Abstract
Many benign breast lesions in the Breast Imaging Reporting and Data System (BI-RADS) 4 category defined by ultrasonography (US) undergo unnecessary biopsies. This study aims to investigate the efficiency of acoustic radiation for impulse elastography (ARFI) in diagnosing BI-RADS 4 breast lesions. The ARFI elastography technique was utilized to assess the lesions both qualitatively and quantitatively. By using quantitative elastography measurement, we found that the shear wave velocity (SWV) of BI-RADS 4a lesions was significantly lower compared to the SWV of BI-RADS 4b and 4c lesions (p = 0.00). In qualitative evaluation, pattern 1 only defined benign lesions, and a negative predictive value (NPV) of 100% was obtained. Using quantitative, qualitative and combined methods, the Likelihood ratios was determined to be 1.81, 2.8 and 4.7 respectively. In addition to the ultrasound examination of BI-RADS 4 lesions, the addition of combined elastography assessment increases the accuracy of BI-RADS. BI-RADS 4a lesions can be followed in a similar way as BI-RADS 3 lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Conventional US plays an essential role in breast cancer screening and the differential diagnosis of breast lesions [1]. BI-RADS category 4 lesions are associated with malignancy, and malignancy rates are highly variable (2–94%). Lesions in BI-RADS category 4 are classified as 4a, 4b, or 4c based on their malignancy risk [2, 3]. B-mode US findings lack specificity for biopsy indication, leading to unnecessary biopsies of benign breast lesions and anxiety in patients [2, 4]. Breast radiologists have a major problem in reducing unnecessary biopsies and increasing US specificity and positive predictive value (PPV) without missing breast cancer in BI-RADS 4 lesions.
Malignant breast lesions are often stiffer than benign masses, with tissue stiffness measurement aiding in differentiation [5]. ARFI imaging is a non-invasive technique used to assess tissue stiffness, aiding in the detection of breast cancer [6]. ARFI utilizes two modes for assessing tissue stiffness: virtual touch tissue quantification (VTTQ) and virtual touch tissue imaging (VTTI) [7]. Both quantitative and qualitative evaluation can be achieved through these two modes. The VTTI method effectively demonstrates the desmoplastic reaction surrounding malignant lesions [6].
Combining quantitative and qualitative ARFI elastography methods can prevent false positives in BI-RADS 4a and 4b lesions by showing desmoplastic features and stiffness of the lesions. Our study aims to evaluate the effectiveness of these methods in reducing unnecessary biopsies without missing false-negative cases.
Patients and Methods
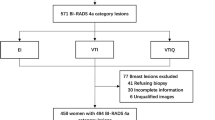
Ethical approval was waived for this retrospective study. A total of 260 breast lesions were reviewed, with confirmed histopathology, using the Picture Archiving and Communication Systems (PACS) archive of the breast radiology unit from January 2019 to June 2020. The breast lesions were classified according to the BI-RADS US system. The study included only lesions that were smaller than 3 cm in size. A total of 170 patients and 170 BI-RADS 4 breast lesions were included in the study. Excluded from the study were masses that could give false results in ultrasound elastography (UE), such as mucinous cancer, idiopathic granulomatous mastitis, other mastitis, ductal carcinoma in situ, complex cysts, galactocele, and fat necrosis.
US-UE Examination
The radiologist with five years of experience in breast radiology and UE performed the US-UE lesion sampling. During the examination, a bandwidth of 14 MHz linear array transducer was used for B-mode US, while a bandwidth of 9 MHz linear array transducer was used for elastography. All lesions underwent US-guided cutting needle biopsy using a 14G fully automatic biopsy gun, and histopathological results were obtained. While analyzing the study data, breast US and UE images recorded in the PACS before the biopsy were re-evaluated by another radiologist. The other radiologist who examined the patient's US and UE images was not aware of the results of the histopathological analysis. Lesions were categorized as BI-RADS 4a, 4b, or 4c based on echo pattern, shape, margin, posterior acoustic features, and the presence of microcalcification. The US findings at lesions, similar to the literature, were classified as minor (round shape, microlobulation, indistinct margin, angular contour, non-parallel orientation, ductal extension, heterogeneous echo pattern, posterior shadowing) and major findings (irregular shape, spiculated contour, and microcalcifications) [4]. The presence of 1–3 minor criteria indicates BI-RADS 4a, > 3 minor criteria indicate BI-RADS 4b, and one major ± one minor criterion indicates BI-RADS 4c subgroup [5]. The BI-RADS 4a, 4b, and 4c classifications have been standardized using objective criteria. This ensured that the classification was uniform and consistent across all breast lesions in US.Both qualitative (VTTI; Siemens) and quantitative (VTTQ; Siemens) examinations were applied to the elastography assessment. The same imaging parameters were used for all elastography measurements, and the "breast" imaging mode was employed. The US probe was affixed to the skin using gel, and no pressure was applied to the skin. A split-screen display mode was used to obtain B-mode US and shear wave elastography (SWE) images of the same area. The patients were instructed to hold their breath during SWE imaging. The lesion was visible in grayscale on the right split-screen. A grayscale map indicating tissue stiffness in the region of interest (ROI) was generated using the VTTI mechanism. At VTTI, the lesions were categorized based on their attributes and appearance. An evaluation was conducted to compare the lesions observed on qualitative elastography images with those on the B-mode images. The lesions were categorized into four patterns: Pattern 1 indicated the absence of any findings on elastography images. Pattern 2 indicated the presence of a bright (i.e., soft) area. Pattern 3 indicated the presence of both bright (i.e., soft) and dark (i.e., stiff) areas. Pattern 4 indicated the complete absence of brightness (i.e., stiffness). Lesions in pattern 4 were subclassified as 4a if equal to B-mode US size and 4b if smaller. Visually compared lesion size between ARFI elastographic and B-mode images to classify as pattern 4a or 4b. Lesions with patterns 1–3 were considered benign, and lesions with patterns 4a-b were deemed malignant [6, 8]. The VTTQ method measured shear wave velocity (SWV) of breast lesions by placing a 5 × 5 mm ROI in the center of the lesion. The system was not able to measure SWV's greater than 10 m/s. Taking into account other studies, the optimal SWV cut-off value was obtained to ensure adequate sensitivity and specificity [9].
Statistical Analysis
The Statistical Package for the Social Sciences software version 13.0 (SPSS Inc., Chicago, IL, USA) was used to perform all statistical analyses. Descriptive statistics are means, standard deviations, and minimum and maximum values. The independent samples t-test was used to analyze the significant difference in SWV between benign and malignant lesions. The one-way ANOVA test was used to compare SWV values of BI-RADS 4 subgroups. To test the intergroup significance of SWV values in BI-RADS 4 subgroups, the homogeneity of variances was tested with the Levene statistic. Receiver operating characteristic (ROC) curves were established to determine the diagnostic performance of VTTI, VTTQ, and their combinations. The area under the receiver operating characteristic (AUROC), sensitivity, specificity, accuracy, PPV, and negative predictive value (NPV) were calculated. Cohen’s kappa statistic was performed to evaluate the agreement between the observations of 2 different radiologists for B-mode US and VTTI elastography results.
Results
There were 93 (54.7%) benign and 77 (45.3%) malignant lesions. The mean age was 35.8 SD12.7 years in patients with benign lesions and 49.07 SD13.14 years in patients with malignant lesions (p < 0.05). The mean lesion diameter was 21.16 SD10.52 mm and 19.77 SD8.9 mm in benign and malignant lesions, respectively. The malignancy rates for BI-RADS 4a, 4b, and 4c lesions were 7.1%, 48.1%, and 77.4%, respectively. When considering BI-RADS 4 lesions as malignant, the PPV was found to be 45%. Fibroadenoma was the most common diagnosis in BI-RADS categories 4a and 4b, while invasive ductal carcinoma (IDC) was the most common in BI-RADS category 4c (Table 1). On elastography, the mean SWV value was 2.90 SD0.86 m/s and 4.34 SD1.41 m/s for benign and malignant lesions, respectively (p = 0.001). It has observed that malignant lesions have a significantly higher SWV value compared to benign lesions. When evaluating the lesions with VTTI, we categorized the images into five different patterns: patterns 1, 2, 3, 4a, and 4b. Patterns 1, 2, and 3 were considered a descriptor of benignity, while patterns 4a and 4b were considered a descriptor of malignancy. Pattern 1 was only observed in benign lesions (Fig. 1), and its NPV was 100%. Pattern 2 described cystic lesions. The lesion (Fig. 2), previously categorized as BI-RADS 4b and appearing solid on ultrasound, was identified as a galactocele on histopathological examination, with a corresponding pattern 2 category on VTTI. Pattern 3 was observed in 5 (6.5%) malignant lesions and 37 (40.7%) benign lesions. Malignant lesions were found to predominantly exhibit pattern 4b, accounting for 85.7% of cases (p < 0.05) (Fig. 3). The most common patterns on VTTI for sclerosing adenosis were pattern 3 (61.1%) and pattern 4a (33.3%), which were also the stiffest benign lesions (Fig. 4) (Table 2).
In a 25-year-old patient, BI-RADS category 4a breast lesion's US, elastography and histopathological appareance. a In the US findings of parallel orientation, regular shape, and smooth margin feature (left), and VTTI elastography revealed a Pattern 1 (right). b VTTQ elastography imaging showed low stiffness (SWV 1.6 m/s). c Histopathological examination confirmed the diagnosis of fibroadenoma (H&E X200)
In a 49-year-old patient with a BI-RADS 4c breast lesion's US, elastography and histopathological appareance. a In US findings of the lesion a round-irregular shape spiculated margin feature (left), and VTTI elastography revealed Pattern 4b (right). b VTTQ elastography imaging showed high stiffness (SWV 4.67 m/s). c Pathological examination confirmed invasive ductal carcinoma of grade II (H&E X200)
In a 28-year-old patient with a BI-RADS 4b breast lesion's US, elastography appareance. a In US findings of the lesion a non-parallel orientation, regular shape, and smooth margin feature (left), and VTTI elastography revealed pattern 4a (right). b VTTQ elastography revealed low stiff lesion (SWV 0.54 m/s). c Pathological examination confirmed sclerosing adenosis (H&E X200)
The one-way ANOVA revealed a significant difference in SWV values among BI-RADS 4 subgroups (p = 0.00). The post-hoc Bonferroni test was used to compare SWV between BI-RADS 4 subgroups. Results showed a significant difference in SWV between BI-RADS 4a lesions and BI-RADS 4b/c lesions (p = 0.00). There was no significant difference in SWV values observed between BI-RADS 4b and 4c lesions (p > 0.05) as shown in Table 3. After determining the optimal cut-off value of 3.05 m/s for SWV on VTTQ, the sensitivity, specificity, PPV, NPV, and accuracy for BI-RADS 4 lesions were calculated to be 89%, 51%, 60%, 85%, and 68%, respectively. The area under the receiver operating characteristic (AUROC) curve for VTTQ was 0.80 (95% confidence interval [CI], 0.73–0.86), as shown in Table 4.
After being found the optimal cut-off value of pattern 3 on VTTQ, the sensitivity, specificity, PPV, NPV, and accuracy for all BI-RADS 4 lesions were 94%, 66%, 70%, 93%, and 79%, respectively. Table 4 shows that VTTI had an AUROC of 0.86 (95% CI: 0.81–0.92). The Likelihood ratios was 1.81, 2.8, and 4.7 for VTTQ, VTTI, and VTTQ + VTTI, respectively. The highest sensitivity, specificity, PPV, NPV, accuracy, and + LR ratios were obtained when VTTQ and VTTI applications were both (p = 0.01) (Fig. 5, Table 4). In the VTTQ assessment, the optimal cut-off value of SWV for BI-RADS 4a lesions was determined to be 3.6 m/s. At this cut-off value, the test exhibited 100% sensitivity, 83% specificity, 44% PPV, 100% NPV, and 91% accuracy. When the VTTI cut-off value was set to pattern 3, the combination of VTTQ + VTTI had high accuracy, sensitivity, specificity, PPV, NPV, and Likelihood ratios in predicting malignancy of BI-RADS 4a lesions [AUROC, (0.97(0.92–100)] (Table 4). When assessing BI-RADS 4a lesions with elastography added to B-mode US, no false-negative malignant lesions were found. The agreement rate for the B-mode US examination was 0.956 (p = 0.001) and for the VTTI evaluation of the lesions was 0.865 (p = 0.001). The agreement rate was not analyzed for VTTQ because it is a numerical value.
Discussion
Our study found that incorporating VTTQ and VTTI called combined elastography with B-mode ultrasound of the breast can enhance the accuracy of diagnosis when evaluating BI-RADS 4a and 4b lesions. The highest AUROC value in our study was achieved with the use of combined elastography techniques. Combined elastography achieved highest sensitivity, specificity, PPV, NPV, and Likelihood ratios.
Studies suggest that BI-RADS 4a lesions can be downgraded with elastography and monitored similarly to BI-RADS 3 [10]. In our study, the SWV values were significantly lower for BI-RADS 4a lesions compared to BI-RADS 4b and 4c lesions. Assessment of BI-RADS 4a lesions using VTTQ elastography achieved high sensitivity and NPV values. However, the sensitivity, specificity, PPV, Likelihood ratios, and AUROC values for VTTI and combined elastography were higher than those for VTTQ alone. Studies show that VTTQ evaluation can yield high SWV values in both benign and malignant lesions [11]. This inverse situation may decrease the specificity of VTTQ elastography. According to the findings of our study, the highest sensitivity and specificity values were obtained when the optimal cut-off value for SWV was accepted as 3.6 m/s in BI-RADS 4a lesions. Based on these findings, using a higher SWV cut-off value for BI-RADS 4a lesions than the BI-RADS 4b-c category lesions improves the diagnostic accuracy of elastography and reduces false positives.
Our study found no false-negative findings in BI-RADS 4a lesions. Therefore, Including elastography in the evaluation of BI-RADS 4a category lesions enables a follow-up plan similar to BI-RADS 3 to be implemented. In particular, the VTTI assessment revealed no malignant lesions with pattern 1, and NPV was found to be 100% for lesions with pattern 1. Our study has found that Pattern 1 is solely linked with benignity. The literature suggests that BI-RADS 4 category breast lesions with Pattern 1 in VTTI may be monitored as BI-RADS 3. This means that such lesions may not necessarily require biopsy and can be safely followed up [10].
Using elastography to assess BI-RADS category 4b lesions improved diagnostic accuracy compared to B-mode US alone. However, two cases of invasive cancer with BI-RADS 4b categorization were mistakenly interpreted as benign at elastography. In our study, combining elastography with BI-RADS 4b increased the PPV for malignancy prediction from 48 to 72%. However, it is important to note that the use of elastography in assessing malignant lesions with BI-RADS 4b appearance can result in inaccurate benign results. Therefore, B-mode US findings should be given priority when deciding to perform a biopsy on these lesions.
Sclerosing adenosis is benign hypertrophy of a lobule with fibrotic hypertrophy of the surrounding connective tissue. It appears as a nodule with micro-lobulated margins and indistinct contour on US. The nodule may have angular and irregular margins simulating carcinoma due to significant fibrosis [11]. It has been reported in the literature that the stiffness value of the UE is an effective way to differentiate between sclerosing adenosis and malignant lesions [12]. We found a lower SWV value for sclerosing adenosis compared to malignant lesions, consistent with existing literature. However, in VTTI, patterns 3 and 4a were observed more frequently in these lesions. Our findings were insufficient to include sclerosing adenosis lesions in the BI-RADS 3 category. Therefore, elastography findings of sclerosing adenosis lesions resembling malignancy on the B-mode US due to peripheral fibrosis could not prevent us from performing a biopsy for these lesions.
On SWE images, the stiff-rim sign is defined as the stiffness of the breast tissue surrounding the lesion. It indicates the desmoplastic reaction in the peritumoral region of the lesion, and the stiff-rim sign that appears between the tumoral lesion and the surrounding breast tissue may indicate malignancy [13]. A study on the multimodal US in BI-RADS 4 lesions reported a 79.5% sensitivity and a 93.2% specificity of the stiff-rim sign for malignant lesions [13]. The other study found a 98.2% sensitivity and a 72.3% specificity when quantitative and qualitative elastography were added to the conventional US, while the sensitivity and specificity were 98.2% and 92.0%, respectively, with the addition of the stiff-rim sign. The stiff-rim sign did not alter the sensitivity, but it did improve the specificity [14]. On ARFI-VTTI elastography, the stiff-rim sign can be defined with pattern 4b [6]. Our study showed that detecting pattern 4b on VTTI is a reliable predictor of malignancy, with a sensitivity and specificity of 92% and 91%, respectively. A meta-analysis of 25 articles, with 5.147 breast lesions, found a 41.1% decrease in unnecessary biopsies when SWE was combined with B-mode US [15]. In our study when we used combined elastography only for BI-RADS 4a lesions, the unnecessary biopsy rate decreased by 46%. Although elastography can reduce unnecessary breast biopsies, its limited accessibility due to the high cost of sonography machines equipped with elastography remains a challenge.
Our study's most significant limitation is that it has a retrospective design. Another limitation is that we did not include medullary cancer or lesions that metastasize to the breast that can often be well-circumscribed, which resemble benign lesions in the US. In addition, they may not show the peripheral desmoplastic reaction and may exhibit low stiffness on elastography [11]. Therefore, It is important to be cautious about possible malignancy when evaluating newly discovered lesions during routine breast check-ups.
Conclusion
This study highlights the importance of utilizing both applications for optimal results. With this, combining US and UE modalities can significantly reduce the risk of missing malignancy, and unnecessary biopsies applications, particularly for BI-RADS category 4a lesions. This radiological approach can narrow the range of malignancy prediction in BI-RADS 4 lesions, and accelerate workflow in breast radiology units while preventing patient anxiety.
References
Moon HJ, Jung I, Park SJ, Kim MJ, Youk JH, Kim EK (2015) Comparison of cancer yields and diagnostic performance of screening mammography vs. supplemental screening ultrasound in 4394 women with average risk for breast cancer. Ultraschall Med 36:255–263
Spinelli Varella MA, Teixeira da Cruz J, Rauber A, Varella IS, Fleck JF, Moreira LF (2018) Role of BI-RADS Ultrasound Subcategories 4A to 4C in Predicting Breast Cancer. Clin Breast Cancer 18:505–511
D’Orsi CJ, Bassett LW, Berg WA (2003) Breast Imaging Reporting and Data System, BI-RADS: Mammography, 4th edn. American College of Radiology, Reston, VA
Kim EK, Ko KH, Oh KK, Kwak JY, You JK, Kim MJ (2008) Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol 190:1209–1215
Nightingale K, Soo MS, Nightingale R, Trahey G (2002) Acoustic radiation force impulse imaging: In vivo demonstration of clinical feasibility. Ultrasound Med Biol 28:227–235
Tozaki M, Isobe S, Sakamoto M (2012) Combination of elastography and tissue quantification using the acoustic radiation force impulse (ARFI) technology for differential diagnosis of breast masses. Jpn J Radiol 30:659–670
You QQ, Xu M, Yao MH, Xu G, Liu H, Pu H et al (2018) Diagnostic value of acoustic radiation force impulse for BI-RADS category 4 breast lesions of different sizes. Clin Hemorheol Microcirc 70:143–154
Wang L, Wan CF, Du J, Li FH (2018) Preliminary results of acoustic radiation force impulse imaging by combined qualitative and quantitative analyses for evaluation of breast lesions. J Ultrasound Med 37:2405–2412
Han J, Li F, Peng C, Huang Y, Lin Q, Liu Y et al (2019) Reducing unnecessary biopsy of breast lesions: preliminary results with combination of strain and shear-wave elastography. Ultrasound Med Biol 45:2317–2327
Tozaki M, Isobe S, Fukuma E (2011) Preliminary study of ultrasonographic tissue quantification of the breast using the acoustic radiation force impulse (ARFI) technology. Eur J Radiol 80:182–187
Jalaguier-Coudray A, Thomassin-Piana J (2014) Solid masses: what are the underlying histopathological lesions? Diagn Interv Imaging 95:153–168
Liu W, Li W, Li Z, Shi L, Zhao P, Guo Z et al (2020) Ultrasound characteristics of sclerosing adenosis mimicking breast carcinoma. Breast Cancer Res Treat 181:127–134
Liu G, Zhang MK, He Y, Liu Y, Li XR, Wang ZL (2019) BI-RADS 4 breast lesions: could multi-mode ultrasound be helpful for their diagnosis? Gland Surg 8:258–270
Zhou J, Zhan W, Chang C, Zhang X, Jia Y, Dong Y et al (2014) Breast lesions: evaluation with shear wave elastography, with special emphasis on the “stiff rim” sign. Radiology 272:63–72
Park SY, Kang BJ (2021) Combination of shear-wave elastography with ultrasonography for detection of breast cancer and reduction of unnecessary biopsies: a systematic review and meta-analysis. Ultrasonography 40:318–332
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
All procedures performed in studies involving human participants were following the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was waived due to the retrospective nature of the study.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toprak, N., Yokus, A., Gunduz, A.M. et al. The Role of Elastography in Reducing Unnecessary Biopsies in BI-RADS 4a and 4b Breast Lesions. Indian J Surg (2023). https://doi.org/10.1007/s12262-023-04001-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-023-04001-w