Abstract
Purpose
Risks and benefits of colorectal cancer resection in octogenarians are not clearly defined. This study aimed to assess the relationship between morbidity and mortality within 1 year after colorectal cancer resection in octogenarians compared with other age groups.
Methods
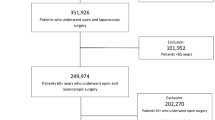
A single-institution, prospectively maintained database was queried to identify patients with sporadic, pathological stages I–III colorectal adenocarcinoma, electively undergoing radical resection with curative intent between 2000 and 2012. Patients were divided into three age groups: ‘octogenarians’ if ≥80 years of age; ‘intermediate’ if ≥65 and <80 years of age; and ‘younger’ if <65 years of age.
Results
Overall, 2485 patients fulfilled the inclusion criteria—326 in the octogenarian age group, 949 in the intermediate age group, and 1210 in the younger age group. Postoperative morbidity disproportionally increased 1-year mortality in octogenarians when compared with the younger age group (37 vs. 6.5 %; p < 0.001). Anastomotic leak, abdominopelvic abscess, reoperation, and readmission rates were comparable among different age groups, but were associated with a disproportionate risk of 1-year mortality in octogenarians (67, 43, 33, and 41 %, respectively). Multivariate analysis indicated that older age and postoperative complications were the only two independent variables associated with 30- and 90-day mortality. Besides these, American Society of Anesthesiologists (ASA) and pathological stage III were additional independent variables associated with 1-year mortality. An interaction test confirmed that age and postoperative complications were independent variables, with additive effect on 30-day, 90-day, and 1-year mortality.
Conclusions
Age plays an important and independent role in affecting mortality when complications occur following surgery for colorectal cancer. The full magnitude of postoperative risks should be taken into consideration when discussing colorectal cancer surgery in octogenarians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The incidence of elderly patients with colorectal cancer is prone to increase, considering that the risk of colorectal cancer increases proportionally with age1 and life expectancy in the general population is becoming progressively longer.2
However, the specific risks and benefits of resection for colorectal cancer in the elderly subpopulation, especially octogenarians, are not clearly defined.3–7 In particular, the data used to generate guidelines for the treatment of colorectal cancer are collected on younger patients, which are disproportionately accrued into prospective trials assessing different treatment options, and might not be equally relevant to elderly patients.3,4
It is generally accepted that resection of colorectal cancer in elderly patients is associated with higher morbidity rates,8 as well as high mortality rates, both in the immediate postoperative period and during the first year after surgery.5,8–14 However, scant data are available on the relationship between postoperative morbidity and mortality across different ages, both immediately after surgery and beyond the initial 30 postoperative days. It is also unclear if specific complications influence this relationship more than others, and whether age is a truly independent factor related to mortality or a confounder of severe comorbidity rates.5,8,9,15
The present study therefore aimed to assess the relationship between morbidity and mortality within 1 year after colorectal cancer resection in octogenarians compared with other age groups.
Methods
A single institution, prospectively maintained Institutional Review Board-approved database corroborated by patient medical records was queried to identify patients with pathological stages I–III colorectal adenocarcinoma, electively operated with curative intent between 2000 and 2012. Database variables included patient demographics, body mass index (BMI), American Society of Anesthesiologists (ASA) classification of physical health, tumor site, surgical procedure, length of hospital stay (LOS), complications, reoperation, readmission, and mortality. Data were supplemented by chart review as necessary. Frequencies of specific comorbidities were collected using International Classification of Diseases, Ninth Revision (ICD-9) codes. Exclusion criteria were patients with distant metastases, recurrent disease, synchronous inflammatory bowel disease, hereditary colorectal neoplasm, malignancy other than adenocarcinoma, emergency surgery, and local resections. Patients were divided into three groups based on their age at the time of surgery: ‘octogenarians’ if ≥80 years of age; ‘intermediate’ if ≥65 and <80 years of age; and ‘younger’ if <65 years of age.
Definitions of Study Variables
Intraoperative complications were defined as complications occurring during the operative procedure. The specific intraoperative complications analyzed were anastomosis redo/repair, bladder injury, intraoperative hemorrhage reported in the operative note and requiring packed red blood cell transfusion, rectal perforation, splenic injury, ureteral injury, urethral injury, vaginal injury, and vascular injury.
Postoperative morbidity was defined as a complication occurring within 30 days after surgery, or during the same hospital stay. The specific postoperative complications analyzed were abdominal and/or pelvic abscess (organ space surgical site infection), kidney failure requiring hemodialysis in a patient who did not require dialysis preoperatively, anastomotic leak, arrhythmia, Clostridium difficile infection, stoma complications, dehydration, enteric leak occurring away from any anastomoses, ileus, myocardial infarction, cerebrovascular accident, pneumonia, reintubation, small bowel obstruction, urinary retention, urinary tract infection, deep venous thrombosis, portal venous thrombosis, pulmonary embolism, wound/superficial surgical site infection, fascial dehiscence, and deep fascial infection. The definition of abdominopelvic abscess/organ space infection was an infection related to the operation involving any part of the anatomy, other than the incision, which was opened or manipulated during an operation, and at least one of the following: purulent drainage from a drain placed through a stab wound into the organ/space, organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space, and an abscess or other evidence of infection involving the organ/space that is found on direct examination during reoperation or by radiologic examination. Anastomotic leakage was defined as anastomotic separation, based on extravasation of contrast by radiology study or direct physician documentation. Reoperation and readmission were considered as any unplanned returns to the operating room or to the main hospital within 30 days after surgery, and index hospital discharge, respectively.
Mortality was assessed at 30 days, 90 days, and 1 year following surgery. Morbidity, reoperations and readmissions were based on the number of patients with at least one event, related to either the index hospital stay or readmission.
Statistics
The age groups were compared with respect to patient-related variables, tumor-related variables, procedure characteristics, morbidity, and mortality. Comparisons were performed using Fisher’s exact tests or Chi square tests for categorical variables. Comparisons of age groups with respect to quantitative and ordinal variables were performed using the Kruskal–Wallis test, and statistical significance was defined as p < 0.05.
The association of each complication with mortality rates was initially analyzed considering all patients combined and regardless of their age. In particular, possible associations between each specific complication and 30-day, 90-day, and 1-year mortality were assessed using Fisher’s exact tests or Chi square tests. Multivariate analysis for 30-day, 90-day, and 1-year mortality was performed by logistic regression modeling using the variables that were statistically significant in the univariate analyses. For that purpose, we used postoperative complications combined, due to small numbers to assess each complication separately in the multivariate modeling. We also used logistic regression models to investigate interactions between age and postoperative complications on mortality. The interaction tests assessed if either age or the presence of a complication acted as an effect modifier for the association of the other variable with mortality. Statistical analyses were performed in consultation with a statistician, using R version 2.15.1 (r-project.org).
Results
Between 2000 and 2012, a total of 2485 of 3003 patients treated for stage I–III colorectal cancer in our institution fulfilled the inclusion criteria. Overall, 326 patients were octogenarians, 1210 patients were younger than 65 years of age, and 949 patients had an intermediate age of between 65 and 79 years. The percentage of females and the ASA score proportionally increased with patient age, unlike BMI, which was inversely proportional to patient age. When assessing specific comorbidities for each age group, the octogenarian and intermediate age groups more frequently had diabetes, history of cerebrovascular accident, hypertension, angina, congestive heart failure, myocardial infarction history, chronic obstructive pulmonary disease, dementia, and kidney failure than the younger age group (Table 1). Octogenarians were more likely to undergo surgery for more proximal tumors, while radical resection for rectal cancer was more frequent in younger patients, who also had more advanced disease at the time of diagnosis. In particular, right hemicolectomy amounted to almost half of the operations performed in the octogenarian age group, while anterior resection was the most frequent operation performed in the other age groups. No differences were observed in the use of laparoscopic surgery among the age groups; however, conversions were more likely in the octogenerian group. While no differences in the rates of intraoperative complications were observed among the groups, the rate of postoperative complications increased proportionally with age. Death rates also increased proportionally with age, when taking into account all intervals of interest at 30-day, 90-day, or 1-year after surgery. The mean LOS was also significantly longer in the octogenerian group compared with the other two groups, while no differences were noted with respect to reoperation or readmission rates among the groups (Table 1).
While intraoperative morbidity carried no significant association with mortality at any interval (data not shown), postoperative morbidity was associated with a substantial increase in postoperative mortality in all age groups, especially among octogenarians. For example, 1-year mortality in octogenarians was 5.7 % in the absence of postoperative complications, but jumped to 37 % once at least one postoperative complication occurred (Table 1).
The incidence of specific intraoperative morbidity was similar in the three groups. When examining postoperative complications, the incidences of anastomotic leak, abdominopelvic abscess, myocardial infarction, cerebrovascular accident, and wound infection were also comparable among the different age groups; however, octogenarians were significantly more likely to experience postoperative arrhythmia, pneumonia, reintubation, kidney failure requiring hemodialysis, deep venous thrombosis, pulmonary embolism, and Clostridium difficile infection (Table 2).
When assessing associations between specific perioperative complications and mortality in the entire study population, considering all age groups combined, we did not identify any significant associations between any intraoperative complications and mortality at any interval. Instead, specific postoperative complications significantly associated with mortality were observed, at least in one of the three postoperative time intervals of interest, i.e. anastomotic leak, abdominal/pelvic abscess, myocardial infarction, arrhythmia, cerebrovascular accident, pneumonia, reintubation, kidney failure requiring hemodialysis, pulmonary embolism, and Clostridium difficile infection. Urinary tract infection and wound infection were not associated with mortality (Table 3).
We then evaluated possible differences in the risk of death among different age groups related to hospital readmission or specific complications. Readmission was associated with significantly increased mortality in older patients at all postoperative intervals of interest, while anastomotic leak, abdominopelvic abscess, postoperative arrhythmia, and reoperation were associated with increased postoperative mortality at 90 days and 1 year (Table 4). Lastly, reintubation was found to be associated with significantly increased mortality in older patients within 1 year after surgery. Other complications were equally likely to result in mortality among the different age groups (Table 4).
A stepwise multivariate logistic regression was performed to identify the independent factors associated with mortality. Age, sex, BMI, ASA, cancer site (colon vs. rectum), pathological stage, procedure, intraoperative complications, and postoperative complications were significant on univariate analysis and were therefore used as covariates. Increased age and postoperative complications were the only two independent variables associated with 30-day and 90-day mortality. Besides these, ASA and pathological stage III were additional independent variables associated with 1-year mortality (Table 5).
To confirm the autonomous role of age and postoperative morbidity as risk factors for death following surgery, we then performed an interaction test between age and postoperative morbidity in 30-day, 90-day, and 1-year mortality. The absence of interaction confirmed that age and postoperative complications were independent variables with additive effect on 30-day, 90-day and 1-year mortality (p = 1.0, p = 0.15, and p = 0.60, respectively).
Discussion
Our data indicated that postoperative morbidity following resection for colorectal cancer is more common in elderly patients and results in a significant increase in mortality, which continues to increase well beyond the initial postoperative month. Age and the occurrence of postoperative morbidity were both independent and important factors affecting mortality at 30 days, 90 days and 1 year following surgery. In addition, there were specific complications whose incidences were comparable among age groups but were associated with disproportionate mortality in elderly patients, particularly in octogenarians.
Our results are consistent with previous data indicating increased mortality after surgery for colorectal cancer in the elderly,5,9,16 whose age groups have been defined based on different age cutoffs in the literature. Our age grouping was planned so that we could selectively point out those previously defined as ‘the oldest old’12 when compared with other age groups. Our data also reflect the results of previous investigators who have questioned the validity of the 30-day interval as an accurate endpoint in the measurement of postoperative mortality in the elderly patient population, considering that postoperative mortality extends beyond 30 days.12,13,17–19
Our findings confirm the association between postoperative morbidity and mortality, as previously reported in general surgical populations without particular age restrictions.20,21 However, our analysis also revealed specific and relevant associations between individual postoperative complications and increased risk of death at different time periods. For example, septic complications, such as abdominal/pelvic abscess and anastomotic leak, as well as postoperative arrhythmia, were not significantly associated with death until after the first postoperative month, which might have depended on the effectiveness of perioperative care delivered immediately after surgery.
The original data from the present study on the effect of specific complications on mortality in the elderly could also have practical implications, both in preoperative planning and postoperative care. For example, the sobering data on the consequences of anastomotic leaks and abscesses could prompt greater consideration for proximal stoma diversion or even non-restorative procedures in elderly patients and closer follow-up after hospital discharge if they experienced postoperative arrhythmias.
When examining 1-year mortality, ASA and pathological stage III tumor were also independently associated with mortality, besides age and postoperative complications. This is not surprising and is consistent with previous data.20,22 However, the high odds ratio associated with age and postoperative complications, as well as the absence of statistical interaction between age and morbidity, confirmed that they remained independent and important factors associated with 1-year mortality, both statistically and clinically.
The strengths of this study revolve on the details provided by prospectively collected data on a relatively large number of patients treated in a single institution, including data on specific complications, which are generally more difficult to tease out when assessing large administrative databases. We could therefore analyze not only the relationship between morbidity and mortality in general but also the more nuanced relationship between the incidence of specific complications and mortality for different age groups at defined time intervals.
The limitations of our study were its retrospective design and the inherent referral and selection bias when considering patients for surgery in a single tertiary referral center, particularly in the case of elderly individuals who may have prohibitive comorbidities. It has also been argued that the influence of age on perioperative outcomes is not direct, but rather reflective of the associated comorbidities; however, aging is not only associated with increased comorbidities but also with decline of functional reserve, and personal and social restrictions; these are probably critical factors directly responsible for poorer outcomes.23 The separation between age as a number and specific age-related deficits remains challenging. Our analysis, indicating the independent effect of age on mortality, remains limited in its potential to ultimately address this issue, as comorbidity was mainly based on ASA classification instead of other, perhaps more sophisticated, tools such as Charlson’s comorbidity score,24 or predictors of morbidity such as the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) surgical risk calculator,25 frailty index,26 or POSSUM.27 It has been suggested that a comprehensive geriatric evaluation, including functional assessment, comorbidity, cognition, psychological state, social support, nutrition and medication, might improve outcomes following colorectal cancer resection in older adults.28,29 In particular, in 2012 the ACS NSQIP and the American Geriatrics Society (AGS) collaborated to create best practice guidelines around optimal perioperative care of geriatric surgical patients.30 By following these guidelines, the modifiable factors related to surgery in the elderly population can be optimized, and can probably improve morbidity and mortality outcomes. In the absence of routine implementation of such programs, we believe that the current study provides less sophisticated, but still useful, data, which can be practically utilized in the management of these high-risk patients.
Conclusion
Age plays an important and independent role in affecting mortality when complications occur following surgery for colorectal cancer. The full magnitude of postoperative risks should be taken into consideration when discussing colorectal cancer surgery in octogenarians.
References
Centers for Disease Control and Prevention (2016) Colorectal cancer risk by age. http://www.cdc.gov/cancer/colorectal/statistics/age.htm. Accessed 4 Mar 2016.
Centers for Disease Control and Prevention. National Center for Heath Statistics (2016) Life expectancy. http://www.cdc.gov/nchs/fastats/life-expectancy.htm. Accessed 4 Mar 2016.
Audisio RA, Papamichael D. Treatment of colorectal cancer in older patients. Nat Rev Gastroenterol Hepatol. 2012;9:716–25.
Papamichael D, Audisio RA, Glimelius B et. al. Treatment of colorectal cancer in older patients: International Society of Geriatric Oncology (SIOG) consensus recommendations 2013. Ann Oncol. 2015;26:463–76.
Kunitake H, Zingmond DS, Ryoo J, Ko CY. Caring for octogenarian and nonagenarian patients with colorectal cancer: what should our standards and expectations be? Dis Colon Rectum. 2010;53:735–43.
Nitsche U, Spath C, Muller TC, et. al. Colorectal cancer surgery remains effective with rising patient age. Int J Colorectal Dis. 2014;29:971–9.
Steele SR, Park GE, Johnson EK, Martin MJ, Stojadinovic A, Maykel JA, et al. The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis Colon Rectum. 2014;57:303–310.
Tan KY, Kawamura Y, Mizokami K, Sasaki J, Tsujinaka S, Maeda T, et al. Colorectal surgery in octogenarian patients: outcomes and predictors of morbidity. Int J Colorectal Dis. 2009;24:185–9.
Ihedioha U, Gravante G, Lloyd G, Sangal S, Sorge R, Singh B, et al. Curative colorectal resections in patients aged 80 years and older: clinical characteristics, morbidity, mortality and risk factors. Int J Colorectal Dis. 2013;28:941–7.
Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865–77.
Dekker JW, van den Broek CB, Bastiaannet E, van de Geest LG, Tollenaar RA, Liefers GJ. Importance of the first postoperative year in the prognosis of elderly colorectal cancer patients. Ann Surg Oncol. 2011;18:1533–9.
Al-Refaie WB, Parsons HM, Habermann EB, Kwaan M, Spencer MP, Henderson WG, et al. Operative outcomes beyond 30-day mortality: colorectal cancer surgery in oldest old. Ann Surg. 2011;253:947–52.
Mamidanna R, Almoudaris AM, Faiz O. Is 30-day mortality an appropriate measure of risk in elderly patients undergoing elective colorectal resection? Colorectal Dis. 2012;14:1175–82.
Engel AF, Oomen JL, Knol DL, Cuesta MA. Operative mortality after colorectal resection in the Netherlands. Br J Surg. 2005;92:1526–32.
Manceau G, Karoui M, Werner A, Mortensen NJ, Hannoun L. Comparative outcomes of rectal cancer surgery between elderly and non-elderly patients: a systematic review. Lancet Oncol. 2012;13:e525–e536.
Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY. Identification of specific quality improvement opportunities for the elderly undergoing gastrointestinal surgery. Arch Surg. 2009;144:1013–1020.
Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg. 2012;99:1149–54.
van Gestel YR, Lemmens VE, de Hingh IH, et. al. Influence of comorbidity and age on 1-, 2-, and 3-month postoperative mortality rates in gastrointestinal cancer patients. Ann Surg Oncol. 2013;20:371–80.
Visser BC, Keegan H, Martin M, Wren SM. Death after colectomy: it’s later than we think. Arch Surg. 2009;144:1021–1027.
Gooiker GA, Dekker JW, Bastiaannet E, et. al. Risk factors for excess mortality in the first year after curative surgery for colorectal cancer. Ann Surg Oncol. 2012;19:2428–34.
Greenblatt DY, Weber SM, O’Connor ES, LoConte NK, Liou JI, Smith MA. Readmission after colectomy for cancer predicts one-year mortality. Ann Surg. 2010;251:659–69.
Dekker JW, Gooiker GA, Bastiaannet E, et. al. Cause of death the first year after curative colorectal cancer surgery; a prolonged impact of the surgery in elderly colorectal cancer patients. Eur J Surg Oncol. 2014;40:1481–7.
Korc-Grodzicki B, Downey RJ, Shahrokni A, Kingham TP, Patel SG, Audisio RA. Surgical considerations in older adults with cancer. J Clin Oncol. 2014;32:2647–53.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208:1009–1016.
Makary MA, Segev DL, Pronovost PJ, et. al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010;210:901–908.
Al-Homoud S, Purkayastha S, Aziz O, et. al. Evaluating operative risk in colorectal cancer surgery: ASA and POSSUM-based predictive models. Surg Oncol. 2004;13:83–92.
Cheema FN, Abraham NS, Berger DH, Albo D, Taffet GE, Naik AD. Novel approaches to perioperative assessment and intervention may improve long-term outcomes after colorectal cancer resection in older adults. Ann Surg. 2011;253:867–74.
Tan KY, Tan P, Tan L. A collaborative transdisciplinary “geriatric surgery service” ensures consistent successful outcomes in elderly colorectal surgery patients. World J Surg. 2011;35:1608–1614.
Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF; American College of Surgeons National Surgical Quality Improvement Program, American Geriatrics Society. Optimal preoperative assessment of the geriatric surgical patient: a best practices guideline from the American College of Surgeons National Surgical Quality Improvement Program and the American Geriatrics Society. J Am Coll Surg. 2012;215:453–66.
Disclosure
The authors have no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Duraes, L.C., Stocchi, L., Dietz, D. et al. The Disproportionate Effect of Perioperative Complications on Mortality within 1 Year After Colorectal Cancer Resection in Octogenarians. Ann Surg Oncol 23, 4293–4301 (2016). https://doi.org/10.1245/s10434-016-5445-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5445-3