Abstract
The number of surgeries performed in the super-elderly population has increased annually with improvements in medical technology. Recently, the outcomes of colorectal cancer surgery in patients aged > 90 years have been reported. We retrospectively examined 44 nonagenarian patients who had undergone colorectal cancer surgery at our hospital from July 2007 to April 2021. The median age of the patients was 91.0 years (range, 90–97 years) and the male:female ratio was 21:23. The lesion site was C/A/T/D/S/R in 8/11/10/4/7/4 cases, respectively. The ratio of laparotomy to laparoscopic surgery was 10:34, median operation time was 172 min (range, 92–317 min), and median intraoperative bleeding volume was 20 ml (range, 10–302 ml). The dissection range was D1/2/3 in 9/22/13 cases, respectively, and in 79.5% of cases, dissection of D2 or higher could be performed. Clavian–Dindo classification Grade II or higher complications were observed in five cases (11.3%). Recurrence was observed in 6 of 42 cases, excluding 2 cases of stage IV disease (liver: 3 cases, lung: 3 cases, and peritoneal dissemination: 1 case). The median observation period was 30.5 months, and four deaths occurred from primary disease. Examination of factors influencing complications revealed that a history of ischemic heart disease may increase the incidence of complications following surgery. With sufficient preoperative evaluation, colorectal cancer surgery may be performed safely, even in nonagenarian patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, medical technology has improved, while population aging has rapidly progressed worldwide. According to the United Nations statistics in 2015, 0.8% of the population in developed countries is over 90 years old [1]. These individuals are considered super-elderly, and it is normal for medical care in this group to gradually change. The number of operations performed in the super-elderly has increased annually, and recently, the outcomes of surgery in this population group have been reported. In the future, as the global population ages, the age at which surgery is performed will increase. Thus, the safety of surgical procedures for the super-elderly is of great interest.
Aging is a major risk factor for colorectal cancer, which is the third most common malignant tumor among adults [2]. The incidence of colorectal cancer increases with age, with a median age of diagnosis being approximately 70 years [3]. Colorectal cancer accounts for > 20% of cancer cases among individuals aged over 90 years and is a significant cause of death in the super-elderly. As it progresses, this disease causes stenosis and bleeding; therefore, surgical treatment is required, even in the super-elderly. Regarding resectable colorectal cancer, whether it can be curatively resected by surgery has an impact on the survival rate; thus, surgical treatment is desirable even for the super-elderly.
In general, the super-elderly often have decreased organ reserve and more comorbidities, which significantly impact the prognosis once postoperative complications become severe. Furthermore, the super-elderly population is more likely to die from other diseases, even if they are treated for a fatal disease; therefore, an increase in life expectancy resulting from treatment is small and may not contribute to long-term prognosis. However, withholding appropriate disease management and treatment against the will of the patient because of aging and cognitive decline is problematic. Moreover, aging itself is not considered a prognostic factor for gastrointestinal surgery in cases without significant comorbidity [4]. With recent improvement in perioperative management and establishment of laparoscopic colorectal cancer surgery, surgery can be performed safely, even in the super-elderly, who often have comorbidities.
In the super-elderly, devising an appropriate treatment strategy and taking measures against complications in consideration of curative treatment and decline in the function of major organs are necessary. Therefore, this study aimed to examine the safety of colorectal cancer surgery in super-elderly patients, including factors for postoperative complications. We also evaluated the outcomes of surgery for colorectal cancer in the super-elderly.
Patients and Methods
This study was approved by the Clinical Research Institutional Review Board of Saitama Medical University International Medical Center (approval no. 2021–204) and was performed in accordance with the 1964 Declaration of Helsinki and its later amendments or specified comparable standards.
We retrospectively examined the background, surgical results, and prognosis of 44 patients aged ≥ 90 years who had undergone colorectal cancer surgery from July 2007 to April 2021 at our hospital.
EZR was used for all statistical analyses [5]. EZR is statistical software that extends the functionality of R and R Commander. Chi-square test was used for the univariate analysis of factors affecting complications. Logistic regression analysis was used for multivariate analysis. P-values of ≤ 0.05 were considered statistically significant.
Results
Patient characteristics are shown in Table 1. The median age of the patients was 91.0 years (range, 90–97 years). Among the 44 patients, 21 were males and 23 were females. The median BMI was 21.1 kg/m2, which was considered relatively lean in many cases. Most cases had ASA 2, whereas only three patients had ASA 3. The most common tumor sites were the ascending colon (n = 11 cases), followed by the descending colon (n = 10 cases) and cecum (n = 8 cases). Only two cases were stage IV with distant metastases. Laparotomy was performed in only 10 cases, whereas laparoscopic surgery was performed in 34 cases (77.2%). Laparotomy was the most common sigmoid resection technique (n = 4 cases), and laparoscopic surgery was the most common ileocecal resection technique (n = 13 cases) (Table 2). The surgical results are summarized in Table 3. The median operation time was 172 min (range, 92–317 min), and the median intraoperative bleeding volume was 20 ml. The dissection range was D2 in 22 cases and D3 in 13 cases. In 35 cases (79.5%), lymph node dissection of D2 or higher was performed. In addition, R0 surgery was feasible in 41 cases (93.2%). Clavian–Dindo classification Grade II or higher complications were observed in 5 of the 44 cases (11.3%), including pneumonia in 2 cases, postoperative bleeding in 1 case, stoma removal in 1 case, and esophageal rupture in 1 case (Table 4). Comorbidities were present in three of the five cases with postoperative complications. Cases with suspected pulmonary tuberculosis were transferred to a specialized facility; however, the other four cases were successfully treated conservatively. No Clavian–Dindo classification Grade III or higher complications were observed.
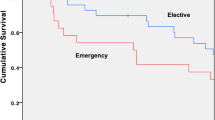
Among the 44 cases, two cases of stage IV disease were excluded from the analysis of postoperative recurrence. Among those included in the analysis, postoperative recurrence was observed in six cases. The organs involved in recurrence included the liver in three cases, lung in three cases, and peritoneal dissemination in one case. The median observation period was 30.5 months, and four patients died of primary illness during the observation period.
To determine the factors that affected complications, we performed a statistical analysis of the correlation among various factors, including sex; BMI; ASA; left and right primary lesions; open surgery or laparoscopic surgery; and history of laparotomy, hypertension, diabetes, ischemic heart disease, and cerebral infarction. The details are shown in Table 5. Of these factors, the incidence of complications was significantly higher in patients with a history of ischemic heart disease than in other patients. Furthermore, a multivariate analysis was performed involving these factors; however, no significant difference was observed.
Discussion
Surgery performed in the super-elderly is often associated with multiple comorbidities during perioperative management. Typical comorbidities, including cerebral infarction, dementia, hypertension, chronic obstructive pulmonary disease, chronic kidney disease, chronic heart disease, and organ disorders, often do not manifest before surgery and only appear after surgery. Therefore, a thorough evaluation by a multidisciplinary team, such as evaluation of preoperative swallowing function, perioperative rehabilitation, and nutritional status, is important. Recently, sarcopenia and flail have been used to predict the perioperative course of patients undergoing surgery for malignant gastrointestinal tumors [6, 7].
In the elderly, adjuvant and systemic chemotherapy regimens are difficult to administer at the time of recurrence and may need to be given extensively because of problems including poor general condition, side effects, and poor drug compliance. Thus, high curability is required for the initial surgery. In contrast, complications often occur during long recovery times because of poor general conditions, which may result in decreased quality of life (QOL). Postoperative complications are often fatal, depending on the patient’s reserve capacity and the extent of complications. In fact, for surgery of a malignant gastrointestinal tumor, the incidence of adverse events and postoperative mortality increases in patients above 75 years of age, and the risk is further increased in patients above 85 years of age [8]. The feasibility and indication of colorectal cancer surgery in the super-elderly aged ≥ 90 years should be carefully considered.
The results of the present study indicated that the surgical time, bleeding volume, and postoperative hospital stay of the super-elderly were comparable to those of nonelderly patients; however, the dissection range was not markedly reduced. Although Clavian–Dindo classification Grade II complications were observed in five cases (11.3%), they were not very common. Furthermore, no Grade III or higher complications were observed. These results indicated that the curability of cancer was not affected by surgery for the super-elderly, and surgery was performed relatively safely.
The univariate analysis showed that the history of ischemic heart disease may be a risk factor for the occurrence of complications; however, no significant difference was observed in the multivariate analysis. Similar and noteworthy results have been reported previously [9]. Although not limited to the elderly, this study considers the history of ischemic heart disease as a risk factor for suture failure following laparoscopic rectal cancer surgery. In addition, the history of ischemic heart disease is a risk factor for postoperative complications in patients above 90 years of age undergoing colorectal cancer surgery [10]. In cases with a history of ischemic heart disease, arteriosclerosis may progress and microcirculatory failure of the intestinal membrane may occur. Furthermore, renal dysfunction is often associated with the progression of arteriosclerosis, suggesting that edematous changes in tissues occur, thereby increasing the risk of delayed wound healing and anastomotic insufficiency [11].
At present, laparoscopic colorectal cancer surgery is performed worldwide. Furthermore, studies have described the usefulness of laparoscopic surgery in the elderly. The results of joint research conducted at other institutions in Japan have been reported, and a comparative study of laparoscopic surgery and laparotomy in patients above 80 years of age has been conducted [12]. In the present study, no significant differences in overall survival, disease-free survival, or cancer-specific survival were observed between the laparoscopic surgery and laparotomy groups. Although no significant difference in the occurrence of postoperative complications in rectal cancer was observed, the occurrence of postoperative complications in colon cancer following laparoscopic surgery was significantly lower. In the present study, laparoscopic surgery was performed in 34 of the 44 cases (77.2%). In the future, laparoscopic surgery will be used for the super-elderly, and it is expected that the number of cases will increase as population aging progresses worldwide. In contrast, laparotomy is an option for patients with a poor general condition who are limited to an operation time of 1 h. Furthermore, in cases with severe respiratory depression, maintaining the pneumoperitoneum for extended periods is difficult; thus, laparotomy may be unavoidable. In the future, evaluating more cases and considering the indications for laparoscopic surgery, including postoperative complications, are necessary.
In the present study, we examined super-elderly (aged ≥ 90 years) patients who had undergone colorectal cancer surgery at a single institution. The total number of cases was small (n = 44); thus, evaluating additional cases is necessary in the future. The median observation period was relatively short (30.5 months). Because the cohort was elderly, many causes of death were encountered other than natural illnesses, and tracking data on the long-term prognosis after surgery may be difficult. Furthermore, postoperative data are limited to the presence or absence of recurrence and confirmation of survival, and other factors, including postoperative QOL and defecation, have not been investigated.
Conclusion
At our institution, colorectal cancer surgery can be safely performed even in nonagenarians without impairing curability through a sufficient preoperative evaluation. Laparoscopic surgery can be safely performed even for the super-elderly, and it is expected that these procedures will increase in frequency in the future.
Data Availability
Data are available upon request.
Code Availability
Not applicable.
References
Department of Economic and Social Affairs. The world population prospects. 2015 revision. United Nations; 2015. https://www.un.org/development/desa/pd/
Kunitake H, Zingmond DS, Ryoo J (2010) Ko CY (2010) Caring for octogenarian and nonagenarian patients with colorectal cancer: what should our standards and expectations be? Dis Colon Rectum 53:735–743. https://doi.org/10.1007/dcr.0b013e3181cdd658
Kordatou Z, Kountourakis P, Papamichael D (2014) Treatment of older patients with colorectal cancer: a perspective review. Ther Adv Med Oncol 6:128–140. https://doi.org/10.1177/1758834014523328
Weber DM (2003) (2003) Laparoscopic surgery: an excellent approach in elderly patients. Arch Surg 138:1083–1088. https://doi.org/10.1001/archsurg.138.10.1083
Kanda Y (2013) (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Nakanishi R, Oki E (2018) Sasaki S (2018) Sarcopenia is an independent predictor of complications after colorectal cancer surgery. Surg Today 48:151–157. https://doi.org/10.1007/s00595-017-1564-0
Okabe H, Ohsaki T, Ogawa K et al (2019) (2019) Frailty predicts severe postoperative complications after elective colorectal surgery. Am J Surg 217:677–681. https://doi.org/10.1016/j.amjsurg.2018.07.009
Yeo HL, O’Mahoney PR, Lachs M et al (2016) (2016) Surgical oncology outcomes in the aging US population. J Surg Res 205:11–18. https://doi.org/10.1016/j.jss.2016.04.038
Shinji S (2018) Ueda Y (2018) Male sex and history of ischemic heart disease are major risk factors for anastomotic leakage after laparoscopic anterior resection in patients with rectal cancer. BMC Gastroenterol 18:117. https://doi.org/10.1186/s12876-018-0846-3
Chan TY, Foo CC, Law WL (2019) Lo O (2019) Outcomes of colorectal cancer surgery in the nonagenarians: 20-year result from a tertiary center. BMC Surg 19:155. https://doi.org/10.1186/s12893-019-0623-4
Tanaka Y, Kanda M, Tanaka C et al (2017) (2017) Usefulness of preoperative estimated glomerular filtration rate to predict complications after curative gastrectomy in patients with clinical T2–4 gastric cancer. Gastric Cancer 20:736–743. https://doi.org/10.1007/s10120-016-0657-6
Hinoi T, Kawaguchi Y, Hattori M et al (2015) (2015) Laparoscopic versus open surgery for colorectal cancer in elderly patients: a multicenter matched case-control study. Ann Surg Oncol 22:2040–2050. https://doi.org/10.1245/s10434-014-4172-x
Acknowledgements
The authors have no conflicts of interest to report and did not receive any financial support for this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This was a self-sponsored study.
Author information
Authors and Affiliations
Contributions
MS and YH wrote the manuscript. IK and YK supervised this report. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the Clinical Research Institutional Review Board of Saitama Medical University International Medical Center (approval no. 2021–204) and was conducted according to the 1964 Declaration of Helsinki and its later amendments or specified comparable standards.
Consent to Participate
Not applicable as this was a retrospective observational study.
Consent for Publication
Not applicable as this was a retrospective observational study.
Conflicts of Interest
The authors have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sasaki, M., Hirano, Y., Okamoto, K. et al. Outcomes of Colorectal Cancer Surgery in Nonagenarian Patients. Indian J Surg 86, 289–293 (2024). https://doi.org/10.1007/s12262-023-03854-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03854-5