Abstract
Several multigene assays have been developed to predict the risk of distant recurrence and response to adjuvant therapy in early breast cancer. However, the prognostic or predictive value of current proliferation gene signature-based assays are limited to hormone receptor-positive, human epidermal growth factor receptor 2-negative (HR+/HER2−) early breast cancer. Considerable discordance between the different assays in classifying patients into risk groups has also been reported, thus raising questions about the clinical utility of these assays for individual patients. Therefore, there still remains a need for better prognostic or predictive biomarkers for breast cancer. The role of immune cells comprising tumor microenvironment in tumor progression has been recognized. Accumulating evidences have shown that immune gene signatures and tumor-infiltrating lymphocytes (TILs) can be prognostic or predictive factors in breast cancer, particularly with regard to HER2+ and triple-negative breast cancer. In this review, I summarize current multigene assays for breast cancer and discuss recent progress in identifying novel breast cancer biomarkers, focusing on the emerging importance of immune gene signatures and TILs as prognostic or predictive biomarkers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For optimal treatment decision-making in patients with early breast cancer, it is important to accurately predict the risk of recurrence and response to therapy. Clinicopathological variables, such as tumor size, lymph node (LN) status, and tumor grade are traditional prognostic factors, whereas estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) status are both prognostic and predictive factors for breast cancer (Donegan 1997; Cianfrocca and Goldstein 2004). ER status predicts responses to endocrine therapy and HER2 status is useful for identifying patients who are likely to benefit from anti-HER2 therapy (Cianfrocca and Goldstein 2004; Nicolini et al. 2018).
However, these traditional factors alone are not sufficient for optimal treatment decisions, and, consequently, several molecular assays based on multiple gene expression signatures have been developed to better predict the prognosis and treatment responses among breast cancer patients. Since the introduction of the first-generation multigene assays, including MammaPrint (van ‘t Veer et al. 2002) and Oncotype DX (Paik et al. 2004), several prognostic assays for early breast cancer, such as Prosigna (Parker et al. 2009) and EndoPredict (Filipits et al. 2011) have been subsequently developed. These assays have been shown to provide additional prognostic value beyond that provided by clinicopathological factors. Two assays—Oncotype DX (Paik et al. 2006; Albain et al. 2010; Sparano et al. 2018) and MammaPrint (Cardoso et al. 2016)—have also been shown to be predictive for adjuvant chemotherapy in hormone receptor-positive and HER2-negative (HR+/HER2−) early breast cancer.
Although substantial progress has been made with regard to molecular breast cancer assays, several major challenges remain. These assays are strong prognostic factors for early recurrence, but they are suboptimal for predicting late recurrence (> 5 years after diagnosis) in HR+/HER2− early breast cancer (Partridge and Carey 2017). Considerable discordance between the different assays in classifying patients into risk groups has also been reported, raising questions about the accuracy of these assays for individual patients (Bartlett et al. 2016; Varga et al. 2019). Moreover, the prognostic or predictive values of these assays are limited to HR+/HER2− breast cancer but not other subtypes of breast cancer (Varga et al. 2019). Therefore, there is a need for better predictors for late recurrence and chemotherapy benefit in HR+/HER2− early breast cancer and novel prognostic or predictive markers for other subtypes of breast cancer, including HR−/HER2+ and triple-negative breast cancer (TNBC, HR−/HER2−), in which it is difficult to accurately predict the response to first-line chemotherapy or HER2-targeted therapy. More recently, with the development of immunotherapies in breast cancer, there is an emerging need to identify reliable biomarkers to predict which patients will benefit from immune checkpoint inhibitors.
Tumors comprise not only tumor cells but also surrounding stroma, including extracellular matrix (ECM) and various stromal cells, such as endothelial cells, fibroblasts and infiltrating immune cells (Joyce 2005). ECM and stromal cells constituting the tumor microenvironment are known to contribute to cancer progression through interactions with malignant cells (Hanahan and Weinberg 2011). Tumor-associated stromal cells, such as cancer-associated fibroblasts and macrophages, have been reported to play roles in breast cancer progression (Mao et al. 2013). There is accumulating evidence supporting the clinical significance of stromal and immune gene signatures as prognostic or predictive markers for breast cancer. However, these gene signatures have not been incorporated into the most current multigene assays, and to date, there is no commercial assay mainly based on immune gene signatures. Given that most of currently available assays rely on the expression of HR or proliferation-related genes in tumor cells and that their utility is limited to early HR+/HER2− breast cancer (Varga et al. 2019), stromal or immune gene expression reflecting the tumor microenvironment may contribute to the development of better prognostic or predictive markers for breast cancer. In this review, I summarize the current multigene prognostic assays for breast cancer and discuss recent progress in identifying novel prognostic or predictive biomarkers, with a focus on immune gene signatures. I also discuss how stromal or immune gene signatures can be incorporated into current multigene assays to improve their prognostic or predictive ability and can be used to develop novel assays for breast cancer.
Multigene signature-based prognostic assays for HR+/HER2− early breast cancer
The commonly used commercial molecular assays for breast cancer include Oncotype DX, MammaPrint, Prosigna, EndoPredict, and Breast Cancer Index (BCI). These assays are available for clinical use. The details of the assays are provided in Table 1.
Oncotype DX, the most commonly used test, is a 21-gene signature assay based on quantitative real-time reverse transcription-PCR (qRT-PCR). Patients are classified into low-, intermediate-, and high-risk categories according to the recurrence score (RS) calculated from the expression of 21 genes, comprising 16 cancer-related and five reference genes (Paik et al. 2004). The prognostic and predictive value of the Oncotype DX RS for patients with pathologic N0 or N1 status (pN0-N1), ER+ breast cancer was validated in several retrospective trials (Paik et al. 2004; Paik et al. 2006; Albain et al. 2010; Dowsett et al. 2010; Mamounas et al. 2017). The TAILORx trial prospectively validated the clinical utility of Oncotype DX in HR+/HER2−, lymph node-negative (LN−) breast cancer. Low-risk patients (RS 0–10) who were treated with endocrine therapy alone had very low recurrence rates at 5 years (Sparano et al. 2015). A further study conducted to assess the predictive value of RS in patients with intermediate risk (RS 11–25) revealed no benefits of chemotherapy in patients aged > 50 years but showed chemotherapeutic benefits in those aged ≤ 50 years who had a RS 16–25 (Sparano et al. 2018). Taken together, TAILORx results demonstrated that patients with low or intermediate RS do not benefit from adjuvant chemotherapy. More recently, a secondary analysis of the TAILORx data demonstrated that clinical risk stratification provided additional prognostic information for patients aged ≤ 50 years with a RS of 16–25 (Sparano et al. 2019). Importantly, this study showed that there was no benefit from chemotherapy for women aged ≤ 50 years with a RS of 16–20 and low clinical risk. However, patients with a RS of 16–25 and high clinical risk benefitted from chemotherapy.
MammaPrint, a microarray-based 70-gene assay was the first molecular assay to receive approval by the Food and Drug Administration (FDA) in the United States (Ross et al. 2008). This assay classifies patients into low- and high-risk groups based on the risk of distant recurrence within 5 years and 10 years (van ‘t Veer et al. 2002). The prognostic ability of this assay in early breast cancer was independently validated by a study conducted by the TRANSBIG consortium (Buyse et al. 2006). The prospective MINDACT trial assessed the clinical utility of the addition of MammaPrint to standard clinicopathological factors for selecting patients for adjuvant chemotherapy. It demonstrated a clinical rationale behind excluding chemotherapy based on low MammaPrint risk scores in early breast cancer (Cardoso et al. 2016). Recently, the PROMIS trial—conducted to determine whether MammaPrint could inform treatment decisions for patients with intermediate Oncotype DX RS (RS 18–30)—showed that, in 33.6% of cases, treatment decisions were changed based on MammaPrint results (Tsai et al. 2018).
The Prosigna assay, which was approved by the FDA in 2013 (Nielsen et al. 2014), calculates a risk of recurrence (ROR) score based on the expression of 50 genes, molecular subtypes, tumor size, LN status, and proliferation score (Parker et al. 2009). The Prosigna assay classifies postmenopausal HR+ breast cancer patients into low-, intermediate-, and high-risk categories according to the risk of 10-year recurrence (Parker et al. 2009; Dowsett et al. 2013). The prognostic value of ROR scores was validated in the ABCSG8 (Gnant et al. 2014) and TransATAC trials (Sestak et al. 2015), showing that low ROR is associated with a very low 10-year risk of distant recurrence. ROR score was also shown to predict 10-year distant recurrence in chemotherapy-treated patients in the DBCG77B trial (Laenkholm et al. 2018). The ability of the Prosigna to predict who might benefit from chemotherapy is currently under investigation in the OPTIMA trial (Bartlett et al. 2013), and some studies have reported its possible predictive value. Prosigna ROR and intrinsic subtype have been demonstrated as significant predictors of response to neoadjuvant chemotherapy in HR+/HER2− breast cancer (Prat et al. 2016). A recent study also showed that ROR is prognostic for high-risk premenopausal patients and the basal-like or luminal B subtypes predict the benefit of adjuvant cyclophosphamide-based chemotherapy in high-risk patients (Jensen et al. 2018).
The EndoPredict assay provides an EPclin score based on a combination of 12 gene signatures (EP score), tumor size, and LN status (Filipits et al. 2011). This assay was validated using the ABCSG06 (Filipits et al. 2011) and ABCSG08 cohorts (Fitzal et al. 2015) of ER+ postmenopausal patients and was demonstrated to be prognostic for 10-year risk of distant recurrence in ER+/HER2− breast cancer treated with endocrine therapy. EPclin score was also shown to be an independent prognostic factor for node-positive (LN+), ER+/HER2− breast cancer patients treated with adjuvant chemotherapy followed by hormone therapy (Martin et al. 2014). Recently, a modified EPclin test (mEPclin), which was a combination of EP score, postneoadjuvant pathologic tumor size, and LN status, was developed; it independently predicted the risk of distant recurrence after neoadjuvant chemotherapy (Loibl et al. 2018).
The BCI is a seven-gene signature, combining the molecular grade index (five genes) and the HOXB13:IL17BR ratio (two genes) (Ma et al. 2008). This index was validated to be prognostic for late distant recurrence as well as early recurrence in ER+/HER2−, LN− breast cancer (Sgroi et al. 2013; Zhang et al. 2013). BCI was also shown to be prognostic in both LN− and LN+ breast cancer (Sgroi et al. 2016).
The GenesWell BCT is a recently developed prognostic assay. The BCT score calculated by this assay was validated to predict the risk of late distant metastasis as well as early recurrence in patients with pN0-N1, HR+/HER2− breast cancer (Gong et al. 2017). BCT score is calculated based on the combination of expression of six prognostic genes normalized by three reference genes with two clinical variables (LN status and tumor size) (Gong et al. 2017). The six prognostic genes consist of five proliferation-related genes (UBE2C, TOP2A, RRM2, FOXM1, and MK167) and one immune response gene (BTN3A2). BCT score was also shown to be predictive of chemotherapy benefit among Asian patients with HR+/HER2−, LN− breast cancer (Kwon et al. 2018). Although further prospective studies for assessing the clinical utility of this assay in large populations are warranted, existing evidence suggests that the inclusion of immune-related genes may be useful for predicting late distant recurrence and chemotherapy benefit in HR+/HER2− early breast cancer. Notably, the prognostic value of this assay was validated in Asian populations including more young patients, whereas most other assays were validated in populations of Western postmenopausal women.
Comparisons among the current multigene assays for breast cancer
The clinical utility of these multigene breast cancer assays has been evaluated by several international guidelines. Based on the increasing evidences supporting the prognostic value of commonly used multigene assays, such as Oncotype DX, MammaPrint, EndoPredict, Prosigna, and BCI, the St. Gallen International Breast Cancer Conference Panel suggested that the results of these assays can help decide whether adjuvant chemotherapy should be included to treat luminal breast cancer (Coates et al. 2015). The American Society of Clinical Oncology Breast Cancer Guidelines Advisory Group and Clinical Practice Guidelines Committee also recently found sufficient clinical utility of the multigene assays Oncotype DX, Prosigna, and BCI, to guide decisions on the need for adjuvant systemic therapy in early breast cancer; however, there is no biomarker to guide the choice of specific regimens (Harris et al. 2016). Importantly, the Oncotype DX RS along with biological factors, such as tumor grade, proliferation rate, ER/PR expression, and HER2 expression, were incorporated into the eighth edition of the American Joint Committee on Cancer staging system for breast cancer (Giuliano et al. 2017). These results demonstrate that the multigene assays provide additional prognostic or predictive information beyond traditional factors and can be used to assist decisions about adjuvant therapy.
Several studies have compared the prognostic values of multigene signatures. ROR (Dowsett et al. 2013) and EPclin (Buus et al. 2016) scores were shown to be more accurate for predicting the risk of distant recurrence than RS among endocrine-treated postmenopausal women with ER+ breast cancer. Similarly, a recent study, which included 774 postmenopausal patients with ER+/HER2− breast cancer from the ATAC trial and compared the prognostic values of six multigene signatures, demonstrated that ROR, BCI, and EPclin are more prognostic for overall and late distant recurrence than RS in patients with LN− breast cancer (Sestak et al. 2018). All six signatures provided less information for distant recurrence in patients with one to three positive nodes. However, it was noteworthy that BCI and EPclin, which are based on the combination of gene expression and clinical information, showed a better prognostic ability than the other signatures in patients with LN+ disease. These results suggest that clinical factors are important for predicting late recurrence and prognosis in LN+ breast cancer.
A recent study reviewed 14 available studies and found discordances among the five commercially available assays for early breast cancer in terms of patient risk stratifications (Varga et al. 2019). Overall discordance between the Oncotype DX and the other assays (MammaPrint, BCI, Prosigna, and EndoPredict) ranged from 42 to 66%. The proportion of patients classified as high risk was the smallest with Oncotype DX RS (11.5%) when patients with a RS ≥ 31 were defined as high risk, whereas 63% and 48.4% of patients were classified as high risk according to the EndoPredict assay’s EP and EPclin scores, respectively. These results showed that there are considerable differences in risk stratification among the five most common multigene assays and that these assays should not be used interchangeably, thereby suggesting that the clinical utility of each assay should be validated by adequate prospective clinical trials.
Most current multigene assays for breast cancer are based on the expression of HR or proliferation-related genes. Oncotype DX relies on the genes that define the ER status, HER2 status, tumor proliferation, and tumor invasion (Paik et al. 2004). EndoPredict is also based on three proliferation genes and five HR-related genes (Filipits et al. 2011). For MammaPrint and Prosigna assays, genes associated with various pathways—such as adhesion and angiogenesis—as well as proliferation and HR-related genes are included (Tian et al. 2010; Wallden et al. 2015). However, proliferation-based gene signatures are known to be strongly prognostic for early recurrence in ER+/HER2− breast cancer but less prognostic for late recurrence (Gingras et al. 2015). Recent studies have reported that the expression of genes associated with epithelial-mesenchymal plasticity and with stromal activation and immune responses can be better predictors for late recurrence (Mittempergher et al. 2013; Cheng et al. 2014). Moreover, it has been suggested that molecular analysis of circulating tumor cells and circulating tumor DNA after adjuvant therapy— rather than transcriptome analysis of primary tumor—may be better for identifying patients at high risk of late recurrence (Ignatiadis and Dawson 2014).
Immune gene signatures as prognostic or predictive biomarkers in breast cancer
Proliferation-related gene signatures from tumor cells have limitations in predicting prognosis of or response to therapies in breast cancer. Given that both tumor cells and the surrounding stromal cells are prognostic, analysis of both the surrounding stromal and tumor tissue may facilitate the identification of better gene signatures associated with patient outcomes and responses to therapy in breast cancer. Accordingly, attempts have been made previously to identify prognostic or predictive stromal gene signatures for breast cancer using gene expression microarray data.
Finak et al. (2008), found a new 26-gene stroma-derived prognostic predictor (SDPP) associated with clinical outcome of breast cancer patients. Importantly, 26-gene SDPP derived from tumor stroma predicted clinical outcomes in several published whole tumor-derived expression datasets. Five biological categories, including matrix remodeling, hypoxia, fibroblast signaling, ER signaling, and immune response, were identified in the 26-gene SDPP. Good clinical outcome clusters overexpressed a set of immune-related genes, including T cells and natural killer (NK) cell markers representing the T-helper type 1 (Th1) immune response. In contrast, poor clinical clusters showed the markers of an increased hypoxic and angiogenic response, tumor-associated macrophage responses, as well as a decrease in chemokines that stimulate NK cell migration and mediate pro-survival signals in T lymphocytes. Of note, SDPP predicted clinical outcome of patients from multiple clinical subtypes, and its prognostic power improved on combining it with other signatures. This suggested that integrating tumor microenvironment factors into prognostic prediction may contribute to the development of novel assays beyond the currently available molecular assays. Another study revealed the importance of the molecular composition of matrix-producing cells—rather than the extent of matrix production—in breast cancer prognosis. (Winslow et al. 2016). Stromal gene signature was also shown to predict resistance to neoadjuvant chemotherapy with 5-fluorouracil, epirubicin, and cyclophosphamide among patients with ER− tumors (Farmer et al. 2009); in that study, a 50-gene signature that predicts poor responses to anthracycline-based neoadjuvant chemotherapy was developed.
A meta-analysis analyzing biological processes in different breast cancer subtypes revealed that tumor invasion and immune response-related genes were associated with the prognosis in HER2+ and ER−/HER2− breast cancer, whereas the prognostic value of proliferation-related genes was limited to the ER+/HER2− subtype (Desmedt et al. 2008). In line with this, a number of studies based on pooled gene expression microarray analyses have identified immune gene signatures associated with clinical outcome of HR− breast cancer patients (Table 2). Generally, high expression of immune response-related genes was associated with favorable prognosis of patients with HR− breast cancer. Downregulation of seven genes related to immune/defense response (C1QA, IGLC2, LY9, TNFRSF17, SPP1, XCL2, and HLA-F) was associated with a greater risk of distant metastasis (Teschendorff et al. 2007), and the classifier based on the expression of these seven genes was further developed and validated to identify ER− patients with a good prognosis independently of LN status (Teschendorff and Caldas 2008). T cell surrogate marker (lymphocyte-specific kinase metagene) had a strong positive prognostic significance in all ER− tumors and ER+/HER2+ breast cancer, whereas B cell surrogate markers (IgG metagenes) had no prognostic significance (Rody et al. 2009). Moreover, 14 novel prognostic genes (CXCL13, CLIC5, RGS4, RPS28, RFX7, EXOC7, HAPLN1, ZNF3, SSX3, HRBL, PRRG3, ABO, PRTN3, MATN1), including eight genes linked to immune/inflammatory chemokine regulation, were identified for HR− breast cancer, including TNBC, and this HR−/TNBC gene signature index was shown to be superior to other gene signatures with regard to the prediction of metastasis outcome of patients with early-stage HR− breast cancer/TNBC (Yau et al. 2010).
Moreover, using two HR−/TNBC gene signatures derived from previous studies, seven gene signatures identified by Treschendorff et al. (Teschendorff et al. 2007; Teschendorff and Caldas 2008), and 14 prognostic gene candidates identified by Yau et al. (Yau et al. 2010), an optimized five-gene (TNFRSF17, CLIC5, HLA-F, CXCL13, XCL2) predictor based on a functional pathway through interferon-gamma (IFN-γ) and IL-10 was further developed. Integrated cytokine score calculated from the expression of this five-gene panel was validated as a significant predictor for distant recurrence in formalin-fixed, paraffin-embedded (FFPE) samples of HR− breast cancer/TNBC (Yau et al. 2013). A ratio of high B-cell and low IL-8 metagenes was reported to be associated with good prognosis in TNBC (Rody et al. 2011). A recent study also found that elevated expression of T cell immune response-related genes (BTN3A2 and CD2) was associated with a lower risk of distant metastasis in FFPE tissue samples of HR−/HER2+ breast cancer, but not in other subtypes (Han et al. 2017). Moreover, risk scores based on the expression of MMP11 and CD2 were prognostic for distant metastasis in HR−/HER2+ breast cancer, demonstrating the prognostic significance of immune signatures for identifying HR−/HER2+ breast cancer patients with good prognoses.
However, some studies have shown that immune gene signatures, such as B cell metagene can be prognostic for HR+ breast cancer—particularly highly proliferative breast cancer—regardless of ER status, whereas most immune gene-based signatures have been shown to be associated with prognosis of patients with HR− breast cancer (Table 2). B cell metagene, including immunoglobulin genes (IGKC, IGHG, and IGHM), was associated with longer metastasis-free survival in highly proliferative LN− breast cancer regardless of ESR1 and ERBB2 status (Schmidt et al. 2008). These results suggest that humoral immune responses may be associated with favorable prognosis in highly proliferative early breast cancer. Similarly, another study (Bianchini et al. 2010) showed that a B cell/plasma cell metagene dominated by immunoglobulin genes (IGKC, IGHG3, IGL, IGHA1, and IGHG3) has a strong prognostic value for ER+ highly proliferative cancer but a lesser prognostic value for ER− cancer and no prognostic value for ER+/low proliferation, indicating that this B cell/plasma cell metagene can identify patients with favorable prognosis among highly proliferative ER− and ER+ cancers. These results are also consistent with a study which revealed that high proliferative activity was associated with an increased immune responses in both ER− and ER+ breast cancer and that a positive prognostic effect of immune response genes was found in LN− breast cancer regardless of ER status (Oh et al. 2012). A five-gene signature including B cell response genes (IGK@, GBP1, STAT1, IGLL5, and OCLN) was associated with relapse-free survival in breast cancer (Ascierto et al. 2012).
More recently, 17 immunity genes (APOBEC3G, CCL5, CCR2, CD2, CD27, CD3D, CD52, CORO1A, CXCL9, GZMA, GZMK, HLA-DMA, IL2RG, LCK, PRKCB, PTPRC, and SH2D1A) were derived from the Affymetrix gene expression microarray dataset that included 1951 patients (Yang et al. 2018). This 17-immunity gene signature was prognostic for distant metastasis-free survival only among patients with ER− and highly proliferative breast cancers. Patients with high expression of these immunity genes had significantly better outcomes. A Cox model to predict the risk of distant metastasis was built using a 72-gene panel incorporating breast cancer subtypes, proliferation score, and immunity score. The prognostic significance of this model was validated in independent gene expression datasets. This study suggested that immunity gene expression is an important prognostic factor, which needs to be incorporated into current multigene assays for improving the prediction of distant metastasis risk in breast cancer.
Immune gene signatures or the expression of immune-related genes have also been reported to be associated with response to treatment in breast cancer. Higher expression of immune-related genes including cytotoxic molecules, T cell receptor signaling pathway components, Th1-related cytokines, and B cell markers was correlated with a pathological complete response in TNBC patients treated with neoadjuvant chemotherapy (Lee et al. 2015). A recent study showed that combining radiosensitivity and immune gene signatures may be potential to predict the response to adjuvant radiotherapy (Cui et al. 2018). These results suggested that immune gene signatures may be useful to select patients who are mostly like to benefit from neoadjuvant chemotherapy or adjuvant radiotherapy in breast cancer.
Tumor-infiltrating lymphocytes as prognostic or predictive biomarkers in breast cancer
Various immune cells present in the tumor microenvironment, including cytotoxic T cells, Th cells, dendritic cells, NK cells, and macrophages, are usually called tumor-infiltrating lymphocytes (TILs) (Fridman et al. 2012; Savas et al. 2016). However, the role of TILs on tumor progression may be different depending on the type of TILs. Some infiltrating immune cells (M2 macrophages, myeloid-derived suppressor cells, regulatory T cells [Treg], and Th2 cells) are known to contribute to pro-tumor activity, whereas tumor-infiltrating dendritic cells, M1 macrophages, Th1 cells, CD8+ T cells, and NK cells suppress tumor progression (Salgado et al. 2015b). TILs are reportedly associated with prognosis and response to therapy in human cancer (Fridman et al. 2012; Luen et al. 2017).
Consistent with these findings, a growing number of studies are showing the significance of TILs as prognostic or predictive markers in breast cancer. In particular, a high TIL level has been observed in TNBC and HER2+ breast cancer and have been associated with a favorable prognosis (Loi et al. 2013; Adams et al. 2014; Loi et al. 2014; Salgado et al. 2015a; Hida et al. 2016; Ingold Heppner et al. 2016; Althobiti et al. 2018). TILs have also been shown to predict improved responses to neoadjuvant chemotherapy, particularly in TNBC (Ono et al. 2012), as well as to trastuzumab in HER2+ breast cancer (Loi et al. 2014; Ingold Heppner et al. 2016), and to neoadjuvant anti-HER2 agents (trastuzumab or lapatinib) in HER2+ breast cancer (Salgado et al. 2015a).
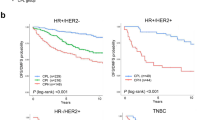
However, the prognostic significance of TILs in breast cancer differs according to the molecular subtype of breast cancer, based on ER/PR or HER2 expression status. In contrast to HR− breast cancer, high TIL levels have been associated with a poor prognosis in ER+ breast cancer (Tsang et al. 2014; Denkert et al. 2018). Tsang et al. (2014), showed that in ER+ breast cancer, high TIL levels were associated with poor prognostic features, including high tumor grade and lymphovascular invasion, and they have a strong positive correlation with intratumoral accumulation of Tregs. However, high TIL levels were associated with favorable prognosis features in ER−/HER2+ breast cancer. Similarly, a recent study including 3771 patients treated with neoadjuvant therapy was conducted for assessing the prognostic and predictive significance of stromal TILs in different subtypes of breast cancer; it demonstrated that high TIL levels were associated with shorter overall survival in HR+/HER2− breast cancer, whereas there was a correlation between favorable prognosis and high TIL levels among patients with TNBC (Denkert et al. 2018). In this study, a high TIL concentration also predicted a response to neoadjuvant chemotherapy in all molecular subtypes. This study suggested that the difference in the prognostic value of TILs between HR+/HER2− and HR− breast cancer may be explained by different immune cell composition and prognostic effect of each type of immune cell in each subtype of breast cancer. Higher infiltration levels of most immune cell types were observed in TNBC than in HR+/HER2− breast cancer, and most immune cells—including T cells, B cells, and macrophages—were associated with a favorable prognosis in TNBC. In contrast, the presence of T cells was not prognostic, and macrophages were associated with a poor prognosis in HR+/HER2− breast cancer, furthermore, the only cell types associated with improved outcome in HR+ breast cancer were B cells and myeloid dendritic cells. Further studies to investigate the difference in interactions between immune cells and tumor cells according to breast cancer subtypes will be required.
With the emerging importance of TILs as a prognostic or predictive biomarker for breast cancer, there have been efforts to standardize the methods for evaluating TILs. Methodological recommendations on the tumor area for evaluation, the type of immune cell, TIL location (stroma or intratumoral TILs), and scoring methods have been made and updated by an international working group (Salgado et al. 2015b; Dieci et al. 2018). However, further efforts are required to incorporate TILs into diagnostic assays and standard practice as current methods are still experimental.
Emerging biomarkers predicting the response to immunotherapies in breast cancer
Breast cancer, particularly HR+ breast cancer (the most common form), is considered a weakly immunogenic cancer because of the low level of TILs and low mutation rates (Kandoth et al. 2013). However, recent studies have shown that immunogenicity is important in subtypes of breast cancer, including TNBC and HER2+ breast cancer and that TNBC is the most immunogenic subtype associated with the highest TIL levels, which in turn suggests that TNBC is an emerging area of immune-oncology therapeutics (Esteva et al. 2019). Although numerous immunotherapies, such as immune checkpoint inhibitors (anti-CTLA4, PD-1, PD-L1 antibodies) have been approved for other cancers, there were no FDA-approved immunotherapies for breast cancer (Vonderheide et al. 2017) until 2019, when the FDA approved the first immunotherapy for patients with locally advanced or metastatic TNBC expressing PD-L1: a combination of atezolizumab (anti-PD-L1 antibody) and nab-paclitaxel (2019). The number of clinical trials of immunotherapies for breast cancer has increased rapidly in the past 6 years, and 285 clinical trials (as of September 2018) of monotherapies or combination breast cancer therapies are ongoing, in which the agents targeting PD-1 or PD-L1 are predominant (Esteva et al. 2019). Although the number of clinical trials of immunotherapies for TNBC is the largest, ongoing clinical trials are testing the efficacy of immunotherapies in all subtypes of breast cancer (Esteva et al. 2019). To maximize the benefits and minimize the toxicities of cancer immunotherapies, it is important to identify effective biomarkers that predict responses to immunotherapies. With the advances in the development of immunotherapies for breast cancer, there is an accompanying need for reliable predictive biomarkers for immunotherapies in breast cancer.
Currently, PD-L1 expression by immunohistochemistry (IHC) is the most widely used biomarker for selecting patients for immunotherapies and is FDA approved as a companion diagnostic test for anti-PD-1 therapy in some cancer types, including non-small cell lung cancer (Chan et al. 2019; Havel et al. 2019). PD-L1 expression varied widely across cancer types. The percentage of tumors with positive PD-L1 expression by IHC was relatively low in breast cancer compared with other cancer types, such as thymic and nasopharyngeal cancers (Yarchoan et al. 2019). PD-L1 expression by IHC or gene expression was observed in approximately 20–40% of breast cancer and higher PD-L1 expression (up to 60% of PD-L1 expression) has been reported in TNBC than other subtypes (Miglietta et al. 2019). As in other cancers, PD-L1 has been suggested as a potential predictive biomarker for immune checkpoint inhibitors in breast cancer and its predictive value has been evaluated in clinical studies. Some studies showed that PD-L1 positivity is associated with greater responses to anti-PD-1/PD-L1 therapies in breast cancer (Dirix et al. 2018; Adams et al. 2019a, b). Importantly, a Phase III trial randomized patients with TNBC to receive atezolizumab+ nab-paclitaxel versus placebo+ nab-paclitaxel demonstrated that there was a greater survival benefit for atezolizumab arm in PD-L1-positive patients than PD-L1-negative patients, suggesting the predictive value of PD-L1 for anti-PD-L1 therapy in TNBC (Schmid et al. 2018). However, many technical and biological issues including the standardization of PD-L1 testing need to be addressed to implement PD-L1 as a reliable marker for identifying patients that will benefit from immunotherapies. Moreover, because PD-L1 expression alone is insufficient for properly selecting patients for immunotherapies, further efforts are needed to identify additional predictive markers to improve patient selection for immunotherapies. Another emerging predictive biomarker is a tumor mutation burden (TMB) and a higher TMB has been shown to be correlated with clinical benefit from immune checkpoint inhibitors across multiple cancer types (Chan et al. 2019). However, the association between TMB and response to immune checkpoint inhibitors in breast cancer is unclear and further investigation is required.
Of note, tumor immune microenvironment features, such as TILs and interferon-inflammatory immune gene signatures, are also known to be associated with the response to immune checkpoint inhibitors (Gibney et al. 2016; Havel et al. 2019). CD8+ T cell density at the invasive margin of a tumor, as measured by IHC, was strongly associated with the pembrolizumab (anti-PD-1 antibody) response in melanoma (Tumeh et al. 2014). Ayers et al. (2017), showed that IFN-γ-related gene expression predicts clinical responses to anti-PD-1 therapy. Another recent study reported that a tumor inflammation signature based on 18 genes that measure an adaptive immune response within tumors is associated with sensitivity to PD-1-targeting therapy (Danaher et al. 2018); these 18 genes comprised the genes associated with cytotoxic cells, antigen presentation, and IFN-γ activity. However, these markers have not yet been clinically validated in several cancers, including breast cancer, and further validation will be required for them to be used clinically.
Conclusion
Over the past two decades, several multigene assays have been developed to predict breast cancer prognosis and responses to therapy beyond what can be accomplished by traditional clinical factors. However, there still remains a need for better prognostic or predictive biomarkers for breast cancer. The clinical significance of stroma, including ECM and immune cells, as well as of tumor cells has been recognized, and several studies have shown that immune gene signatures or TILs can predict prognosis and responses to neoadjuvant chemotherapy or anti-HER2 therapies in HER2+ breast cancer or TNBC. Furthermore, high TIL levels or immunogenicity of HR− breast cancer, particularly TNBC, suggest the needs for appropriate predictive biomarkers for immunotherapies. The integration of immune gene signatures reflecting the tumor microenvironment, in combination with other molecular gene signatures, is expected to improve the prognostic and predictive value of currently available assays (Fig. 1). For example, the incorporation of immune gene signatures into current proliferation gene-based multigene assays may improve their prognostic ability or their ability to predict the response to neoadjuvant chemotherapy or anti-HER2 agents in HR− or HER2+ breast cancer. Furthermore, given the prognostic value of immune gene signatures in highly proliferative tumors regardless of ER status, it will be possible to develop the novel assay identifying low-risk patients from high-risk patients across all subtypes of breast cancer. Immune gene signatures or TILs can also be used to develop the predictive biomarkers to select patients that will benefit from immunotherapies. Therefore, it is necessary to incorporate immune gene signatures into the prognostic and predictive signatures in the future development of novel multigene assays for breast cancer.
Strategies for the development of novel prognostic or predictive biomarkers in breast cancer. Incorporation of immune gene signatures or tumor-infiltrating lymphocytes (TILs) into the prediction of prognosis and response to treatment may improve the prognostic or predictive ability of current multigene assays or may contribute to the development of novel multigene assays beyond the currently available commercial assays. ER estrogen receptor, HER2 human epidermal growth factor receptor 2, HR hormone receptor, TNBC triple-negative breast cancer
References
(2019) Atezolizumab combo approved for PD-L1-positive TNBC. Cancer Discov 9:OF2. https://doi.org/10.1158/2159-8290.cd-nb2019-038
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, Martino S, Wang M, Jones VE, Saphner TJ, Wolff AC, Wood WC, Davidson NE, Sledge GW, Sparano JA, Badve SS (2014) Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol 32:2959–2966. https://doi.org/10.1200/JCO.2013.55.0491
Adams S, Loi S, Toppmeyer D, Cescon DW, De Laurentiis M, Nanda R, Winer EP, Mukai H, Tamura K, Armstrong A, Liu MC, Iwata H, Ryvo L, Wimberger P, Rugo HS, Tan AR, Jia L, Ding Y, Karantza V, Schmid P (2019a) Pembrolizumab monotherapy for previously untreated, PD-L1-positive, metastatic triple-negative breast cancer: cohort B of the phase II KEYNOTE-086 study. Ann Oncol 30:405–411. https://doi.org/10.1093/annonc/mdy518
Adams S, Schmid P, Rugo HS, Winer EP, Loirat D, Awada A, Cescon DW, Iwata H, Campone M, Nanda R, Hui R, Curigliano G, Toppmeyer D, O’Shaughnessy J, Loi S, Paluch-Shimon S, Tan AR, Card D, Zhao J, Karantza V, Cortes J (2019b) Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: cohort A of the phase II KEYNOTE-086 study. Ann Oncol 30:397–404. https://doi.org/10.1093/annonc/mdy517
Albain KS, Barlow WE, Shak S, Hortobagyi GN, Livingston RB, Yeh IT, Ravdin P, Bugarini R, Baehner FL, Davidson NE, Sledge GW, Winer EP, Hudis C, Ingle JN, Perez EA, Pritchard KI, Shepherd L, Gralow JR, Yoshizawa C, Allred DC, Osborne CK, Hayes DF, Breast Cancer Intergroup of North America (2010) Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol 11:55–65. https://doi.org/10.1016/S1470-2045(09)70314-6
Althobiti M, Aleskandarany MA, Joseph C, Toss M, Mongan N, Diez-Rodriguez M, Nolan CC, Ashankyty I, Ellis IO, Green AR, Rakha EA (2018) Heterogeneity of tumour-infiltrating lymphocytes in breast cancer and its prognostic significance. Histopathology 73:887–896. https://doi.org/10.1111/his.13695
Ascierto ML, Kmieciak M, Idowu MO, Manjili R, Zhao Y, Grimes M, Dumur C, Wang E, Ramakrishnan V, Wang XY, Bear HD, Marincola FM, Manjili MH (2012) A signature of immune function genes associated with recurrence-free survival in breast cancer patients. Breast Cancer Res Treat 131:871–880. https://doi.org/10.1007/s10549-011-1470-x
Ayers M, Lunceford J, Nebozhyn M, Murphy E, Loboda A, Kaufman DR, Albright A, Cheng JD, Kang SP, Shankaran V, Piha-Paul SA, Yearley J, Seiwert TY, Ribas A, Mcclanahan TK (2017) IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest 127:2930–2940. https://doi.org/10.1172/JCI91190
Bartlett J, Canney P, Campbell A, Cameron D, Donovan J, Dunn J, Earl H, Francis A, Hall P, Harmer V, Higgins H, Hillier L, Hulme C, Hughes-Davies L, Makris A, Morgan A, Mccabe C, Pinder S, Poole C, Rea D, Stallard N, Stein R (2013) Selecting breast cancer patients for chemotherapy: the opening of the UK OPTIMA trial. Clin Oncol (R Coll Radiol) 25:109–116. https://doi.org/10.1016/j.clon.2012.10.005
Bartlett JM, Bayani J, Marshall A, Dunn JA, Campbell A, Cunningham C, Sobol MS, Hall PS, Poole CJ, Cameron DA, Earl HM, Rea DW, Macpherson IR, Canney P, Francis A, Mccabe C, Pinder SE, Hughes-Davies L, Makris A, Stein RC, Optima TMG (2016) Comparing breast cancer multiparameter tests in the OPTIMA Prelim Trial: no test is more equal than the others. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw050
Bianchini G, Qi Y, Alvarez RH, Iwamoto T, Coutant C, Ibrahim NK, Valero V, Cristofanilli M, Green MC, Radvanyi L, Hatzis C, Hortobagyi GN, Andre F, Gianni L, Symmans WF, Pusztai L (2010) Molecular anatomy of breast cancer stroma and its prognostic value in estrogen receptor-positive and -negative cancers. J Clin Oncol 28:4316–4323. https://doi.org/10.1200/JCO.2009.27.2419
Buus R, Sestak I, Kronenwett R, Denkert C, Dubsky P, Krappmann K, Scheer M, Petry C, Cuzick J, Dowsett M (2016) Comparison of EndoPredict and EPclin with Oncotype DX Recurrence Score for prediction of risk of distant recurrence after endocrine therapy. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw149
Buyse M, Loi S, Van’t Veer L, Viale G, Delorenzi M, Glas AM, d’Assignies MS, Bergh J, Lidereau R, Ellis P, Harris A, Bogaerts J, Therasse P, Floore A, Amakrane M, Piette F, Rutgers E, Sotiriou C, Cardoso F, Piccart MJ, TRANSBIG Consortium (2006) Validation and clinical utility of a 70-gene prognostic signature for women with node-negative breast cancer. J Natl Cancer Inst 98:1183–1192. https://doi.org/10.1093/jnci/djj329
Cardoso F, Van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, Pierga JY, Brain E, Causeret S, Delorenzi M, Glas AM, Golfinopoulos V, Goulioti T, Knox S, Matos E, Meulemans B, Neijenhuis PA, Nitz U, Passalacqua R, Ravdin P, Rubio IT, Saghatchian M, Smilde TJ, Sotiriou C, Stork L, Straehle C, Thomas G, Thompson AM, Van Der Hoeven JM, Vuylsteke P, Bernards R, Tryfonidis K, Rutgers E, Piccart M (2016) 70-Gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med 375:717–729. https://doi.org/10.1056/NEJMoa1602253
Chan TA, Yarchoan M, Jaffee E, Swanton C, Quezada SA, Stenzinger A, Peters S (2019) Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol 30:44–56. https://doi.org/10.1093/annonc/mdy495
Cheng Q, Chang JT, Gwin WR, Zhu J, Ambs S, Geradts J, Lyerly HK (2014) A signature of epithelial-mesenchymal plasticity and stromal activation in primary tumor modulates late recurrence in breast cancer independent of disease subtype. Breast Cancer Res 16:407. https://doi.org/10.1186/s13058-014-0407-9
Cianfrocca M, Goldstein LJ (2004) Prognostic and predictive factors in early-stage breast cancer. Oncologist 9:606–616. https://doi.org/10.1634/theoncologist.9-6-606
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, Thurlimann B, Senn HJ, Panel Members (2015) Tailoring therapies—improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 26:1533–1546. https://doi.org/10.1093/annonc/mdv221
Cui Y, Li B, Pollom EL, Horst KC, Li R (2018) Integrating radiosensitivity and immune gene signatures for predicting benefit of radiotherapy in breast cancer. Clin Cancer Res 24:4754–4762. https://doi.org/10.1158/1078-0432.CCR-18-0825
Danaher P, Warren S, Lu R, Samayoa J, Sullivan A, Pekker I, Wallden B, Marincola FM, Cesano A (2018) Pan-cancer adaptive immune resistance as defined by the Tumor Inflammation Signature (TIS): results from The Cancer Genome Atlas (TCGA). J Immunother Cancer 6:63. https://doi.org/10.1186/s40425-018-0367-1
Denkert C, Von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, Budczies J, Huober J, Klauschen F, Furlanetto J, Schmitt WD, Blohmer JU, Karn T, Pfitzner BM, Kummel S, Engels K, Schneeweiss A, Hartmann A, Noske A, Fasching PA, Jackisch C, Van Mackelenbergh M, Sinn P, Schem C, Hanusch C, Untch M, Loibl S (2018) Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol 19:40–50. https://doi.org/10.1016/S1470-2045(17)30904-X
Desmedt C, Haibe-Kains B, Wirapati P, Buyse M, Larsimont D, Bontempi G, Delorenzi M, Piccart M, Sotiriou C (2008) Biological processes associated with breast cancer clinical outcome depend on the molecular subtypes. Clin Cancer Res 14:5158–5165. https://doi.org/10.1158/1078-0432.CCR-07-4756
Dieci MV, Radosevic-Robin N, Fineberg S, Van Den Eynden G, Ternes N, Penault-Llorca F, Pruneri G, D’Alfonso TM, Demaria S, Castaneda C, Sanchez J, Badve S, Michiels S, Bossuyt V, Rojo F, Singh B, Nielsen T, Viale G, Kim SR, Hewitt S, Wienert S, Loibl S, Rimm D, Symmans F, Denkert C, Adams S, Loi S, Salgado R, International Immuno-Oncology Biomarker Working Group on Breast Cancer (2018) Update on tumor-infiltrating lymphocytes (TILs) in breast cancer, including recommendations to assess TILs in residual disease after neoadjuvant therapy and in carcinoma in situ: A report of the International Immuno-Oncology Biomarker Working Group on Breast Cancer. Semin Cancer Biol 52:16–25. https://doi.org/10.1016/j.semcancer.2017
Dirix LY, Takacs I, Jerusalem G, Nikolinakos P, Arkenau HT, Forero-Torres A, Boccia R, Lippman ME, Somer R, Smakal M, Emens LA, Hrinczenko B, Edenfield W, Gurtler J, Von Heydebreck A, Grote HJ, Chin K, Hamilton EP (2018) Avelumab, an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase 1b JAVELIN Solid Tumor study. Breast Cancer Res Treat 167:671–686. https://doi.org/10.1007/s10549-017-4537-5
Donegan WL (1997) Tumor-related prognostic factors for breast cancer. CA Cancer J Clin 47:28–51. https://doi.org/10.3322/canjclin.47.1.28
Dowsett M, Cuzick J, Wale C, Forbes J, Mallon EA, Salter J, Quinn E, Dunbier A, Baum M, Buzdar A, Howell A, Bugarini R, Baehner FL, Shak S (2010) Prediction of risk of distant recurrence using the 21-gene recurrence score in node-negative and node-positive postmenopausal patients with breast cancer treated with anastrozole or tamoxifen: a TransATAC study. J Clin Oncol 28:1829–1834. https://doi.org/10.1200/JCO.2009.24.4798
Dowsett M, Sestak I, Lopez-Knowles E, Sidhu K, Dunbier AK, Cowens JW, Ferree S, Storhoff J, Schaper C, Cuzick J (2013) Comparison of PAM50 risk of recurrence score with oncotype DX and IHC4 for predicting risk of distant recurrence after endocrine therapy. J Clin Oncol 31:2783–2790. https://doi.org/10.1200/JCO.2012.46.1558
Esteva FJ, Hubbard-Lucey VM, Tang J, Pusztai L (2019) Immunotherapy and targeted therapy combinations in metastatic breast cancer. Lancet Oncol 20:e175–e186. https://doi.org/10.1016/S1470-2045(19)30026-9
Farmer P, Bonnefoi H, Anderle P, Cameron D, Wirapati P, Becette V, Andre S, Piccart M, Campone M, Brain E, Macgrogan G, Petit T, Jassem J, Bibeau F, Blot E, Bogaerts J, Aguet M, Bergh J, Iggo R, Delorenzi M (2009) A stroma-related gene signature predicts resistance to neoadjuvant chemotherapy in breast cancer. Nat Med 15:68–74. https://doi.org/10.1038/nm.1908
Filipits M, Rudas M, Jakesz R, Dubsky P, Fitzal F, Singer CF, Dietze O, Greil R, Jelen A, Sevelda P, Freibauer C, Muller V, Janicke F, Schmidt M, Kolbl H, Rody A, Kaufmann M, Schroth W, Brauch H, Schwab M, Fritz P, Weber KE, Feder IS, Hennig G, Kronenwett R, Gehrmann M, Gnant M (2011) A new molecular predictor of distant recurrence in ER-positive, HER2-negative breast cancer adds independent information to conventional clinical risk factors. Clin Cancer Res 17:6012–6020. https://doi.org/10.1158/1078-0432.CCR-11-0926
Finak G, Bertos N, Pepin F, Sadekova S, Souleimanova M, Zhao H, Chen H, Omeroglu G, Meterissian S, Omeroglu A, Hallett M, Park M (2008) Stromal gene expression predicts clinical outcome in breast cancer. Nat Med 14:518–527. https://doi.org/10.1038/nm1764
Fitzal F, Filipits M, Rudas M, Greil R, Dietze O, Samonigg H, Lax S, Herz W, Dubsky P, Bartsch R, Kronenwett R, Gnant M (2015) The genomic expression test EndoPredict is a prognostic tool for identifying risk of local recurrence in postmenopausal endocrine receptor-positive, her2neu-negative breast cancer patients randomised within the prospective ABCSG 8 trial. Br J Cancer 112:1405–1410. https://doi.org/10.1038/bjc.2015.98
Fridman WH, Pages F, Sautes-Fridman C, Galon J (2012) The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 12:298–306. https://doi.org/10.1038/nrc3245
Gibney GT, Weiner LM, Atkins MB (2016) Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol 17:e542–e551. https://doi.org/10.1016/S1470-2045(16)30406-5
Gingras I, Desmedt C, Ignatiadis M, Sotiriou C (2015) CCR 20th Anniversary Commentary: gene-expression signature in breast cancer-where did it start and where are we now? Clin Cancer Res 21:4743–4746. https://doi.org/10.1158/1078-0432.CCR-14-3127
Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, Weaver DL, Winchester DJ, Hortobagyi GN (2017) Breast cancer—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 67:290–303. https://doi.org/10.3322/caac.21393
Gnant M, Filipits M, Greil R, Stoeger H, Rudas M, Bago-Horvath Z, Mlineritsch B, Kwasny W, Knauer M, Singer C, Jakesz R, Dubsky P, Fitzal F, Bartsch R, Steger G, Balic M, Ressler S, Cowens JW, Storhoff J, Ferree S, Schaper C, Liu S, Fesl C, Nielsen TO, Austrian Breast and Colorectal Cancer Study Group (2014) Predicting distant recurrence in receptor-positive breast cancer patients with limited clinicopathological risk: using the PAM50 Risk of Recurrence score in 1478 postmenopausal patients of the ABCSG-8 trial treated with adjuvant endocrine therapy alone. Ann Oncol 25:339–345. https://doi.org/10.1093/annonc/mdt494
Gong G, Kwon MJ, Han J, Lee HJ, Lee SK, Lee JE, Lee SH, Park S, Choi JS, Cho SY, Ahn SH, Lee JW, Cho SR, Moon Y, Nam BH, Nam SJ, Choi YL, Shin YK (2017) A new molecular prognostic score for predicting the risk of distant metastasis in patients with HR+/HER2− early breast cancer. Sci Rep 7:45554. https://doi.org/10.1038/srep45554
Han J, Choi YL, Kim H, Choi JY, Lee SK, Lee JE, Choi JS, Park S, Choi JS, Kim YD, Nam SJ, Nam BH, Kwon MJ, Shin YK (2017) MMP11 and CD2 as novel prognostic factors in hormone receptor-negative, HER2-positive breast cancer. Breast Cancer Res Treat 164:41–56. https://doi.org/10.1007/s10549-017-4234-4
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674. https://doi.org/10.1016/j.cell.2011.02.013
Harris LN, Ismaila N, Mcshane LM, Andre F, Collyar DE, Gonzalez-Angulo AM, Hammond EH, Kuderer NM, Liu MC, Mennel RG, Van Poznak C, Bast RC, Hayes DF, American Society of Clinical Oncology (2016) Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 34:1134–1150. https://doi.org/10.1200/jco.2015.65.2289
Havel JJ, Chowell D, Chan TA (2019) The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat Rev Cancer 19:133–150. https://doi.org/10.1038/s41568-019-0116-x
Hida AI, Sagara Y, Yotsumoto D, Kanemitsu S, Kawano J, Baba S, Rai Y, Oshiro Y, Aogi K, Ohi Y (2016) Prognostic and predictive impacts of tumor-infiltrating lymphocytes differ between Triple-negative and HER2-positive breast cancers treated with standard systemic therapies. Breast Cancer Res Treat 158:1–9. https://doi.org/10.1007/s10549-016-3848-2
Ignatiadis M, Dawson SJ (2014) Circulating tumor cells and circulating tumor DNA for precision medicine: dream or reality? Ann Oncol 25:2304–2313. https://doi.org/10.1093/annonc/mdu480
Ingold Heppner B, Untch M, Denkert C, Pfitzner BM, Lederer B, Schmitt W, Eidtmann H, Fasching PA, Tesch H, Solbach C, Rezai M, Zahm DM, Holms F, Glados M, Krabisch P, Heck E, Ober A, Lorenz P, Diebold K, Habeck JO, Loibl S (2016) Tumor-infiltrating lymphocytes: a predictive and prognostic biomarker in neoadjuvant-treated HER2-positive breast cancer. Clin Cancer Res 22:5747–5754. https://doi.org/10.1158/1078-0432.CCR-15-2338
Jensen MB, Laenkholm AV, Nielsen TO, Eriksen JO, Wehn P, Hood T, Ram N, Buckingham W, Ferree S, Ejlertsen B (2018) The Prosigna gene expression assay and responsiveness to adjuvant cyclophosphamide-based chemotherapy in premenopausal high-risk patients with breast cancer. Breast Cancer Res 20:79. https://doi.org/10.1186/s13058-018-1012-0
Joyce JA (2005) Therapeutic targeting of the tumor microenvironment. Cancer Cell 7:513–520. https://doi.org/10.1016/j.ccr.2005.05.024
Kandoth C, Mclellan MD, Vandin F, Ye K, Niu B, Lu C, Xie M, Zhang Q, Mcmichael JF, Wyczalkowski MA, Leiserson MDM, Miller CA, Welch JS, Walter MJ, Wendl MC, Ley TJ, Wilson RK, Raphael BJ, Ding L (2013) Mutational landscape and significance across 12 major cancer types. Nature 502:333–339. https://doi.org/10.1038/nature12634
Kwon MJ, Lee SB, Han J, Lee JE, Lee JW, Gong G, Beitsch PD, Nam SJ, Ahn SH, Nam BH, Shin YK (2018) BCT score predicts chemotherapy benefit in Asian patients with hormone receptor-positive, HER2-negative, lymph node-negative breast cancer. PLoS ONE 13:e0207155. https://doi.org/10.1371/journal.pone.0207155
Laenkholm AV, Jensen MB, Eriksen JO, Rasmussen BB, Knoop AS, Buckingham W, Ferree S, Schaper C, Nielsen TO, Haffner T, Kibol T, Moller Talman ML, Bak Jylling AM, Tabor TP, Ejlertsen B (2018) PAM50 risk of recurrence score predicts 10-year distant recurrence in a comprehensive Danish Cohort of postmenopausal women allocated to 5 years of endocrine therapy for hormone receptor-positive early breast cancer. J Clin Oncol 36:735–740. https://doi.org/10.1200/JCO.2017.74.6586
Lee HJ, Lee JJ, Song IH, Park IA, Kang J, Yu JH, Ahn JH, Gong G (2015) Prognostic and predictive value of NanoString-based immune-related gene signatures in a neoadjuvant setting of triple-negative breast cancer: relationship to tumor-infiltrating lymphocytes. Breast Cancer Res Treat 151:619–627. https://doi.org/10.1007/s10549-015-3438-8
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, De Azambuja E, Quinaux E, Di Leo A, Michiels S, Piccart MJ, Sotiriou C (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol 31:860–867. https://doi.org/10.1200/JCO.2011.41.0902
Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, Kellokumpu-Lehtinen PL, Bono P, Kataja V, Desmedt C, Piccart MJ, Loibl S, Denkert C, Smyth MJ, Joensuu H, Sotiriou C (2014) Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 25:1544–1550. https://doi.org/10.1093/annonc/mdu112
Loibl S, Weber K, Huober J, Krappmann K, Marme F, Schem C, Engels K, Pfitzner BM, Kummel S, Furlanetto J, Hartmann A, Darb-Esfahani S, Muller V, Staebler A, Von Minckwitz G, Kronenwett R, Denkert C (2018) Risk assessment after neoadjuvant chemotherapy in luminal breast cancer using a clinicomolecular predictor. Clin Cancer Res 24:3358–3365. https://doi.org/10.1158/1078-0432.CCR-17-2947
Luen SJ, Savas P, Fox SB, Salgado R, Loi S (2017) Tumour-infiltrating lymphocytes and the emerging role of immunotherapy in breast cancer. Pathology 49:141–155. https://doi.org/10.1016/j.pathol.2016.10.010
Ma XJ, Salunga R, Dahiya S, Wang W, Carney E, Durbecq V, Harris A, Goss P, Sotiriou C, Erlander M, Sgroi D (2008) A five-gene molecular grade index and HOXB13:IL17BR are complementary prognostic factors in early stage breast cancer. Clin Cancer Res 14:2601–2608. https://doi.org/10.1158/1078-0432.CCR-07-5026
Mamounas EP, Liu Q, Paik S, Baehner FL, Tang G, Jeong JH, Kim SR, Butler SM, Jamshidian F, Cherbavaz DB, Sing AP, Shak S, Julian TB, Lembersky BC, Wickerham DL, Costantino JP, Wolmark N (2017) 21-Gene recurrence score and locoregional recurrence in node-positive/ER-positive breast cancer treated with chemo-endocrine therapy. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djw259
Mao Y, Keller ET, Garfield DH, Shen K, Wang J (2013) Stromal cells in tumor microenvironment and breast cancer. Cancer Metastasis Rev 32:303–315. https://doi.org/10.1007/s10555-012-9415-3
Martin M, Brase JC, Calvo L, Krappmann K, Ruiz-Borrego M, Fisch K, Ruiz A, Weber KE, Munarriz B, Petry C, Rodriguez CA, Kronenwett R, Crespo C, Alba E, Carrasco E, Casas M, Caballero R, Rodriguez-Lescure A (2014) Clinical validation of the EndoPredict test in node-positive, chemotherapy-treated ER+/HER2− breast cancer patients: results from the GEICAM 9906 trial. Breast Cancer Res 16:R38. https://doi.org/10.1186/bcr3642
Miglietta F, Griguolo G, Guarneri V, Dieci MV (2019) Programmed cell death ligand 1 in breast cancer: technical aspects, prognostic implications, and predictive value. Oncologist. https://doi.org/10.1634/theoncologist.2019-0197
Mittempergher L, De Ronde JJ, Nieuwland M, Kerkhoven RM, Simon I, Rutgers EJ, Wessels LF, Van’t Veer LJ (2011) Gene expression profiles from formalin fixed paraffin embedded breast cancer tissue are largely comparable to fresh frozen matched tissue. PLoS ONE 6:e17163. https://doi.org/10.1371/journal.pone.0017163
Mittempergher L, Saghatchian M, Wolf DM, Michiels S, Canisius S, Dessen P, Delaloge S, Lazar V, Benz SC, Tursz T, Bernards R, Van’t Veer LJ (2013) A gene signature for late distant metastasis in breast cancer identifies a potential mechanism of late recurrences. Mol Oncol 7:987–999. https://doi.org/10.1016/j.molonc.2013.07.006
Nicolini A, Ferrari P, Duffy MJ (2018) Prognostic and predictive biomarkers in breast cancer: past, present and future. Semin Cancer Biol 52:56–73. https://doi.org/10.1016/j.semcancer.2017.08.010
Nielsen T, Wallden B, Schaper C, Ferree S, Liu S, Gao D, Barry G, Dowidar N, Maysuria M, Storhoff J (2014) Analytical validation of the PAM50-based Prosigna Breast Cancer Prognostic Gene Signature Assay and nCounter Analysis System using formalin-fixed paraffin-embedded breast tumor specimens. BMC Cancer 14:177. https://doi.org/10.1186/1471-2407-14-177
Oh E, Choi YL, Park T, Lee S, Nam SJ, Shin YK (2012) A prognostic model for lymph node-negative breast cancer patients based on the integration of proliferation and immunity. Breast Cancer Res Treat 132:499–509. https://doi.org/10.1007/s10549-011-1626-8
Ono M, Tsuda H, Shimizu C, Yamamoto S, Shibata T, Yamamoto H, Hirata T, Yonemori K, Ando M, Tamura K, Katsumata N, Kinoshita T, Takiguchi Y, Tanzawa H, Fujiwara Y (2012) Tumor-infiltrating lymphocytes are correlated with response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Res Treat 132:793–805. https://doi.org/10.1007/s10549-011-1554-7
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351:2817–2826. https://doi.org/10.1056/NEJMoa041588
Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, Costantino JP, Geyer CE Jr, Wickerham DL, Wolmark N (2006) Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 24:3726–3734. https://doi.org/10.1200/JCO.2005.04.7985
Parker JS, Mullins M, Cheang MC, Leung S, Voduc D, Vickery T, Davies S, Fauron C, He X, Hu Z, Quackenbush JF, Stijleman IJ, Palazzo J, Marron JS, Nobel AB, Mardis E, Nielsen TO, Ellis MJ, Perou CM, Bernard PS (2009) Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol 27:1160–1167. https://doi.org/10.1200/JCO.2008.18.1370
Partridge AH, Carey LA (2017) Unmet needs in clinical research in breast cancer: where do we need to go? Clin Cancer Res 23:2611–2616. https://doi.org/10.1158/1078-0432.CCR-16-2633
Prat A, Galvan P, Jimenez B, Buckingham W, Jeiranian HA, Schaper C, Vidal M, Alvarez M, Diaz S, Ellis C, Nuciforo P, Ferree S, Ribelles N, Adamo B, Ramon YCS, Peg V, Alba E (2016) Prediction of response to neoadjuvant chemotherapy using core needle biopsy samples with the Prosigna Assay. Clin Cancer Res 22:560–566. https://doi.org/10.1158/1078-0432.CCR-15-0630
Rody A, Holtrich U, Pusztai L, Liedtke C, Gaetje R, Ruckhaeberle E, Solbach C, Hanker L, Ahr A, Metzler D, Engels K, Karn T, Kaufmann M (2009) T-cell metagene predicts a favorable prognosis in estrogen receptor-negative and HER2-positive breast cancers. Breast Cancer Res 11:R15. https://doi.org/10.1186/bcr2234
Rody A, Karn T, Liedtke C, Pusztai L, Ruckhaeberle E, Hanker L, Gaetje R, Solbach C, Ahr A, Metzler D, Schmidt M, Muller V, Holtrich U, Kaufmann M (2011) A clinically relevant gene signature in triple negative and basal-like breast cancer. Breast Cancer Res 13:R97. https://doi.org/10.1186/bcr3035
Ross JS, Hatzis C, Symmans WF, Pusztai L, Hortobagyi GN (2008) Commercialized multigene predictors of clinical outcome for breast cancer. Oncologist 13:477–493. https://doi.org/10.1634/theoncologist.2007-0248
Salgado R, Denkert C, Campbell C, Savas P, Nuciforo P, Aura C, De Azambuja E, Eidtmann H, Ellis CE, Baselga J, Piccart-Gebhart MJ, Michiels S, Bradbury I, Sotiriou C, Loi S (2015a) Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO Trial. JAMA Oncol 1:448–454. https://doi.org/10.1001/jamaoncol.2015.0830
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van Den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S, International TILs Working Group (2015b) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26:259–271. https://doi.org/10.1093/annonc/mdu450
Savas P, Salgado R, Denkert C, Sotiriou C, Darcy PK, Smyth MJ, Loi S (2016) Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol 13:228–241. https://doi.org/10.1038/nrclinonc.2015.215
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, Dieras V, Hegg R, Im SA, Shaw Wright G, Henschel V, Molinero L, Chui SY, Funke R, Husain A, Winer EP, Loi S, Emens LA, Investigators IMT (2018) Atezolizumab and Nab-Paclitaxel in advanced triple-negative breast cancer. N Engl J Med 379:2108–2121. https://doi.org/10.1056/NEJMoa1809615
Schmidt M, Bohm D, Von Torne C, Steiner E, Puhl A, Pilch H, Lehr HA, Hengstler JG, Kolbl H, Gehrmann M (2008) The humoral immune system has a key prognostic impact in node-negative breast cancer. Cancer Res 68:5405–5413. https://doi.org/10.1158/0008-5472.CAN-07-5206
Sestak I, Cuzick J, Dowsett M, Lopez-Knowles E, Filipits M, Dubsky P, Cowens JW, Ferree S, Schaper C, Fesl C, Gnant M (2015) Prediction of late distant recurrence after 5 years of endocrine treatment: a combined analysis of patients from the Austrian breast and colorectal cancer study group 8 and arimidex, tamoxifen alone or in combination randomized trials using the PAM50 risk of recurrence score. J Clin Oncol 33:916–922. https://doi.org/10.1200/JCO.2014.55.6894
Sestak I, Buus R, Cuzick J, Dubsky P, Kronenwett R, Denkert C, Ferree S, Sgroi D, Schnabel C, Baehner FL, Mallon E, Dowsett M (2018) Comparison of the performance of 6 prognostic signatures for estrogen receptor-positive breast cancer: a secondary analysis of a Randomized Clinical Trial. JAMA Oncol 4:545–553. https://doi.org/10.1001/jamaoncol.2017.5524
Sgroi DC, Sestak I, Cuzick J, Zhang Y, Schnabel CA, Schroeder B, Erlander MG, Dunbier A, Sidhu K, Lopez-Knowles E, Goss PE, Dowsett M (2013) Prediction of late distant recurrence in patients with oestrogen-receptor-positive breast cancer: a prospective comparison of the breast-cancer index (BCI) assay, 21-gene recurrence score, and IHC4 in the TransATAC study population. Lancet Oncol 14:1067–1076. https://doi.org/10.1016/S1470-2045(13)70387-5
Sgroi DC, Chapman JA, Badovinac-Crnjevic T, Zarella E, Binns S, Zhang Y, Schnabel CA, Erlander MG, Pritchard KI, Han L, Shepherd LE, Goss PE, Pollak M (2016) Assessment of the prognostic and predictive utility of the Breast Cancer Index (BCI): an NCIC CTG MA.14 study. Breast Cancer Res 18:1. https://doi.org/10.1186/s13058-015-0660-6
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Perez EA, Olson JA Jr, Zujewski J, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Ravdin P, Keane MM, Gomez Moreno HL, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Atkins JN, Berenberg JL, Sledge GW (2015) Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med 373:2005–2014. https://doi.org/10.1056/NEJMoa1510764
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Goetz MP, Olson JA Jr, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Ravdin PM, Keane MM, Gomez Moreno HL, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Berenberg JL, Abrams J, Sledge GW Jr (2018) Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med 379:111–121. https://doi.org/10.1056/NEJMoa1804710
Sparano JA, Gray RJ, Ravdin PM, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Goetz MP, Olson JA Jr, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Keane MM, Gomez Moreno HL, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Berenberg JL, Abrams J, Sledge GW Jr (2019) Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N Engl J Med 380:2395–2405. https://doi.org/10.1056/NEJMoa1904819
Teschendorff AE, Caldas C (2008) A robust classifier of high predictive value to identify good prognosis patients in ER-negative breast cancer. Breast Cancer Res 10:R73. https://doi.org/10.1186/bcr2138
Teschendorff AE, Miremadi A, Pinder SE, Ellis IO, Caldas C (2007) An immune response gene expression module identifies a good prognosis subtype in estrogen receptor negative breast cancer. Genome Biol 8:R157. https://doi.org/10.1186/gb-2007-8-8-r157
Tian S, Roepman P, Van’t Veer LJ, Bernards R, De Snoo F, Glas AM (2010) Biological functions of the genes in the mammaprint breast cancer profile reflect the hallmarks of cancer. Biomark Insights 5:129–138. https://doi.org/10.4137/BMI.S6184
Tsai M, Lo S, Audeh W, Qamar R, Budway R, Levine E, Whitworth P, Mavromatis B, Zon R, Oldham D, Untch S, Treece T, Blumencranz L, Soliman H (2018) Association of 70-gene signature assay findings with physicians’ treatment guidance for patients with early breast cancer classified as intermediate risk by the 21-gene assay. JAMA Oncol 4:e173470. https://doi.org/10.1001/jamaoncol.2017.3470
Tsang JY, Hui SW, Ni YB, Chan SK, Yamaguchi R, Kwong A, Law BK, Tse GM (2014) Lymphocytic infiltrate is associated with favorable biomarkers profile in HER2-overexpressing breast cancers and adverse biomarker profile in ER-positive breast cancers. Breast Cancer Res Treat 143:1–9. https://doi.org/10.1007/s10549-013-2781-x
Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, Chmielowski B, Spasic M, Henry G, Ciobanu V, West AN, Carmona M, Kivork C, Seja E, Cherry G, Gutierrez AJ, Grogan TR, Mateus C, Tomasic G, Glaspy JA, Emerson RO, Robins H, Pierce RH, Elashoff DA, Robert C, Ribas A (2014) PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515:568–571. https://doi.org/10.1038/nature13954
Van ‘t Veer LJ, Dai H, Van De Vijver MJ, He YD, Hart AA, Mao M, Peterse HL, Van Der Kooy K, Marton MJ, Witteveen AT, Schreiber GJ, Kerkhoven RM, Roberts C, Linsley PS, Bernards R, Friend SH (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature 415:530–536. https://doi.org/10.1038/415530a
Varga Z, Sinn P, Seidman AD (2019) Summary of head-to-head comparisons of patient risk classifications by the 21-gene Recurrence Score(R) (RS) assay and other genomic assays for early breast cancer. Int J Cancer 145:882–893. https://doi.org/10.1002/ijc.32139
Vonderheide RH, Domchek SM, Clark AS (2017) Immunotherapy for breast cancer: what are we missing? Clin Cancer Res 23:2640–2646. https://doi.org/10.1158/1078-0432.CCR-16-2569
Wallden B, Storhoff J, Nielsen T, Dowidar N, Schaper C, Ferree S, Liu S, Leung S, Geiss G, Snider J, Vickery T, Davies SR, Mardis ER, Gnant M, Sestak I, Ellis MJ, Perou CM, Bernard PS, Parker JS (2015) Development and verification of the PAM50-based Prosigna breast cancer gene signature assay. BMC Med Genomics 8:54. https://doi.org/10.1186/s12920-015-0129-6
Winslow S, Lindquist KE, Edsjo A, Larsson C (2016) The expression pattern of matrix-producing tumor stroma is of prognostic importance in breast cancer. BMC Cancer 16:841. https://doi.org/10.1186/s12885-016-2864-2
Yang B, Chou J, Tao Y, Wu D, Wu X, Li X, Li Y, Chu Y, Tang F, Shi Y, Ma L, Zhou T, Kaufmann W, Carey LA, Wu J, Hu Z (2018) An assessment of prognostic immunity markers in breast cancer. NPJ Breast Cancer 4:35. https://doi.org/10.1038/s41523-018-0088-0
Yarchoan M, Albacker LA, Hopkins AC, Montesion M, Murugesan K, Vithayathil TT, Zaidi N, Azad NS, Laheru DA, Frampton GM, Jaffee EM (2019) PD-L1 expression and tumor mutational burden are independent biomarkers in most cancers. JCI Insight. https://doi.org/10.1172/jci.insight.126908
Yau C, Esserman L, Moore DH, Waldman F, Sninsky J, Benz CC (2010) A multigene predictor of metastatic outcome in early stage hormone receptor-negative and triple-negative breast cancer. Breast Cancer Res 12:R85. https://doi.org/10.1186/bcr2753
Yau C, Sninsky J, Kwok S, Wang A, Degnim A, Ingle JN, Gillett C, Tutt A, Waldman F, Moore D, Esserman L, Benz CC (2013) An optimized five-gene multi-platform predictor of hormone receptor negative and triple negative breast cancer metastatic risk. Breast Cancer Res 15:R103. https://doi.org/10.1186/bcr3567
Zhang Y, Schnabel CA, Schroeder BE, Jerevall PL, Jankowitz RC, Fornander T, Stal O, Brufsky AM, Sgroi D, Erlander MG (2013) Breast cancer index identifies early-stage estrogen receptor-positive breast cancer patients at risk for early- and late-distant recurrence. Clin Cancer Res 19:4196–4205. https://doi.org/10.1158/1078-0432.CCR-13-0804
Acknowledgements
This research was supported by the Basic Science Research Program through the National Research Foundation of a Korea (NRF) funded by the Ministry of Education (Grant Number: NRF-2018R1D1A1B07043031).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kwon, M.J. Emerging immune gene signatures as prognostic or predictive biomarkers in breast cancer. Arch. Pharm. Res. 42, 947–961 (2019). https://doi.org/10.1007/s12272-019-01189-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12272-019-01189-y