Abstract
Introduction
The employment of reverse shoulder arthroplasty for dislocated proximal humerus fractures of elderly patients becomes increasingly relevant. The standard inclination angle of the humeral component was 155°. Lately, there is a trend towards smaller inclination angles of 145° or 135°. Additionally, there has been an increased focus on the lateralization of the glenosphere. This retrospective comparative study evaluates clinical and radiological results of patients treated for proximal humerus fractures by reverse shoulder arthroplasty with different inclination angles of the humeral component, which was either 135° or 155°. Additionally, a different lateral offset of the glenosphere, which was either 0 mm or 4 mm, was used.
Methods
For this retrospective comparative analysis, 58 out of 66 patients treated by reverse total shoulder arthroplasty for proximal humerus fractures were included. The minimum follow-up was 24 months. Thirty (m = 3, f = 27; mean age 78 years; mean FU 35 months, range 24–58 months) were treated with a standard 155° humeral component and a glenosphere without lateral offset (group A), while 28 patients (m = 2, f = 26; mean age 79 years; mean FU 30 months, range 24–46 months) were treated with a 135° humeral component and a glenosphere with a 4 mm lateral offset (group B). We determined range of motion, Constant score, and the American Shoulder and Elbow Surgeons Shoulder score as clinical outcomes and evaluated tuberosity healing as well as scapula notching.
Results
Neither forward flexion (A = 128°, B = 121°; p = 0.710) nor abduction (A = 111°, B = 106°; p = 0.327) revealed differences between the groups. The mean Constant Score rated 63 in group A, while it was 61 in group B (p = 0.350). There were no differences of the ASES Score between the groups (A = 74, B = 72; p = 0.270). There was an increased risk for scapula notching in group A (47%) in comparison to group B (4%, p = 0.001). Healing of the greater tuberosity was achieved in 57% of group A and in 75% of group B (p = 0.142). The healing rate of the lesser tuberosity measured 33% in group A and 71% in group B (p = 0.004).
Conclusions
Both inclination angles of the humeral component are feasible options for the treatment of proximal humerus fractures in elderly patients. Neither the inclination angle nor the lateral offset of the glenosphere seem to have a relevant influence on the clinical outcome. The healing rate of the lesser tuberosity was higher in implants with a decreased neck-shaft angle. There is an increased risk for scapula notching, if a higher inclination angle of the humeral component is chosen.
Level of evidence
III. Retrospective comparative study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the humeral head are encountered frequently in the aging population [1,2,3]. In particular, female patients with osteoporosis have an increased risk of complex and displaced fractures [4]. While undisplaced proximal humerus fractures (PHF) in elderly patients should be treated conservatively, displaced fractures may be treated by osteosynthesis (locking plate, nail), anatomic fracture hemiarthroplasty or reverse total shoulder arthroplasty (RTSA).
In elderly patients, osteosynthesis may lead to specific complications such as secondary dislocation, screw cut out, hardware failure, avascular necrosis, non-union, stiffness and rotator cuff insufficiency [5]. Anatomic fracture hemiarthroplasty is related to inferior and less predictable clinical results when compared to RTSA [6, 7]. The main reason for less predictable results of fracture hemiarthroplasty is necrosis or malunion of the tuberosities, in particular in elderly patients with poor bone quality. While tuberosity non-union or malunion may cause inferior results in cases of RTSA implanted for PHFs [8], it may result in instability and even pseudoparalysis in cases of anatomic fracture hemiarthroplasty [6].
Due to known risks of humeral head-preserving treatment options or fracture hemiarthroplasty, reverse shoulder arthroplasty has become a widely used treatment option for complex and displaced proximal humerus fractures in elderly patients [9,10,11,12,13]. Advantages of primary RTSA in cases of displaced PHF are early rehabilitation, early pain relief and a definitive treatment option. Disadvantages are the risks for typical problems and complications of RTSA such as infection, dislocation, aseptic loosening, scapular notching (SN) or nerve palsy [14].
RTSA was introduced by Paul Grammont and worked with a standard neck-shaft angle or inclination angle (IA) of the humeral component of 155° [15]. This type of RTSA leads to a medialized and distalized center of rotation of the glenohumeral joint, which enables the deltoid muscle to perform abduction and forward flexion [16], but which is also known for a poor function concerning internal and external rotation [17]. A major concern of the Grammont style RTSA is SN [18].
Lower IAs of the humeral component of 145° or 135° potentially lead to better external and internal rotation and increased adduction. They also decrease the risk for scapular notching [19, 20]. The main biomechanical reason for better internal and external rotation and increased adduction capacity is a reduced friction between the scapular pillar and the polyethylene insert of the humeral component [16]. Tuberosity healing improves, if a lower IA is employed in PHFs [21].
In addition to IA, there has been increasing interest in the lateral offset (LO) of the glenosphere. An increased LO of the glenosphere results in a longer neck of the scapula, thus decreasing the risk of scapular notching [22]. Furthermore, the increased LO potentially achieves better rotation, abduction and stability as well as a reduced risk for glenohumeral impingement [22,23,24,25,26,27].
Both, higher stability, better rotation and a reduced risk for scapular notching are comprehensive reasons to implant RTSA with smaller IAs of the humeral component and a larger LO of the glenosphere. To date, only few clinical data dealing with the IA and the LO of RTSA in context of PHF are available [13, 21, 28].
This retrospective study assesses clinical and radiological results of a standard 155° IA humeral component without LO of the glenosphere in comparison with a 135° IA humeral component in combination with a 4-mm lateralized glenosphere in context of displaced PHFs in elderly patients. Our hypothesis was, that a lower IA and an increased LO lead to better rotatory function of the shoulder as well as a decreased rate of SN. We furthermore assumed that humeral implants with lower IAs lead to improved tuberosity healing in spite of a lateralized glenosphere.
Materials and methods
Patients:
For this retrospective comparative analysis, we compared two different types of RTSA, one with a standard neck-shaft angle of 155° and one with a decreased neck-shaft angle of 135° with 4 mm LO of the glenosphere. These two different prosthetic designs were employed because of a changed preference of the senior surgeon of this study.
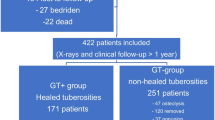
Fifty-eight out of 66 patients treated by RTSA for PHFs were included. Five patients were lost to follow-up due to severe general disease (n = 3) and unwillingness to take part in a study (n = 3). Two patients with preexisting glenohumeral osteoarthrtitis were excluded from this study. Inclusion criteria and exclusion criteria are summarized in Table 1.
Patients were matched for gender and age. The minimum follow-up was 24 months. Thirty (m = 3, f = 27; mean age 78 years; mean FU 35 months, range 24–58 months) were treated with a standard 155° humeral component (group A), while 28 patients (m = 2, f = 26; mean age 79 years; mean FU 30 months, range 24–46 months) were treated with a 135° humeral component (group B). The implant used in group A was the Delta Xtend prostehesis (DePuy, Warsaw, Indiana, USA), while the Universe Reverse prosthesis (Arthrex, Naples, Florida, USA) was used in group B. The stem was cemented in most of the patients in group A (83%) and in a minority of the patients of group B (11%). All patients of group B were treated with a 4-mm lateralized glenosphere. Reconstruction of lesser tuberosity (LT) and greater tuberosity (GT) was carried out in all patients.
In group A, a 42-mm glenosphere was implanted in seven patients, while the remaining 23 patients received a 38-mm glenosphere. In group B, a 39-mm glenosphere was used in ten cases, while the remaining 18 patients were treated with a 36-mm glenosphere.
Surgical technique
All patients were operated by a single surgeon (J.S.) via a standard deltopectoral approach. The surgical technique (approach and tuberosity repair) did not differ between the two different implant types. Tuberosity repair was performed accordingly to the technique described by Sirveaux et al. [29]. The rotator cuff was assessed clinically during the surgical procedure. Patients with complete rotator cuff tears were excluded from the study.
After identification of the bicipital groove, the LT and the subscapularis tendon were mobilized using a scalpel and an osteotome. The supraspinatus tendon was excised, before the GT was mobilized with and osteotome. After extracting the humeral head, the tuberosities were armed with non-absorbable sutures (Fig. 1). Shaft preparation was performed using reamers and broaches. The retroversion of the humeral component measured 10° in both groups. Subsequently, the glenoid was exposed with Hohmann retractors and prepared with specific reamers and drills via a central guide pin, which had previously been placed using a jig. While the baseplate in group A was positioned inferiorly to avoid SN, the anatomically formed baseplate of group B was positioned flush with the native glenoid. In group A, an eccentric glenosphere was used in all cases to provide an inferior overhang. In group B, all glenospheres had a 4-mm LO but no eccentricity. After implantation of trials and trial reduction as well as checking for range of motion and stability, the original prosthesis was implanted. Stems were cemented, in cases of poor bone quality and if press-fit stability was not achieved with the trial stem.
Tuberosity reconstruction was performed using non-absorbable suture tapes in all cases. Three sutures were used to reattach the GT to the metaphyseal humeral component of the prosthesis (Fig. 2). One suture was used to reattach the LT. After reattachment of the tuberosities, two sutures that were placed into holes in the proximal humeral diaphysis were passed through the infraspinatus tendon, respectively, the subscapularis tendon and tied tightly to prevent the tuberosities from cranial migration and to complete tuberosity reconstruction (Fig. 3).
Postoperatively all patients were immobilized in an abduction sling for 3 weeks. During this period, patients were allowed to remove the sling during personal hygiene and food intake. Lymphatic drainage and local ice were applied consequently in the first week. After three weeks, patients were allowed to start assisted active exercises until 90 degress of forward flexion and abduction. External rotation was allowed until 20°. After 6 weeks, patients were allowed to move their affected shoulder pain-adapted, without any restrictions under supervision of a physiotherapist.
Clinical and radiological assessment
Preoperatively all patients were studied with standard radiographs (anteroposterior, and axial view), computer tomography and the Constant-Murley Score (CS). Fatty infiltration of the rotator cuff was graded according to the Goutallier classification on sagittal computer tomography scans.
The Neer classification system and the Orthopaedic Trauma Association (OTA) classification system were used to categorize the fracture type [30, 31]. Postoperatively patients were assessed with radiographs (a.p. and sagittal view). Proper reconstruction of the greater tuberosity (GT) was achieved, if the greater tuberosity was clearly visible on a.p. radiographs with direct contact to the lateral metaphyseal component of the humeral implant.
At follow-up, the CS, the ASES Score, range of motion (ROM) and radiographs were (a.p. and axial view) were investigated. The pain level was identified using a visual analogue scale (VAS) between zero and ten. The CS was adjusted to age and gender by comparing the absolute values to mean standard values as described by Thomas et al. [32]. X-rays were checked for SN, heterotopic ossifications, stress shielding and radiolucency of the baseplate and the shaft by an independent shoulder surgeon. The grade of SN was rated with the Sirveaux classification [33]. Healing of the GT was rated on a.p. radiographs. If the GT was clearly visible on a.p. radiographs with direct contact to the lateral metaphyseal component of the humeral implant, it was considered healed. If the distance between the humeral component and the GT was higher than 5 mm, the GT was considered dislocated. The GT was considered resorbed if it was neither visible on a.p. nor on axial x-rays. Analogue to the GT healing of the lesser tuberosity (LT) was rated on axial X-rays.
Statistical analysis
Statistical analysis was processed with SPSS 25.0 software (IBM Corp, Armonk, NY, USA). Two independent samples were compared by Mann–Whitney U test. Paired samples were investigated with the Wilcoxon test. Cross tables were assessed with the Chi Square test. A difference of p < 0.05 was considered to be statistically significant.
A power analysis was performed using PASS 14.0.8 software (NCSS, East Kaysville, Utah, USA). Given a significance level of 5%, a Cohens’s d effect size of 1 and statistical power of 80% a minimum sample size of 34 patients was mandatory.
Results
Preoperative findings
All patients suffered from displaced 3- or 4-part fractures according to the Neer classification. Eleven patients of group A and ten patients of group B were treated for 3-part fractures, while 19 patients of group A and 18 patients of group B were operated because of a displaced 4-part fracture.
The OTA classification showed a type 11-B3 fracture in 11 patients of each group. Type 11-C1 (group A = 12 and group B = 10), type 11-C2 (group A = 3 and group B = 4) and type 11-C3 (group A = 4 and group B = 3) were observed in both groups.
The preoperative Constant score did not differ between group A and group B (9.6 vs. 9.9; p = 0.777).
Clinical results
At follow-up, the CS had improved in each group (group A: 10 vs. 63; p < 0.001 and group B: 10 vs. 61; p < 0.001). The clinical results were similar in both groups concerning the CS (group A = 63 vs. group B = 61; p = 0.350), the adjusted CS (group A = 78% vs. group B = 74%; p = 0.468) and the ASES score (group A = 75 vs. group B = 72; p = 0.270). There were comparable results between the two groups for ROM, pain level and abduction force. The clinical results are summarized in Table 2. In general, greater tuberosity healing did not affect the clinical outcome concerning active range of motion and clinical scores (Table 3).
Radiological results
Radiological reconstruction of the GT was achieved in 25 patients of group A (83%) and 26 patients of group B (93%) immediately after the surgical procedure.
At follow-up, the rate of healed GTs was 57% (n = 17) in group A and 75% (n = 21) in group B (p = 0.142). LTs healed in an anatomic position in 33% (n = 10) of the patients of group A and in 71% (n = 20) of the patients of group B (p = 0.004).
The rate of SN was higher in group A (47%) in comparison to group B (4%, p = 0.001). Overall, SN did not influence the clinical outcome regarding the CS (no notching: 63 vs. SN: 61; p = 0.794) and the ASES score (no notching: 74 vs. SN: 73; p = 0.456). In group A, the grade of SN varied between 1 and 3. Radiolucency around the humeral component was detected in two patients of group A (7%) and one patient of group B (4%). Stress shielding at the proximal humerus was observed in one patient of group A (3%) and two patients of group B (9%).
Heterotopic ossifications were observed in both groups (group A = 7% vs. group B = 9%). The heterotopic ossifications in group A were located at the triceps origin. In group B, one heterotopic ossification was found at the triceps origin, while the other was located in the area of the infraspinatus tendon in the axial view. Radiologic results are presented in Table 4.
Figures 4a, 5a demonstrate anteroposterior radiographs (a. p.) of 4-part PHFs, which were treated by RTSA. Figures 4b, 5b demonstrate a. p. at follow-up with healed GTs of a group A and group B.
(a and b): Preoperative anteroposterior radiograph of a 4-part fracture (OTA 11-C1) of the right proximal humerus of a 77-year-old female patient (a). The patient was treated with a reversed shoulder prosthesis with a humeral inclination angle of 155° and standard glenosphere with caudal eccentricity. The white arrow shows the healed greater tuberosity at follow-up (b)
(a and b): Preoperative anteroposterior radiograph of a 4-part fracture (OTA 11-C1) of the left proximal humerus of an 80-year-old female patient (a). The patient was treated with a reversed shoulder prosthesis with a humeral inclination angle of 135° and a 4-mm lateral offset of the glenosphere. The anteroposterior radiograph at follow-up shows grade 1 scapular notching (SN), stress shielding at the proximal lateral diaphysis (SS) and a healed greater tuberosity at follow-up (b)
Complications
The overall complication rate was 13% (n = 4) in group A and 11% (n = 3) in group B. One patient of group B needed a two-staged exchange of the RTSA to a hemi-prosthesis due to an infection with cutibacterium acnes. Another patient of group B suffered from a low-grade infection caused by staphylococcus epidermidis. After explantation of the prosthesis, this patient did not wish to undergo another surgical procedure. Minor neurologic complications with intermitting hypoesthesia occurred in one patient of each group. Two patients of group A required surgical revision in the early postoperative period. One patient was revised because of hematoma, while another patient was revised because of recurrent prosthetic instability. This patient was treated with a larger inlay and remained stable after the revision procedure.
Discussion
Since numerous different designs for RTSA are available on the market with different humeral inclination, inferior glenosphere eccentricity, glenosphere size, LO and medialized humeral trays [34], it is almost impossible to find the optimal implant combination for different indications of RTSA. Primarily invented for cuff tear arthropathy, RTSA is now frequently used for primary osteoarthritis and also PHFs in elderly patients.
Biomechanical and computer model studies evaluated different designs of RTSA [17, 20, 23, 35, 36]. These studies are very helpful to understand theoretical advantages and disadvantages of each combination. To date, there is a lack of clinical results of comparative studies concerning different RTSA implant designs in context of PHFs. This is why our study may be helpful to understand the role of the IA on the humeral side and the LO on the glenoid side.
The healing rate of the tuberosities is a highly debated topic in RTSA in context of PHFs. Healing of the greater tuberosity has shown positive effects on clinical outcome and range of motion in different studies [8, 13, 21, 37], while excision of the GT may even lead to increased instability rates [8]. Potentially, a reconstructed GT facilitates external rotation, if the infraspinatus tendon is intact. However, it is still unclear if external rotation is improved in cases of reconstructed GTs following RTSA for PHFs [8, 21, 37].
While different neck-shaft angles have been studied frequently in context of PHF, as demonstrated in a recent review by O’Sullivan et al. [21], the LO has not been of major interest in the literature. Because of a combination of a 4-mm lateralized glenosphere and a decreased neck-shaft angle of 135° in group B our study may add new information to the existing literature. The most important finding of our clinical trial is that neither the IA of the humeral component nor the LO of the glenosphere seem to have an effect on the clinical outcome regarding the CS (group A = 63.1 vs. group B = 60.5; p = 0.350) and the ASES score (group A = 75.0 vs. group B = 71.8; p = 0.270). Some authors reported comparable or better clinical results with mean Constant scores between 60 and 71 points [10,11,12,13, 38, 39]. Other authors observed a lower mean CS between 44 and 55 points [9, 40, 41]. O’Sullivan et al. compared three different IAs (155°, 145°, 135°) in a literature review [21]. In line with our results, these authors found no differences between the different implants.
Tuberosity healing
There is still a debate if tuberosity healing is beneficial for the clinical outcome of RTSA employed for PHFs. While several studies reported better clinical outcomes in cases of GT reconstruction [8, 13, 21, 37, 42], some authors could not confirm a clinical or biomechanical relevance of tuberosity reconstruction [28, 43, 44]. Even though GT healing was not affected by the implant design in our study, LT healing was better in patients with a higher LO and a lower IA. O’Sullivan et al. assumed that implants with a lower IA lead to reduced distalization of the proximal humerus, which may be beneficial for tuberosity healing [21]. These authors reported improved healing rates of the GT in a literature review in cases with a lower IA. We observed a higher healing rate of the GT in patients treated with a lower IA and a higher LO. However, this difference was not significant. The increased LO might be a reason, why the healing rate of the GT in patients treated with a lower IA was not significantly higher than in standard Grammont style implants. An increased LO theoretically leads to an increased soft tissue tension [17] and thus to an increased tension of the rotator cuff and the reconstructed tuberosities. This circumstance may be disadvantageous for tuberosity healing.
Our sample size was too small to allow for a statistical comparison of tuberosity healing within the groups. We noted a higher healing rate of the LT in patients with a lower IA, but we did not notice any clinical relevance, since internal or external rotation was not affected.
It is of note, that proper reconstruction of the GT was achieved in only 83% of the patients of group A and in 93% of the patients of group B on immediate postoperative radiographs. This finding demonstrates that poor bone quality or an insufficient reconstruction technique may lead to failed GT reconstruction immediately after the surgical procedure. Even if the GT was reconstructed adequately, radiological healing of the GT was not always achieved at follow-up in patients of both groups (GT healing rate group A = 57% and GT healing rate group B = 75%). Other authors reported GT healing rates between 66 and 83% in context of RTSA employed for PHFs [13, 21, 37].
Implant design
The implant design did not seem to affect the ability to rotate the affected shoulder externally or internally. Although cadaveric studies and finite element analysis predict a better rotatory capacity and less anterior or posterior impingement, if a RTSA with an increased LO and a smaller IA is employed [19, 22, 23, 26], differences concerning rotatory function may not be evident in clinical studies, because the prediction of deltoid muscle function and the function of other rotatory muscles of the shoulder (M. pectoralis major, M. teres major and M. latissimus dorsi) cannot be simulated adequately. Several authors reported that higher IAs led to increased abduction capacity [19, 36, 45]. We did not assess a different abduction between the groups in our study (group A = 111° and group B = 106°; p = 0.327). This finding is interesting because the potentially increased pretension of the deltoid muscle in implants with a higher IA did neither lead to higher abduction angles nor to an increased abduction force in the two different groups of our study. Other authors reported a wide range of abduction ability after the implantation of RTSA for PHFs between 91° and 139° [11,12,13, 38,39,40,41, 46]. These results show a great variety, which may depend on the surgical technique of tuberosity repair and of course on tuberosity healing. It has been reported that tuberosity healing improves abduction [8, 13, 21]. However, we did not observe a clinical relevance of tuberosity healing in our study. A larger patient number would have been mandatory to allow for a subgroup analysis comparing tuberosity healing for both implant types.
A further notable finding was the rate of SN, which was 47% in patients treated with a standard Grammont style implant with an IA of 155°, while SN rarely occurred in cases with a higher LO and a lower IA.
Scapular notching
Scapular notching is an important issue in RTSA. The rate of SN between following RTSA varies from10% to 96% [47,48,49]. There seems to be a clinical relevance of SN, which may be related to poorer clinical outcomes, higher complication rates and component loosening [48, 50, 51]. By our study, we can confirm the results of other authors who reported that higher IAs of the humeral implant lead to an increased rate of scapular notching [17, 20, 52,53,54].
Gobezie et al. reported results of patients treated with two different inclination angles (155° and 135°) with a standard glenosphere without an increased LO in a randomized controlled trial in context of cuff tear arthropathy and osteoarthritis [18]. These authors observed a higher rate of SN in patients treated with a higher IA of the humeral implant (IA 155° = 58% and IA 135° = 21%). Our results demonstrate that an increased LO in combination with a lower IA does not lead to better active range motion but almost to an elimination of scapular notching. One possible reason for the absence of scapular notching in in patients treated with a lower IA is the additionally increased LO and the different indication for implantation of RTSA.
Problems and complications
The other observed radiological problems like stress shielding, heterotopic ossifications or radiolucency have been described as problems following reverse shoulder arthroplasty rather than true complications [14]. These problems and the observed complications that required surgical revision occurred in both groups and are probably not related to the implant.
Jain et al. reported similar complications in all studies of a literature review dealing with RTSA implanted for PHFs [37].
Limitations
Our study is related to several limitations. The study is retrospective and offers a limited follow-up period and a limited patient number. The follow-up period was relatively short regarding the occurrence of scapular notching. Numerous patients were lost to follow-up. The patient collective was too small to compare the effect of tuberosity healing for the two different implants.
Strengths
Strengths of our study are its single-center and single-surgeon design.
Conclusion
In comparison to a standard reverse total shoulder arthroplasty with a neck-shaft angle of 155° implants with a decreased neck-shaft angle of 135° and an increased lateral offset of 4 mm achieve similar clinical outcomes in context of proximal humerus fractures. An increased lateral offset in combination with a decreased neck-shaft angle of the humeral component eliminates the risk for scapular notching.
References
Murray IR, Amin AK, White TO et al (2011) Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br 93:1–11
Palvanen M, Kannus P, Niemi S et al (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442:87–92
Roux A, Decroocq L, El Batti S et al (2012) Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res 98:715–719
Bahrs C, Stojicevic T, Blumenstock G et al (2014) Trends in epidemiology and patho-anatomical pattern of proximal humeral fractures. Int Orthop 38:1697–1704
Laux CJ, Grubhofer F, Werner CML et al (2017) Current concepts in locking plate fixation of proximal humerus fractures. J Orthop Surg Res 12:137
Sebastia-Forcada E, Cebrian-Gomez R, Lizaur-Utrilla A et al (2014) Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg 23:1419–1426
Cuff DJ, Pupello DR (2013) Comparison of hemiarthroplasty and reverse shoulder arthroplasty for the treatment of proximal humeral fractures in elderly patients. J Bone Joint Surg Am 95:2050–2055
Ohl X, Bonnevialle N, Gallinet D et al (2018) How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg 27:2139–2144
Cazeneuve JF, Cristofari DJ (2011) Long term functional outcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res 97:583–589
Cazeneuve JF, Cristofari DJ (2014) Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5 to 12 years follow-up. Orthop Traumatol Surg Res 100:93–97
Grubhofer F, Wieser K, Meyer DC et al (2016) Reverse total shoulder arthroplasty for acute head-splitting, 3- and 4-part fractures of the proximal humerus in the elderly. J Shoulder Elbow Surg 25:1690–1698
Ross M, Hope B, Stokes A et al (2015) Reverse shoulder arthroplasty for the treatment of three-part and four-part proximal humeral fractures in the elderly. J Shoulder Elbow Surg 24:215–222
Schmalzl J, Jessen M, Sadler N et al (2020) High tuberosity healing rate associated with better functional outcome following primary reverse shoulder arthroplasty for proximal humeral fractures with a 135 degrees prosthesis. BMC Musculoskelet Disord 21:35
Zumstein MA, Pinedo M, Old J et al (2011) Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 20:146–157
Boileau P, Watkinson DJ, Hatzidakis AM et al (2005) Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 14:147S-161S
Ladermann A, Denard PJ, Boileau P et al (2015) Effect of humeral stem design on humeral position and range of motion in reverse shoulder arthroplasty. Int Orthop 39:2205–2213
Ladermann A, Denard PJ, Collin P et al (2020) Effect of humeral stem and glenosphere designs on range of motion and muscle length in reverse shoulder arthroplasty. Int Orthop 44:519–530
Gobezie R, Shishani Y, Lederman E et al (2019) Can a functional difference be detected in reverse arthroplasty with 135 degrees versus 155 degrees prosthesis for the treatment of rotator cuff arthropathy: a prospective randomized study. J Shoulder Elbow Surg 28:813–818
Gutierrez S, CaT C, Luo ZP et al (2008) Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty. Hierarchy of surgical and implant-design-related factors. J Bone Joint Surg Am 90:2606–2615
Werner BS, Chaoui J, Walch G (2017) The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elbow Surg 26:1726–1731
O’sullivan J, Ladermann A, Parsons BO et al (2020) A systematic review of tuberosity healing and outcomes following reverse shoulder arthroplasty for fracture according to humeral inclination of the prosthesis. J Shoulder Elbow Surg 29:1938–1949
Boileau P, Moineau G, Roussanne Y et al (2017) Bony increased offset-reversed shoulder arthroplasty (BIO-RSA). JBJS Essent Surg Tech 7:e37
Werthel JD, Walch G, Vegehan E et al (2019) Lateralization in reverse shoulder arthroplasty: a descriptive analysis of different implants in current practice. Int Orthop 43:2349–2360
Greiner S, Schmidt C, Herrmann S et al (2015) Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg 24:1397–1404
Ferle M, Pastor MF, Hagenah J et al (2019) Effect of the humeral neck-shaft angle and glenosphere lateralization on stability of reverse shoulder arthroplasty: a cadaveric study. J Shoulder Elbow Surg 28:966–973
Kim SJ, Jang SW, Jung KH et al (2019) Analysis of impingement-free range of motion of the glenohumeral joint after reverse total shoulder arthroplasty using three different implant models. J Orthop Sci 24:87–94
Ladermann A, Tay E, Collin P et al (2019) Effect of critical shoulder angle, glenoid lateralization, and humeral inclination on range of movement in reverse shoulder arthroplasty. Bone Joint Res 8:378–386
Fortane T, Beaudouin E, Lateur G et al (2020) Tuberosity healing in reverse shoulder arthroplasty in traumatology: Use of an offset modular system with bone graft. Orthop Traumatol Surg Res 106:1113–1118
Sirveaux F, Roche O, Mole D (2010) Shoulder arthroplasty for acute proximal humerus fracture. Orthop Traumatol Surg Res 96:683–694
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Meinberg EG, Agel J, Roberts CS et al (2018) Fracture and dislocation classification compendium-2018. J Orthop Trauma 32(Suppl 1):S1–S170
Thomas M, Dieball O, Busse M (2003) Normal values of the shoulder strength in dependency on age and gender–comparison with the constant, UCLA, ASES scores and SF36 health survey. Z Orthop Ihre Grenzgeb 141:160–170
Sirveaux F, Favard L, Oudet D et al (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86:388–395
Middernacht B, Van Tongel A, De Wilde L (2016) A critical review on prosthetic features available for reversed total shoulder arthroplasty. Biomed Res Int 2016:3256931
Langohr GD, Giles JW, Athwal GS et al (2015) The effect of glenosphere diameter in reverse shoulder arthroplasty on muscle force, joint load, and range of motion. J Shoulder Elbow Surg 24:972–979
Virani NA, Cabezas A, Gutierrez S et al (2013) Reverse shoulder arthroplasty components and surgical techniques that restore glenohumeral motion. J Shoulder Elbow Surg 22:179–187
Jain NP, Mannan SS, Dharmarajan R et al (2019) Tuberosity healing after reverse shoulder arthroplasty for complex proximal humeral fractures in elderly patients-does it improve outcomes? A systematic review and meta-analysis. J Shoulder Elbow Surg 28:e78–e91
Klein M, Juschka M, Hinkenjann B et al (2008) Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 22:698–704
Reitman RD, Kerzhner E (2011) Reverse shoulder arthoplasty as treatment for comminuted proximal humeral fractures in elderly patients. Am J Orthop (Belle Mead NJ) 40:458–461
Gallinet D, Clappaz P, Garbuio P et al (2009) Three or four parts complex proximal humerus fractures: hemiarthroplasty versus reverse prosthesis: a comparative study of 40 cases. Orthop Traumatol Surg Res 95:48–55
Valenti P, Katz D, Kilinc A et al (2012) Mid-term outcome of reverse shoulder prostheses in complex proximal humeral fractures. Acta Orthop Belg 78:442–449
Simovitch RW, Roche CP, Jones RB et al (2019) Effect of tuberosity healing on clinical outcomes in elderly patients treated with a reverse shoulder arthroplasty for 3- and 4-part proximal humerus fractures. J Orthop Trauma 33:e39–e45
Reuther F, Petermann M, Stangl R (2019) Reverse shoulder arthroplasty in acute fractures of the proximal humerus: does tuberosity healing improve clinical outcomes? J Orthop Trauma 33:e46–e51
Sabesan VJ, Lima DJL, Yang Y et al (2020) The role of greater tuberosity healing in reverse shoulder arthroplasty: a finite element analysis. J Shoulder Elbow Surg 29:347–354
Oh JH, Shin SJ, Mcgarry MH et al (2014) Biomechanical effects of humeral neck-shaft angle and subscapularis integrity in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 23:1091–1098
Lenarz C, Shishani Y, Mccrum C et al (2011) Is reverse shoulder arthroplasty appropriate for the treatment of fractures in the older patient? Early observations. Clin Orthop Relat Res 469:3324–3331
Ball CM (2020) Delta Xtend reverse shoulder arthroplasty - results at a minimum of five years. Shoulder Elbow 12:114–123
Mollon B, Mahure SA, Roche CP et al (2017) Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 476 shoulders. J Shoulder Elbow Surg 26:1253–1261
Nicholson GP, Strauss EJ, Sherman SL (2011) Scapular notching: Recognition and strategies to minimize clinical impact. Clin Orthop Relat Res 469:2521–2530
Friedman RJ, Barcel DA, Eichinger JK (2019) Scapular notching in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 27:200–209
Raiss P, Edwards TB, Deutsch A et al (2014) Radiographic changes around humeral components in shoulder arthroplasty. J Bone Joint Surg Am 96:e54
Ladermann A, Gueorguiev B, Charbonnier C et al (2015) Scapular notching on kinematic simulated range of motion after reverse shoulder arthroplasty is not the result of impingement in adduction. Medicine (Baltimore) 94:e1615
Kramer M, Baunker A, Wellmann M et al (2016) Implant impingement during internal rotation after reverse shoulder arthroplasty. The effect of implant configuration and scapula anatomy: a biomechanical study. Clin Biomech (Bristol, Avon) 33:111–116
De Biase CF, Ziveri G, Delcogliano M et al (2013) The use of an eccentric glenosphere compared with a concentric glenosphere in reverse total shoulder arthroplasty: two-year minimum follow-up results. Int Orthop 37:1949–1955
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
Ethical approval was given from the ethical committee of the medical faculty of the University of Münster, Münster, Germany on January 20th 2018 (study number: 2016–632-f-S).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Holschen, M., Körting, M., Khourdaji, P. et al. Treatment of proximal humerus fractures using reverse shoulder arthroplasty: do the inclination of the humeral component and the lateral offset of the glenosphere influence the clinical outcome and tuberosity healing?. Arch Orthop Trauma Surg 142, 3817–3826 (2022). https://doi.org/10.1007/s00402-021-04281-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04281-5