.
We did not find any statistically significant difference between groups about Constant–Murley score and DASH score and neither about abduction and forward flexion (p > 0.05).
We found a statistically significant difference between two groups for external rotation (p = 0.0059) that was better in patients treated with ORIF. Also, it offered better results for internal rotation (Table 2).
The group treated with plate was characterized by 5 cases of avascular necrosis of the humeral head (19.2%), in particular, 4 cases were complete necrosis and 1 case was partial necrosis.
We observed 3 cases (11.5%) of loss of reduction with varus displaced humeral head (1 of those had a screw cut-out) and 1 case (3.8%) of deep infection. Also, we registered 2 cases (7.6%) of great tuberosity malunion and 2 cases (7.6%) of subacromial plate impingement.
The group treated with RTSA was characterized by 1 case (4.5%) of instability, 1 case (4.5) of deep infection and 7 cases (31.8%) of inferior scapular notching (grade 1 or 2). We also registered 5 cases (22.7%) of great tuberosity malunion.
In the ORIF group, 3 out of 5 patients with necrosis required a surgical revision with reverse arthroplasty because of the persistent pain and poor ROM. In 2 cases of varus dislocation, a second reduction and fixation with plate was needed. In the patient with screw cutout, the removal of internal devices after fracture healing was sufficient. In the patient with deep infection, a two-step surgery was necessary, and in patients with impingement, the plates were removed after fracture healing (Table 3). The revision rate was 34.6% in the ORIF group.
In the RTSA group, the patient with instability of the arthroplasty required implant revision. In the patient with deep infection, a two-step revision surgery was needed (Table 4). The revision rate was 9.1% in the RTSA group.
At the end, we concluded that the revision rate was significantly higher in the group treated with ORIF than the group treated with RTSA (p = 0.045).
Discussion
The best treatment for 3- and 4-part dislocated fractures in elderly patients remains under doubt. The most frequent operative treatments are the open reduction and internal fixation, and the reverse shoulder arthroplasty.
However, in the literature, we found only two works that compared these two techniques in patient over 65.
Giardella et al. [16] obtained a better Constant–Murley score and forward flexion with RTSA; while they achieved a better external rotation in patients with angular stable plate. The authors concluded that RTSA is one of the best treatments in elderly patients, in which rotator cuff is frequently poor and degenerated.
Chalmers et al. [11] found that RTSA offers better results in forward flexion, but they did not find any difference in quality life scores neither in other evaluated ROMs.
In our study, we reached great DASH and Constant–Murley scores with both the techniques. We did not find any significant difference in abduction and forward flexion among the groups, but ORIF offers better results in external and internal rotation. In fact, it achieved 28° ± 14.18° during external rotation, while RTSA only obtained 14.25° ± 13.69°. The patients treated with plate usually have an internal rotation that reached D7, and patients treated with RTSA achieved L5-S1.
There are a lot of factors that could influence rotations in patient with reverse arthroplasty [12, 17,18,19,20,21]. In particular, in our study, the high index of great tuberosity malunion (22.7%) played an important role. We have also to consider that the synthesis of the tuberosities sometimes was not possible due to the poor bone stock or to the excessive fracture comminution.
However, osteosynthesis with plate remains a challenge even for superior limb expert orthopedics. In fact, even though new implants and materials are developed, complications and revision rate remain very high [21,22,23].
Du et al. meta-analysis [23] compared various types of treatment including RTSA and ORIF. In this metanalysis, RTSA has higher Constant–Murley score, and it also has lower revision rates in comparison with plate, hemiarthroplasty, and conservative approach. In the same metanalysis, the plate is characterized by the worst results.
AVN incidence rate is between 3 and 68% [24, 25], and it depends a lot on the fracture pattern, metaphyseal extension, and calcar integrity [26]. We have also to consider the important damage that the surgeon can do to the vascular system during the reduction with ORIF [21].
We registered several AVN cases (19.2%) in our study, and it was the most frequent cause leading to an implant revision.
The second most frequent complication in patients treated with plate was the loss of reduction with varus dislocation of the humeral head (11.5%), and in one case among those, we observed a screw cutout. In order to avoid this complication, we suggest to follow tips and strategies that the literature gives us: supporting the medial hinge, restoring the cervical-diaphyseal angle, putting screws on calcar, using cement augmentation [21, 27]. Even if the surgeon follows all these tips, the loss of reduction incidence rate is still elevated.
About the RTSA procedure, there was a single case of dislocation (4.5%) that was in line with the literature [11]. The difficulty in preventing dislocation lies in the fact of having to establish the correct height of the humeral stem in the presence of a subverted anatomy, and therefore, the risk of an unstable or a rigid shoulder is high.
The group treated with ORIF was characterized by high revision rate (34.6%) and that confirms what we knew [21, 28,29,30,31,32,33].
Reverse shoulder arthroplasty was more reliable, with a revision rate of 9.1%.
Many plate revisions (33%) required a conversion to reverse prosthesis. However, RTSA, as a revision treatment, is described as definitely worse if compared with a case in which it is used as first implant [34].
Summarizing the present study could represent a valid guide for the choise of the treatment of complex proximal humeral fractures. Indeed, RTSA represents a safe and effective option in elderly with a lower complication rate than ORIF. However, this study has several limitations: (1) small sample size for each group; (2) it is a retrospective and non-randomized study; (3) only medium-term follow-up was obtained; (4) we lost some patients during the follow-up.
Further prospective studies with a higher sample size and a longer follow-up are needed in order to more properly define the role of reverse shoulder arthroplasty in this kind of fractures.
Conclusions
We confirm good clinical results in patients treated both with open reduction and internal fixation using an angular stable plate and with the reverse shoulder arthroplasty for 3- and 4-part proximal humeral fractures in patients older than 65 years. Even if external and internal rotation in RTSA patients were worse than the ORIF group, they did not affect the patient’s quality of life.
However, osteosynthesis with locking plate is characterized by a higher revision rate than the group treated with RTSA. Therefore, the reverse shoulder arthroplasty seems to be a more reliable treatment.
References
Court-Brown CM, Garg A, McQueen MM (2001) The epidemiology of proximal humeral fractures. Acta Orthop Scand 72(4):365–371. https://doi.org/10.1080/000164701753542023
Bengner U, Johnell O, Redlund-Johnell I (1988) Changes in the incidence of fracture of the upper end of the humerus during a 30-year period. A study of 2125 fractures. Clin Orthop Relat Res 231:179–182
Palvanen M, Kannus P, Niemi S, Parkkari J (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442:87–92
Fink HA, Ensrud KE, Nelson DB, Kerani RP, Schreiner PJ, Zhao Y et al (2003) Disability after clinical fracture in postmenopausal women with low bone density: the fracture intervention trial (FIT). Osteoporos Int 14(1):69–76. https://doi.org/10.1007/s00198-002-1314-y
Hodgson S (2006) Proximal humerus fracture rehabilitation. Clin Orthop Relat Res 442:131–138
Handoll HH, Ollivere BJ (2010) Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000434.pub2
Zyto K (1998) Non-operative treatment of comminuted fractures of the proximal humerus in elderly patients. Injury 29(5):349–352
Cuff D, Clark R, Pupello D, Frankle M (2012) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am 94(21):1996–2000
Porcellini G, Combi A, Merolla G, Bordini B, Stea S, Zanoli G, Paladini P (2018) The experience of the RIPO, a shoulder prosthesis registry with 6-year follow-up. Musculoskelet Surg 102(3):273–282
Fjalestad T, Iversen P, Hole MO, Smedsrud M, Madsen JE (2014) Clinical investigation for displaced proximal humeral fractures in the elderly: a randomized study of two surgical treatments: reverse total prosthetic replacement versus angular stable plate Philos (The DELPHI-trial). BMC Musculoskelet Disord 15:323. https://doi.org/10.1186/1471-2474-15-323
Chalmers PN, Slikker W 3rd, Mall NA, Gupta AK, Rahman Z, Enriquez D et al (2014) Reverse total shoulder arthroplasty for acute proximal humeral fracture: comparison to open reduction-internal fixation and hemiarthroplasty. J Shoulder Elbow Surg 23(2):197–204. https://doi.org/10.1016/j.jse.2013.07.044
Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86(3):388–395
Gallinet D, Clappaz P, Garbuio P, Tropet Y, Obert L (2009) Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res 95(1):48–55
Luciani P, Farinelli L, Procaccini R, Verducci C, Gigante A (2019) Primary reverse shoulder arthroplasty for acute proximal humerus fractures: A 5-year long term retrospective study of elderly patients. Injury 50(11):1974–1977
Kralinger F, Unger S, Wambacher M, Smekal V, Schmoelz W (2009) The medial periosteal hinge, a key structure in fractures of the proximal humerus: a biomechanical cadaver study of its mechanical properties. J Bone Jt Surg Br 91(7):973–976. https://doi.org/10.1302/0301-620X.91B7.21857
Giardella A, Ascione F, Mocchi M, Berlusconi M, Romano AM, Oliva F et al (2017) Reverse total shoulder versus angular stable plate treatment for proximal humeral fractures in over 65 years old patients. Muscles Ligaments Tendons J 7(2):271–278. https://doi.org/10.11138/mltj/2017.7.2.271
Acevedo DC, Vanbeek C, Lazarus MD, Williams GR, Abboud JA (2014) Reverse shoulder arthroplasty for proximal humeral fractures: update on indications, technique, and results. J Shoulder Elbow Surg 23(2):279–289. https://doi.org/10.1016/j.jse.2013.10.003
Boileau P, Watkinson DJ, Hatzidakis AM, Balg F (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 14:147S–161S. https://doi.org/10.1016/j.jse.2004.10.006
Bufquin T, Hersan A, Hubert L, Massin P (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Jt Surg Br 89(4):516–520. https://doi.org/10.1302/0301-620X.89B4.18435
Jobin CM, Brown GD, Bahu MJ, Gardner TR, Bigliani LU, Levine WN et al (2012) Reverse total shoulder arthroplasty for cuff tear arthropathy: the clinical effect of deltoid lengthening and center of rotation medialization. J Shoulder Elbow Surg 21(10):1269–1277. https://doi.org/10.1016/j.jse.2011.08.049
Jobin CM, Galatz LM (2012) Proximal Humerus Fractures: Pin, Plate, or Replace? Semin Arthroplast 23(2):74–82. https://doi.org/10.1053/j.sart.2012.03.003
Boesmueller S, Wech M, Gregori M, Domaszewski F, Bukaty A, Fialka C et al (2016) Risk factors for humeral head necrosis and non-union after plating in proximal humeral fractures. Injury 47(2):350–355. https://doi.org/10.1016/j.injury.2015.10.001
Du S, Ye J, Chen H, Li X, Lin Q (2017) Interventions for Treating 3- or 4-part proximal humeral fractures in elderly patient: A network meta-analysis of randomized controlled trials. Int J Surg 48:240–246. https://doi.org/10.1016/j.ijsu.2017.09.002
Gerber C, Hersche O, Berberat C (1998) The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elbow Surg 7(6):586–590
Jost B, Spross C, Grehn H, Gerber C (2013) Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg 22(4):542–549. https://doi.org/10.1016/j.jse.2012.06.008
Hertel R, Hempfing A, Stiehler M, Leunig M (2004) Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 13(4):427–433. https://doi.org/10.1016/S1058274604000795
Laux CJ, Grubhofer F, Werner CML, Simmen H-P, Osterhoff G (2017) Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res. https://doi.org/10.1186/s13018-017-0639-3
Aguado HJ, Mingo J, Torres M, Alvarez-Ramos A, Martin-Ferrero MA (2016) Minimally invasive polyaxial locking plate osteosynthesis for 3–4 part proximal humeral fractures: our institutional experience. Injury 47(Suppl 3):S22–S28. https://doi.org/10.1016/S0020-1383(16)30602-7
Fattoretto D, Borgo A, Iacobellis C (2016) The treatment of complex proximal humeral fractures: analysis of the results of 55 cases treated with PHILOS plate. Musculoskelet Surg 100(2):109–114. https://doi.org/10.1007/s12306-015-0395-7
Frangen TM, Muller EJ, Dudda M, Arens S, Muhr G, Kalicke T (2007) Proximal humeral fractures in geriatric patients Is the angle-stable plate osteosynthesis really a breakthrough? Acta Orthop Belg 73(5):571–579
Gupta AK, Harris JD, Erickson BJ, Abrams GD, Bruce B, McCormick F et al (2015) Surgical management of complex proximal humerus fractures-a systematic review of 92 studies including 4500 patients. J Orthop Trauma 29(1):54–59. https://doi.org/10.1097/BOT.0000000000000229
Tepass A, Rolauffs B, Weise K, Bahrs SD, Dietz K, Bahrs C (2013) Complication rates and outcomes stratified by treatment modalities in proximal humeral fractures: a systematic literature review from 1970–2009. Patient Saf Surg 7(1):34. https://doi.org/10.1186/1754-9493-7-34
Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg 18(6):837–844. https://doi.org/10.1016/j.jse.2009.06.004
Dezfuli B, King JJ, Farmer KW, Struk AM, Wright TW (2016) Outcomes of reverse total shoulder arthroplasty as primary versus revision procedure for proximal humerus fractures. J Shoulder Elbow Surg 25(7):1133–1137. https://doi.org/10.1016/j.jse.2015.12.002
Acknowledgements
None
Funding
This manuscript was not supported financially by any funding agency.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Pierfrancesco Luciani and Francesco Pettinari collected the patient data. Roberto Procaccini performed the surgeries. Marco Rotini and Pierfrancesco Luciani analyzed the patient data. Antonio Gigante supported Pierfrancesco Luciani and Marco Rotini with analyzing and interpreting the data. Francesco Pettinari wrote the manuscript. All authors helped write the manuscript and have read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board and performed in accordance with 1964 Helsinki Declaration.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luciani, P., Procaccini, R., Rotini, M. et al. Angular stable plate versus reverse shoulder arthroplasty for proximal humeral fractures in elderly patient. Musculoskelet Surg 106, 43–48 (2022). https://doi.org/10.1007/s12306-020-00669-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00669-5