Abstract
Plummer-Vinson syndrome (PVS) or the Patterson-Brown-Kelly syndrome is a triad of iron deficiency anaemia (IDA), dysphagia and oesophageal webs. Commonly seen in middle-aged Caucasian females in the 4th to 7th decade, it is rare in males. It is usually a diagnosis made solely on clinical suspicion as history and clinical examination findings are equivocal. We have described a 55-year-old lady who presented with complaints of dysphagia and IDA. With all her initial investigations pointing towards gastritis, pure suspicion lead us to the diagnosis with a barium swallow. She was managed successfully with medications and currently on regular follow up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Plummer-Vinson syndrome (PVS) or the Patterson-Brown-Kelly syndrome is a triad of iron deficiency anaemia (IDA), dysphagia and oesophageal webs [1, 2]. Commonly seen in middle-aged Caucasian females in the 4th to 7th decade, it is rare in males [3]. Diagnosis rests solely on clinical suspicion as history and clinical examination are usually equivocal. Here, we describe a 55-year-old lady who presented with complaints of dysphagia and IDA and was diagnosed with PVS.
Case Report
A 55-year-old lady presented with complaints of non-progressive difficulty in swallowing for 4 years duration for both solids and liquids. She had an occasional epigastric burning type of pain, aggravated by food and relieved by antacids. She had multiple diagnosed episodes of gastritis; however, she denied any history of loss of appetite, loss of weight, malena or hematemesis. There was no relevant family history.
Clinical examination was unremarkable but for deep pallor. Her blood investigations reported marked anaemia with a microcytic hypochromic anaemia with eosinophilia (Table 1). Her other blood investigations were normal with creatinine of 0.7, sodium 145 mEq/L, potassium of 4.5 mEq/L, chloride of 100 mEq/L and bicarbonate of 24 mEq/L.
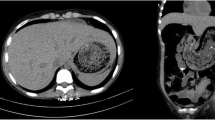
She underwent oesophageal-gastro-duodenoscopy (OGD) with difficult negotiation through the upper oesophagus (Fig. 1). Gastric mucosa showed features of gastritis with a lax lower oesophagal sphincter. Hence, a provisional diagnosis of gastro-oesophagal reflux disease was made. Mucosal biopsy divulged chronic antral gastritis. For anaemia, a comprehensive workup was done in the form of stool occult blood testing, abdomen imaging and colonoscopy. All tests were reported as negative for any mitotic changes.
At this point, pure clinical suspicion led to us performing a barium swallow for the patient which demonstrated an upper oesophageal web, establishing the triad for a diagnosis of PVS (Figs. 2, 3). The patient then underwent a repeat endoscopy under sedation and the oesophageal web was visualised 20 cm from the incisors. Biopsy obtained from the oesophagus ruled out dysplasia/malignancy and eosinophilic oesophagitis.
She was maintained on proton pump inhibitors and prokinetics during her in-hospital stay along with iron supplementation. On achieving reasonable symptomatic relief, she was discharged. She is currently on follow-up and has been advised annual endoscopy to rule out dysplastic changes.
Discussion
First described independently, by Harvey Plummer and Porter Vinson as a triad of swallowing difficulty with nutritional anaemia, it had been termed as Plummer-Vinson syndrome since. It was also described by Patterson and Brown-Kelly independently in the United Kingdom around the same time and hence known by their name also. Iron deficiency causing mucosal degeneration due to its effect on enzymes has been postulated as one of the causes [4].
The diagnosis relies on history taking, haematological examination for anaemia and radiological examination like barium swallow. Direct endoscopy examination techniques have often missed this finding [5]. Differential diagnosis includes other causes of dysphagia like motility disorders, strictures, gastroesophageal reflux disease and carcinoma. This syndrome is a pre-malignant state hence, regular annual follow-up with endoscopy and biopsy is mandated [6].
Management includes treatment for IDA which is usually complete with just nutritional supplements. Increased menstrual flow in females could explain why it has a female preponderance. In males, underlying malignancy should be ruled out. For the webs causing dysphagia, it often requires dilatation either endoscopically or with Savary dilators. Breaking the webs with electrocautery is also practised. Eosinophilic oesophagitis should be ruled out before endoscopic dilatation as it has been associated with greater perforation rates.
Multiple studies have shown that most webs require intervention [4]. However, there are isolated reports of successful management with iron supplementation alone, driven in part due to social conditions or the non-availability of higher endoscopic facilities [7]. In our study, she was maintained solely on iron supplementation. On review, she reported an increase in haemoglobin as well as an improvement in dysphagia. She is currently on regular follow-up.
The rates of PVS have demonstrated a downhill course in terms of incidence due to modern nutritious diets and deficiencies being identified and corrected earlier. This trend has unconsciously dismissed PVS as a cause of dysphagia. This case report underlines the importance of retaining PVS in differentials for dysphagia, particularly in developing nations where nutritional anaemia is still rampant and advocates the routine use of barium swallows in the evaluation of dysphagia [8].
References
Paterson DR (1919) A clinical type of dysphagia. Proc R Soc Med 12(Laryngol Sect):235–9
Kelly AB (1919) Spasm at the entrance to the œsophagus. J Laryngol Otol 34(8):285–289
Wynder EL, Hultberg S, Jacobsson F, Bross IJ (1957) Environmental factors in cancer of the upper alimentary tract; a Swedish study with special reference to Plummer-Vinson (Paterson-Kelly) syndrome. Cancer 10(3):470–487
Novacek G (2006) Plummer-Vinson syndrome. Orphanet J Rare Dis 1(1):36
Hoffman RM, Jaffe PE (1995) Plummer-Vinson syndrome. A case report and literature review. Arch Intern Med 155(18):2008–11
Rashid Z, Kumar A, Komar M (1999) Plummer-Vinson syndrome and postcricoid carcinoma: late complications of unrecognized celiac disease. Am J Gastroenterol 94(7):1991
Tahara T, Shibata T, Okubo M, Yoshioka D, Ishizuka T, Sumi K et al (2014) A case of plummer-vinson syndrome showing rapid improvement of dysphagia and esophageal web after two weeks of iron therapy. Case Rep Gastroenterol 8(2):211–215
Chen TS, Chen PS (1994) Rise and fall of the Plummer-Vinson syndrome. J Gastroenterol Hepatol 9(6):654–658
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sekaran, P.G., Kirouchenaradj, V. & Moorthy, N. Plummer-Vinson Syndrome—Out of Sight, Out of Mind?. Indian J Surg 86, 222–224 (2024). https://doi.org/10.1007/s12262-023-03837-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-023-03837-6