Abstract
Aspergillus lateral-flow device (LFD) was recently introduced as a practical tool for the diagnosis of invasive aspergillosis (IA). We investigated the performance of Aspergillus-LFD as a point-of-care test for the diagnosis of IA. Serum samples were collected twice weekly from patients who received intensive chemotherapy for acute leukemia, or recepients of allogeneic stem cell transplantation. Aspergillus galactomannan (GM) antigen, 1,3-beta-d-glucan and Aspergillus-LFD tests were carried out according to manufacturers’ recommendations. GM testing was repeated with a modified procedure which was proven to increase the sensitivity. Aspergillus-LFD was performed without applying any pretreatment procedure to allow the kit to fit as a point-of-care test. Fungal infections were categorized according to European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria. A total of 75 neutropenia episodes in 64 patients were prospectively followed between February 2012 and January 2013. Probable IA was diagnosed in 11 patients, probable pulmonary fungal disease was diagnosed in one patient, and rhinocerebral aspergillosis was diagnosed in one patient. Fungemia was detected in two patients. Aspergillus-LFD was positive in serum of a patient with probable IA and in the bronchoalveolar lavage fluid of an other patient with probable IA. Aspergillus-LFD was false positive in serum of two patients. Although there was no radiological finding of IA or documented fungemia, fever resolved after empirical caspofungin therapy in one of these patients. The sensitivity of Aspergillus-LFD as a point-of-care test without any pretreatment of serum sample is low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diagnosis of IA is a challange in high risk hematology patients. Severe hypoxemia or thrombocytopenia usually limit the deep tissue sampling for culture which is the golden standard for the diagnosis. The well characterized serological tools such as galactomannan (GM) and 1,3-beta-d-glucan (BDG) need spesific laboratory equipment and experienced staff [1].
Aspergillus-lateral-flow device (Aspergillus-LFD) has been recently developed by Chris Thornton from the University of Exeter, UK. This test is an immuno-chromatographic assay which is based on the detection of Aspergillus antigen released during the hyphal invasion by a monoclonal IgG antibody JF5. It can be performed easily in bronchoalveolar lavage (BAL) fluid and serum specimens without any specific laboratory equipments, and the test result is available approximately in 15 min [2, 3]. A recent meta-analysis reported a sensitivity and specificity of 86 and 93 % in BAL fluid, and 68 and 87 % in serum for Aspergillus-LFD [4]. There are two studies which examined the performance of Aspergillus-LFD in human serum. A pretreatment protocol including EDTA treatment and heating was followed in both of the studies contrast to the initial recommendations as direct inoculation of human serum to LFD device [5–7]. In an animal infection model, there were no significant differences between the positivity rate either the serum was processed with the pretreatment protocol or not [8]. The direct inoculation of serum to LFD assay without any pretreatment enables Aspergillus-LFD as a promising point-of-care test at bedside. Here, we aimed to analyze the performance of Aspergillus-LFD as point-of-care test for the diagnosis of IA in high risk hematology patients.
Patients and Methods
Study Setting and Patient Selection
This study was conducted at the Erciyes University Hospital, a 1300-bed tertiary care centre in Kayseri, Turkey. The haematology ward has 30 beds and there is a 38-bed HSCT centre. The study was approved by the ethics committee of the Erciyes University Medical Faculty and patients were required to give written informed consent. Patients who had undergone chemotherapy for acute myelogenous leukaemia (AML), acute lymphocytic leukaemia (ALL), or allogenic Hematopoietic stem cell transplantation (HSCT) with an expected neutropenia period longer than 7 days were included in the study. AML/ALL patients who were previously included in the study and received an other cycle of chemotherapy after recovering from the first neutropenia episode or received allogenic HSCT were also included in the study for the second neutropenia episode.
Institutional Antifungal Prophylaxis and Febrile Neutropenia Follow-up Protocol
During the study period, fluconazole was the antifungal prophylaxis for patients receiving chemotherapy for ALL and recepients of allogeneic HSCT. Posaconazole prophylaxis was used in patients receiving remission-induction chemotherapy for AML. Patients who had a previous history of proven, probable or possible IA received voriconazole as secondary prophylaxis. Thoracic multislice computed tomography (CT) was performed in the case of neutropenic fever which does not resolve in 72–96 h or fever relapsing after 48 h of defervescence under broad spectrum antibacterial therapy, presence of any respiratory symptoms, and/or positive GM antigenemia. Additional examinations such as abdominal ultrasound, sinus or brain CT, or bronchoalveolar lavage (BAL) were performed when required. All CT images were independently re-evaluated by an expert radiologist who was blind to the clinical status of the patients after the study was completed.
Sample Collection and Biomarker Testing
During the study period, patients were screened for GM antigenemia (Platelia Aspergillus ELISA; Bio-Rad Laboratories) twice a week as a part of routine care that were processed according to the manufacturer’s instructions. The results were expressed in terms of the GM index. Cut-off level of 0.7 were used to define the positivity of the test [1]. Screening tests were started at the day of an absolute neutrophil count of <500/mm3 until recovery of neutropenia or diagnosis of IFDs.
The serum samples that were used for BDG and Aspergillus-LFD testing were drawn at the same time when blood were drawn for routine GM screening. All serum samples were separated, aliquoted and frozen at −20 °C until Aspergillus-LFD and BDG testing. BDG levels in sera were assayed using the Fungitell kit (Associates of Cape Cod, East Falmouth, MA, USA) according to manufacturer’s specifications. The cut-off was 80 pg/ml [1].
The serum samples from patients with radiologic evidence of IA were re-tested by a modified methodology which was previously proven to increase the sensitivity of GM antigen detection [9]. Serum samples which were drawn closer to the radiologic diagnosis IA and a number of serum samples from patients without IA were tested (1–10 ratio) with modified protocol.
For Aspergillus-LFD testing, the serum samples were thawn at room temperature, mixed by vortexing and centrifuged for 1 min at 14,000 rpm before testing. Tissue culture medium (TCM) which consists of RPMI-1640 medium, 10 % (v/v) fetal calf serum, 1 % (v/v) of 200 mM l-glutamine solution, and sodium azide (0.02 % w/v) as preservative was prepared. The serum was diluted with TCM (1:1), and 100 µl serum was applied to the release port of the device by using a sterile pipette tip. Then tests were allowed to run for 15 min at room temperature. Results were recorded as weak positive, moderate positive, and strong positive. In the absence of the Aspergillus antigen, no complex was formed in the zone containing solid-phase antibody, and a single internal control line was observed. This result was recorded as negative for Aspergillus antigen [5]. All tests were performed twice. An amount of 100 µl BAL fluid was tested without any pretreatment [5]. Different concentrations of BAL fluid were also tested to observe the role of sample volume on the results.
Two users independently check each LFD device in a blinded fashion. Concurrent results were recorded, whereas incongruent results were ratified by a third user. The researchers who carried out the tests were blinded to the patients clinical situation, and results of GM antigen test performed as a part of routine patient care.
Definitions for Invasive Fungal Disease and Response to Antifungal Therapy
The European Organization for Research and Treatment of Cancer and the Mycoses Study Group (EORTC/MSG) criteria were used to categorize the patients as having proven, probable, or possible IA [10]. Response to systemic antifungal therapy was assessed based on EORTC/MSG consensus criteria at the time of discharge from the hospital. Success was defined as radiological stabilization (defined as 25 % reduction in the diameter of the lesion), resolution of all attributable symptoms and signs of IA [11].
Statistical Analysis
For statistical analysis, patients with radiological evidence of IA were considered as true- positive cases, and patients without any radiological evidence of IA were considered as true-negative cases. Performance parameters for each assay were determined by construction of 2 × 2 tables with true positives being cases, with degree of certainty as defined by the EORTC/MSG possible IA, and true negatives being controls with no EORTC/MSG evidence of IA. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for the all assays. Serum samples from patients with fungemia were excluded from the statistical analysis performed for BDG because positivity of serum BDG during fungemia can not be labeled as true or false positive when evaluating the performance of BDG for IA. All statistical analyses were performed using MedCalc for Windows, version 11.5.1.0 (MedCalc Software, Mariakerke, Belgium).
Results
A total of 75 neutropenia episodes in 64 patients were prospectively followed between February 2012 and January 2013. Median age of the patients were 41-years (range 18–69 years), and 34 of them were female. The underlying hematological disease was AML in 38 patients, ALL in 24 patients, biphenotypic leukemia in 1 patient, and aplastic anemia in 1 patient. Seven out of 24 patients with ALL, 5 out of 38 patients with AML, and 1 patient with aplastic anemia received allogeneic HSCT. Antifungal propylaxis was posaconazole in 31 neutropenia episodes, fluconazole in 42 neutropenia episodes, and voriconazole was used as secondary propylaxis in two neutropenia episodes.
Three patients were diagnosed as probable IA. Nine patients were diagnosed as possible IA with radiological findings.The most common radiological lesion was halo with a nodule. One patient was diagnosed as rhinocerebral aspergillosis When the modifed GM results were taken into account, 12 patients had probable IA (Supplement 1).
Aspergillus-LFD was strong positive in the serum of one patient with probable IA. While GM antigen carried out with standard methodology was negative in this patient, BDG and GM antigen carried out with modified procedure were also positive. The consecutive serum samples from this patient were as strong positive result from the first sample which was followed by a moderate positive serum, and the consecutive serum sample became negative under antifungal therapy. Aspergillus-LFD was false positive in serum of two patients (one strongly positive, the other weak positive) without any radiological evidence of IFDs. One of these patients was receiving induction chemotherapy for AML under posacoconazole prophylaxis. BDG was also positive in the serum sample which gave strong false positive for Aspergillus-LFD. Although there was no radiological finding of IA or documented fungemia, fever resolved after empirical caspofungin therapy. The consecutive serum samples obtained under caspofungin was weak positive and became negative. Due to the limited kit stock we were able to test only ten serum samples from patients with probable IA by using a pretreatment procedure at the end of the study [5]. There were two positive results. One serum sample which was obtained from a patient with previous negative Aspergillus-LFD gave a moderate positive reaction. Also, the serum sample which was positive without any pretreatment was positive when tested after pretreatment.
Aspergillus-LFD carried out in BAL fluid of a patient with thoracic lesions concordant with IA was moderate positive despite 2 days of mold active antifungal therapy. Radiological lesions were completely healed after a long course of liposomal amphotericin B followed by oral posaconazole (Fig. 1). We get the best visible band for BAL fluid when the sample was centrifugated at 14,000 rpm for 3 min and 100 µl was applied to the device (Fig. 1).
Blastoschizomyces capitatus fungemia was detected in a patient with AML receiving posaconazole prophylaxis, and non-albicans Candida spp. was isolated from a patient with ALL who was under empirical caspofungin therapy. BDG was >80 pg/ml at an avarage of 1 week before the results of the blood cultures were available in patients with fungemia.
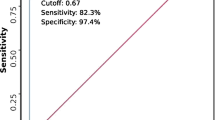
A total of 354 serum samples were included in the statistical analysis. The sensitivity of Aspergillus-LFD, GM, and BDG were as 13.7, 35.7, and 53.5 %; the specificity of Aspergillus-LFD, GM, and BDG were as 99.1, 99.6, and 76 % (Table 1).
To analyze the diagnostic performance of modified GM procedure, we tested 13 serum samples from patients with radiological evidence of IA, and 130 serum samples from patients without IA. The sensitivity, specificity, positive predicitive value (PPV), and negative predictive value (NPV) were as; 92.3 (95 % CI 62.1–99.6), 97.6 % (95 % CI 92.3–99.4), 80 % (95 % CI 51.3–94.6), and 99.2 % (95 % CI 94.9–99.9).
When we analyzed the factors potentially related to false positive BDG; presence of bacteraemia, erythrocyte infusion, platelet infusion, use of leukocyte filters, and albumin infusion were not found to be related with false positive BDG (Table 2). None of the patients included in this study were diagnosed as Pneumocyctis jiroveci pneumonia (PCP) or received treatment with suspicion of PCP which can cause BDG positivity.
Discussion
In this study, we were able to identify Aspergillus-LFD positivity only in serum of one patient with probable IA and in BAL fluid of another patient with probable IA. When we carried out Aspergillus-LFD in pretreated serum from patients with probable IA, we were able to identify one more positive result in one of the serum samples. However, the tests with pretreatment procedure had a limitation with the shelf-life of the device. Aspergillus-LFD has a shelf-life of 1 year [5], and the tests were carried out nearly 1 year after supplying the kits. When we compare our findings with the previously published studies which pretreated the serum before Aspergillus-LFD [6, 7], it is clear that pretreatment increases the sensitivity of Aspergillus-LFD in the diagnosis of IA. However, the pretreatment protocols in two studies were different, and apart from the pretreatment procedure, White et al. [7], determined Aspergillus specific test line in a period 10-20 min while this period was 15 min in the study by Held et al. [6]. These findings suggest that further studies are requried to optimize the methodology for Aspergillus-LFD for testing serum samples.
One of the promising findings of our study is the very rare false positive results for Aspergillus-LFD. This suggest that whenever a positive results is obtained, this should trigger the diagnostic and therapeutic pathways.
GM (carried out with the standard procedure) was negative in serum of 10 out of 13 patients with radiological lesions concordant with IA (supplement 1). When we repeated GM with the modified methodology, the sensitivity increased from 35.7 to 92.3 % and observed a slight decrease in the specificity from 99.6 to 97.6 %. Only three serum samples from patients without IA were false positive at a threshold of ≥0.7 with the modified procedure. Our findings confer the statement of possible IA as early aspergillosis resulted from the re-analysis of big drug trials according to revised EORTC/MSG criteria [12, 13]. In patients with pulmonary IA the halo sign on a CT scan was reported to be the first reliable sign of IA, with a low sensitivity (33 %), but high specificity (93 %) [14]. The radiological finding was halo with nodule for nine patients with IA and the early CT screening in 72–96 h for patients with persistent fever can be the reason for detecting the cases without any biomarker positivity in our study.
The major benefit of BDG screening was early diagnosis of fungemia in our study. If BDG screening was part of the routine diagnostic algorithm, commencing early prompt antifungal therapy would be possible in these patients based on persistent fever and BDG positivity. However, cost-effectivity of this approach needs to be well characterized by taking into account of both fungemia insidence and the rate of false positive BDG tests.
The major limitation of our study was lack of proven cases of IA. This was also the case in the two studies which report promising results for Aspergillus-LFD, the number of proven IA cases were only nine [6,7]. Also, posaconazole prophylaxis in five patients with IA, can be an important limitation of GM screening and Aspergillus-LFD testing in our setting. A multicenter study with adequate number of patients with proven IA and with a methodology of real time testing from serum samples obtained from the patients without mold active prophylaxis will be helpful to establish the role of Aspergillus-LFD for the diagnosis of IA.
As a conclusion, none of the serological tools that are used to diagnose IA is perfect. Aspergillus-LFD is a candidate to replace or adjust the complex laboratory tests for the diagnosis of IA, however, there is a need for better standardization of the pretreatment procedure with further studies for serum samples.
References
Marchetti O, Lamoth L, Mikulska M, Viscoli C, Verweij P, Bretagne S, The European Conference on Infections in Leukemia (ECIL) Laboratory Working Groups (2012) ECIL recommendations for the use of biological markers for the diagnosis of invasive fungal diseases in leukemic patients and hematopoietic SCT recipients. Bone Marrow Transplant 47:846–854
Thornton CR (2008) Development of an immunochromatographic lateral-flow device for rapid serodiagnosis of invasive aspergillosis. Clin Vaccine Immunol 15:1095–1105
Wiederhold NP, Thornton CR, Najvar LK, Kirkpatrick WR, Bocanegra R, Patterson TF (2009) Comparison of lateral flow technology and galactomannan and (1-3)-beta-d-glucan assays for detection of invasive pulmonary aspergillosis. Clin Vaccine Immunol 16:1844–1846
Pan Z, Fu M, Zhang J, Zhou H, Fu Y, Zhou J (2015) Diagnostic Accuracy of a novel lateral-flow device in invasive aspergillosis: a meta-analysis. J Med Microbiol 2015(64):702–707
Thornton C, Johnson G, Agrawal S (2012) Detection of invasive pulmonary aspergillosis in haematological malignancy patients by using lateral-flow technology. J Vis Exp 61:3721
Held J, Schmidt T, Thornton CR, Kotter E, Bertz H (2013) Comparison of a novel Aspergillus lateral-flow device and the Platelia® galactomannan assay for the diagnosis of invasive aspergillosis following haematopoietic stem cell transplantation. Infection 41:1163–1169
White PL, Parr C, Thornton C, Barnes RA (2013) Evaluation of real-time PCR, galactomannan enzyme-linked immunosorbent assay (ELISA), and a novel lateral-flow device for diagnosis of invasive aspergillosis. J Clin Microbiol 51:1510–1516
Wiederhold NP, Najvar LK, Bocanegra R, Bocanegra R, Kirkpatrick WR, Patterson TF, Thornton CR (2013) Interlaboratory and interstudy reproducibility of a novel lateral-flow device and influence of antifungal therapy on detection of invasive pulmonary aspergillosis. J Clin Microbiol 51:459–465
Mennink-Kersten MA, Ruegebrink D, Klont RR, Warris A, Blijlevens NM, Donnelly JP, Verweij PE (2008) Improved detection of circulating Aspergillus antigen by use of a modified pretreatment procedure. J Clin Microbiol 46:1391–1397
De Pauw B, Walsh TJ, Donnelly JP, Tevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA, Denning DW, Patterson TF, Maschmeyer G, Bille J, Dismukes WE, Herbrecht R, Hope WW, Kibbler CC, Kullberg BJ, Marr KA, Muñoz P, Odds FC, Perfect JR, Restrepo A, Ruhnke M, Segal BH, Sobel JD, Sorrell TC, Viscoli C, Wingard JR, Zaoutis T, Bennett JE (2008) Revised definitions of ınvasive fungal disease from the European organization for research and treatment of cancer/ınvasive fungal ınfections cooperative group and the national ınstitute of allergy and ınfectious diseases mycoses study group (EORTC/MSG) consensus group. Clin Infect Dis 46:1813–1821
Segal BH, Herbrecht R, Stevens DA, Ostrosky-Zeichner L, Sobel J, Viscoli C, Walsh TJ, Maertens J, Patterson TF, Perfect JR, Dupont B, Wingard JR, Calandra T, Kauffman CA, Graybill JR, Baden LR, Pappas PG, Bennett JE, Kontoyiannis DP, Cordonnier C, Viviani MA, Bille J, Almyroudis NG, Wheat LJ, Graninger W, Bow EJ, Holland SM, Kullberg BJ, Dismukes WE, De Pauw BE (2008) Defining responses to therapy and study outcomes in clinical trials of invasive fungal diseases: Mycoses Study Group and European Organization for Research and Treatment of Cancer consensus criteria. Clin Infect Dis 47:674–683
Cornely OA, Maertens J, Bresnik M, Ebrahimi R, Dellow E, Herbrecht R, Donnelly JP (2011) Efficacy outcomes in a randomised trial of liposomal amphotericin B based on revised EORTC/MSG 2008 definitions of invasive mould disease. Mycoses 54:449–455
Herbrecht R, Patterson TF, Slavin MA, Marchetti O, Maertens J, Johnson EM, Schlamm HT, Donnelly JP, Pappas PG (2015) Application of the 2008 definitions for invasive fungal diseases to the trial comparing voriconazole versus Amphotericin B for therapy of invasive aspergillosis. A collaborative study of the Mycoses Study Group (MSG 05) and the EORTC Infectious Diseases Group. Clin Infect Dis 60:713–720
Maertens J, Van Eldere J, Verhaegen J, Verbeken E, Verschakelen J, Boogaerts M (2002) Use of circulating galactomannan screening for early diagnosis of invasive aspergillosis in allogeneic stem cell transplant recipients. J Infect Dis 186:1297–1306
Acknowledgments
This study was supported by Erciyes University Scientific Foundation (Project No: TSA-12-3951). Fungitell kits were supplied by Associates of Cape Cod, East Falmouth, MA, USA as a part research support programme. We thank to Dr. Chris Thornton for supplying Aspergillus lateral-flow devices for Kök-Biotechnics, Erciyes Teknopark, Kayseri. We also thank to Malcolm Finkelman who encouraged us to apply for research support programme of Cape Cod, East Falmouth, MA, USA. Erciyes University Scientific Foundation, Associates of Cape Cod, Malcolm Finkelman, and Dr. Chris Thornton did not have a role in planning, analysis or data interpretation and preparation of the manuscript. The initial results of Aspergillus-lateral flow device were shared with Dr. Chris Thornton, and initial results for Fungitell testing were shared with Malcolm Finkelman. The findings of this study were partially presented as posters at the 6th Trends in Medical Mycolology, Copenhagen, Denmark (2013) with title of “Aspergillus-lateral flow device as a point-of-care test for the diagnosis of invasive fungal infections in patients with leukemia or receiving allogenic stem cell transplantation” and at 24th European Congress of Clinical Microbiology and Infectious diseases, Barcelona, Spain with title of “A combined screening strategy for invasive fungal infections in high-risk haematology patients: early computed thoracic tomograpy and serum 1,3-beta-d-glucan”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
G.M. has received honarium for speaking at symposia and lecture organized by Gilead, financial compensation from Pfizer for the time and expenses for a meeting organised to discuss the content of a review paper, member of advisory board of Pfizer and Astellas, and received travel Grants form MSD, Pfizer, and Gilead to participate conferences. L.K. has recieved honarium for speaking at a lecture organized by Gilead. The other authors declared to have any completing interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Metan, G., Keklik, M., Dinç, G. et al. Performance of Galactomannan Antigen, Beta-d-Glucan, and Aspergillus-Lateral-Flow Device for the Diagnosis of Invasive Aspergillosis. Indian J Hematol Blood Transfus 33, 87–92 (2017). https://doi.org/10.1007/s12288-016-0653-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-016-0653-3