Abstract
We present two cases of Bouveret Syndrome managed conservatively with endoscopic holmium laser lithotripsy. Two elderly patients with gastric outlet obstruction caused by gallstone migration into the duodenum through a cholecystoduodenal fistula underwent endoscopic holmium laser lithotripsy. The procedure was performed under general anaesthesia in the operating theatre using a holmium laser probe and a standard gastroscope. In both patients, complete fragmentation of the obstructive gallstone was achieved. Following the treatment, the first patient was asymptomatic and due to multiple co-morbidities, definitive surgery with cholecystectomy was not deemed appropriate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bouveret’s syndrome (BS) is gastric outlet obstruction due to an impacted gallstone in the duodenum or the pylorus following its migration through a cholecystoduodenal fistula. It is a very rare complication of gallstone disease [1,2,3]. In patients with high surgical risk and suspicion of underlying biliary malignancy, endoscopic therapy can be used as a first-line treatment [1]. We present two cases of Bouveret syndrome treated with endoscopic holmium laser lithotripsy (EHLL).
Patients and Methods
Patients
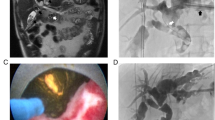
Two patients diagnosed with BS underwent EHLL. The first patient was a 76-year-old man with multiple co-morbidities including type 2 diabetes, hypertension, atrial fibrillation and ischaemic heart disease. The patient had presented 2 months earlier with acute cholecystitis that was managed conservatively with a cholecystostomy, which subsequently became dislodged after two weeks. Six weeks later, he was re-admitted with epigastric pain and vomiting. A computed tomography (CT) scan of his abdomen and pelvis reported recurrent cholecystitis and the suspicion of a large gallstone compressing the gastric outlet which was fistulating towards the duodenum. The radiological findings were subsequently confirmed on gastroscopy (Fig. 1). The second patient was an 80-year-old woman with a medical history significant for hypertension, arthritis and bilateral knee and left hip replacements, who presented with a 2-week history of epigastric pain, vomiting and weight loss of 32 kg. A CT scan demonstrated gallbladder wall thickening with possible communication to the pylorus with a large eroding calculus which was causing gastric outlet obstruction. Furthermore, soft tissue extension from the gallbladder to the hepatic flexure was noted and several hypodense hepatic lesions adjacent to the gallbladder were observed. Gastroscopy diagnosed an impacted gallstone in the pylorus with surrounding ulceration, which was not amenable to endoscopic retrieval. We have previously described the laser-assisted-bile-duct-exploration-by-laparoendoscopy (LABEL) procedure for complex (large and/or impacted) choledocholithiasis [4]. The reported outcomes have demonstrated that this procedure is highly efficacious and safe. Therefore, following the same technical principles, EHLL was proposed as the management strategy in both patients.
Endoscopic Laser Lithotripsy
Both patients underwent EHLL of the impacted, obstructing gallstone and were consented following national guidelines. The procedure was performed in an operating theatre under general anaesthesia with orotracheal intubation. The patient was positioned in supine position, strapped to the operating table at the level of the thighs and placed in reverse Trendelenburg with right lateral tilt. A 10.9-mm gastroscope (Olympus, Melville, New York, USA) with a single 3.7-mm working channel was used. Initial gastroscopy was performed to assess the upper gastrointestinal anatomy and identify the offending stone. Holmium laser lithotripsy (HLL) requires a liquid medium to transmit the energy from the laser probe to the stone and therefore an Olympus irrigation system, operated by foot pedal, was connected to the gastroscope to fill in the duodenum and stomach with saline facilitated by the reverse Trendelenburg position with right lateral tilt. Continuous irrigation also helped stone fragments to be flushed distally into the duodenum. The anaesthetist performed regular aspirations through the nasogastric tube in order to minimise the risk of airway aspiration. A 200 to 365-µm holmium laser fibre (ScopeSafe™, Optical Integrity, Florida, USA) was introduced through the working channel of the gastroscope. The generator was initially set at 0.5 J and 5 Hz (2.5 W). The tip of the probe with the light diode was positioned to target the stone under continuous irrigation in order to start the procedure (Fig. 2). Lithotripsy was performed until the impacted stone was fragmented into smaller pieces that could be flushed distally to the duodenum. It is important that the fragments are small enough (less than 2–2.5 cm) to prevent distal small bowel obstruction [5]. After complete fragmentation and clearance of debris, the impacted mucosa and remaining duodenal anatomy were assessed and biopsies taken. The nasogastric tube was removed after the procedure in both patients.
Results
The two patients with BS were treated successfully with EHLL. The high content of calcium within the stones resulted in a lengthy lithotripsy procedure. The duration of the procedure was 6 hours in the first case and 2 hours in the second. Three laser fibres were used in the first patient, and one in the second. There was minor post-operative morbidity in both patients. The first patient, with known atrial fibrillation, was observed to have fast atrial fibrillation immediately post-procedure (Clavien-Dindo II), which resolved with pharmacological measures. He tolerated a soft diet from the first post-procedural day and was discharged on the seventh post-procedure day. There was no recurrence of gallstone-related complications during the follow-up period of 20 months. Due to his multiple co-morbidities, the risk of surgery was deemed to outweigh any potential benefit, and therefore, he was not subsequently scheduled for elective cholecystectomy. The second patient developed gastroparesis following the procedure, which required prokinetic medication (Clavien-Dindo I). Her oral intake was progressively increased until she was able to tolerate a soft diet. Biopsies taken during the procedure did not show dysplasia or invasive malignancy; however, due to the ongoing suspicion of an underlying malignancy, further investigations were performed. Subsequent imaging and histology from liver biopsies supported a diagnosis of epithelioid angiosarcoma, most likely arising from the gallbladder. Endoscopic stenting of the pylorus was subsequently undertaken and the patient was referred to oncology and palliative care services.
Discussion
BS is a rare complication of cholelithiasis with gastric outlet obstruction caused by a gallstone migrating through a fistula between the gallbladder and either the duodenum or stomach (1–3% of gallstone ileus) [1, 2, 5,6,7]. It was first described in 1770 by Beaussier and later published in two case reports diagnosed pre-operatively by Bouveret in 1896 [6, 8]. More than 70% occur in patients over 70 years old, usually with multiple co-morbidities. Factors that favour bilio-enteric fistula formation are gallstone size (2–8 cm), long-standing biliary disease, recurrent cholecystitis, female sex, and age 60–80 years [2, 8]. Potential long-term complications of bilio-enteric fistulas include biliary infection and gallbladder cancer (15%) [2]. This condition remains difficult to diagnose as the symptoms are nonspecific and the physical examination findings may be subtle [3, 5, 6]. It must be suspected in elderly patients with a previous history of chronic calculous cholecystitis, and abdominal pain of sudden onset mainly in the epigastrium and right upper quadrant accompanied by nausea, vomiting and fever [9]. Early diagnosis can be achieved using abdominal CT in the emergency setting showing Rigler’s triad (dilated stomach, pneumobilia and a gallstone, present only in 50% of cases) [2, 3, 9]. MRCP has high diagnostic value as it can detect the presence of a fistula, as well as the size and location of the stone and its relationship with the fistula [9]. Gastroscopy is needed in most cases for diagnosis, being considered the most specific diagnostic test [5]. BS can be associated with high mortality rates (12–25%), mainly due to the frailty of the patients that present with this condition [6, 8].
There are multiple available treatment modalities, including surgical and endoscopic approaches [6, 7]. However, no definitive guidelines have been proposed to manage BS. Surgical management is the most common treatment despite its high risks and complication rates (morbidity 65%, mortality 12–30%) [2, 9, 10]. In most series, patients were treated with laparotomy and stone extraction through either an enterotomy or gastrotomy [6]. Although feasible, laparoscopic management of BS is challenging, with a high chance of converting to open surgery. However, given the high morbidity and mortality (19–24%) associated with surgery, it is often more desirable to follow a more conservative approach in frail patients [11]. The first case of successful endoscopic management of BS was reported in 1985 by Begdoni, who used an endoscopic basket to remove an impacted gallstone in the duodenum [10]. In recent years, therapeutic endoscopy has been more frequently and successfully used to extract the obstructing stones [6]. Extra-corporeal lithotripsy or intra-corporeal lithotripsy (laser, electrohydraulic and mechanical), along with stone extraction using different devices, has been described in different case reports [1, 2, 5,6,7, 10, 11]. EHLL has been used successfully and safely in BS, representing an alternative to immediate surgery in unfavourable surgical candidates [1, 5]. The benefit of using EHLL is precise targeting of energy onto the stone with minimal tissue injury (morbidity 1.6%). EHLL should be considered when a large impacted, calcified stone is identified, in order to achieve complete or partial fragmentation with stone extraction or distal flushing of the smaller fragments. Furthermore, the ability to manoeuvre the various instruments (e.g. baskets, graspers, balloons, snares, nets) endoscopically to reach difficult positions is advantageous [3, 10]. EHLL is usually not indicated when smaller stones are discovered that can be mobilized with endoscopic instruments alone. One of the advantages of EHLL over electrohydraulic lithotripsy (EHL) is that all the equipment is usually already available in most hospitals due to its use within urological services. This procedure should be carried out in an operating theatre under general anaesthesia. Patients should be positioned in supine position and strapped to the operating table, allowing change in positions and rapid access to the abdomen if a complication that requires urgent surgery occurs. The gastric antrum needs to be flooded with saline because the laser can only function in a fluid environment. This can be achieved with the use of a foot activated pump, in combination with reverse Trendelenburg and right tilt position, to facilitate fluid accumulation in the obstructed antrum. If stone fragments are being flushed distally, the operating surgeon must ensure that individual pieces are smaller than the diameter of the duodenum (2–2.5 cm), in order to avoid distal gallstone ileus [1]. Recurrent gallstone ileus is a possible risk, but the benefit of minimal surgical stress outweighs this risk in high-surgical-risk patients. Moreover, doing an initial endoscopic procedure allows a more extensive study for appropriate diagnosis and staging of patients with suspicion of malignancy, avoiding a complex surgical procedure with high risk of peritoneal seeding and therefore worsening the prognosis. Failure of endoscopic treatment should be followed by surgical intervention, as the main aim of the treatment of BS is to overcome the obstruction [12]. Failures in endoscopic retrieval are usually associated with the presence of large stones where retrieval is attempted only with endoscopic instruments or just mechanical lithotripsy [9, 12]. Fragmentation of the stone with EHLL or EHL can help overcome this situation [2, 10, 11]. Ideally, this procedure should be performed in a single session, as between lithotripsy treatments, there is a risk of distal gallstone ileus if a partially fragmented stone dislodges and subsequently migrates distally. However, if this is not technically feasible or the patient does not tolerate a lengthy procedure due to their comorbidities, staged fragmentation and retrieval can be considered as reported by other authors [1, 10, 12]. Alsolaiman et al. described partial fragmentation of an impacted gallstone over two 1-h sessions [1]. In other case reports, lengthy single-stage procedures have been described [2, 10].
The management of this uncommon condition should be tailored to the patient’s clinical presentation and co-morbidities. Whenever possible, an endoscopic approach should be offered first after immediate resuscitation [6]. If that fails, surgical management for stone extraction via enterotomy or gastrotomy should be considered. It is not recommended to perform a cholecystectomy or fistula dissection in the acute setting, as this can be associated with significant morbidity and mortality [6]. Although fistula repair may be unnecessary, as these fistulas can close spontaneously in 30 to 60 days if the cystic duct is patent and residual gallstones are not present, cholecystectomy and fistula repair is recommended due to the risk of recurrent cholecystitis and gallbladder cancer (4.9%) [2]. However, in elderly frail patients with multiple co-morbidities and shorter life expectancy, the risk of post-operative morbidity and mortality outweighs the benefits of surgery, and therefore, surgery is generally not recommended [3, 12].
Conclusions
Bouveret syndrome is a rare condition but should be considered within the differential diagnosis of gastric outlet obstruction in elderly patients. Endoscopic holmium laser lithotripsy is a valid minimally invasive alternative therapy that allows resolution of the obstruction, and avoids a complex surgical procedure in elderly frail patients with multiple co-morbidities. It is a safe procedure when performed by experienced surgeons or gastroenterologists familiar with its use.
References
Alsolaiman MM, Reitz C, Nawras AT, Rodgers JB, Maliakkal BJ (2002) Bouveret’s syndrome complicated by distal gallstone ileus after laser lithotripsy using Holmium: YAG laser. BMC Gastroenterol 2:15
Futai R, Iemoto T, Inoue Y, Miki M, Abe T, Abe S, Sasaki A, Tanaka K, Yoshie T, Ose T, Morikawa T, Sanuki T (2019) Successful treatment of Bouveret syndrome by electrohydraulic lithotripsy and double balloon endoscopy. Am J Case Rep 20:1320–1324
Caldwell KM, Lee SJ, Leggett PL, Bajwa KS, Mehta SS, Shah SK (2018) Bouveret syndrome: current management strategies. Clin Exp Gastroenterol 11:69–75
Navarro-Sánchez A, Ashrafian H, Segura-Sampedro JJ, Martinez-Isla A (2017) LABEL procedure: laser-assisted bile duct exploration by laparoendoscopy for choledocholithiasis: improving surgical outcomes and reducing technical failure. Surg Endosc 31(5):2103–2108
Schweiger F, Shinder R (1997) Duodenal obstruction by a gallstone (Bouveret’s syndrome) managed by endoscopic stone extraction: a case report and review. Can J Gastroenterol 11(6):493–496
Al-Habbal Y, Ng M, Bird D, McQuillan T, Al-Khaffaf H (2017) Uncommon presentation of a common disease – Bouveret’s syndrome: a case report and systematic literature review. World J Gastrointest Surg 9(1):25–36
Duarte M, Traple F, Prado J, Scoppetta L (2020) Bouveret’s syndrome—an unusual fistula. Indian J Surg 82:2–3
Sharma D, Jakhetia A, Agarwal L, Baruah D, Rohtagi A, Kumar A (2010) Carcinoma gall bladder with Bouveret’s syndrome: a rare cause of gastric outlet obstruction. Indian J Surg 72(4):350–351
Wang F, Du ZQ, Chen YL, Chen TM, Wang Y, Zhou XR (2019) Bouveret syndrome: a case report. World J Clin Cases 7(23):4144–4149
Rogart JN, Perkal M, Nagar A (2008). Successful Multimodality endoscopic treatment of gastric outlet obstruction caused by an impacted gallstone (Bouveret’s syndrome). Diagn Ther Endosc 2008:471512
Makker J, Muthusamy VR, Watson R, Sedarat A (2015) Electrohydraulic lithotripsy and removal of a gallstone obstructing the duodenum: Bouveret syndrome. Gastrointest Endosc 81(4):1021–1022
Osman K, Maselli D, Kendi AT, Larson M (2020) Bouveret’s syndrome and cholecystogastric fistula: a case-report and review of the literature. Clin J Gastroenterol 13(4):527–531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
For this type of study, formal consent was not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 222994 KB)
Rights and permissions
About this article
Cite this article
Senra Lorenzana, F.S., Navaratne, L., Liasis, L. et al. Endoscopic Holmium Laser Lithotripsy (EHLL) as an Alternative Minimally Invasive Therapy to the Surgical Management of Bouveret Syndrome. Indian J Surg 85, 131–134 (2023). https://doi.org/10.1007/s12262-022-03350-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-022-03350-2