Abstract
Prevention of birth of thalassemia major children by identification of risk couples and prenatal diagnosis has been recommended as a realistic and cost effective method for control of thalassemia. We present our experience of antenatal thalassemia screening and prenatal diagnosis (PND) in a tertiary care teaching hospital. All antenatal women presenting to the antenatal clinic over 6 years were counseled for beta thalassemia screening. If the lady was detected heterozygous for thalassemia/hemoglobinopathy, partner screening was advised. If the husband was also detected to be heterozygous, the risk couple was offered prenatal diagnosis by chorionic villus tissue DNA analysis. A total of 5392 antenatal women were counseled for beta thalassemia screening, with compliance in 4376 (81.1%) cases. Beta Thalassemia heterozygosity was detected in 147(3.4%) cases, borderline HbA2 in 75(1.7%) and other hemoglobin variants in 91(2.1%). Partner screening was advised in 313 (7.1%) affected antenatal women, with non-compliance in 33.8% cases. Of 27 risk couples identified, prenatal diagnosis was done in 19 couples, detecting 3 affected fetuses. In 8 couples, PND could not be done because of late gestation, financial constraints, lost follow up, failed CVS tissue aspiration and miscarriage prior to CVS tissue biopsy. Late presentation to the antenatal clinic, non-compliance to screening advice and financial constraints could be the factors impeding the thalassemia control program. This emphasizes on the need for community level awareness and inclusion of Thalassemia screening and prenatal diagnosis in the healthcare system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inherited disorders of hemoglobin are the most common monogenic disorders in the world with most of the affected children being born in developing and low-income countries [1, 2]. Approximately 7% of the population worldwide carries the gene for thalassemia or structural hemoglobin variants. Over 3,00,000 severely affected babies are born annually worldwide, of which approximately 56,000 have thalassemia major [3]. In India, the overall prevalence of β-thalassemia carrier state varies from 3–4%, while in some communities it ranges from 5%-15% [4, 5]. About 10,000 to 12,000 thalassemia major births occur each year in India [6, 7]. The north Indian state of Punjab has a high prevalence of β-thalassemia carrier state with a predicted 170 annual thalassemia homozygous births, considering the state population of 27.7 million (https://censusindia.gov.in/census.website/data/data-visualizations/PopulationSearch_PCA_Indicators.) [8]. However, due to the lack of a national registry, the extrapolated figures may underestimate the disease burden.
Thalassemia causes significant morbidity and mortality in sub-optimally managed patients and is also a financial and social burden on the family. It is a drain of precious healthcare resources especially in developing countries. Prevention of birth of thalassemia major babies has been recommended as a realistic and cost effective method for thalassemia control. This can be achieved by thalassemia screening, awareness generation, identification of at risk couples, genetic counseling, and prenatal diagnosis which forms the basis of any community level thalassemia control program [9]. We report our experience of 6 years in screening, diagnosis and prenatal testing of beta thalassemia in antenatal patients reporting to a tertiary care teaching hospital.
Materials and Methods
This study was done in the Thalassemia Molecular Genetics Laboratory, Department of Pathology of a tertiary care teaching hospital in North India. The data was retrospectively collected from the patient medical records and electronic database over a period of 6 years from April 2014 to March 2019 and later from March 2022 to March 2023. The break in study was due to the Covid-19 pandemic restrictions. The laboratory has approval from the local health authority as a certified genetic laboratory to carry out prenatal diagnosis. Necessary consent for prenatal diagnosis procedure was obtained. Under the Institutional antenatal thalassemia control program, all antenatal patients attending the antenatal clinic irrespective of the gestational age were counseled and referred for thalassemia screening. In case the lady was detected to have thalassemia, hemoglobinopathy or a combination of the two, screening for husband was advised. To avoid delay in risk assessment, the couple was telephonically contacted and advised for partner screening. Non complying couples were counseled and encouraged for partner screening on their subsequent visit to the antenatal clinic.
Venous blood was collected in 2 ml K2-EDTA evacuated containers. Complete blood count was done using Beckman Coulter LH750 automated hematology analyzer. Leishman stained peripheral blood smears were evaluated. Thalassemia screening was done by Biorad D10 Hemoglobin testing system (Biorad Laboratories, USA) using the D10 Dual HbA2/F/A1c program. Manufacturer supplied lyophilized bilevel quality control (Lyphochek Hemoglobin A2 Control) were run with each batch. The instrument is based on the principle of cation exchange-High Performance Liquid Chromatography (CE-HPLC).
A diagnosis of beta thalassemia trait was made when HbA2 was between 4 and 9%. Cases with HbA2 in the range of 3.5%-3.9% were reported as borderline HbA2 level. DNA study/beta globin gene sequencing was advised when the partner had borderline HbA2 levels or beta thalassemia trait.
Couples consenting to undergo prenatal diagnosis were registered in compliance with the prevailing local health body prenatal diagnostic testing rules. Screening was done for nine common beta thalassemia mutations: CD8/9(+ G); CD15(G- > A); IVS1-1(G > T); IVS1-5(G > C); CD41/42(-CTTT); CD30(G > C); 619 bp-deletion; Cap Site + 1(A > C) and -88(C > T). Three structural variants [HbE, HbS and HbD] were also screened. Mutation detection was done by Restriction Fragment Length Polymorphism (RFLP)/ Amplified Refractory Mutation System-Polymerase Chain Reaction (ARMS PCR) as per established protocol [10].
Chorionic villus sampling (CVS) was done by trans-vaginal ultrasound guided procedure, wherever indicated, between 11 to 14 weeks of pregnancy. CVS tissue was cleaned under a dissecting microscope to remove the maternal decidua. DNA extraction from the chorionic villi was done by the QiaAmp DNA extraction kit (Qiagen, Hilden, Germany). DNA from parental blood was also extracted. Maternal contamination was excluded by variable number tandem repeat (VNTR) analysis for the polymorphic markers ACTBP2, D1S80 and ApoB using established protocols [11]. DNA from CVS tissue was evaluated for the parental thalassemia mutations. In couples detected with an affected fetus, non-directive counseling was given.
Results
During the study period, 5392 patients were counseled and advised for beta thalassemia screening on their first visit to the antenatal clinic. Of these, 4376 (81.1%) patients complied with thalassemia screening advice. More than half of the antenatal cases presented in the first trimester of pregnancy (Fig. 1).
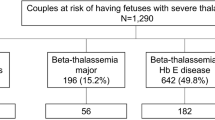
Three hundred thirteen (7.1%) antenatal patients with hemoglobin disorders warranting partner screening were identified. Of these, 147 (3.4%) had beta thalassemia trait, 75 (1.7%) had borderline HbA2 values (3.5–3.9%), while 91(2.1%) had other hemoglobin disorders (Table 1). Red cell indices in borderline HbA2 and beta thalassemia trait cases showed statistical significant difference (Table 2). Partner screening was advised in all these 313 antenatal cases (Fig. 2). Non-compliance to partner screening advice was seen in 106/313 (33.8%) couples. Of the 207 antenatal cases where partner screening was done, the husband was detected to have normal HbA2 levels in 169 (81.6%) cases and the risk of an affected child was excluded. In 38 (18.3%) couples, both husband and wife had a hemoglobin disorder, however only 27 couples had the risk of having a child with clinically severe form of the disease, depending on the mutations carried by the parents (Fig. 2). Of these 27 at risk couples, 10 had a thalassemia major child from earlier pregnancy, while 17 at-risk couples were detected under the screening program. These couples were counseled and offered prenatal diagnosis.
PND procedure was done in 19 at risk couples. The fetus was unaffected in 16 cases while in 3 cases, the fetus was affected. All the three couples bearing the affected fetus opted for termination of pregnancy. In 8 couples, PND could not be done because of late gestation age (3 cases), financial constraints (2 cases), failure to aspirate CVS tissue (1 case), lost to follow up (1 case) and miscarriage prior to CVS tissue biopsy (1 case). The cases presenting in late gestational age were counseled and referred to higher center for PND by amniocentesis.
In two antenatal cases with β-thalassemia trait, partner screening showed borderline HbA2 (3.9% each) levels with normal red cell indices. In both cases, partner thalassemia mutation screening detected the capsite + 1 (A > C) mutation. PND in one of these couples showed an unaffected fetus and the couple continued with the pregnancy. PND testing in the other couple detected an affected fetus, which the couple opted to terminate. In the subsequent pregnancy, this couple again presented for PND. Homozygosity was excluded and the couple continued with the pregnancy. The various thalassemia mutations detected in the ANC couples who presented for PND were IVS 1–5(G > C), IVS 1–1(G > T), Cd 8/9(+ G), 619 bp del, CD 41/42(-CTTT) and capsite + 1(A > C). There was no case of misdiagnosis during prenatal testing.
Discussion
The key findings of our study were late presentation of a considerable number of pregnant women to the antenatal clinic and non-compliance in nearly one thirds of cases for partner screening. Late presentation to the antenatal clinics and non-compliance to thalassemia screening advice has been reported to be a setback in thalassemia control even in populations where medical expertise and thalassemia control technology is available. In our study, late presentation (in 2nd / 3rd trimester) to the antenatal care clinic was seen in 43% of pregnant women. Similar findings were reported by a recent study from north India with 42.7% pregnant women presenting to the health care facility late in the pregnancy [12]. An earlier large scale study from western India done in 61,935 antenatal cases from various public hospitals, had reported late antenatal clinic presentation in 81% cases [13]. An earlier Indian Council of Medical Research (ICMR) sponsored study from our institute had also reported 78.1% antenatal cases presenting late in the 2nd/ 3rd trimester [14].
The overall prevalence of hemoglobin disorders among the ANC cases was 7.1%, which comprised of β thalassemia (3.4%), HbD Punjab (1.1%), borderline HbA2 levels (1.7%) besides other hemoglobin disorders (1.0%). In a study of 7737 antenatal cases in New Delhi, the prevalence of thalassemias/hemoglobinopathy and β-thalassemia trait was reported 6.0% and 5.0% respectively. This could be attributed to Delhi being a cosmopolitan city with an admixture of population. Further, the cases enrolled were also pre-screened for thalassemia by NESTROFT or complete blood count [15]. A study from another city of Punjab had reported a low (4.53%) overall prevalence of hemoglobin disorders [16], while a study from the same city as ours reported a comparable 6.73% overall prevalence [17]. Regional and community differences in hemoglobin disorders have been reported and micromapping of hemoglobinopathies has been emphasised [18].
A 3.96% prevalence of beta thalassemia trait was reported from our center, under a large-scale thalassemia screening in 9991 cases from the general population [8]. Another hospital based study done on 2509 reproductive age group females from the same city had reported beta thalassemia trait prevalence 4.86% [17]. The variation may be attributed to the difference in study sample size.
Although partner screening (in antenatal patients with beta thalassemia / structural variants) was advised by a personal telephonic call, non-compliance for partner screening advice was recorded in 33.8% cases. A previous ICMR funded study from our center had reported non-compliance in 20.6% cases [14]. In another study from North India, 42% non-compliance to screening advice was recorded [12]. A 31% non-compliance to partner screening advice was also reported in a study from Western India [13]. The non-compliant couples potentially remain at-risk of having an affected child in case the unscreened partner is also a carrier. In the current study, though first trimester antenatal clinic presentation among pregnant women has improved (43%) over the years, non-compliance with partner screening advice was still observed in a significant proportion (33.8%) of cases.
In our study, borderline HbA2 levels ranging from 3.5–3.9% was detected in 1.7%of the antenatal cases. In another study from the North of India done in 752 cases, borderline HbA2 levels (3.1–3.9%) were recorded, in 3.1% beta thalassemia carriers who were parents of children with homozygous thalassemia [19]. In two couples from our study, the lady was a beta thalassemia carrier and the husband was detected to have borderline HbA2 level (3.9% each). Molecular diagnosis confirmed capsite + 1 (A > C) mutation in the husband. In India, capsite + 1(A > C) and poly A (T > C) are the common silent mutations presenting with borderline HbA2 levels and near normal/ mildly reduced red cell indices [5, 20]. Borderline HbA2 level in thalassemia heterozygotes has also been related to coexisting delta gene mutations and a spectrum of other mutations [21].
Rangan et al. in a pilot study from North India had demonstrated presence of an underlying beta thalassemia mutation in 32% (8/25) cases with borderline HbA2 levels [20]. Various studies have emphasized that in areas with high prevalence of beta thalassemia carriers, detecting borderline HbA2 levels is not a rare event. It is necessary to investigate these cases at a molecular level, particularly if the partner is a carrier of β-thalassemia [22, 23]. This further emphasizes upon the need to evaluate the beta thalassemia mutation pattern in patients with borderline HbA2 levels, which can contribute significantly to the success of a thalassemia control program.
Prenatal diagnosis has been the widely accepted procedure worldwide to reduce the burden of thalassemia [24]. In our ANC screening program, 27 at-risk couples were alerted and three affected fetus births were prevented. Ten couples who had a β-thalassemia major baby from previous pregnancy presented voluntarily for PND in the subsequent pregnancy. These couples were not screened for β-thalassemia during earlier pregnancy, which reflects the lack of awareness at the population level as well as among healthcare providers. One of the at-risk couple, in the previous pregnancy had declined prenatal diagnosis and delivered a thalassemia major child. In the subsequent pregnancy, the couple voluntarily presented for the PND procedure, which detected an unaffected fetus and the couple continued with the pregnancy.
In 8 at-risk couples, PND could not be done because of late gestation age (3 cases), financial constraints (2 cases), failure to aspirate CVS tissue (1 case), lost to follow up (1 case) or miscarriage prior to CVS tissue biopsy (1 case). An earlier study from Hong Kong had evaluated the causes for birth of thalassemia major children in communities with PND based Thalassemia control program, and found lack of maternal screening, late antenatal visits, lack of paternal screening, and occasional parental refusal as the major setbacks [25]. In our study also lack of awareness in general public and healthcare providers, late presentation to antenatal clinics and financial constraints were found to be the setbacks for optimal thalassemia control.
Conclusion
In absence of a definitive cure, screening and prenatal diagnosis based prevention strategies hold the promise for control of thalassemia. Late presentation to antenatal clinics and non-compliance with screening protocols remain formidable obstacles to the effective implementation of thalassemia control programs. Additionally, the financial constraints associated with both screening and prenatal diagnosis emerge as significant contributing factors to this challenge. The study thus reinforces a multifaceted approach of prioritizing mass awareness, accessibility, and early intervention, integrated with affordability of prenatal testing, which is needed to reduce the burden of Thalassemias and Hemoglobinopathies.
References
Weatherall DJ (2010) The inherited diseases of hemoglobin are an emerging global health burden. Blood 115(22):4331–4336
Modell B, Darlison M (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ [Internet]. [cited 2018 Dec 24];86(6):480–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18568278
Williams TN, Weatherall DJ (2012) World distribution, population genetics, and health burden of the hemoglobinopathies. Cold Spring Harb Perspect Med 2(9):a011692
Madan N, Sharma S, Sood SK, Colah R, Bhatia HM (2010) Frequency of β-thalassemia trait and other hemoglobinopathies in northern and western India. Indian J Hum Genet 16(1):16–25
Colah RB, Gorakshakar A (2014) Control of thalassemia in India. Thal Rep 4:16–19
Verma IC, Saxena R, Kohli S (2011) Past, present & future scenario of thalassaemic care & control in India. Indian J Med Res 134:507–521
Grow K, Vashist M, Abrol P, Sharma S, Yadav R (2014) Beta thalassemia in India: Current status and challenges ahead. Int J Pharm Pharm Sci 6:28–33
Mohanty D, Colah RB, Gorakshakar AC, Patel R, Master D, Mahanta J et al (2013) Prevalence of β -thalassemia and other haemoglobinopathies in six cities in India : a multicentre study. J Community Genet 4:33–42
Management of hemoglobin disorders, Report of Joint WHO-TIF meeting, Nicosia, Cyprus, 16–18 November, 2007. Geneva: WHO; 2008. World Health Organization
Old JM (2003) Screening and genetic diagnosis of haemoglobin disorders. Blood Rev 17(1):43–53
Batanian JR, Ledbetter DH, Fenwick RG (1998) A simple VNTR-PCR method for detecting maternal cell contamination in prenatal diagnosis. Genet Test 2(4):347–350
Mendiratta SL, Bajaj S, Popli S, Singh S (2015) Screening of women in the antenatal period for thalassemia carrier status: comparison of NESTROFT, red cell indices, and HPLC analysis. J Fetal Med 2(1):21–25
Colah R, Surve R, Wadia M, Solanki P, Mayekar P, Thomas M et al (2008) Carrier screening for β-Thalassemia during pregnancy in India: A 7-year evaluation. Genet Test 12(2):181–185
Mohanty D, Colah R, Gorakshakar A (eds) (2008) Jai Vigyan S & T Mission Project on Community Control of Thalassemia Syndromes- Awareness, Screening, Genetic Counseling and Prevention. Director General, Indian Council of Medical Research, New Delhi
Mendiratta SL, Mittal M, Naaz F, Singh S, Anand S (2016) Role of thalassemia screening in prevention and control of thalassemia - a 5 year experience. Int J Reprod Contracept Obstet Gynecol 5(9):3107–11
Sharma A, Uppal N, Kukreja S, Kaur M, Kaur S (2020) Screening of thalassemia in pregnant females visiting tertiary hospital in Amritsar. Int J Clin Biochem Res 7:226–231
Narang V, Jain A, Grover S, Soni A, Narang M, Taneja A (2023) Prevalence and spectrum of haemoglobinopathies in females of reproductive age group- a first tertiary care center experience in Punjab, North India. Indian J Pathol Microbiol 66:564–567
Das R (2012) Micro mapping the frequencies of beta thalassemia and sickle cell anemia in India: a way forward to plan control strategies. Indian J Hum Genet 18(2):148–149
Sharma P, Das R, Trehan A, Bansal D, Chhabra S, Kaur J et al (2015) Impact of iron deficiency on hemoglobin A2% in obligate β-thalassemia heterozygotes. Int J Lab Hematol 37(1):105–111
Rangan A, Sharma P, Dadu T, Saxena R, Verma IC, Bhargava M (2011) β-Thalassemia mutations in subjects with borderline HbA2 values: a pilot study in North India. Clin Chem Lab Med 49(12):2069–2072
Hariharan P, Colaco S, Colah R, Ghosh K, Nadkarni A (2016) Delta globin gene variations leading to reduction in HbA 2 levels. Int J Lab Hematol [Internet]. [cited 2018 Mar 7];38(6):610–5
Giambona A, Passarello C, Renda D, Maggio A (2009) The significance of the hemoglobin A2 value in screening for hemoglobinopathies. Clin Biochem [Internet]. [cited 2018 Mar 7];42(18):1786–96
Mosca A, Paleari R, Galanello R, Sollaino C, Perseu L, Demartis FR et al (2008) New analytical tools and epidemiological data for the identification of HbA2 borderline subjects in the screening for beta-thalassemia. Bioelectrochemistry 73(2):137–140
Munkongdee T, Tanakulmas J, Butthep P, Winichagoon P, Main B, Yiannakis M et al (2016) Molecular Epidemiology of Hemoglobinopathies in Cambodia. Hemoglobin [Internet]. [cited 2018 Dec 22];40(3):163–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27117566
Lee A, Wong K, So K, Cheng M (1998) Why are thalassemia patients born when prenatal screening is available? Hong Kong Med J 4:121–124
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Authors have no financial or non financial interests related to the work submitted in the manuscript.
Disclosures
Dr. Naveen Kakkar is associated with the journal as Associate Editor.
Dr. Ranjeet Singh Mashon has been contributing as Reviewer for the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mashon, R.S., Mandrelle, K. & Kakkar, N. Experience of Antenatal Thalassemia Screening and Prenatal Diagnosis from a Tertiary Care Teaching Hospital in Punjab. Indian J Hematol Blood Transfus (2024). https://doi.org/10.1007/s12288-024-01785-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12288-024-01785-z