Abstract
There has been a surge in haploidentical hematopoietic stem cell transplantation (HSCT) in India recently. However, there is a paucity of data on haploidentical HSCT from India. The report is an analysis of data of haploidentical HSCT performed at our center. Analysis of patients with acute leukemia or chronic myeloid leukemia who underwent haploidentical HSCT during 2014–2019 was performed. The graft versus host disease (GVHD) prophylaxis was post-transplant Cyclophosphamide with Mycophenolate-mofetil and Cyclosporine. All patients were transfused peripheral blood stem cells from donors. Overall survival (OS) was calculated using the Kaplan–Meier method. Twenty-one patients underwent haploidentical HSCT. Fourteen-patients were males. The median age of patients was 15 years. Fludarabine with total body irradiation was the most common conditioning regimen (n = 15, 71.4%). The median duration for neutrophil and platelet engraftment was 14 days. Cumulative incidence of acute and chronic GVHD was 19%, and 38% respectively. The median follow-up was 26 months and the two-year OS was 38%. Twelve (57%) patients died during the study period, 8 patients (38%) died from transplant-related mortality (TRM), and 4 from disease relapse. Sepsis was the cause of death in six of the eight TRM. Nine out of 21 patients (42.8%) are leukemia-free on follow-up. Haploidentical HSCT is a promising modality of treatment in patients who have no suitable matched donors. Though the TRM remains high, good disease control was achieved in 42.8% of patients. Multi-drug resistant bacterial infection remains a challenge in performing haploidentical HSCT in developing countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lack of availability of matched sibling donor (MSD) or matched unrelated donor (MUD) has been the biggest hindrance in the past to offer potentially curative allogeneic hematopoietic stem cell transplantation (HSCT) for patients with relapsed/refractory or high-risk acute leukemia’s [1, 2]. The rapid progress in haploidentical donor HSCT and the use of post-transplant cyclophosphamide (PTCY) to prevent GVHD has enabled HSCT accessible to a wider pool of patients [3, 4].
India has a genetically heterogeneous population due to ethnic diversity and therefore there is a high degree of polymorphism in the human leukocyte antigen (HLA) gene complex [5]. This polymorphism reduces the probability of finding a MUD donor in registries to less than 10% compared to 80% observed with a homogenous population in many countries [5]. This limits the potential use of MUD HSCT in patients without an MSD.
The cost of procuring and processing stem cells from haploidentical donors are considerably lesser than that for MUD transplants [6, 7]. The reduced probability of getting a MUD, easy availability of a haploidentical donor, and less cost makes haploidentical HSCT a more viable option in resource-challenged countries [6].
It would be helpful if centers in India shared their data on haploidentical HSCT for understanding and improving outcomes. We, therefore, performed a retrospective analysis to look at the clinical profile and outcomes of haploidentical HSCT performed at our center.
Patients and Methods
Patients
Clinical outcome and treatment details were collected from the case records of patients with acute leukemia from the tumor registry who underwent haploidentical HSCT at our center from 2013 to 2019. Institute ethics committee approval was obtained to conduct the study. All patients with acute leukemia either in the first remission or with recurrence who required HSCT and did not have any MSD or MUD donor were considered for haploidentical HSCT. Patients whose disease was in remission underwent a detailed pre-haploidentical transplant workup to assess major organ function and to rule out any current ongoing infective pathology along with dental inspection and counseling.
Donor Selection
The donor selection was individualized and was based on donor age, sex, presence of antibodies against donor-specific HLA antigens (DSA) in the recipient, and comorbidities. Donors who were young, male, DSA negative and had no comorbidities were preferred to reduce the incidence of graft failure and GVHD. Anti-A and Anti B-titres were performed in recipients who had a blood group mismatch with the donor.
Stem Cell Source and Harvest
All donors were treated with Filgrastim (GCSF) 10 ug/kg/day in two divided doses for 5 days before initiation of harvest on the 5th day. Preharvest (on 4th day of filgrastim) and mid-harvest CD34 + cell count was assessed and accordingly, an adequate volume was harvested. Peripheral blood stem cells were collected using apheresis machine through peripheral venous access. A target CD34 + cell dose of 5 × 106/kg recipient body weight was planned, with a minimum required CD 34 + cell dose of 3 × 106/kg recipient body weight. CD3 cell count in the graft was not performed as we did not perform ex-vivo graft manipulation.
Conditioning Regimen and GVHD Prophylaxis
Patients received a fludarabine (FLU) based conditioning regimen. The choice of the conditioning regimen was dictated by multiple factors including physician preference, indication for transplant, age, and presence of co-morbidities. The dose and schedule of the conditioning regimes have been provided in Table 1. The GVHD prophylaxis consisted of PTCY, cyclosporine (CSA), and mycophenolate mofetil (MMF). PTCY was administered in two doses on Day + 3 and Day + 4 after graft infusion at 50 mg/kg/day, along with mesna. CSA was administered intravenously at a dose of 3 mg/kg/day in 2 divided doses starting from day + 5 and the patients were switched to the oral formulation when appropriate. Serum CSA levels were checked biweekly and doses were adjusted to maintain a trough level of 200–300 ng/µL. MMF 15 mg/kg 3 times daily was started along with CSA and continued till Day + 35 post-transplantation in the absence of GVHD. CSA was tapered from day + 90 over 2–4 weeks if there was no GVHD. Filgrastim (GCSF) was started on Day + 5 at a dose of 5 µgm/kg/day and was continued till engraftment.
Supportive Care
All patients were treated in the designated hematopoietic stem cell transplant unit provided with high-efficiency particle air filters. Patients received antimicrobial prophylaxis with fluconazole, acyclovir, and levofloxacin. Pre-emptive cytomegalovirus (CMV) treatment was guided by close monitoring of viral CMV load by quantitative PCR twice weekly until day + 100 or till immunosuppressive agents were tapered. The presence of adenovirus and Epstein Barr Virus (EBV) infection were not monitored routinely and performed guided by symptomatology. All patients had tunneled central venous access (Hickman double lumen catheter). Neutrophil engraftment was defined as an absolute neutrophil count of more than 500/mm3 for 3 consecutive days and platelet engraftment was defined as an unsupported platelet count more than 20,000/mm3 for 7 consecutive days [8]. Failure to achieve neutrophil engraftment by day 28 of stem cell infusion was taken as primary graft failure [8]. Toxicities were graded according to the Common Terminology Criteria for Adverse Events (CTCAE).
HLA Typing and Chimerism Analysis
HLA typing was performed by next-generation sequencing. Antibodies in the recipient to donor HLA class I and II antigens were tested using a single antigen bead assay. Donor-recipient chimerism was assessed through polymerase chain reaction (PCR) based amplification. Chimerism testing was assessed at Day + 30 and Day + 90 and whenever clinically indicated.
Statistical Analysis
Overall survival (OS) was calculated from the date of stem cell infusion to date of death or last follow-up. Baseline characteristics are reported as descriptive statistics and OS was estimated using the Kaplan–Meier method. The cumulative incidence rates of non-relapse mortality (NRM), acute GVHD (aGVHD), and chronic GVHD (cGVHD) were also computed. All analyses were performed using SPSS version 20 (IBM, Armonk, NY).
Result
Patient and Donor Characteristics
A total of twenty-one patients with a median age of 15 years (range 1.5–43 years) underwent haploidentical HSCT from a family donor. Fourteen out of the 21 (66%) patients were pediatric (less than 18 years age) and 14/21 (66%) patients were males. Patient characteristics are detailed in Table 2. The primary diagnosis of patients was acute lymphoblastic leukemia (ALL) in 8, acute myeloid leukemia (AML) in 10, chronic myeloid leukemia (CML) blast crisis, and accelerated phase in 2 and 1 respectively. All patients were in complete remission (CR) before the transplant and their pretransplant workup for the cardiac, renal, hepatic, and pulmonary function was normal. Seven patients were transplanted in first CR (ALL: 2, AML: 2 and CML: 3) and 14 patients in second CR (ALL: 6 and AML: 8). Myeloablative conditioning regimen was used in 20 patients. One patient with AML received a reduced-intensity conditioning regimen due to life-threatening toxicities during the induction and consolidation phase of treatment. Initially, all patients in our study received a TBI based conditioning regimen except one child with ALL, who has received chemotherapy based conditioning regimen because of age (1.5 years). Over time we have changed our policy to using TBI based conditioning regimen for lymphoid leukemia and chemotherapy-based regimen for myeloid leukemia.
The median age of donors was 39 years (range 17–70). Most of the donors were male (n = 18), the father being the most common (n = 15). A sex mismatch was present in eight patients, of which six were female recipients and two were male recipients. Ten out of 21 donors had mismatched ABO blood groups, among these 3 were major and 7 were a minor mismatch. None of the recipients had donor-specific antibodies. All peripheral blood stem cell collections from donors were performed through peripheral access and none had complications due to the procedure.
Engraftment and Chimerism
The mean dose of CD34 + cells transfused to patients was 6 × 106/kg/recipient body weight (range: 4–8.6 × 106/kg). The median time to neutrophil engraftment was 14 days (range 12–23 days) and platelet engraftment was 14 days (range 12–54). One patient had primary graft failure. None had secondary graft failure. Donor chimerism at day + 30 and day + 90 was greater than 96% in all the remaining patients who are alive and are on follow-up.
Toxicity
Toxicities are detailed in Table 3 Seven of 8 patients had hemorrhagic cystitis. Cystitis was associated with BK virus infection in urine in 4 patients and adenovirus infection in one patient. CMV reactivation was observed in 15 patients and all responded well to preemptive therapy with ganciclovir. One patient had a probable pulmonary fungal infection (radiological) and was managed with amphotericin B.
Among the gastrointestinal toxicities, Mucositis was observed in all the patients (n = 21) for a median of 8 days (range 2–63 days). Grade 3 and 4 mucositis were observed in 50% of patients (n = 12). Sixteen patients (76%) patients required total parenteral nutrition (TPN). The median duration of TPN was 8 days (range 3–70 days). Nausea and vomiting were observed in 18 (85%) and diarrhea in 11 patients (52%). Sinusoidal obstruction syndrome (SOS) of the liver, was observed in 1 patient on day + 8 of transplant. This patient died on day + 13 due to sepsis and multi-organ dysfunction.
GVHD
Two patients developed aGVHD (9.5%), and six patients developed cGVHD (28.5%), of which two patients developed both types of GVHD (9.5%). Cumulative incidence of acute GVHD was 19%, at a median of 74 days (range: 54–96 days), whereas for chronic GVHD was 38%, at a median of 184 days (range: 156–410 days). Most patients had GVHD limited to one organ, whereas only one patient had GVHD in 3 organs. GVHD details have been provided in Table 4.
Treatment-Related Mortality (TRM), Relapses and Survival Outcomes
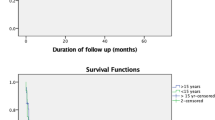
The median follow-up was 26 months and the two-year OS was 38% with a median OS of 17 months (Fig. 1). Nine out of 21 patients (42.8%) are leukemia-free on follow-up. Twelve (57.1%) patients died during the study period among whom eight (38%) had early transplant-related (less than 100 days) mortality. Among the 12 who died, 8 were due to TRM, and 4 were due to relapse of disease. TRM was observed in 3 patients with AML, 4 with ALL, and one with CML.
The median follow-up for adult and pediatric patients (< 18 years) was 29 and 25 months respectively. The 2 year OS for adult patients (n = 7) was 57.1% and for pediatric patients (n = 14) was 25% (P = 0.46). Among the 14 pediatric patients, 5 (36%) are alive and in CR, 4 (29%) have died due to disease relapse and 5 (36%) died due to TRM. Among the 7 adult patients, 4 (57%) are alive and in CR and 3 (43%) patients have died due to TRM.
Most patients had multiple factors contributing to mortality. Sepsis was the most common cause of TRM (n = 6) followed by encephalitis due to unknown causes (n = 2). One patient with sepsis had graft failure, one had SOS of the liver, one had aGVHD and fungal pneumonia and one had secondary hemophagocytic lymphohistiocytosis (HLH). Gram-negative multidrug-resistant (MDR) organism was cultured from 4 patients with sepsis (3 patients had Klebsiella pneumoniae and one Escherichia coli). Two of our patients died due to meningoencephalitis without a known cause. Cerebrospinal fluid PCR for Herpes simplex virus (HSV), Adenovirus, and Japanese encephalitis virus and blood PCR for EBV and CMV were negative in both the patients who developed meningoencephalitis. One patient with encephalitis also had hemorrhagic cystitis. All the TRM occurred within day 60 of the transplant.
Among the 4 relapses, 3 were observed in AML (4.5 months, 17 months, and 18 months post-transplant respectively) and one in ALL (3 months post-transplant).
Discussion
A meta-analysis of 30 studies including 22 974 participants comparing haploidentical HSCT with PTCY versus other donor transplants in adults observed that haploidentical HSCT was associated with increased all-cause mortality and NRM when compared to MSD HSCT [9]. Haploidentical HSCT had similar all-cause mortality but reduced NRM in comparison to MUD HSCT. Relapses were similar between haploidentical HSCT and MSD HSCT but more in comparison to MUD HSCT. This data indicates that haploidentical HSCT is a reasonable alternative for patients who do not have an MSD.
Data from Indian Stem Cell Transplant Registry (ISCTR) has shown that between 2102 and 2018 haploidentical HSCT accounted for 25% of allogeneic HSCT in children (< 18 years) and 20% in adults (personal communication).
Jaiswal et al. reported the outcomes of haploidentical HSCT in 25 children treated at their center [10]. Twenty of the 25 patients had acute leukemia and the rest had non-malignant conditions. They reported an aGVHD incidence of 40.3% and a cGHVD incidence of 16.7%. In contrast, we observed an aGVHD incidence of 19% and a cGVHD incidence of 38%. The platelet and neutrophil engraftment was 14 days in their study and was comparable to our observation. Their 2-year failure-free survival was 63.5% and 1 year NRM was 24%.
George et al. from Christian Medical College, Vellore, India, reported their outcomes on 149 patients who underwent 159 haploidentical HSCT between 2010 and 2017 [11]. Eight-five patients in their study had malignant neoplasms. aGVHD was seen in 32% of evaluable patients which is higher than what was observed in our study. Bacteremia was observed in 41% (the majority were gram-negative) and viral infections in 68% (CMV and BK virus). The 2 year OS for the entire cohort was 39.2% and comparable to our 2 year OS of 38%.
Nataraj et al. have reported the outcomes of 120 patients with AML who were treated with Allogenic HSCT at their center [12]. Forty-six patients in their cohort underwent haploidentical HSCT. The incidence of aGVHD (40.9% vs 32.6%; p = 0.372) and cGVHD (16.7% vs 15.2%; p = 0.837) were similar in MSD and haploidentical transplantation. However, the day-100 and overall survival were significantly better in the MSD cohort.
Alpha/Beta T-cell and CD19 B-cell depletion of donor stem cells ex-vivo is one method of reducing GVHD in a haploidentical transplant. Bhatt et al. reported their outcomes in haploidentical HSCT using this technique [13]. Among the 22 patients in the study, nine had hematological malignancy. The aGVHD incidence was 5% and none of the patients had cGVHD. The TRM was 14% and one-year event-free survival was 77%. The advantages of using Alpha/Beta T-cell and CD19 B-cell depletion are that patients do not require GVHD prophylaxis. However, it is expensive compared to PTCY and it has lesser graft versus leukemia effect.
Four out of 21 (19%) patients in our study died due to MDR gram-negative bacterial sepsis. A study from the Francophone Society of Stem Cell Transplantation and Cellular Therapy (SFGM-TC) on 381 patients who underwent haploidentical HSCT reported that infections accounted for 45.7% of the deaths and 40.9% infections were bacterial and 34.1% viral [14].
Cytokine release syndrome (CRS) is observed in patients undergoing haploidentical HSCT post stem cell infusion [15]. CRS is seen during the first few days after stem cell infusion and can be difficult to differentiate from sepsis, engraftment syndrome, and (HLH) [16]. All the above conditions can co-exist in a patient. We did not formally grade symptoms suggestive of CRS in our patients or measure inflammatory markers like interleukin-6 or use tocilizumab (anti-IL-6). All our patients developed a fever before engraftment and few required inotropic support and oxygen, and these symptoms were managed as sepsis.
Adult patients in our study had a better 2 year OS compared to pediatric patients (57% vs 25%, P = 0.46). However, the TRM rates in adult and pediatric patients were similar (43% vs 36% respectively). Pediatric patients had higher relapse mortality (29%) compared to adult patients (0%) and this accounted for their inferior OS. The higher relapse mortality in children compared to adults could be attributed to more transplants in CR2 in children (72%) compared to adults (57%).
We used a TBI based myeloablative conditioning regimen for 7 out of 8 patients with ALL. A recent European Bone Marrow Transplant (EBMT) group study observed that TBI based regimen for haploidentical transplant in patients with ALL resulted in a significant reduction of NRM, translating into a better leukemia-free survival without impacting aGVHD, chronic GVHD, or OS when compared to non-TBI based chemotherapy regimens [17]. Access to TBI may be restricted in a few centers in India and therefore a chemotherapy based conditioning regimen may be appropriate in such situations.
All our patients received a peripheral blood stem cell graft. A meta-analysis has shown no difference in outcomes between a peripheral blood stem cell graft and a bone marrow graft in haploidentical HSCT with PTCY [18].
It is our policy to give donor lymphocyte infusion (DLI) if day 30 donor T-cell chimerism is less than 96% or there is a loss of donor chimerism and/or there is a molecular relapse. All patients in our study who engrafted achieved day 30 chimerism > 96%, none had a loss of donor chimerism and patients who relapsed had an overt morphological relapse. We did not routinely monitor post-transplant minimal residual disease status and therefore could not identify early relapses. Therefore, none of our patients received DLI.
Our study has limitations that include the retrospective collection of data and a definitive cause for few infections could not be ascertained due to the non-availability of an extensive viral testing panel.
To conclude the present study is one of the few reports that has investigated the outcomes of haploidentical HSCT from India. Sepsis especially caused gram-negative MDR bacteria remains a major challenge in the success of haploidentical HSCT in India.
Data Availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
McCurdy SR, Luznik L (2019) How we perform haploidentical stem cell transplantation with posttransplant cyclophosphamide. Blood 134(21):1802–1810
Fuchs EJ (2012) Haploidentical transplantation for hematologic malignancies: where do we stand? Hematolo Am Soc Hematol Educ Program 2012:230–236
O’Donnell PV, Luznik L, Jones RJ et al (2002) Nonmyeloablative bone marrow transplantation from partially HLA-mismatched related donors using post-transplantation cyclophosphamide. Biol Blood Marrow Transpl 8:377–386
Robinson TM, O’Donnell PV, Fuchs EJ, Luznik L (2016) Haploidentical bone marrow and stem cell transplantation: experience with post-transplantation cyclophosphamide. Semin Hematol 53:90–97
Dedhia L, Gadekar S, Mehta P, Parekh S (2015) HLA haplotype diversity in the South Indian population and its relevance. Indian J Transplant 9:138–143
Kulkarni U, George B (2019) Access to hematopoietic stem-cell transplantation in India. J Postgrad Med 65:1–4
Debals-Gonthier M, Siani C, Faucher C et al (2018) Cost-effectiveness analysis of haploidentical vs matched unrelated allogeneic hematopoietic stem cells transplantation in patients older than 55 years. Bone Marrow Transpl 53:1096–1104
Hutt D. (2018) Engraftment, Graft Failure, and Rejection. 2017 Nov 22. In: Kenyon M, Babic A, editors. The European Blood and Marrow Transplantation Textbook for Nurses: Under the Auspices of EBMT [Internet]. Cham (CH): Springer. Chapter 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK543659/
Gagelmann N, Bacigalupo A, Rambaldi A et al (2019) Haploidentical stem cell transplantation with posttransplant cyclophosphamide therapy vs other donor transplantations in adults with hematologic cancers: a systematic review and meta-analysis. JAMA Oncol 5:1739–1748
Jaiswal SR, Chakrabarti A, Chatterjee S, Ray K, Chakrabarti S (2016) Haploidentical transplantation in children with unmanipulated peripheral blood stem cell graft: the need to look beyond post-transplantation cyclophosphamide in younger children. Pediatr Transpl 20(5):675–682
George B, Abraham A, Korula A et al (2018) Haploidentical transplants using post transplant cyclophosphamide (ptcy) are associated with good outcomes if transplanted with early disease - a single centre analysis from India. Blood 132(Supplement 1):4652
Nataraj KS, Prabhu S, Bhat S et al (2020) Hematopoietic stem cell transplant outcomes in patients with acute myeloid leukemia from a tertiary care center in South India. Biol Blood Marrow Transplant 26:123–124
Bhat S, Ngangbam S, Iqbal W et al (2017) Outcomes of myeloablative haploidentical hematopoietic stem cell transplant in pediatric patients with TCR a/b; and CD 19 depletion. Biol Blood Marrow Transplant 23:S191–S192
Fayard A, Daguenet E, Blaise D et al (2019) Evaluation of infectious complications after haploidentical hematopoietic stem cell transplantation with post-transplant cyclophosphamide following reduced-intensity and myeloablative conditioning: a study on behalf of the Francophone Society of Stem Cell Transplantation and Cellular Therapy (SFGM-TC). Bone Marrow Transplant 54:1586–1594
Abboud R, Keller J, Slade M et al (2016) Severe cytokine-release syndrome after t cell-replete peripheral blood haploidentical donor transplantation is associated with poor survival and anti-il-6 therapy is safe and well tolerated. Biol Blood Marrow Transplant 22(10):1851–1860
Abid MB, Hamadani M, Szabo A, Hari PN, Graham MB, Frank MO, Runaas L (2020) Severity of Cytokine Release Syndrome and Its Association with Infections after T Cell-Replete Haploidentical Related Donor Transplantation. Biol Blood Marrow Transplant 26(9):1670–1678
Dholaria B, Labopin M, Angelucci E et al (2019) Outcomes of total body irradiation-versus chemotherapy-based myeloablative conditioning regimen in haploidentical hematopoietic cell transplantation with post-transplant cyclophosphamide for acute lymphoblastic leukemia: ALWP of the EBMT Study. Blood 134((Supplement_1)):320
Yu X, Liu L, Xie Z et al (2019) Bone marrow versus peripheral blood as a graft source for haploidentical donor transplantation in adults using post-transplant cyclophosphamide-a systematic review and meta-analysis. Crit Rev Oncol Hematol 133:120–128
Acknowledgements
We would like to acknowledge our transplant coordinator, Ms. Vanita for help in coordinating and streamlining the transplant process.
Funding
None.
Author information
Authors and Affiliations
Contributions
All co-authors have reviewed the manuscript and have contributed substantively and intellectually to the work described.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the ethical committee of the hospital and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Batra, A., Perumal Kalaiyarasi, J., Kannan, K. et al. Haploidentical Hematopoietic Stem Cell Transplantation in Leukemia’s: Experience from a Cancer Center in India. Indian J Hematol Blood Transfus 37, 463–471 (2021). https://doi.org/10.1007/s12288-020-01374-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-020-01374-w