Abstract
Despite all technological advances in imaging, many insulinomas remain occult. The aim of this study was to investigate the sensitivity of various pre-operative localization modalities used over the last three decades in our center. Tertiary care hospital, retrospective study (January 1990 and December 2020). This study consists of 36 patients of biochemically diagnosed cases of organic hyperinsulinemic hypoglycemia. Radiology findings were correlated with operative and histology findings. Median age of the patients was 45 years (M:F = 1:1.8). Multiple endocrine neoplasia type 1, islet cell hyperplasia (ICH), and malignancy were noted in 13.9, 5.6, and 5.6% patients, respectively. The median number of pre-operative localization tests used was 2 (1 = 41.7, 2–50, ≥ 3–8.4%). Contrast enhanced computerized tomography (CECT) was the commonest imaging modality used in 91.7% patients (standalone—39.5%) followed by ultrasonography (USG) in 41.7% patients. Pre-operative localization rate was 86.1% (66.6% vs 92.6% before and after 2005). The sensitivity of USG, CECT, MRI, and selective arterial calcium stimulation with hepatic venous sampling (ASVS) was 35.7%, 83.3%, 71.4%, and 75%, respectively. The pre-operative localization rates with one, two, and more modalities were 93.3, 77.7, and 100%, respectively. Bi-digital palpation and intraoperative USG were accurate in 97% cases resulting in successful primary surgery. Pre-operative localization techniques for insulinoma continue to evolve. CECT scan was found to be the most sensitive pre-operative localization modality in our experience. Almost all insulinomas can be detected pre-operatively by an experienced surgeon and expert performed IOUS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Insulinoma is a rare pancreatic neoplasm resulting in condition of hyperinsulinemic hypoglycemia. Surgery is curative in almost all cases [1]. The diagnosis of hyperinsulinemic hypoglycemia is based on biochemical evaluation, and the role of imaging is to localize the tumor in order to plan the appropriate surgical strategy. Despite advancement in imaging technology, all insulinomas cannot be localized pre-operatively and non-localization rate varies between 10 and 27% in various series [2, 3]. Further, imaging cannot differentiate between insulinoma and islet cell hyperplasia (ICH), the two chief conditions responsible for organic hyperinsulinism. Surgical strategy for insulinoma and ICH is entirely different, while majority of insulinomas can be managed by enucleation of tumor, a formal resection is required in ICH [2]. It is well-established that an experienced surgeon can localize insulinoma with digital palpation during surgery resulting in successful outcome and reverting of hypoglycemia in 90–95% of patients [4]. Addition of intraoperative ultrasonography (IOUS) improves the results of digital palpation [1, 5]. Considering all the aforementioned facts, the need and extent of pre-operative localization of insulinoma remains controversial [6, 7]. But it is important to realize that accurate pre-operative localization has potential to reducing operation time, add to surgeons’ confidence, and would be absolutely necessary if minimal invasive surgery is being planned [8, 9].
Due to the rarity of the condition, the consensus on the optimal pre-operative localization strategy is not established. World over various centers, depending on local expertise, have developed their own protocol for pre-operative localization of insulinoma [1, 4, 9]. An ideal localization modality should be cheap, widely available with reproducible results. Due to rarity of the condition, no head on comparisons are possible. Our center is one of the few tertiary referral centers in India which deal with this rare condition. The aim of this study was to find out the sensitivity of various pre-operative localization modalities for insulinoma over the last three decades and to compare the results with outcome of surgery in terms of reverting hypoglycemia.
Material and Methods
Retrospective study (Jan 1990–Dec 2020) consisting of biochemically proven cases of hyerinsulinemic hypoglycemia. Only those patients who underwent surgery were included and those who declined were excluded from the study. All patients were operated by a single team of two surgeons. Clinical, imaging, operative, histology, and follow-up findings were noted.
Diagnosis and Localization Protocol and Operative Technique
Diagnosis was established by 72-h supervised fasting test, and serum glucose, insulin, and C-peptide levels measured when patients developed symptoms or glucose level fell below 45 mg/dL. Preferred cross-section imaging technique at our center remains triple phase contrast enhanced computerized tomography (CECT) + ultrasonography (USG). Some cases underwent magnetic resonance imaging (MRI) on physicians’ discretion or when CECT was contraindicated. Selective arterial calcium stimulation with hepatic venous sampling (ASVS) was performed in selected instances in case when tumor was not localized on cross-sectional imaging and provided patient could afford the test. Intraoperative USG (IOUS) was performed in almost all cases except for one case of technical failure. Radiologist experienced in pancreatic USG helped in IOUS, and for the last 2–3 years, surgeons are performing on their own. Apart from identification of insulinoma, IOUS help in ruling out multicentric lesion and to delineate relationship of lesion with vascular structures and main pancreatic duct.
Open surgical technique remained the preferred technique at our center. The head and tail of pancreas are mobilized, and bi-digital palpation and IOUS are used to confirm the presence of already localized insulinoma and to detect the occult ones. Discrete lesions situated at least 5 mm away from the major pancreatic duct and blood vessels were enucleated, and pancreatic resection was performed when enucleation is not feasible—due to proximity of insulinoma with duct. Minimal normal parenchyma surrounding insulinoma is resected so as to preserve normal function as much as possible. Formal pancreatic resections, i.e., distal, subtotal pancreatectomy, is only performed in patients having positive gradient (regionalization) on ASVS but no discrete lesion found during surgery and/or when ICH was present or suspected. The area to be resected is determined by the territory showing the gradient—for example, splenic (distal pancreatectomy), superior mesenteric (subtotal/mid-segmental pancreatectomy), gastrodudenal (pancreato-duodenal resection), or all (near-total pancreatectomy). The anesthetists are asked to stop dextrose infusion half-hour prior to enucleation or resection. Rebound hyperglycemia is observed and is indicative of cure. This gradually settles down over the next 4–5 days. Insulin administration is avoided until blood sugar are more than 180 mg/dL so as to stimulate the suppressed beta cells to secrete insulin. Patients are allowed orally on 3rd–5th day and discharged after drain removal. Annual screening for MEN1 component is done in follow-up.
Statistical analysis was done on SPSS software (version 17). Continuous data was reported as mean or median and frequency as percentages.
Results
Thirty-eight patients were identified during the study period. Two patients with malignant insulinoma (with hepatic metastases) who were not operated were excluded from study. One of those died at home while awaiting surgery and another had inoperable lesion. Thirty-six patients were included in the final analysis. Median age of the patients was 45 years (7–67). Women outnumbered men (63.9%). Fourteen percent of patients were pediatric (≤ 18 years of age). Median duration of symptoms was 16 months (range: 0.5–120). Median insulin, C-peptide, and serum glucose concentration at the zenith of glucose level were 34.4 mIU/L (range: 8.4–116), 8.2 nmol/L (range: 0.36–308), and 35 mg/dL (range: 18–49), respectively. Multiple endocrine neoplasia type 1 (MEN1), ICH, and malignancy were noted in 13.9%, 5.6%, and 5.6% patients respectively and remaining had sporadic insulinoma. Multiple insulinoma were observed in 16.7%. Clinical and operative findings of the cohort are summarized in Table 1.
The number of imaging modalities employed was one, two, three, and four in 41.7%, 50%, 2.8%, and 5.6% patients, respectively. CECT was the commonest pre-operative modality used in 91.7% patients either standalone or in combination. Similarly, USG, MRI, ASVS, THPVS, and EUSG were performed in 41.7, 22.2, 8.3, 2.8, and 2.8% patients, respectively (Table 2). All patients had at least one cross-sectional imaging either CECT or/and MRI (CT—77.8%, MRI—8.3%, both CECT and MRI 13.9%). CT was standalone modality employed in 15 (41.7%) patients. Pre-operative localization was successful in 86.1% patients including 8.3% those where no discrete lesion could be made out but a territorial gradient hinting at a particular region of pancreas could be marked on ASVS or THVS. One (2.8%) had false positive localization. Thus, 13.9% patients were explored as occult insulinoma. The sensitivity of localizing insulinoma for US, CECT scan, MRI, and ASVS was 35.7%, 83.3%, 71.4%, and 75%, respectively. When one, two, and three or more pre-operative localization modalities were used, the localization rate was 93.3%, 88.9%, and 100%, respectively. All patients having undergone 3 or more modality had at least one cross-sectional imaging (CECT or MRI), and 66.6% had an invasive imaging in the form of ASVS or THVS (Table 3). Pre-operative localization rate was 66.6% before 2005 and 92.6% afterwards. The sensitivity of triple phase CECT has improved from 55.6 to 94.7% in the last 15 years. Of the 5 patients who had non-localized tumor on CT, three could be localization and/or regionalization on ASVS and in one abdominal USG helped. Addition of MRI did not help in any of these cases. Out of 5 patients with non-localized lesion prior to surgery, 4 had insulinoma, and 1 ICH. Thus, 4 out of 32 (12.5%) benign insulinoma and 50% of ICH remained unlocalized and/or non-regionalized prior to surgery (Fig. 1).
Intraoperative USG was used in 97.2% of cases and could not be used in one patient with malignant insulinoma due to technical reasons. Bi-digital palpation and IOUS were accurate in 97.2% cases. In three patients with positive pre-operative localization, IOUS detected another tumor besides the one localized pre-operatively. IOUS also helped in correctly localizing an insulinoma in a different location in one patient with false positive on CT. The lesion picked up on CECT turned out to be a lymph node. Surgery was successful in all but one patient (97.2%). Enucleation was performed in 44.4% patients and resection in 50%. In remaining patients who had MEN1, distal pancreatectomy + enucleation of tumors in head of the pancreas was done (5.5%). Out of two patients with final histology of ICH, one with positive pre-operative regionalization on THVS had distal pancreatectomy and remained euglycemic until last follow-up. Another who could not afford invasive testing remained non-localized. This patient had a false positive localization on IOUS and had persistent hypoglycemia following enucleation and later underwent a successful re-operation (subtotal pancreatectomy) at a later date. One patient with malignant insulinoma has wedge resection of liver at same sitting while another had recurrent metastatic disease 5 years later and underwent resection of 2 segments of liver. Four patients with MEN1 had subtotal parathyroidectomy, 3 during insulinoma surgery and 1 at later date. One with mild hypercalcemia did not consent for parathyroidectomy and is still under follow-up. The median size of insulinoma was 18 mm (range 9–35). All patients were cured of hypoglycemia, 3 of those undergoing resection developed diabetes. The summary of operative findings and outcome are provided in Table 4.
Discussion
CECT with current sensitivity rate of 83.3% turned out to be the most useful single modality for pre-operative localization of insulinoma in our experience. In case of non-localization, addition of another cross-sectional imaging did not contribute much. In this scenario, ASVS could help in regionalization of pathology. In a biochemically proven case of hyperinsulinism, non-localization could be suggestive of ICH, and based on ASVS results, a gradient driven resection can be performed. Almost all insulinomas can be detected peroperatively by an experienced surgeon and expert performed IOUS.
The reported success of pre-operative localization has varied from 46 to 100% [2, 4, 8]. The success rate has been dependent on the center and period of reporting. Mayo Clinic, a pioneer in insulinoma surgery, has reported a very constant overall sensitivity of about 75% with non-invasive localization modalities over different period of time whereas in recent times, addition of invasive procedures in form of EUS and ASVS (SACST) improved sensitivity of pre-operative localization. It is to note that earlier they were employing USG, triple phase CECT, and MRI as primary localizing modality [4]. Overall, EUS had a sensitivity of 75% and SACST of 93% for the localization or regionalization of [4]. The blind exploration rate at their center dropped from 26 to 0% from 1978 to 2007. Other centers also have reported an improved pre-operative localization rate over the time and similar to us have also observed improved sensitivity of CECT in insulinoma localization [2, 4, 8].
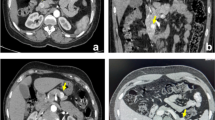
Sensitivity of CECT has improved in the last decade due to technological advances. Rapid acquisition and standardized protocol helped to improve localization and is the main reason of improved sensitivity at our institution after the year 2005. Due to increase vascularity, insulinoma appears as hyper vascular lesion in early arterial or capillary phase (Fig. 2). A few have reported similar or better results of localization with MRI but the results have not been consistent 7–71% [4, 9]. In comparison to MRI, CECT is more easily available and is an inexpensive technique. Among invasive modalities, the reported sensitivity of THVS and SASI is usually more than 95% [1, 2, 4, 9, 10]. Recently, EUS seems to be emerging as modality of choice in many centers and these report very high sensitivity particularly for the insulinoma located in the head and body [4, 11, 12]. But it is important to remember that these modalities require a high degree of technical expertise and are available in limited centers and the results could not be easily reproducible. We do not have much experience in utilizing this modality and expertise is still evolving. Some studies have reported success with Ga-68 DOTANOC PET/CT scan, since majority of insulinoma do not express somatostatin receptors, the success remain varied [9, 12, 13]. Therefore, essentially the choice of modality to be employed would be dictated by the availability of technology and expertise at a particular center.
Notwithstanding the imperfect pre-operative localization, the success of surgery varies from 95 to 100% in experienced hand. Bi-digital palpation in experience hands has been reported to detect 95% insulinoma. With the addition of IOUSG, the success ranges between 98 and 100%. The same finding was observed in the current study. But despite good results of surgery, improvement in pre-operative localization technique is much desirable. An accurate pre-operative localization would help in reducing operation time, boost surgeons’ confidence, reduce incidence of blind resection, and greatly help in planning laparoscopic enucleation and/or resection [2,3,4, 14]. With the evolution of minimal invasive surgery, some centers have reported small series of laparoscopic resection of insulinoma [14]. Though pancreatic fistula rate following open or laparoscopic removal of insulinoma remains comparable, patients are likely to have easy convalescence following minimal invasive surgery. As the patients’ positioning for laparoscopic surgery vary with the region of pancreas to be operated (head, body, and tail) and bi-digital palpation is not an option, pre-operative localization seems to be absolutely necessary before intervening. Laparoscopic USG could guide but even then, issue of patient positioning remains [3, 14]. But despite all the current advances in imaging, ICH still poses problem and in case of non-localization, we are not sure if we are missing a small insulinoma or are dealing with ICH. In this scenario, regionalization with ASVS and THVS could help in taking decision for gradient driven resection during the first surgery itself thus avoiding failed exploration or blind resections [4].
The strength of current study is that it reports a series of patients who have a constant pre-operative protocol which reports an improvement in pre-operative localization due to technological advances. The weakness is it being a retrospective study, and due to time lag, comparative sensitivity of different modality might not be a true reflection of facts. Nonetheless, insulinoma being a very rare surgical entity, our experience could contribute to developing a protocol in our own country.
Conclusion
Pre-operative localization techniques of insulinoma continue to evolve. In our experience, triple phase CECT seems to be the best single modality. Pre-operative identification of ICH remains a challenge. Experience of surgeon aided by IOUS results in successful surgery even in almost all patients.
Data Availability
Data is property of the Institute and would be made available on specific request.
Code Availability
Not applicable.
References
Boukhman MP, Karam JH, Shaver J, Siperstein AE, Duh QY, Clark OH (1998) Insulinoma—experience from 1950 to 1995. West J Med 169:98–104
Pasieka JL, McLeod MK, Thompson NW (1992) Surgical approach to insulinomas: assessing the need for preoperative localization. Arch Surg 127:442–447. https://doi.org/10.1001/archsurg.1992.01420040088015
Abboud B, Boujaoude J (2008) Occult sporadic insulinoma: localization and surgical strategy. World J Gastroenterol 14:657–665
Placzkowski KA, Vella A, Thompson GB, Grant CS, Reading CC, Charboneau JW, Andrews JC, Lloyd RV, Service FJ (2009) Secular trends in the presentation and management of functioning insulinoma at the Mayo Clinic, 1987–2007. J Clin Endocrinol Metab 94:1069–73. https://doi.org/10.1210/jc.2008-2031
Agarwal A, Mishra SK, Baijal SS, Agarwal G (1997) Intraoperative ultrasonography for insulinoma: a preliminary experience. Indian J Gastroenterol 16:58–59
Hashimoto LA, Walsh RM (1999) Preoperative localization of insulinomas is not necessary. J Am Coll Surg 189:368–373
Daggett PR, Goodburn EA, Kurtz AB, Le Quesne LP, Morris DV, Nabarro JD, Raphael MJ (1981) Is preoperative localisation of insulinomas necessary? Lancet 1:483–486
Nikfarjam M, Warshaw AL, Axelrod L, Deshpande V, Thayer SP, Ferrone CR, F-del CC (2008) Improved contemporary surgical management of insulinomas: a 25-year experience at the Massachusetts General Hospital. Ann Surg 247:165–172. https://doi.org/10.1097/SLA.0b013e31815792ed
Shin JJ, Gorden P, Libutti SK (2010) Insulinoma: pathophysiology, localization and management. Future Oncol 6:229–237. https://doi.org/10.2217/fon.09.165
Zhao K, Patel N, Kulkarni K, Gross JS, Taslakian B (2020) Essentials of insulinoma localization with selective arterial calcium stimulation and hepatic venous sampling. J Clin Med 9:3091. https://doi.org/10.3390/jcm9103091
Sotoudehmanesh R, Hedayat A, Shirazian N, Shahraeeni S, Ainechi S, Zeinali F, Kolahdoozan S (2007) Endoscopic ultrasonography (EUS) in the localization of insulinoma. Endocrine 31:238–241
Jyotsna VP, Pal S, Kandasamy D, Gamanagatti S, Garg PK, Raizada N, Sahni P, Bal CS, Tandon N, Ammini A (2016) Evolving management of insulinoma: experience at a tertiary care centre. Indian J Med Res 144:771–777. https://doi.org/10.4103/ijmr.IJMR_1477_14
Nockel P, Babic B, Millo C, Herscovitch P, Patel D, Nilubol N, Sadowski SM, Cochran C, Gorden P, Kebebew E (2017) Localization of insulinoma using 68Ga-DOTATATE PET/CT scan. J Clin Endocrinol Metab 102:195–199. https://doi.org/10.1210/jc.2016-3445
Arbuckle JD, Kekis PB, Lim A, Jackson JE, Todd JF, Lynn J (2009) Laparoscopic management of insulinomas. Br J Surg 96:185–190
Acknowledgements
A part of this study was presented as poster at the 47th World Congress of Surgery (WCS 2017) held at Basel, Switzerland, from August 13 to 17, 2017.
Author information
Authors and Affiliations
Contributions
Anjali Mishra: (1) conception and design of the study, acquisition of data, and analysis and interpretation of data, (2) drafting the article and revising it critically for important intellectual content, (3) final approval of the version to be submitted. Zafar Neyaz: (1) Intra-operative Ultrasound, acquisition and analysis of imaging data (2) revising manuscript critically for important intellectual content, (3) final approval of the version to be submitted. Subhash Yadav: (1) conception and design of the study, and analysis and interpretation of data, (2) revising the article critically for important intellectual content, (3) final approval of the version to be submitted. Archana Gupta: (1) conception and design of the study and analysis and interpretation of data, (2) revising the article critically for important intellectual content, (3) final approval of the version to be submitted. Eesh Bhatia: (1) acquisition and analysis of data (2) revising the article critically for important intellectual content, (3) final approval of the version to be submitted. Saroj Kanta Mishra: (1) the conception and design of the study (2) revising the article critically for important intellectual content, (3) final approval of the version to be submitted.
Corresponding author
Ethics declarations
Ethics Approval
Approved by the Department Research Forum.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
The manuscript publication is approved by all authors and by the responsible authorities where the work was carried out.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mishra, A., Neyaz, Z., Yadav, S. et al. Outcome of Pre-operative vs Intraoperative Localization Techniques in Insulinoma: Experience in a Tertiary Referral Center. Indian J Surg (2022). https://doi.org/10.1007/s12262-022-03569-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12262-022-03569-z