Abstract
Because of chronic anemia, hypogonadotropic hypogonadism, and iron chelation, pregnancy in homozygous and heterozygous compound beta-thalassemia patients stays a challenge. Pregnancies of transfused beta-thalassemia women registered in the French National Registry, conducted between 1995 and 2015, are described. These pregnancies were compared with pregnancies in healthy women and to data previously published in the literature. Fifty-six pregnancies of 37 women were studied. There were 5 twin pregnancies. Assisted reproductive technologies (ART) were used in 9 pregnancies. Median term at delivery was 39 amenorrhea weeks, and median weight at birth was 2780 g. Cesarean section was performed in 53.6% of the pregnancies. There were 6 thromboembolic events, 6 serious infections, 6 pregnancy-induced hypertensions (PIH), 6 intrauterine growth retardations (IUGR), 5 severe hemorrhages, 4 gestational diabetes, 3 alloimmunizations, 2 heart diseases, and 1 pre-eclampsia. There were 5 infections and 4 osteoporosis in the first year of post-partum. ART and cesarean sections were more often used in the beta-thalassemia group, compared to control subjects. Thromboembolic events, PIH, hemorrhage at delivery, and IUGR were more frequent in the beta-thalassemia group. Time to delivery was not different, but infant weight at birth was significantly smaller in the beta-thalassemia group. In the post-partum period, global maternal complications were more frequent in the beta-thalassemia group. Pregnancy in transfused beta-thalassemia women is safe with rare obstetrical and fetal complications. Cesarean section remains often chosen, and infant weight at birth remains smaller than that in the general population, despite delivery at full term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beta-thalassemia is one of the most common autosomal recessive disorders worldwide. A higher prevalence involves Mediterranean countries (mainly Italy, Greece, Cyprus, and countries of the north coast of Africa) and South-East Asia [1,2,3]. Beta-thalassemia results from the reduction or absence of beta globin chain synthesis of the hemoglobin (Hb) tetramer [1]. Unassembled alpha chains precipitate, leading to oxidative damage of the erythrocyte membrane and to apoptosis (ineffective erythropoiesis) [1, 2, 4].
Only homozygous or heterozygous compound beta-thalassemia patients are clinically symptomatic. Thalassemia major (TM) represents the most severe phenotype. Symptoms occur during the first 2 years of life, leading to transfusion dependency and iron overload which is potentially responsible for endocrinal deficiencies (especially hypogonadotropic hypogonadism), hepatic fibrosis, and progressive heart failure [1], leading to deaths in 71% of cases [5]. With better transfusion management and early iron chelation, survival and quality of life improved these last 10 years for these patients.
Patients with thalassemia intermedia (TI) develop symptoms later in their lifetime and require little or no transfusion needs. However, they also often present iron overload, due to iron hyperabsorption by inhibition of hepcidin expression (1, 6, 7). Severity of symptoms mainly depends on residual beta-globin chain synthesis.
Because of chronic anemia, hypogonadotropic hypogonadism, and iron overload, pregnancy in TM and TI women is challenging and requires a multidisciplinary decision-making [8]. Since the first published case in 1969 of a successful pregnancy in a woman with TM [9], numerous descriptive series have been reported [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
The aim of the present study was first to describe pregnancy management in transfused women with homozygous or heterozygous compound beta-thalassemia registered in the French National Registry, secondly to compare pregnancy outcomes with those in healthy women, and finally to compare our results to data previously published in the literature.
Materials and methods
This is a retrospective, multicenter, descriptive, and cross-sectional study, conducted between 1995 and 2015 in France. All women were reported for having TM or TI, requiring at least one red blood cell (RBC) transfusion during pregnancy.
Patient data
Data were retrospectively collected from clinical charts. The study was performed in accordance with guidelines of the National Ethics Committee, and each patient signed a written informed consent or gave her oral consent before inclusion in the French National Registry.
Demographic information and women clinical and biological characteristics (thalassemia complications, co-infections, transfusions, iron chelation), were collected at the time of registration. Pregnancy characteristics and outcomes and data regarding management of the disease during pregnancy were also collected. Maternal and neonatal complications and thalassemia management were also reviewed after 1-year follow-up post-delivery.
Control subjects
Pregnancies in healthy women were used as controls. Beta-thalassemia women and healthy women were only compared for their first pregnancy. One TM or TI case was paired with two control cases. Healthy women and beta-thalassemia women were matched on age at first pregnancy and on parity. Healthy women were selected from data bases of a unique tertiary hospital maternity.
Review from the literature
Regarding the review of prior published series, the Medline database (National Library of Medicine, Bethesda, MD) was searched from August 1995 to June 2017, using the following words: “beta-thalassemia,” “beta-thalassemia major,” “thalassemia,” “homozygous beta thalassemia,” “beta-thalassemia intermedia,” and “pregnancy.” References of included papers were further screened to identify reports that could have been missed by the initial search. Only articles in English were selected. We excluded articles about minor beta-thalassemia, cases of other types of thalassemia, and series with less than five cases. Eighteen reports were then identified leading to 941 reported cases.
Statistical analysis
Descriptive data were reported as means or medians with interquartile range (IQR). Fisher test was used for the comparison with the control cohort. In all analyses, p values less than 0.05 were considered statistically significant. All analyses were performed using R v3.0.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics
Sixty-eight women with TM or TI included into the French National Registry had at least one pregnancy between 1995 and 2015. Among them, 31 women were excluded from our study: 2 women with TM who underwent hematopoietic stem cell transplantation; 7 women with TI who did not require chronic red blood cell transfusions regimen; 16 women whose first pregnancy was before 1995; 4 women who were lost of follow-up; and 2 women with incomplete medical record. Overall, 37 women were included in the study: 16 with TM and 21 with TI. Women characteristics before pregnancy are summarized in Table 1. Seven women had a positive hepatitis C virus (HCV) serology, of which 2 TI patients with an active form who required Interferon and Ribavirin therapy before pregnancy. None had a human immunodeficiency virus (HIV) or hepatitis B virus (HBV) positive serology. Seven women had primary amenorrhea and received a hormonal substitutive treatment. Five women presented secondary amenorrhea. One of them received a hormonal supplementation. All TM women and 3 TI women regularly required red blood cells (RBC) transfusions before pregnancy. Median hepatic iron concentration before pregnancy was 280 µmol/g (300 for TM and 240 for TI, IQR: 200–350). Two TM patients had cardiac iron deposition before pregnancy (MRI T2* 10 and 16 ms), but one of women had diabetes mellitus or cardiac function deterioration. Iron chelation was performed in 87.5% of TM cases and in 48% of TI cases. Two TM women were not in chelation treatment, due to lack of observance or lack of specialized follow-up. Two TI women who had phlebotomies were treated by erythropoietin. One TM patent was treated by erythropoietin despite transfusions. These 3 women were followed in the same hospital.
Thalassemia management during pregnancy
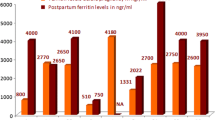
Iron chelation was stopped during pregnancy, except in one case which kept going with deferoxamine. In TM women, the median RBC transfusion interval was 21 days (IQR: 14–28) during pregnancy. In TI women, transfusion need was marginal (≤ 3 times) for 11 pregnancies and at regular intervals for 19 pregnancies with a median RBC transfusion interval of 28 days (IQR: 21–70). Transfusions were required after a median of 22 weeks of amenorrhea (IQR: 0–41) for TI women. Platelet antiaggregant therapy was introduced for 8 pregnancies (2 TM and 6 TI) and anticoagulant prophylaxis for 4 pregnancies (2 TM and 2 TI). Hb and ferritin levels during pregnancy and after delivery are shown in Fig. 1.
Pregnancy outcome
During the time of study, the 37 included patients had 79 pregnancies. Fifty-six pregnancies were analyzed of which 5 twin pregnancies. Twenty-three pregnancies were excluded from the analyses because of early miscarriage (16 pregnancies), missing data (4 pregnancies), and absence of RBC transfusion need (3 pregnancies). Most pregnancies (84%) were conceived without assisted reproductive technologies (ART). ART was used in 9 pregnancies: ovarian stimulation (3 pregnancies), artificial insemination (2 pregnancies), in vitro fertilization (2 pregnancies), intra-cytoplasmic sperm injection (1 pregnancy), and oocyte donation (1 pregnancy). Characteristics and outcomes of pregnancies are summarized in Table 2. Mean age at the time of first pregnancy was 29 years (IQR 17–38). Mean number of pregnancies per woman giving birth to a living baby was 1.7 (IQR 1–4). The median time to delivery was 39 weeks of amenorrhea. Twelve newborns were premature (born before 37 weeks of amenorrhea). Median weight at birth was 2.78 kg. Median 5-min Apgar score was 10. Cesarean section was performed in 53.6% of the pregnancies, because of prior uterine scar (8 cases), prolonged labor (6 cases), abnormal fetal heart rate (3 cases), pathologic pelvis (3 cases), premature rupture of the membranes (2 cases), breech birth (1 case), pre-eclampsia (1 case), retroplacental hematoma (1 case), curative anticoagulant treatment (1 case), maternal heart failure (1 case), or for unidentified reasons (3 cases).
Six venous thromboembolic events in 4 women (1 TM and 3 TI) were reported during pregnancy: One TI woman with S protein deficit presented pulmonary embolism, while the 3 others women presented deep vein thrombosis. Two women were reported with heart disease not related to iron overload (one pericarditis and one cardiac failure secondary to infectious endocarditis). Severe infections were observed in 6 cases, including 2 pneumonias and 2 Staphylococcus aureus bacteremia favored by infected vascular devices and prior splenectomy. Six women developed pregnancy-induced high blood pressure (PIH) and one presented pre-eclampsia. Three cases of alloimmunization were observed during pregnancy (2 TM and 1 TI women). It was the first pregnancy for each woman. Four women developed gestational diabetes. Five women had severe hemorrhage at delivery. There was one intrauterine fetal death due to a retroplacental hematoma.
One-year post-partum outcome
There was no neonatal or maternal death in the first year of post-partum. Mothers decided to breastfeed in 66% of cases. Five women developed an infection (2 endometritis, 2 breast infections, one fever of unknown origin) during post-partum period. No woman had antibiotic prophylaxis after delivery to avoid these infections. Four women developed osteoporosis. One woman had hearing loss, secondary to deferoxamine. There were no thromboembolic events, no pulmonary hypertension, and no cardiac or hepatic events. RBC transfusions during the post-partum period were performed every 28 days in TM women (IQR 21–42) and were only continued in 3 TI women (median interval of 60 days; IQR: 56–90). Iron chelation was re-introduced after a median of 12 weeks (IQR: 3–40) following delivery (always after breastfeeding) in TM women and 14 weeks (IQR: 8–54) in TI women. There was no evaluation of hepatic and cardiac iron charge during the first post-partum year except for one TM patient who had cardiac iron charge before pregnancy. The MRI T2* improved after pregnancy (from 10 to 15 ms). Ten newborns developed jaundice, and among them 3 had anemia.
Comparison with the control cohort
Results regarding first pregnancies were compared with those observed in healthy women (Table 3). In the beta-thalassemia group, HCV infection was significantly more frequent (p = 0.003), ART use was more frequent (p = 0.006), and cesarean section was more often performed (p = 0.002). Thromboembolic events (p = 0.01), PIH (p = 0.003), hemorrhage at delivery (p = 0.012), and intrauterine growth retardation (IUGR) (p = 0.01) were also more frequent in the beta-thalassemia group. Reversely, no differences were observed in terms of twin pregnancies. The time to delivery and the Apgar score were not significantly different among the two groups, but infant weight at birth was significantly smaller in the beta-thalassemia group (p = 0.004). Post-partum maternal complications were more frequent in the beta-thalassemia group (p < 0.001), especially regarding infections (p = 0.03).
Discussion
Despite some study limitations, such as its retrospective design and its length over many years, leading to some missing data and patients lost of follow-up, we confirmed that the number of transfused women with beta-thalassemia having a safe and successful pregnancy is currently increasing [12,13,14, 19, 26,27,28,29]. This can be explained by the improvement in ART and iron chelation, and in RBC transfusion management. However, pregnancy in transfused patients with beta-thalassemia remains uncommon. This explains the small number of pregnancies found in our National Registry over the last two decades. Moreover, while bone marrow transplantation has led to a greater improvement of the disease, little data is currently available regarding the pregnancy outcome in transfused patients with beta-thalassemia.
Our study confirms prior published reports (Table 4) [10,11,12,13,14,15, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. However, among initial symptomatology, hypogonadotropic hypogonadism was less frequent in our study: 19% of primary amenorrhea and 13.5% of secondary amenorrhea versus 21.5% of primary amenorrhea and 26.1% of secondary amenorrhea in a previous study from Italy [10] and even 60% of secondary amenorrhea in another study [19]. Similarly, osteoporosis (21.6%) was less frequently observed in our series than in prior reports (33–41%) [13, 18, 19, 28]. Consequences of iron overload, such as hypothyroidism, hypoparathyroidism, or hepatic fibrosis, were observed, but there were no diabetes mellitus and no cardiac failures in our cases. This could be explained by the French guidelines which recommend pregnancy only after optimal control of cardiac and metabolic complications [32]. Three women presented thromboembolic events before pregnancy, a well-known complication in patients with homozygous beta-thalassemia favored by a prior splenectomy [1, 2, 33]. HCV serology was positive in 18.9% of the patients, which was less than the reported incidence in previous reports (20–100%) [10, 11, 13, 18, 29]. One explanation is the better screening of blood donors to exclude HCV blood form transfusion and a better knowledge of this disease compared to older studies.
Mean age at first pregnancy was in agreement with data from the literature [11, 13, 14, 29]. ART was necessary for 9 pregnancies (16%), especially for women with TM [7]. Ovarian stimulation is the first line therapy in these TM women suffering from hypogonadotropic hypogonadism [34] and was successful in 3 patients from our study. Assisted reproduction was necessary for 2 women with TI: one oocyte donation, after ovarian stimulation failure, in one woman with severe ovarian deficiency, and one intra-cytoplasmic sperm injection for oligoasthenoteratozoospermia. ART use in patients with beta-thalassemia appeared heterogeneous in the literature but seemed more frequent in women with TM (10–63%) [10, 18,19,20, 22, 24, 25, 27, 29] than in those with TI (0–10.2%) [14, 16, 26]. This is consistent with iron overload, which is more frequent, more severe, and occurs earlier in TM patients [1, 34]. Iron infiltration of the anterior pituitary gland has also been described as one of the main causes of hypogonadotropic hypogonadism in patients with beta-thalassemia [34]. Furthermore, assisted reproduction can induce a high rate of multiple pregnancies [21, 33] and was found in 4 of the 5 twin pregnancies in our study.
Pre-term deliveries were observed in 21.4% of cases, which is in agreement with other studies (0–35.2%) [2, 10, 11, 13, 14, 17,18,19,20, 22]. These cases could be explained by multiple pregnancies and obstetrical complications [8]. Infant weight at birth was also consistent with data from the literature [12, 14, 17, 19,20,21,22,23, 25, 26, 29, 30]. However, the rate of cesarean sections was especially high in our study (53.6%). Actually, this practice was very heterogeneous in the previous reports ranging from 24 to 100% [10, 15, 17, 27,28,29]. In the beta-thalassemia setting, planning cesarean section seemed easier, in order to avoid maternal and fetal complications [8, 13, 19, 20]. Indeed, obstetrical complications are more frequently observed than in the general population [8]. PIH and pre-eclampsia [13, 19, 21, 23, 28, 29], gestational diabetes [11,12,13, 27], and hemorrhages at delivery [31] were frequently reported in previous publications. IUGR has been described with a higher prevalence in women with beta-thalassemia and seems related to maternal anemia, which reduces oxygen supply to the fetus [13, 16, 19, 26,27,28, 30].
Thromboembolic events are also well known complications in women with beta-thalassemia, especially with TI. They are related to the presence of defective innate red blood cells with disrupted membranes circulating in the bloodstream that expose thrombogenic negatively charged lipids on the external cell surface [8, 33]. Splenectomy increases the incidence [1, 8, 33] that could also be majored during pregnancy, despite prophylaxis using low-dose aspirin or preventive anticoagulants [33, 35]. In our cohort, all the patients who developed thromboembolic events during pregnancy were splenectomized. Two of them had anterior thromboembolic events and had S protein deficiency. The thrombosis appeared despite anticoagulant prophylaxis for these two women. None was treated by erythropoietin before pregnancy. Alloimmunization was observed in 3 women who were occasionally transfused before pregnancy. This seemed also favored by a prior splenectomy [8, 13, 14, 33].
Regarding fetal complications, abnormal fetal heart rates could be explained by the presence of non-transferrin-bound iron in the serum of transfusion-dependent women, which can cause cardiac dysrhythmias [35].
Two types of infections could be observed during pregnancy: first chronic infections, such as HIV and hepatitis, transmitted by the mother to the fetus, which were not observed in our study, but could be more common in developing countries [8, 20], and also bacterial infections, potentially favored by gestational estrogen and iron overload that disturb the immune balance [35], by the frequent prior history of splenectomy, and by the presence of implanted central venous access, relatively common in case of transfusion dependency.
Cardiac issues were not observed in our study, as in other recent studies [12,13,14], while severe adverse events have previously been reported [8, 11, 17, 18, 23, 33, 35]. These lethal complications became uncommon with the development of effective iron chelation and cardiac screening before pregnancy. Iron chelation should, however, be avoid during the first trimester of pregnancy according to expert recommendations but can be re-introduced during the second and third trimesters in patients with a strong treatment requirement [35,36,37].
Women with TM generally increase their RBC transfusion needs during pregnancy [13]. This can be explained by hemodilution and a Hb level cut-off at 10 g/dL in this setting for transfusion [10, 13].
Post-partum evolution was relatively safe in our study. The lack of severe maternal complications in the post-partum period can be explained by a good management of iron overload and chelation re-introduction rapidly after delivery (median: 12 weeks).
To our knowledge, our study is the second one comparing pregnancy outcome of patients with thalassemia with a control group. Luewan et al. compared in Thailand women with compound beta-thalassemia/HbE with a control group and found more IUGR, pre-term delivery, and lower infant weight at birth in the studied group [31]. Our study confirmed a higher incidence of IUGR and a lower infant weight at birth in the beta-thalassemia group. It also showed more HCV positive serology (which can be explained by transfusion-dependency in TM women) and more ART-induced pregnancies in the thalassemia group than in the healthy group. Cesarean section was also more frequently used, for reasons described above. Women with beta-thalassemia were more preventively treated by anticoagulants or low-dose aspirin, because of the thrombosis risk in this population. However, thromboembolic events remained more frequent for women with beta-thalassemia than in the control group. More post-partum complications were observed in thalassemia women.
Overall, an increasing number of women with beta-thalassemia can have children, despite frequent hypogonadotropic hypogonadism. Effective iron chelation and advances in ART are major parts of this improvement. Pregnancies in this population are relatively safe, with few obstetrical and fetal complications. However, cesarean section remains often chosen in beta-thalassemia women, considering this situation at risk, and infant weight at birth remains lower than that in the general population, despite delivery at full term.
References
Cao A, Galanello R (2010) Beta-thalassemia. Genet Med Off J Am Coll Med Genet 12(2):61–76
Galanello R, Origa R (2010) Beta-thalassemia. Orphanet J Rare Dis 5:11
Flint J, Harding RM, Boyce AJ, Clegg JB (1998) The population genetics of the haemoglobinopathies. Baillieres Clin Haematol 11(1):1–51
Rund D, Rachmilewitz E (2005) Beta-thalassemia. N Engl J Med 353(11):1135–1146
Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC et al (2004) Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica 89(10):1187–1193
Tanno T, Bhanu NV, Oneal PA, Goh S-H, Staker P, Lee YT et al (2007) High levels of GDF15 in thalassemia suppress expression of the iron regulatory protein hepcidin. Nat Med 13(9):1096–1101
Wang R-H, Li C, Xu X, Zheng Y, Xiao C, Zerfas P et al (2005) A role of SMAD4 in iron metabolism through the positive regulation of hepcidin expression. Cell Metab 2(6):399–409
Leung TY, Lao TT (2012) Thalassaemia in pregnancy. Best Pract Res Clin Obstet Gynaecol 26(1):37–51
Walker EH, Whelton MJ, Beaven GH (1969) Successful pregnancy in a patient with thalassaemia major. J Obstet Gynaecol Br Commonw 76(6):549–553
Gulino FA, Vitale SG, Fauzia M, Cianci S, Pafumi C, Palumbo MA (2013) Beta-Thalassemia major and pregnancy. Bratisl Lek Listy 114(9):523–525
Thompson AA, Kim H-Y, Singer ST, Vichinsky E, Eile J, Yamashita R et al (2013) Pregnancy outcomes in women with thalassemia in North America and the United Kingdom. Am J Hematol 88(9):771–773
Al-Riyami N, Al-Khaduri M, Daar S (2014) Pregnancy Outcomes in Women with Homozygous Beta Thalassaemia: A single-centre experience from Oman. Sultan Qaboos Univ Med J 14(3):e337-341
Origa R, Piga A, Quarta G, Forni GL, Longo F, Melpignano A et al (2010) Pregnancy and beta-thalassemia: an Italian multicenter experience. Haematologica 95(3):376–381
Voskaridou E, Balassopoulou A, Boutou E, Komninaka V, Christoulas D, Dimopoulou M et al (2014) Pregnancy in beta-thalassemia intermedia: 20-year experience of a Greek thalassemia center. Eur J Haematol 93(6):492–499
Aessopos A, Karabatsos F, Farmakis D, Katsantoni A, Hatziliami A, Youssef J et al (1999) Pregnancy in patients with well-treated beta-thalassemia: outcome for mothers and newborn infants. Am J Obstet Gynecol 180(2 Pt 1):360–365
Nassar AH, Usta IM, Rechdan JB, Koussa S, Inati A, Taher AT (2006) Pregnancy in patients with beta-thalassemia intermedia: outcome of mothers and newborns. Am J Hematol 81(7):499–502
Ansari S, Azarkeivan A, Kivan AA, Tabaroki A (2006) Pregnancy in patients treated for beta thalassemia major in two centers (Ali Asghar Children’s Hospital and Thalassemia Clinic): outcome for mothers and newborn infants. Pediatr Hematol Oncol 23(1):33–37
Tuck SM (2005) Fertility and pregnancy in thalassemia major. Ann N Y Acad Sci 1054:300–307
Mancuso A, Giacobbe A, De Vivo A, Ardita FV, Meo A (2008) Pregnancy in patients with beta-thalassaemia major: maternal and foetal outcome. Acta Haematol 119(1):15–17
Kumar RM, Khuranna A (1998) Pregnancy outcome in women with beta-thalassemia major and HIV infection. Eur J Obstet Gynecol Reprod Biol 77(2):163–169
Bajoria R, Chatterjee R (2009) Current perspectives of fertility and pregnancy in thalassemia. Hemoglobin 33(Suppl 1):S131-135
Tampakoudis P, Tsatalas C, Mamopoulos M, Tantanassis T, Christakis JI, Sinakos Z et al (1997) Transfusion-dependent homozygous beta-thalassaemia major: successful pregnancy in five cases. Eur J Obstet Gynecol Reprod Biol 74(2):127–131
Toumba M, Kanaris C, Simamonian K, Skordis N (2008) Outcome and management of pregnancy in women with thalassaemia in Cyprus. East Mediterr Health J Rev Sante Mediterr Orient Al-Majallah Al-Sihhiyah Li-Sharq Al-Mutawassit 14(3):628–635
Jensen CE, Tuck SM, Wonke B (1995) Fertility in beta thalassaemia major: a report of 16 pregnancies, preconceptual evaluation and a review of the literature. Br J Obstet Gynaecol 102(8):625–629
Daskalakis GJ, Papageorgiou IS, Antsaklis AJ, Michalas SK (1998) Pregnancy and homozygous beta thalassaemia major. Br J Obstet Gynaecol 105(9):1028–1032
Roumi JE, Moukhadder HM, Graziadei G, Pennisi M, Cappellini MD, Taher AT (2017) Pregnancy in β-thalassemia intermedia at two tertiary care centers in Lebanon and Italy: a follow-up report on fetal and maternal outcomes. Am J Hematol 92(6):E96–E99
Fozza C, Asara MA, Vacca N, Caggiari S, Monti A, Zaccheddu F et al (2017) Pregnancy outcome among women with beta-thalassemia major in North Sardinia. Acta Haematol 138(3):166–167
Vlachodimitropoulou E, Thomas A, Shah F, Kyei-Mensah A (2018) Pregnancy and iron status in β-thalassaemia major and intermedia: six years’ experience in a North London Hospital. J Obstet Gynaecol 38(4):567–570
Cassinerio E, Baldini IM, Alameddine RS, Marcon A, Borroni R, Ossola W et al (2017) Pregnancy in patients with thalassemia major: a cohort study and conclusions for an adequate care management approach. Ann Hematol 96(6):1015–1021
Nassar AH, Naja M, Cesaretti C, Eprassi B, Cappellini MD, Taher A (2008) Pregnancy outcome in patients with beta-thalassemia intermedia at two tertiary care centers Beirut and Milan. Haematologica 93(10):1586–1587
Luewan S, Srisupundit K, Tongsong T (2009) Outcomes of pregnancies complicated by beta-thalassemia/hemoglobin E disease. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet 104(3):203–205
Haute Autorité de Santé (2008) Syndromes thalassémiques majeurs et intermédiaires. Protocole National de Diagnostic de Soins pour une maladie rare
Lao TT (2017) Obstetric care for women with thalassemia. Best Pract Res Clin Obstet Gynaecol 39:89–100
Castaldi MA, Cobellis L (2016) Thalassemia and infertility. Hum Fertil Camb Engl 19(2):90–96
Petrakos G, Andriopoulos P, Tsironi M (2016) Pregnancy in women with thalassemia: challenges and solutions. Int J Womens Health 8:441–451
Diamantidis MD, Neokleous N, Agapidou A, Vetsiou E, Manafas A, Fotiou P et al (2016) Iron chelation therapy of transfusion-dependent β-thalassemia during pregnancy in the era of novel drugs: is deferasirox toxic? Int J Hematol 103(5):537–544
Rachmilewitz EA, Giardina PJ (2011) How I treat thalassemia. Blood 118(13):3479–3488
Author information
Authors and Affiliations
Contributions
EV collected and interpreted the data, conducted the statistical analysis, wrote the manuscript, and gave final approval. SJ conducted the statistical analysis; IT, RH, FLa, FLi, MJL, JM, SN, BP, JAR, DS, CR, and FG included patients. GC included patients and reviewed the manuscript. AH included patients, interpreted the data, reviewed the manuscript, and gave final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Virot, E., Thuret, I., Jardel, S. et al. Pregnancy outcome in women with transfused beta-thalassemia in France. Ann Hematol 101, 289–296 (2022). https://doi.org/10.1007/s00277-021-04697-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04697-4