Abstract
Background
Mammography is the standard examination for breast cancer screening of woman aged ≥ 40 years. High breast density on mammography indicates that mammary gland parenchyma occupy a high percentage of the breast. The objective of this study was to investigate factors associated with breast density and the risk of high breast density for breast cancer.
Methods
A multicenter case–control study was performed in 530 patients and 1043 controls. Breast density was classified as C1–C4 using the Breast Imaging Reporting and Data System (BI-RADS). Clinical factors were obtained from questionnaires or medical records, and the influence of each factor (breast density, menopausal status, body mass index (BMI), parity, presence or absence of breastfeeding history, age at menarche, age at first birth, and familial history of breast cancer) on breast cancer risk in all patients was calculated as an age-adjusted odds ratio (OR). Multivariate logistic regression analyses were then performed in all patients and in pre- and postmenopausal and BMI-stratified groups using factors with a significant age-adjusted OR as adjustment factors.
Results
Age-adjusted ORs for breast cancer were significant for breast density, BMI, parity, and breast feeding, but not for age at menarche, age at first birth, or family history of breast cancer. In multivariate analysis, there was a significant correlation between breast density and breast cancer in postmenopausal women (OR for C1 vs. C2 1.90 [95% CI 1.34–2.70]; C1 vs. C4 2.85 [95% CI 1.10–7.16]). This correlation was also significant in patients in the third BMI quartile (22.3–24.5 kg/m2) (OR for C1 vs. C4 8.76 [95% CI 2.38–42.47]); and fourth BMI quartile (>24.5 kg/m2) (OR for C1 vs. C2 1.92 [95% CI 1.17–3.15]; C1 vs. C4 11.89 [95% CI 1.56–245.17]).
Conclusion
Breast density on mammography is a risk factor for breast cancer after adjustment for other risk factors. This risk is particularly high in postmenopausal women and those with a high BMI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mammography is the first-choice method for breast cancer screening and the only method with evidence for an effect on reduction of mortality for women aged ≥ 40 years [1]. In mammography, breast density is evaluated based on the Breast Imaging Reporting and Data System (BI-RADS) [2], as well as mass, calcification, architectural distortion, and other findings. High breast density indicates a high percentage of mammary gland parenchyma in the breast. The parenchyma is comprised of interstitium and mammary gland epithelium and has lower radiolucency than that of adipose tissue.
There are two problems with breast density on mammography. First, an increase in breast density limits detection of tumors in dense tissue, which decreases the sensitivity of mammography. This is referred to as a masking effect. In a study of 329,495 women screened by mammography in the US between 1996 and 1998, Carney et al. found sensitivities and specificities of 87% and 97%, respectively, in women with fatty breast (BI-RADS class 1, C1), but only 63% and 89%, respectively, in those with a high-density mammary gland (BI-RADS class 4, C4) [3]. The second problem is that an increase in breast density increases the risk of breast cancer. In a meta-analysis of 42 studies, McCormack et al. found that the relative risk of breast cancer in all women was 1.79 (95% CI 1.48–2.16) at 5–24%, 2.11 (95% CI 1.7–2.63) at 25–49%, 2.92 (95% CI 2.49–3.42) at 50–74%, and 4.64 (95% CI 3.64–5.91) at ≥ 75% breast density, indicating a strong association [4]. Similar findings were obtained in three case–control studies in Japanese subjects [5,6,7].
Age, delivery, and breastfeeding decrease breast density and breast cancer risk, whereas female hormone replacement therapy increases breast density and breast cancer risk [8]. In contrast, body mass index (BMI) decreases breast density, but increases breast cancer risk [9,10,11]. The effects of BMI on breast density and breast cancer risk are seemingly contradictory. However, there have been no reports on the confounding effects of BMI and breast density on breast cancer risk. Therefore, there are many unclear aspects of patient background that influence the association between high breast density and breast cancer risk, and risk stratification of patients with high breast density has not been established. In this study, we examined the association between breast density on mammography and breast cancer risk, and investigated factors that may influence this relationship.
Patients and methods
Subjects
A multicenter population-based case–control study was performed in women aged ≥ 20 years who were histologically diagnosed with non-invasive or invasive breast cancer and treated at Okayama University Hospital, Okayama Rousai Hospital, and Mizushima Kyodo Hospital (Okayama, Japan) and Kagawa Prefecture Central Hospital (Kagawa, Japan) between December 2010 and November 2011. The controls were women aged ≥ 20 years with no history of breast cancer who were screened for breast cancer at Mizushima Kyodo Hospital and Okayama Saiseikai Hospital (Okayama Japan), Kagawa Prefectural Cancer Detection Center (Kagawa, Japan), and Yakage Hospital. All subjects and controls gave written informed consent. This study was approved by the Institutional Ethics Committee on Human Research of Okayama University.
Mammography
Evaluation of breast density on mammography (mammographic density) was performed using a bilateral mediolateral oblique view for patients and controls. Based on the BI-RADS of the American College of Radiology, the mammographic density was classified as follows: C1, almost fatty (<25% glandular); C2, scattered fibroglandular densities (25–50% glandular); C3, heterogeneously dense (51–75% glandular); and C4, extremely dense (>75% glandular) [2]. The healthy side was evaluated in patients, and the bilateral sides were evaluated in controls. Independent judgments were made by two physicians and the concordance rate was determined. When the density differed between the bilateral sides in a control subject, the average was used for the density. If the judgments did not match, the final decision was made by discussion between the two physicians.
Lifestyle survey
Self-administered questionnaires were directly handed to the subjects. These were completed at home and sent back to Okayama University Hospital by mail. Data for the following items were extracted from the questionnaires and from medical records: age, menopausal status, height and body weight (at the times of diagnosis in patients and screening in controls), parity, breastfeeding, lactation, age at menarche, age at first birth, family history of breast cancer, and body mass index (BMI) calculated as body weight (kg)/square of height (m2). For familial history of breast cancer, the history of breast cancer was surveyed in mothers, daughters, and sisters (first-degree family history).
statistical analysis
The primary outcome was risk of breast cancer. Quartiles of BMI were determined and the subjects were classified into 4 groups. BMI, parity (0, 1, 2, ≥ 3), breastfeeding experience, family history of breast cancer, and mammographic density were analyzed as categorical variables; and age, age at menarche, and age at first birth were analyzed as continuous variables. In univariate analysis, categorical variables were analyzed by Chi-squared test or Fisher test, and continuous variables by Wilcoxon test. The influence of each factor (breast density, menopausal status, BMI, parity, presence or absence of breastfeeding history, age at menarche, age at first birth, and familial history of breast cancer) on the breast cancer risk in all patients was calculated as an age-adjusted odds ratio (OR). Following these calculations, multivariate analysis of breast cancer risk was performed in all patients and in pre- and postmenopausal patients using logistic regression analysis. In this model, analysis was performed using factors with a significant age-adjusted OR in all patients and age as adjustment factors. Similar multivariate analysis of breast cancer risk was performed in groups stratified by BMI quartiles, again using factors with a significant age-adjusted OR in all patients and age as adjustment factors. Patients with missing data were excluded from analyses. All statistical analyses were performed with JMP ver. 9.0.3 (SAS Institute). A P value below 0.05 was regarded as significant in all analyses.
Results
Consent was obtained from 654 patients and 1602 controls, and 614 patients (93.9%) and 1542 controls (96.3%) returned the self-administered questionnaires. Finally, both questionnaires with complete data and readable mammograms acquired at the time of diagnosis or screening were available in 530 patients and 1043 controls, and analysis was performed using this data set.
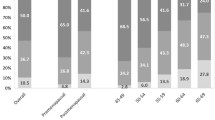
The patient background is shown in Table 1. The median ages of the patients and controls were 56 and 58 years, respectively. The mammographic density classes in the patients were C1 in 119 (22%), C2 in 227 (43%), C3 in 146 (28%), and C4 in 38 (7%); and those in the controls were C1 in 275 (26%), C2 in 370 (35%), C3 in 339 (33%), and C4 in 59 (6%). The rate of postmenopausal subjects was lower in patients than in control s(60% vs 69%), whereas the rates of subjects with parity and breastfeeding history were significantly higher in controls. The median BMI was 22.3 kg/m2 in patients and 22.1 kg/m2 in controls. There was no significant difference in age at menarche, age at first birth, or familial history between the two groups (Table 1). Independent judgments were made by two physicians with over 20 years of experience and the concordance rate was determined (Table 2). The α coefficient and concordance rate were 0.99 and 0.98 in patients, and 0.99 and 0.97 in controls.
Age-adjusted ORs of the mammographic density, BMI, parity, and breastfeeding experience were significant, but age at menarche, age at first birth, and family history of breast cancer were not significant (Table 3). In multivariate analyses in all patients and in pre- and postmenopausal groups performed using BMI, parity, breastfeeding experience, and age as adjustment factors, there was a significant correlation between breast cancer risk and mammographic density in the postmenopausal group, but not in all patients or in the premenopausal group (Table 4).
Multivariate analysis of breast cancer risk based on BMI quartiles was performed using parity, breastfeeding experience and age as adjustment factors. As shown in Table 5, there was a significant correlation between breast cancer risk and mammographic density in the two higher quartiles (BMI 22.3–24.5 and > 24.5 kg/m2), but not in the two lower quartiles (BMI < 20.3 and 20.3–22.2 kg/m2).
Discussion
This study was performed to investigate the association between breast density on mammography and breast cancer risk, with inclusion of the influence of other risk factors on mammographic density. Breast density showed a strong association with breast cancer risk, and this association was stronger in postmenopausal women and in those with high BMI.
High BMI increases breast cancer risk, while increased body fat percentage decreases breast density. At first glance, these seem to be conflicting events regarding breast cancer risk. Our study revealed that high BMI and breast density have additive effects on breast cancer risk. Thus, breast cancer risk is extremely high in women with high BMI and high breast density. Therefore, it is particularly important to evaluate risk factors and breast density on mammography, and use effective interventions, in this high risk group. Ultrasonography and MRI are useful auxiliary modalities for screening of women with high breast density, and these methods contribute to the sensitivity and rate of cancer detection, but the specificity is low and the false positive rate may be high [12]. Mammography is the only screening modality related to decreased breast cancer mortality, and care is required regarding introduction of countermeasure-type breast cancer screening [9]. Thus, it may be ideal for cost-effectiveness to use ultrasonography and MRI as auxiliary modalities after identifying risk factors such as obesity and postmenopausal status.
Previous studies in European and American women have shown a strong association between high breast density and breast cancer risk [13,14,15]. Many case–control and cohort studies have been performed [8] since Wolfe et al. [16] initially reported the association in 1976. Three small case–control studies in Japanese subjects also all found that high breast density was a significant risk factor for breast cancer [5,6,7]. In 2014, Pettersson et al. [17] performed a meta-analysis of 13 case–control studies of high-density mammary glands and breast cancer risk, and found that breast density was a risk regardless of the menopausal status (before or after menopause). In contrast, in our study, a strong association was found only in postmenopausal women. In a study of the association of breast density and lifestyle in Japanese women, BMI was the only factor influencing breast density before menopause, and BMI and parity influenced breast density after menopause (age 50s and 60s) [11].
Parity is tending to decrease in Japan, and the number of women with high breast density after menopause may increase and elevate the postmenopausal breast cancer risk. Obesity as a risk factor for breast cancer has been widely discussed. In a study of this relationship in Japanese women, 8 cohort studies were pooled and analyzed, and breast cancer risk was found to increase in proportion to BMI, regardless of the menopausal status [18]. These results differ from those in World Cancer Research Fund (WCRF) /American Institute for Cancer Research (AICR) reports showing that obesity of premenopausal women decreases breast cancer risk [19], which might reflect differences between Japanese and western women.
In our analysis using BMI quartiles, an association between high breast density and breast cancer risk was found in the two higher quartiles (BMI 22.3–24.5 and > 24.5 kg/m2), and the OR for C4 (vs. C1) was 12.14 in the most obese quartile (BMI > 24.5 kg/m2). These results show that high breast density in women with severe obesity increases the risk of breast cancer. A similar tendency was found in a case–control study in Asian subjects reported by Wong et al. in 2011, in which breast cancer risk due to high breast density was also higher in the high BMI group [20]. Normally, breast density on mammography decreases as BMI increases because the adipose component in the breast increases with an increase in BMI. A high breast density despite a high BMI indicates that mammary gland tissue is well developed, which theoretically suggests a high breast cancer risk, and our data also showed this tendency. Generally, associations of breast cancer with age at menarche, age at first birth, and family history of breast cancer have been pointed out, but these associations were not found in the current study.
Several limitations of this study may have an influenced the above results. Examinees of breast cancer screening were selected as the control group, but many of them may have been aware of breast cancer risk because of the presence of a relative who had developed breast cancer. Moreover, many of the controls were examined in a workplace health check-up; i.e., many women in employment were included and this status may have been a cause of the absence of a significant association of breast cancer risk with age at first birth and familial history. In addition, breast density was qualitatively evaluated by experts in this study, but software that automatically measures breast density based on digitalized mammography data and conditions has recently become available and may provide more accurate results.
In conclusion, in this case–control study, breast density on mammography was found to be a risk factor for breast cancer after adjustment for other breast cancer risk factors, and this association was stronger in postmenopausal women and in those with higher BMI. However, high breast density also reduces the sensitivity of mammography, and screening using other modalities, such as US and MRI, may be more appropriate for postmenopausal obese women with high breast density.
References
Smith RA, Duffy SW, Gabe R, Tabar L, Yen AM, Chen TH. The randomized trials of breast cancer screening: what have we learned? Radiol Clin North Am. 2004;42:793–806.
American College of Radiology (ACR). ACR BI-RADS®-Mammography, 4th edn. In: ACR breast imaging reporting and data system, breast imaging atlas. Reston, VA: American College of Ragiology; 2013. pp 181–9
Carney PA, Miglioretti DL, Yankaskas BC, Kerlikowske K, Rosenberg R, Rutter CM, et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138:168–75.
McCormack VA, dos Santos SI. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev. 2006;15:1159–69.
Kotsuma Y, Tamaki Y, Nishimura T, Tsubai M, Ueda S, Shimazu K, et al. Quantitative assessment of mammographic density and breast cancer risk for Japanese women. Breast. 2008;17:27–35.
Nagao Y, Kawaguchi Y, Sugiyama Y, Saji S, Kashiki Y. Relationship between mammographic density and the risk of breast cancer in Japanese women: a case-control study. Breast Cancer. 2003;10:228–33.
Nagata C, Matsubara T, Fujita H, Nagao Y, Shibuya C, Kashiki Y, et al. Mammographic density and the risk of breast cancer in Japanese women. Br J Cancer. 2005;92:2102–6.
Huo CW, Chew GL, Britt KL, Ingman WV, Henderson MA, Hopper JL, et al. Mammographic density-a review on the current understanding of its association with breast cancer. Breast Cancer Res Treat. 2014;144:479–502.
Taira N, Arai M, Ikeda M, Iwasaki M, Okamura H, Takamatsu K, et al. The Japanese Breast Cancer Society clinical practice guidelines for epidemiology and prevention of breast cancer, 2015 edition. Breast Cancer. 2016;23:343–56.
Sala E, Warren R, McCann J, Duffy S, Luben R, Day N. High-risk mammographic parenchymal patterns and anthropometric measures: a case-control study. Br J Cancer. 1999;81:1257–61.
Ishihara S, Taira N, Kawasaki K, Ishibe Y, Mizoo T, Nishiyama K, et al. Association between mammographic breast density and lifestyle in Japanese women. Acta Med Okayama. 2013;67:145–51.
Uematsu T. The need for supplemental breast cancer screening modalities: a perspective of population-based breast cancer screening programs in Japan. Breast Cancer. 2017;24:26–31.
Boyd NF, Byng JW, Jong RA, Fishell EK, Little LE, Miller AB, et al. Quantitative classification of mammographic densities and breast cancer risk: results from the Canadian National Breast Screening Study. J Natl Cancer Inst. 1995;87:670–5.
Razzaghi H, Troester MA, Gierach GL, Olshan AF, Yankaskas BC, Millikan RC. Mammographic density and breast cancer risk in White and African American women. Breast Cancer Res Treat. 2012;135:571–80.
Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ. Mammographic densities and breast cancer risk. Cancer Epidemiol Biomark Prev. 1998;7:1133–44.
Wolfe JN, Saftlas AF, Salane M. Mammographic parenchymal patterns and quantitative evaluation of mammographic densities: a case-control study. AJR Am J Roentgenol. 1987;148:1087–92.
Pettersson A, Graff RE, Ursin G, Santos Silva ID, McCormack V, Baglietto L, et al. Mammographic density phenotypes and risk of breast cancer: a meta-analysis. J Natl Cancer Inst. 2014;106:78.
Wada K, Nagata C, Tamakoshi A, Matsuo K, Oze I, Wakai K, et al. Body mass index and breast cancer risk in Japan: a pooled analysis of eight population-based cohort studies. Ann Oncol. 2014;25:519–24.
WCRFAIfC. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington DC: AICR; 2007.
Wong CS, Lim GH, Gao F, Jakes RW, Offman J, Chia KS, et al. Mammographic density and its interaction with other breast cancer risk factors in an Asian population. Br J Cancer. 2011;104:871–4.
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research, Scientific Research (C) from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain studies on animals.
Informed consent
All subjects and controls gave written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nishiyama, K., Taira, N., Mizoo, T. et al. Influence of breast density on breast cancer risk: a case control study in Japanese women. Breast Cancer 27, 277–283 (2020). https://doi.org/10.1007/s12282-019-01018-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-019-01018-6