Abstract
Purposes
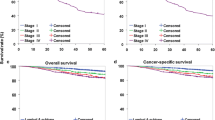
We conducted a study to analyze the clinicopathological characteristics of breast cancer in Japan registered to the Japanese Breast Cancer Registry of the Japanese Breast Cancer Society (JBCS). Trends in the management of breast cancer patients in Japan were also analyzed.
Patients and methods
More than 250,000 breast cancer patients were registered to the JBCS registry between 2004 and 2011. Demographic and clinicopathological factors in newly diagnosed primary breast cancer patients were registered to the JBCS through the Web-based system from affiliated institutes nationwide.
Results
Two distinct peaks were observed, in patients in their late 40s and early 60s, in the population-adjusted age distribution of breast cancer patients. An increased rate of screen-detected breast cancer may contribute to an earlier detection of breast cancer and increased rate of non-invasive ductal carcinoma. The positive rate of either ER or PgR appears to have increased in recent years. The annual rates of patients treated with breast-conserving surgery increased until 2006, but these increases stopped in 2007 and thereafter plateaued at approximately 60 %. The annual rates of patients treated with sentinel lymph node dissection alone have steadily increased. The annual rates of patients treated with preoperative trastuzumab plus chemotherapy have also increased, as well as those treated with postoperative aromatase inhibitors. The annual rates of patients treated with postoperative anthracycline-containing regimens have decreased, whereas those treated with postoperative taxane-containing regimens have increased. The postoperative use of trastuzumab has markedly increased since 2007.
Conclusion
Although this study was based on the registry database, several unique clinicopathological characteristics of breast cancer in Japan have been unveiled. Our results suggest that recent trends in the management of breast cancer patients in Japan were strongly followed by clinical evidence that originated from a number of clinical trials worldwide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is one of the leading causes of cancer-related death in Japan and western countries. It has also been the most prevalent cancer in women in the last 20 years in Japan. The morbidity of breast cancer has been increasing for over 40 years in Japan. The main reason for this increase is considered to be the westernization of Japanese women in terms of their lifestyles. The lifetime risk for breast cancer in Japanese women was previously reported to be one in twelve in 2014 [1]. The prevention and early detection of breast cancer as well as the medical and social management of patients with breast cancer have been important medical issues in Japan. The Japanese Breast Cancer Society (JBCS) was founded in 1992 and has been a leading scientific society dealing with these issues.
In order to obtain a deeper insight into the clinicopathological characteristics of breast cancer and recent trends in the management of breast cancer patients in Japan, the JBCS started a Web-based registration system in 2004 [2]. The number of registered patients has steadily increased every year. A total of 48,133 patients were registered in 2010. According to the latest statistical analysis by the Center for Cancer Control and Information Services, National Cancer Center, Japan, a total of 68,107 breast cancer patients were estimated to be newly diagnosed in 2010 [1]. Approximately 70 % of newly diagnosed breast cancer patients in Japan were registered to the JBCS registry in 2010.
Since ethnic differences and significant differences in the morbidity of breast cancer have been reported between Japanese women in Japan and Caucasian women in western countries, significant differences are considered to exist in breast cancer characteristics; however, these differences have not yet been elucidated in detail. A large number of Japanese breast cancer patients (more than 250,000) were registered to the JBCS registry between 2004 and 2011; therefore, we conducted this study in order to analyze the clinicopathological characteristics of breast cancer in Japan registered to the JBCS registry. Recent trends in the management of breast cancer patients in Japan were also examined because a number of new local and systemic therapies have been introduced into clinics in the last decade.
Patients and methods
Data collection
More than 50 items on the demographic and clinicopathological factors of newly diagnosed primary breast cancer patients were voluntarily registered to the Japanese Breast Cancer Registry of the JBCS through the Web-based system from affiliated institutes. The TNM classification was registered according to the Unio Internationalis Contra Cancrum (UICC) staging 6th edition [3]. Histological classification was registered according to the WHO classification [4].
This registry system has been conducted by the Registration Committee of the JBCS and supported by the Public Health Research Foundation (Tokyo, Japan). Annual reports on this registry have been published in Japanese and publicized through the JBCS homepage to active members of the JBCS (http://www.jbcs.gr.jp/Member/tourokusyukei.html).
Statistical analysis
Right and left breast tumors in patients with synchronous or asynchronous bilateral breast cancer were respectively treated as two different breast tumors in this registration system. The age-adjusted prevalence of primary breast cancer per 100,000 women was calculated based on the population database in each year provided from the Ministry of Health, Labour and Welfare, Japan. Statistical analyses were performed using SAS software (SAS Institute Japan Ltd., Tokyo, Japan) and Microsoft Excel software (Microsoft Japan, Tokyo, Japan).
Results and discussion
Breast cancer patients registered to the Breast Cancer Registry of the JBCS between 2004 and 2011
The annual number of breast cancer patients registered and that of affiliated institutes markedly increased between 2004 and 2011 (Supplementary Figure 1A and 1B). In the first year (2004) of the Web system, a total of 14,805 breast cancer patients were registered from 387 affiliated institutes nationwide in Japan. In the last year (2011), a total of 48,481 patients were registered from 845 affiliated institutes nationwide in Japan.
Gender
The annual rate of male breast cancer patients was between 0.38 and 0.49 % of all breast cancer patients registered in these eight years. According to reviews on male breast cancer [5], breast cancer is a rare disease in men, accounting for nearly 1 % of all breast cancer cases in western countries. The rate of male breast cancer patients appears to be lower than in western countries.
Only female breast cancer patients were analyzed in the following data analyses.
Bilateral breast cancer
The annual rates of synchronous bilateral breast cancer gradually increased from 3.5 % in 2004 to 4.8 % in 2011, while those of asynchronous bilateral breast cancer were 2.8–3.2 % in these years. An increase in the sensitivity of breast imaging modalities such as magnetic resonance imaging to detect early breast cancer may have led to increases in the rate of synchronous bilateral breast cancer.
According to a large cohort study (n = 6550) in Sweden, the rate of synchronous bilateral breast cancer was 1.5 % and that of asynchronous bilateral breast cancer was 3.8 % [6]. Another cohort study (n = 1465) reported that the rate of synchronous bilateral breast cancer was 3.0 % and that of asynchronous bilateral breast cancer was 7.1 % [7]. The rate of synchronous bilateral breast cancer appears to be slightly higher in Japan than in western countries.
Family history
The annual rates of breast cancer patients with a family history of breast cancer gradually increased from 8.0 % in 2004 to 9.7 % in 2011. A positive family history in this registry included not only breast cancer cases in first-degree relatives, but also those in second- or third-degree relatives. According to the Utah Population Database survey (n = 3864), the rate of patients with a family history of first-degree relatives was 5.7 % [8]. Difficulties have been associated with comparing the rates of family history between breast cancer patients in Japan and those in western countries.
Menopausal status
The annual rates of premenopausal and postmenopausal breast cancer patients were 33.2–35.7 % and 61.3–63.8 % in these 8 years, respectively, while those with an unknown menopausal status including post-hysterectomy patients were 2.6–3.5 % in these years. Menopause was not strictly defined in this registry. According to data from the surveillance, epidemiology, end results (SEER) Program between 2007 and 2011 in the United States, the rates of newly diagnosed breast cancer patients less and more than or equal to 55 years old were 33.1 and 66.9 %, respectively [9]. The rate of premenopausal breast cancer patients appears to be slightly higher in Japan than in western countries.
Age
Two distinct peaks were observed, in patients in their late 40s and early 60s, in the population-adjusted age distribution of breast cancer patients in Japan (Fig. 1).
According to the SEER database between 2007 and 2011, there was only one peak, at the early 60s, in the age distribution of newly diagnosed breast cancer patients in the USA [9]. In contrast, there was one peak, in patients in their 40s, in this age distribution in South Korea [10]. These findings indicate that there are two mixed peaks in Japan: in patients in their 40s, similar to East Asian women, and those in their early 60s, similar to western women.
Body mass index (BMI)
The annual rates of obese breast cancer patients (BMI >25) were 22.4–23.4 % between 2004 and 2011. The distribution of BMI in breast cancer patients did not change between 2004 and 2011.
Based on data from one of the largest clinical trials in western countries, the Arimidex, Tamoxifen Alone, or in Combination study [11], BMI over 25 was observed in 56.8 % of the enrolled postmenopausal patients. In addition, based on data from the large breast cancer database of the University of Texas MD Anderson Cancer Center (n = 6342), BMI over 25 was observed in 60 % of the registered premenopausal and postmenopausal patients [12]. The rate of obese breast cancer patients appears to be markedly lower in Japan than in western countries.
Detection by breast cancer screening
The annual rates of breast cancer patients without any symptoms and detected by breast cancer screening steadily increased from 14.9 % in 2004 to 28.6 % in 2011 (Fig. 2). These marked changes have been attributed to an increase in the annual rates of Japanese women receiving breast cancer screening, in particular, mammographic screening. According to statistical data provided from the Ministry of Health, Labour and Welfare in Japan, the annual rates of women receiving breast cancer screening in Japan increased from 24.7 % in 2007 to 30.6 % in 2011 [13]. These findings indicate that the earlier detection of primary breast cancer may be mainly caused by an increase in the rate of women receiving breast cancer screening in Japan.
Clinical tumor size
The annual rates of patients with tumors larger than 2.0 cm in size steadily decreased from 51.2 % in 2004 to 36.3 % in 2011 (Fig. 3). These marked changes also appear to have been due to an increase in the annual rates of Japanese women receiving breast cancer screening.
Skin changes, chest wall fixation, and inflammatory breast cancer
The annual rates of patients with tumors with skin changes were 3.6–4.4 % in these eight years, while those of patients with breast tumors fixed to chest wall were 0.5–1.2 %. The annual rates of patients with inflammatory breast cancer decreased from 1.2 % in 2004 to 0.3 % in 2011.
TNM stage
The annual rates of patients with Tis and T1 breast tumors increased from 7.4 and 37.3 % in 2004 to 11.2 and 45.3 % in 2011, respectively, whereas those with T2, T3, and T4 breast tumors decreased from 38.4, 5.0, and 5.9 % in 2004 to 27.5, 2.8, and 3.9 % in 2011, respectively (Supplementary Figure 2).
The annual rates of patients with N0 increased from 77.0 % in 2004 to 82.3 % in 2011. In addition, the annual rates of patients with M0 increased from 95.6 % in 2004 to 97.0 % in 2011.
The annual rates of patients with stage 0 and I breast cancer increased from 7.0 and 33.1 % in 2004 to 10.8 and 41.5 % in 2011, respectively (Supplementary Figure 3).
Pathological findings
-
1.
Infiltrating tumor size
The annual rates of patients with breast tumors equal to or less than 2 cm in pathologically infiltrating tumor size increased from 53.6 % in 2004 to 63.0 % in 2011, whereas those with breast tumors 2.1–5.0 cm and over 5.0 cm in pathologically infiltrating tumor size decreased from 36.3 and 6.9 % in 2004 to 26.6 and 4.9 % in 2011, respectively (Supplementary Figure 4).
-
2.
Nodal status
The annual rates of patients with no lymph node metastasis increased from 58.7 % in 2004 to 68.7 % in 2011, while those with 1-3, 4-9, and more than or equal to 10 metastatic lymph nodes decreased from 20.8, 7.2, and 4.7 % in 2004 to 16.9, 4.2, and 2.2 % in 2011, respectively (Fig. 4).
According to analyses based on the SEER database (2001–2008) and a cohort study in Belgium (2000–2009), the rates of node-negative breast cancer patients were 65.4 and 62.0 %, respectively [14, 15]. No significant difference was observed in the rate of node-negative breast cancer patients between patients in Japan and those in western countries.
-
3.
Histological classification
The annual rates of patients with non-invasive ductal carcinoma increased from 8.2 % in 2004 to 14.3 % in 2011. These results indicated that this increase was mainly due to an increase in the rate of breast cancer patients detected by mammographic screening. According to a large cohort study in the USA [16], the rate of non-invasive ductal carcinoma has markedly increased for the last 20 years in parallel with increases in the rate of breast cancer patients detected by mammographic screening, and was approximately 20 % in 2003.
In contrast, the annual rates of patients with invasive ductal carcinoma decreased from 79.8 % in 2004 to 74.0 % in 2011, while those with non-invasive lobular carcinoma, special types, and others did not significantly change in those years.
The annual rates of patients with invasive lobular carcinoma slightly increased from 3.1 % in 2004 to 3.7 % in 2011. Previous studies reported that the rate of invasive lobular carcinoma had increased and was 5–15 % in western countries [17, 18].
-
4.
Estrogen receptor (ER) and progesterone receptor (PgR) status
The annual rates of patients with ER-positive breast tumors increased from 71.8 % in 2004 to 79.7 % in 2011, whereas those with ER-negative breast tumors decreased from 24.5 % in 2004 to 17.5 % in 2011, respectively.
It should be noted that not only the cutoff level of ER positivity, but also test procedures for ER immunostaining have not yet been standardized in Japan or other countries. Therefore, it is difficult to conclude the trend in the rate of ER positivity in Japan.
The annual rates of patients with PgR-positive breast tumors increased from 58.8 % in 2004 to 69.5 % in 2011, whereas those with PgR-negative breast tumors decreased from 37.2 % in 2004 to 27.7 % in 2011, respectively. Because of its similar background to ER positivity, it is difficult to conclude the trend in the rate of PgR positivity in Japan.
The annual rates of patients with ER-positive and PgR-positive breast tumors increased from 58.9 % in 2004 to 70.8 % in 2011, whereas those with ER-positive and PgR-negative, ER-negative and PgR-positive, and ER-negative and PgR-negative breast tumors have decreased from 15.5, 2.4, and 23.2 % in 2004 to 11.2, 0.7, and 17.2 % in 2011, respectively.
According to our previous cohort study, either the ER-positive rate or PgR-positive rate of breast tumors was higher in patients in their 40s than in those over 50 [19, 20]. To clarify this finding, we analyzed both ER-positive and PgR-positive rates stratified by age in breast cancer patients registered in 2011. As expected, the ER-positive rate was approximately 90 % in patients in their 40s and approximately 80 % in those over 50, and the PgR-positive rate was approximately 85 % in patients in their 40s and less than 70 % in those over 50 (Supplementary Figure 5).
-
5.
HER2 status
The annual rates of patients with HER2-positive and HER2-negative breast tumors were 12.3–15.5 and 67.4–77.7 %, respectively. No significant changes were observed between 2004 and 2011. The annual rates of patients with HER2-unknown breast tumors steadily decreased from 20.2 % in 2004 to 7.7 % in 2011.
According to an analysis of the California Cancer Registry database (2006–2008), HER2 positivity rates were 13 % for white women, 17 % for black women, 18 % for Hispanic women, and 20 % for Asian women, respectively [21]. Since not only the cutoff level of HER2 positivity, but also test procedures for HER2 immunostaining and HER2 gene amplification have not yet been standardized in Japan or other countries, it is difficult to compare HER2 positivity rates among different countries.
Local therapies
-
1.
Surgical procedures for breast tumors
The annual rates of patients treated with breast-conserving surgery increased from 50.1 % in 2004 to 58.6 % in 2011. However, these increases stopped in 2007 and thereafter plateaued at 59 %. The annual rates of patients treated with modified radical mastectomy steadily decreased from 42.5 % in 2004 to 26.9 % in 2011, while those with standard or extended radical mastectomy were 0.3–0.6 % and did not significantly change in those years. The annual rates of patients treated with simple mastectomy increased from 5.6 % in 2004 to 13.0 % in 2011, and this was attributed to an increased rate of patients receiving simultaneous breast reconstruction in recent years (Fig. 5).
Medical care systems and socio-economic backgrounds strongly influenced the choice of modalities of local therapy for breast cancer among different countries. The rate of breast-conserving surgery was previously reported to be 50–60 % in western countries and 10–30 % in China and India [22, 23].
-
2.
Surgical procedures for axillary lymph nodes
The annual rates of patients treated with sentinel lymph node biopsy alone steadily increased from 18.3 % in 2004 to 59.0 % in 2011, whereas those treated with axillary lymph node dissection steadily decreased from 69.6 % in 2004 to 31.7 % in 2011 (Fig. 6).
Sentinel lymph node biopsy was approved for practical use by the Ministry of Health, Labour and Welfare, Japan in 2010. This approval clearly increased the rate of sentinel lymph node biopsy alone in Japan, and the rate of 59 % in 2011 was almost equal to that in western countries [24].
-
3.
Postoperative radiotherapy
Stage IV breast cancer patients were excluded to simplify this analysis, and patients treated with two major breast surgical procedures, breast-conserving surgery and modified radical mastectomy, were selected as study subjects.
The annual rates of patients treated with breast-conserving surgery followed by postoperative radiotherapy steadily increased from 72.0 % in 2004 to 80.0 % in 2011, while those treated with modified radical mastectomy followed by postoperative radiotherapy also increased from 8.6 % in 2004 to 14.6 % in 2011 (Supplementary Figure 6).
According to an analysis on the SEER database for patients with invasive breast cancer in Detroit and Los Angeles (2005–2007), postoperative radiotherapy was performed if indicated in 80.0–95.4 % of patients treated with breast-conserving surgery and in 47.5–77.6 % of patients treated with mastectomy [25]. These findings suggest that postoperative radiotherapy was more frequently performed in the USA than in Japan.
Systemic therapies
-
1.
Preoperative systemic therapies
The annual rates of patients treated with preoperative systemic therapies increased from 9.6 % in 2004 to 14.2 % in 2008, but decreased from 14.0 % in 2009 to 9.3 % in 2011. Preoperative chemotherapies were more common than preoperative endocrine therapies. However, the annual rates of patients treated with preoperative endocrine therapies in all patients treated with preoperative systemic therapies slightly increased from 15.8 % in 2004 to 20.6 % in 2011 (Supplementary Figure 7).
Anthracycline- and taxane-containing regimens were frequently used as preoperative chemotherapies between 2004 and 2011. Approximately 70 % of patients treated with preoperative systemic therapies received both regimens. Aromatase inhibitors were the most frequently used as preoperative endocrine therapeutic agents. The annual rates of patients treated with preoperative trastuzumab plus chemotherapy increased from 5.8 % in 2004 to 20.5 % in 2011.
-
2.
Postoperative systemic therapies
The annual rates of patients treated with postoperative systemic therapies were 85.9–90.6 % between 2004 and 2011. No significant changes were observed in these rates during that time. Postoperative endocrine therapies were more common than postoperative chemotherapies. The annual rates of patients treated with postoperative chemotherapies in all patients treated with postoperative systemic therapies gradually decreased from 40.0 % in 2004 to 33.7 % in 2011 (Fig. 7).
Aromatase inhibitors and tamoxifen were the most commonly used as postoperative endocrine therapeutic agents. The annual rates of patients treated with postoperative aromatase inhibitors in all patients treated with postoperative systemic therapies increased from 39.5 % in 2004 to 49.2 % in 2011, whereas those treated with postoperative tamoxifen slightly decreased from 38.3 % in 2004 to 32.8 % in 2011.
Anthracycline- and taxane-containing regimens were commonly used as postoperative chemotherapies between 2004 and 2011. The annual rates of patients treated with postoperative anthracycline-containing regimens in all patients treated with postoperative systemic therapies gradually decreased from 35.7 % in 2004 to 20.6 % in 2011, whereas those treated with postoperative taxane-containing regimens steadily increased from 14.7 % in 2004 to 22.4 % in 2011 (Supplementary Figure 8).
The postoperative use of trastuzumab markedly increased since 2007 because its postoperative application was approved by the Ministry of Health, Labour and Welfare, Japan in 2007. The annual rates of patients treated with postoperative trastuzumab in all patients treated with postoperative systemic therapies were 0.1–2.5 % between 2004 and 2006, and significantly increased to 7.7–12.5 % between 2007 and 2011.
Conclusions
The results of the present study, which was based on the data of the Web-based registry for newly diagnosed breast cancer patients between 2004 and 2011 in Japan, revealed a number of interesting findings with regard to breast cancer characteristics and recent trends in the management of breast cancer patients in Japan as follows:
-
1.
Two distinct peaks were observed, in patients in their late 40s and early 60s, in the population-adjusted age distribution of breast cancer patients.
-
2.
The rate of obese breast cancer patients was markedly lower in Japan than in western countries.
-
3.
Although the morbidity of breast cancer continues to increase in Japan, the higher rate of screen-detected breast cancer may contribute to the earlier detection of breast cancer and an increased rate of non-invasive ductal carcinoma.
-
4.
Although there are some confounding factors influencing the positivity of ER or PgR in breast cancer, the positive rate of either ER or PgR appears to have increased in recent years.
-
5.
The annual rates of patients treated with breast-conserving surgery increased until 2006, but these increases stopped in 2007 and thereafter plateaued at approximately 60 %. The annual rates of patients treated with modified radical mastectomy steadily decreased between 2004 and 2011, while those treated with simple mastectomy increased in these years.
-
6.
The annual rates of patients treated with sentinel lymph node biopsy alone steadily increased between 2004 and 2011.
-
7.
The annual rates of patients treated with breast-conserving surgery followed by postoperative radiotherapy and with modified radical mastectomy followed by postoperative radiotherapy have increased in recent years.
-
8.
The annual rates of patients treated with preoperative endocrine therapies have increased in recent years.
-
9.
The annual rates of patients treated with preoperative trastuzumab plus chemotherapy have increased in recent years.
-
10.
The annual rates of patients treated with postoperative aromatase inhibitors have increased, whereas those treated with postoperative tamoxifen have decreased in recent years.
-
11.
The annual rates of patients treated with postoperative anthracycline-containing regimens have decreased, whereas those treated with postoperative taxane-containing regimens have increased in recent years.
-
12.
The postoperative use of trastuzumab has markedly increased since 2007.
Although this study was based on the registry database and several categories in the data registration, such as family history and the positivity of ER and PgR, were not strictly defined, several unique clinicopathological characteristics of breast cancer in Japan have been unveiled. In addition, our results suggested that recent trends in the management of breast cancer patients in Japan were strongly followed by clinical evidence that originated from a number of clinical trials worldwide.
References
Center for Cancer Control and Information Services, National Cancer Center, Japan. http://ganjoho.jp/public/index.html.
Tokuda Y. The Japanese Breast Cancer Society Breast Cancer Registry in the National Clinical Database: current status and future perspectives. Nihon Geka Gakkai Zasshi. 2014;115(1):17–21 (in Japanese).
Greene FL. Breast tumours. In: Sobin LH, Wittekind C, editors. TNM classification of malignant tumours. 6th ed. New York: Wiley; 2002. p. 131–41.
World Health Organization. Tumours of the Breast and Female Genital Organs. Oxford: Oxford University Press; 2003.
Pant K, Dutta U. Understanding and management of male breast cancer: a critical review. Med Oncol. 2008;25(3):294–8.
Hartman M, Czene K, Reilly M, Adolfsson J, Bergh J, Adami HO, et al. Incidence and prognosis of synchronous and metachronous bilateral breast cancer. J Clin Oncol. 2007;25(27):4210–6.
Heron DE, Komarnicky LT, Hyslop T, Schwartz GF, Mansfield CM. Bilateral breast carcinoma: risk factors and outcomes for patients with synchronous and metachronous disease. Cancer. 2000;88(12):2739–50.
Slattery ML, Kerber RA. A comprehensive evaluation of family history and breast cancer risk. The Utah population database. JAMA. 1993;270(13):1563–8.
Surveillance, Epidemiology, End Results Program. http://seer.cancer.gov/statfacts/html/breast.html.
Kim Z, Min SY, Yoon CS, Lee HJ, Lee JS, Youn H, et al. Korean Breast Cancer Society. The basic facts of Korean breast cancer in 2011: results of a nationwide survey and breast cancer registry database. J Breast Cancer. 2014;17(2):99–106.
Baum M, Budzar AU, Cuzick J, Forbes J, Houghton JH, Klijn JG, ATAC Trialists’ Group, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet. 2002;359(9324):2131–9.
Jiralerspong S, Kim ES, Dong W, Feng L, Hortobagyi GN, Giordano SH. Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol. 2013;24(10):2506–14.
Ministry of Health, Labour and Welfare, Japan. http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa13/index.html.
Chen AC, Paulino AC, Schwartz MR, Rodriguez AA, Bass BL, Chang JC, Teh BS. Population-based comparison of prognostic factors in invasive micropapillary and invasive ductal carcinoma of the breast. Br J Cancer. 2014;111(3):619–22.
Brouckaert OI, Laenen A, Vanderhaegen J, Wildiers H, Leunen K, Amant F, et al. Applying the 2011 St Gallen panel of prognostic markers on a large single hospital cohort of consecutively treated primary operable breast cancers. Ann Oncol. 2012;23(10):2578–84.
Burstein HJ, Polyak K, Wong JS, Lester SC, Kaelin CM. Ductal carcinoma in situ of the breast. N Engl J Med. 2004;350:1430–41.
Li CI, Anderson BO, Daling JR, Moe RE. Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA. 2003;289(11):1421–4.
Ellis IO, Cornelisse CJ, Schnitt SJ, Sasco AJ, Sastre-Garau X, Kaaks R, et al. Invasive breast carcinoma. In: Tavassoli FA, Devilee P, editors. World Health Organization Classification of Tumors: pathology and genetics of tumors of the breast and female genital organs. Lyon: IARC Press; 2003. p. 13–59.
Yamashita H, Iwase H, Toyama T, Takahashi S, Sugiura H, et al. Estrogen receptor-positive breast cancer in Japanese women: trends in incidence, characteristics, and prognosis. Ann Oncol. 2011;22:1318–25.
Hosoda M, Yamamoto M, Nakano K, Hatanaka K, Takakuwa E, Hatanaka Y, et al. Differential expression of progesterone receptor, FOXA1, GATA3 and p53 between pre- and postmenopausal women with estrogen receptor-positive breast cancer. Breast Cancer Res Treat. 2014;144:249–61.
Clarke CA, Keegan TH, Yang J, Press DJ, Kurian AW, Patel AH, et al. Age-specific incidence of breast cancer subtypes: understanding the black-white crossover. J Natl Cancer Inst. 2012;104(14):1094–101.
Ko BS, Noh WC, Kang SS, Park BW, Kang EY, Paik NS, et al. Korean Breast Cancer Society. Changing patterns in the clinical characteristics of Korean breast cancer from 1996-2010 using an online nationwide breast cancer database. J Breast Cancer. 2012;15:393–400.
Leong SPL, Shen Z-Z, Liu T-J, Agarwal G, Tajima T, Paik N-S, Sandelin K, et al. Is breast cancer the same disease in Asian and Western Countries? World J Surg. 2010;34:2308–24.
Rescigno J, Zampell JC, Axelrod D. Patterns of axillary surgical care for breast cancer in the era of sentinel lymph node biopsy. Ann Surg Oncol. 2009;16:687–96.
Jagsi R, Abrahams P, Morrow M, Hawlet ST, Griggs JJ, Graff JJ, et al. Patterns and correlates of adjuvant radiotherapy receipt after lumpectomy and after mastectomy for breast cancer. J Clin Oncol. 2010;28:2396–403.
Acknowledgments
The authors thank the Registration Committee of the JBCS and the Public Health Research Foundation for their data collection and analysis. They also thank the affiliated institutes participating in the Breast Cancer Registry of the JBCS for their efforts to register patients’ data.
Conflict of Interest
J. Kurebayashi and S. Saji received research funding from Eisai Co. and Chugai Pharmaceutical Co., Ltd, respectively. The other authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kurebayashi, J., Miyoshi, Y., Ishikawa, T. et al. Clinicopathological characteristics of breast cancer and trends in the management of breast cancer patients in Japan: Based on the Breast Cancer Registry of the Japanese Breast Cancer Society between 2004 and 2011. Breast Cancer 22, 235–244 (2015). https://doi.org/10.1007/s12282-015-0599-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-015-0599-6