Abstract
Purpose
Mammographic breast density (MBD) has been consistently associated with breast cancer (BC) risk, and at the same time it is modulated by established BC risk factors related to reproductive and hormonal history and to lifestyle. We aimed to evaluate the association between the clinical breast imaging reporting and data system (BI-RADS), a qualitative MBD classification used in clinical setting, and BC risk through a case–control nested in the EPIC Florence cohort where baseline information on reproductive history, lifestyle and anthropometry were collected.
Methods
The study includes 136 newly diagnosed BC cases and 635 controls from the 10,083 healthy women enroled in the cohort between 1993 and 1998 and followed for 6 years on average. MBD was assessed on a negative mammogram performed at least one year before diagnosis in cases and on a mammogram performed in the same period for controls matched for age, enrolment date and menopausal status. Multivariate analyses adjusted for education, body mass index, parity, number of children, breastfeeding, BC family history, history of breast biopsies and Hormone Replacement Therapy use were performed.
Results
An increase in BC risk across BI-RADS categories emerged with adjusted odds ratios (OR) 1.79 (95% CI 1.06–3.01), OR 2.09 (95% CI 1.17–3.74) and OR 2.67 (95% CI 1.08–6.62) for categories 2, 3 and 4 in comparison with the reference category (p for trend = 0.008).
Conclusions
We confirm in this Mediterranean population the association of increasing MBD, classified according to BI-RADS with BC risk also taking into account other well-known risk factors for this neoplasm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The extent of mammographically detected fibroglandular breast tissue, known as mammographic breast density (MBD) has emerged in the last few decades as one of the strongest risk factors for breast cancer (BC) and this association seems to persist after adjustment for other factors related to BC risk [1]. High MBD has been consistently associated with increased BC in studies using different methods of MBD evaluation ranging from subjective MBD evaluation of radiologists aimed to classify subjects in broad categories to fully automated methods allowing to obtain quantitative measures of breast density and in studies based both on films and digital mammograms [2, 3].
Among the qualitative systems of MBD classification based on the radiologist’s visual evaluation, the breast imaging reporting and data system (BI-RADS) is the most widely used in clinical settings and it has been reported to be able to classify women at different BC risks [2, 4, 5].
MBD is influenced by many factors that in turns modulate BC risk. Most of these factors including reproductive variables, hormonal aspects and possibly diet and physical exercise modulate in the same direction MBD and BC risk, however, MBD decreases with age and more strongly with increasing BMI. Therefore the availability of accurate information on the above-mentioned variables is mandatory in the evaluation of the relationship between MBD and BC risk [6].
Moreover, the interplay between MBD and other strong risk factors for BC such as history of breast biopsies has been investigated and these aspects have been included in models for the prediction of absolute risk of BC development [7]. We aimed to investigate the association between increased MBD as assessed according to BI-RADS classification and BC risk through a case–control study nested in a cohort of Mediterranean women, taking into account several factors known to influence MBD and in turns to modulate BC risk.
Materials and methods
Study cohort
The European Prospective Investigation into Cancer and nutrition (EPIC) Florence cohort has been set up as a part of the EPIC Europe prospective study and enroled (between 1993 and 1998) 10,083 clinically healthy women aged 35–64 years residing in the Florence area (Tuscany, Central Italy). All study participants signed an informed consent and gave permission to use the data collected during the study. The study was approved by the local Ethics Committee.
At enrolment, weight, height, waist and hip circumferences were measured by trained nurses according to an international standard protocol. Data on frequency of consumption of over 160 foods and drinks and usual portion size were obtained through a validated self-administered Food Frequency Questionnaire specifically developed to capture the Italian dietary habits. A standardized lifestyle questionnaire collected detailed information on reproductive history, smoking and alcohol drinking history, exposure to environmental tobacco, medical history including history of breast biopsies, educational level and other socio-economic and lifestyle variables including physical activity. Information on drug use including use of hormone replacement therapy (HRT), occupation and family history of cancer was also collected [8].
Standardized follow-up procedures have been periodically implemented for the identification of cancer cases diagnosed after enrolment. The ascertainment of vital status was carried out through the linkage with the local town offices and the local Mortality Registry, thereby identifying the deceased subjects and the date and cause of death. The identification of BC cases, was obtained through linkages with hospital discharge system and other sources such as Pathology Department registries [8].
We also linked periodically the EPIC Florence female cohort with the mammographic archives of the population-based mammographic screening in the Florence area of which the Cancer Research and Prevention Institute—ISPO (formerly CSPO)—is in charge and with the archive of the mammograms performed in a clinical setting at our Institution, in order to update the mammographic examination history of the EPIC female participants [9].
Design of the nested case–control study
Cases
All newly diagnosed invasive breast cancer cases (code C50 according to ICD-O-2 classification) after the date of recruitment until 31 December 2001 for which it was possible to identify and retrieve one negative mammogram at least 1 year before the diagnosis.
Controls
For each case, a maximum of six controls, individually matched by age (±12 months), date of enrolment (±12 months), menopausal status and date of mammographic examination (±6 months) were randomly selected among those still at risk of BC at the time of diagnosis of each case.
Mammographic breast density assessment
The assessment of MBD was performed by an experienced radiologist (D.A.), blind to case–control status, according to BI-RADS classification (4th edition) in the following four categories: 1—the breast is entirely fatty (<25% fibroglandular tissue); 2—there are scattered fibroglandular densities (25–50%); 3—the breast tissue is heterogeneously dense which may obscure small masses (51–75%) and 4—the breasts are extremely dense, which lowers the sensitivity of mammography (>75%) [10].
We retrieved most of the identified mammographic examinations (screen film mammograms) directly from the ISPO archives, but we also invited study participants to send us the films if these were kept at home. The oblique medio-lateral view of both breasts was used for mammographic assessment. Only this view was utilized to assess the MBD even in the group of subjects with two films because in the mammographic population screening programme in Florence, the two views (oblique medio- lateral and cranio-caudal) were performed at the subsequent screening test after the first screening mammogram only in women with dense breast until 2000. In order to avoid reader being aware of the previous classification, for all subjects only the oblique medio-lateral view was used. We have already evaluated the effect of using only the oblique medio-lateral view to assess parenchymal patterns versus both views in a subset of 50 MEs utilized in a previous study and we found a very high concordance [9].
Statistical analysis
Distribution of the main baseline characteristics and of BI-RADS categories was reported separately for BC cases and controls. Tests of heterogeneity between categories were performed.
The association of MBD, classified according to BI-RADS categories, with BC risk was evaluated by conditional logistic regression, which takes into account the matching of controls to cases. Crude and adjusted odds ratios (OR) and 95% confidence intervals (CI) were estimated.
Adjustments were performed by variables that were reported to be associated with both MBD and BC risk in previous studies [9, 11]: education (primary/secondary school, high school/university), BMI (continuous), number of children (0, 1–2, ≥3), breast feeding(≤6 months, >6 months), first-degree BC family history (yes/no), previous breast biopsy(yes/no) and current HRT use (yes/no). To calculate the p value for trend, categories of BI-RADS were entered as an ordinal term in the model.
The analyses were also carried out separately according to menopausal status.
Interaction of MBD with previous history of breast biopsies, BMI, first-degree BC family history and HRT use were also investigated.
All analyses were performed using the SAS statistical software (SAS/STAT version 9.2); a p value <0.05 was considered statistically significant.
Results
For 140 (78.2%) out of the 179 BC cases occurred in the follow-up period, we were able to identify and retrieve a negative mammographic examination suitable for the study. The remaining 39 BC cases were younger (45.2 vs. 54.0 years p < 0.0001), more educated (66.7% reported to have obtained at least a high school degree vs. 55.0% p = 0.002), with a lower proportion of previous breast biopsies (2.6 vs. 17.9% p = 0.001) and a lower proportion of reported BC first-degree family history (5.1 vs. 14.3% p = 0.07). The assessment of MBD was not possible for the mammograms of four cases due to technical problems, thus leaving 136 cases for the analysis. We identified 635 matched controls for which the mammograms were available for the MBD assessment. Most cases (n 76) had five matched controls while one case had only one matched control.
The mammograms used for the definition of the breast density were performed on average 2.7 years (SD 1.96) before BC diagnosis.
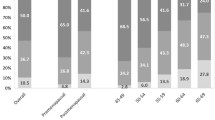
In Table 1, the distribution of BI-RADS categories and of selected characteristics is reported separately for cases and controls. Overall, 28.7% (n 39) of BC cases and 43.0% (n 273) of controls were categorized to have a “entirely fatty breast” (category 1) while the proportion of BC cases and controls categorized in the category 4 “extremely dense breast” was 8.8% (n 12) and 6.5% (n 41), respectively (overall p = 0.02). Cases and controls also differed with respect to the proportion of previous breast biopsies and first-degree BC family history as reported at enrolment (p = 0.02).
Both in crude and adjusted analyses, the positive significant association between BI-RADS categories and BC risk emerged, ranging in multivariate analyses from a 79% increase in category 2 to a more than twofold increase in categories 3 and 4 in comparison to the lowest category (Table 2). The adjusted OR for a single category increase in the BI-RADS scale was 1.41 (95% CI 1.09–1.81) with a significant trend (p = 0.008).
In the multivariate models, we also observed a significant positive association of breast biopsy history with BC risk (OR 1.90; 95% CI 1.08–3.35).
The results did not change in analyses carried out separately by menopausal status (data not shown). No effect modification of the association between MBD and BC risk by BMI, previously reported breast biopsies, first-degree BC family history or HRT use emerged.
Discussion
In this case–control study nested in the EPIC Florence cohort, we confirmed the positive association between high mammographic breast density, classified according to BI-RADS (4th edition) and breast cancer risk.
In comparison with women in the lowest category of BI-RADS (1: <25% fibroglandular tissue), the risk to develop BC increased across categories with a significant trend up to a 2.67-fold increase in women in the most dense breast BI-RADS category (4: >75% of fibroglandular tissue). These results were obtained taking into account a series of variables known to affect both MBD and BC risk including BMI. No differences emerged in the evaluation of the association between high MBD BI-RADS categories and BC risk according to menopausal status. No interactions emerged by breast biopsy history, first-degree family history for BC or HRT use.
A series of studies have evaluated the association between BI-RADS and BC risk showing consistently an increase in risk over categories of increasing breast density although different designs that have been adopted could at least partially explain some differences in estimates. In a nested case–control study carried out in the cohort set up in the population-based screening programme in Denmark, an approximately two- and fourfold age-adjusted increase in BC risk emerged among women classified in the 3 and 4 BI-RADS categories, respectively [12]. The BI-RADS classification in this study was based on a negative mammogram performed on average 26 months before diagnosis [12]. In a population-based case–control study including both Afro-American and Caucasian women in which MBD assessment using reported BI-RADS was performed on mammograms performed between 5 years before and 1 year after diagnosis, an increase in BC risk emerged for all women with extremely dense breast having a threefold increase in BC risk in comparison with women in the lowest BI-RADS category [13]. The association was more evident in Caucasian women, and a significant effect modification emerged by HRT use [13]. The proportion of current HRT users in our Mediterranean population was low as expected and no effect modification emerged in our analyses.
The association between BI-RADS categories of MBD and BC risk has been also evaluated in a case–control study in which MBD assessment was based on full-field digital mammograms and performed with different tools and also using BI-RADS classification extracted by mammography reports. Women in the highest BI-RADS category had a twofold increase in BC risk in comparison with women in the lowest category in models adjusted for BMI, parity, and menopausal status and the BI-RADS was as accurate as computer-assisted methods in discriminating cases and controls [14]. Some studies have evaluated the association of BI-RADS categories with BC risk by BC subtypes and no specific differences emerged [15, 16].
We have also reported the independent contribution of MBD and previous self-reported breast biopsies to BC risk. Having a history of breast biopsies per se increases the BC risk and this information has been incorporated in predictive models for the assessment of BC risk [17,18,19]. We can postulate a higher occurrence of breast biopsies in women with higher MBD. Moreover, some studies showed the independent effect of previous histologically confirmed benign breast disease and high MBD in increasing BC risk [20]. In our study, we confirm that high MBD and a previous history of breast biopsies are both associated with increased BC risk thus supporting the independent role of these two characteristic in identifying high-risk women.
In spite of its relatively small size, this study has a number of strengths, especially based on the case–control design nested in a cohort in which standardized and well-established procedures for the identification of cases have been applied. BMI measures were obtained through a standardized protocol, and series of other BC risk factors to adjust for were collected. The evaluation of MBD was performed by a single experienced radiologist and based on mammograms obtained in the same setting. Moreover, all mammographic examination included in the study were performed with the same imaging technology. Limitations of the study are mainly related to the method used to assess MBD that allow only a broad categorization of MBD thus possibly leading to a misclassification, and consequently to an attenuation of the risk estimates.
In conclusion, we confirm, in a Mediterranean population, the positive association between higher MBD assessed by BI-RADS, a method of qualitative assessment of MBD widely used in clinical settings, and increased BC risk also taking into account the aspects related to personal characteristics, reproductive variable and anthropometry well known to influence both MBD and BC risk. These results support the possibility to use this classification as a tool to identify women with differential BC risk to be targeted by specific interventions of risk reduction or by different diagnostic/screening protocols.
Abbreviations
- BC:
-
Breast cancer
- BI-RADS:
-
Breast imaging reporting and data system
- BMI:
-
Body mass index
- EPIC:
-
European prospective investigation into cancer and nutrition
- HRT:
-
Hormone replacement therapy
- MBD:
-
Mammographic breast density
- OR:
-
Odds ratio
References
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, Yaffe MJ (2007) Mammographic density and the risk and detection of breast cancer. N Engl J Med 356:227–236
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomark Prev 15:1159–1169
Eng A, Gallant Z, Sherpherd J, McCormack V, Li J, Dowsett M, Vinnicombe S, Allen S, dos Santos Silva I (2014) Digital mammographic density and breast cancer risk: a case control study of six alternative density assessment methods. Breast Cancer Res 16:349
Olson JE, Sellers TA, Scott CG, Schueler BA, Brandt KR, Serie DJ, Jensen MR, Wu FF, Morton MJ, Heine JJ, Couch FJ, Pankratz VS, Vachon CM (2012) The influence of mammogram acquisition on the mammographic density and breast cancer association in the Mayo Mammography Health Study cohort. Breast Cancer Res 14:R147
Engmann NJ, Golmakani MK, Miglioretti DL, Sprague BL, Kerlikowske K, Breast Cancer Surveillance Consortium (2017) Population-attributable risk proportion of clinical risk factors for breast cancer. JAMA Oncol. doi:10.1001/jamaoncol.2016.6326
Boyd NF, Martin LJ, Sun L, Guo H, Chiarelli A, Hislop G, Yaffe M, Minkin S (2006) Body size, mammographic density, and breast cancer risk. Cancer Epidemiol Biomark Prev 15:2086–2092
Tice JA, Miglioretti DL, Li CS, Vachon CM, Gard CC, Kerlikowske K (2015) Breast density and benign breast disease: risk assessment to identify women at high risk of breast cancer. J Clin Oncol 33:3137–3143
Palli D, Berrino F, Vineis P, Tumino R, Panico S, Saieva C, Masala G, Salvini S, Ceroti M, Decarli A, Krogh V, on behalf of EPIC-Italy (2003) A molecular epidemiology project on diet and cancer: the EPIC-Italy prospective study. Design and baseline characteristics of participants. Tumori 89:586–593
Masala G, Ambrogetti D, Assedi M, Giorgi D, Rosselli Del Turco M, Palli D (2006) Dietary and life-style determinants of mammographic breast density. A longitudinal study in a Mediterranean population. Int J Cancer 118:1782–1789
American College of Radiology (2003) Breast imaging reporting and data system (BI-RADS®), 4th edn. American College of Radiology, Reston
Assi V, Warwick J, Cuzick J, Duffy SW (2011) Clinical and epidemiological issues in mammographic density. Nat Rev Clin Oncol 9:33–40
Winkel RR, von Euler-Chelpin M, Nielsen M, Petersen K, Lillholm M, Nielsen MB, Lynge E, Uldall WY, Vejborg I (2016) Mammographic density and structural features can individually and jointly contribute to breast cancer risk assessment in mammography screening: a case-control study. BMC Cancer 16:414
Razzaghi H, Troester MA, Gierach GL, Olshan AF, Yankaskas BC, Millikan RC (2012) Mammographic density and breast cancer risk in White and African American Women. Breast Cancer Res Treat 135:571–580
Jeffers AM, Sieh W, Lipson JA, Rothstein JH, McGuire V, Whittemore AS, Rubin DL (2017) Breast cancer risk and mammographic density assessed with semiautomated and fully automated methods and BI-RADS. Radiology 282:348–355
Ziv E, Tice J, Smith-Bindman R, Shepherd J, Cummings S, Kerlikowske K (2004) Mammographic density and estrogen receptor status of breast cancer. Cancer Epidemiol Biomark Prev 13:2090–2095
Phipps AI, Buist DS, Malone KE, Barlow WE, Porter PL, Kerlikowske K, O’Meara ES, Li CI (2012) Breast density, body mass index, and risk of tumor marker-defined subtypes of breast cancer. Ann Epidemiol 22:340–348
Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, Mulvihill JJ (1989) Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 81:1879–1886
Decarli A, Calza S, Masala G, Specchia C, Palli D, Gail MH (2006) Gail model for prediction of absolute risk of invasive breast cancer: independent evaluation in the Florence-European Prospective Investigation Into Cancer and Nutrition cohort. J Natl Cancer Inst 98:1686–1693
Tice JA, Cummings SR, Smith-Bindman R, Ichikawa L, Barlow WE, Kerlikowske K (2008) Using clinical factors and mammographic breast density to estimate breast cancer risk: development and validation of a new predictive model. Ann Intern Med 148:337–347
Tice JA (2013) o’Meara ES, Weaver DL, Vachon C, Ballard-Barbash R, Kerilowske K (2013) Benign breast disease, mammographic breast density, and the risk of breast cancer. J Natl Cancer Inst 105:1043–1049
Acknowledgements
The authors wish to thank all EPIC Florence participants. The study has been supported by a grant from Associazione Italiana per la Ricerca sul Cancro (AIRC, Milan, Italy).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study has been approved by the local Florence Ethical Committee (2001/96) and have been performed in accordance with the ethical standard as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Masala, G., Ambrogetti, D., Assedi, M. et al. Mammographic breast density and breast cancer risk in a Mediterranean population: a nested case–control study in the EPIC Florence cohort. Breast Cancer Res Treat 164, 467–473 (2017). https://doi.org/10.1007/s10549-017-4274-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4274-9