Abstract
We present a case of successful minimally invasive treatment of a completely obstructed rectal anastomosis by using a transanal plasmakinetic resectoscope, along with a review of the relevant literature. A 75-year-old man underwent low anterior resection for rectal cancer. Complete obstruction of the rectal anastomosis was visualized at 6.0 cm from the anal verge, 5 months later. We carefully cut at the center of the circular staple line to find the orifice of anastomosis with a plasmakinetic resectoscope. Then, a sufficient amount of fibrotic tissue at the stenosis was resected to maintain the continuity of the bowel. At 4 months follow-up, the patient had complete resolution of symptoms. Transanal plasmakinetic resection is a possible choice for treatment of a completely obstructed colorectal anastomosis. However, these techniques have risks and should be implemented with great caution in selected patients by skilled endoscopists or surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Benign anastomotic stenosis occurs in up to 22% of patients after lower rectal surgeries for rectal cancer [1]. However, completely obstructed anastomosis after rectal resection is rare, so the treatment measures depend on each individual’s situation [2,3,4,5,6,7,8,9,10,11,12]. Completely obstructed anastomosis normally needs conventional redo surgery, but redo surgery is invasive and does not eliminate the risk of recurrence [1, 2, 13]. Thus, modified minimally invasive treatment strategy is attractive, and it has been successfully performed in some cases [3,4,5,6,7,8,9,10,11,12]. Plasmakinetic resectoscope is widely used for transurethral resection of prostate. Here, we discuss a case of a completely obstructed anastomosis after low anterior resection (LAR), which has been successfully treated utilizing transanal plasmakinetic resection of massive scar tissue in the anastomotic site, together with a review of the relevant literature.
Case Report
A 75-year-old man underwent LAR for rectal cancer. Three months later, he developed an anastomotic stenosis due to postoperative leakage and pelvic infection, and then endoscopic balloon dilatation was performed several times with minimal success. The placement of a rectal stent alleviated the symptom, but the symptom did not resolve completely. Finally, the patient was referred to our hospital for treatment, 5 months after LAR.
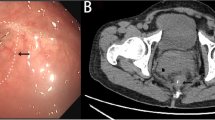
The patient’s BMI was 23.4 kg/m2. Computed tomography showed that the thick membranous web was present around a tiny orifice (rectal stent) (Fig. 1a). Subsequent fluoroscopy indicated that the colorectal anastomosis was almost completely obstructed (Fig. 1b). During fluoroscopy, the rectal stent was removed. Although surgical revision was considered, the patient was strongly against undergoing redo surgery. In addition, because of significant risk of postoperative morbidity, redo surgery should be the last resort.
Findings of the computed tomography and fluoroscopy 5 months after low anterior resection. Computed tomography showed that well-enhanced tissue was present around a tiny orifice (rectal stent) (white arrow), suggesting that patency of the anastomosis was almost discontinued by the thick membranous web (a). Fluoroscopy showed that the colorectal anastomosis was almost completely occluded (black arrow) (b)
The procedures were done in the modified lithotomy position. One experienced urologist carried out all procedures accompanied by a colorectal surgeon in this case. Routine disinfection was conducted, and sterile drapes were applied. The plasmakinetic resectoscope (Simai Corp., Zhuhai, China) with ring electrode was used (Fig. 2). The resection power was set at 120 W, and the coagulating power was set at 80 W. A plasmakinetic resectoscope with outer sheath of Fr 26 was used.
Normal saline continuously irrigated the operative field throughout the surgical procedures. We first introduced the resectoscope into the rectum to assess the stenosis. The anastomotic stricture was visualized at 6.0 cm from the anal verge. We could not identify any orifice at the anastomotic site, so the diagnosis of completely obstructed colorectal anastomosis was established (Fig. 3). We carefully cut at the center of the circular staple line where it also has a different appearance from the normal mucosal tissue around (Fig. 3). About 5-mm-thick scar tissues were removed, and then the orifice of anastomosis was found (Fig. 4a). The resectoscope could easily pass through the orifice after the marginal scar tissues were fully trimmed with surrounding staples removed. The luminal continuity was finally reestablished with a wide anastomotic site of 3.0 cm in diameter (Fig. 4b). A clear surgical field was easily maintained (Fig. 4c), and an F22 drainage tube was indwelled inside (Fig. 4d). Totally 20 g scar tissue was taken out and sent for histopathological examination. There was little bleeding during and after surgery.
Resectoscopic appearance of the anastomotic ring. A completely obstructed anastomosis at 6 cm from the anal verge was identified. The expected location of the circular stapler ring is shown by dotted black line. The center of the circular stapler line was the expected position of the lumen which was also different from normal mucosal tissue around (white arrow)
The patient received cephalosporin antibiotics once during operation. Intacted protein enteral nutrition power (Nutrison, Milupa GmbH, Fulda, Germany) was given orally with only clear fluids for two days after surgery. The patient had an uneventful recovery without sign of bleeding or perforation and then was discharged on the 7th postoperative day without any complication. Two months after surgery, the patient underwent endoscopic balloon dilatation. One month later, the patient had complete resolution of symptoms. Written consent of publishing of this paper was obtained from the patient when he was discharged.
Discussion
Lower rectal surgeries with colorectal anastomosis are complicated by benign anastomotic strictures in between 3 and 30 percent of patients [1]. The apparent heterogeneity may be associated with various anastomotic stenosis definitions used. Complete obstruction of colorectal anastomosis is rare, so treatment consensus is unavailable for this condition. Therefore, reporting new cases is necessary for sharing useful experiences. In this condition, abdominal redo surgery has a satisfactory success rate, but it is too invasive [1, 2, 13], so the minimally invasive surgery is favored.
Minimally invasive surgery for completely obstructed anastomosis has a particular challenge, because it has a significant risk of bowel perforation to cross the occluded part to reestablish luminal continuity. Here, we report a successful treatment of completely obstructed anastomosis after LAR using transanal plasmakinetic resectoscope. We list several valuable and unique aspects of the successful treatment:
-
1.
Easy accessibility to the rectum, minimal invasion and direct vision under resectoscope. It is hard to implement local treatment in the rectum because of the pelvis anatomical structure, especially when the lesion is at a distance from the anal verge. A plasmakinetic resectoscope enables optimal visual control and provides a superior operative field without light backscatter and smoke, while working in a rectum distended with normal saline.
-
2.
Excellent vaporizing and coagulating properties. The plasmakinetic resectoscope actually performs tissue resection at lower temperatures with a lower voltage, so there is less thermal injury to the adjacent tissues. The excellent coagulating property of plasmakinetic resectoscope significantly reduces the intraoperative blood loss.
-
3.
Excision of massive scar tissue and removal of staples. It has been proven that the circular end-to-end stapled anastomosis used for LAR is a risk factor for stenosis [14]. Most benign anastomotic strictures are consequent to cicatricial response including proliferation of fibroblasts and cross-linking of collagen fibers [15, 16]. Transanal plasmakinetic resectoscope enables precise incision, adequate excision of massive scar tissue, and removal of staples at the anastomotic site. Therefore, it can be better at preventing recurrence of stricture than other methods.
-
4.
Reduced instrumentation compared with transanal minimally invasive surgery (TAMIS) [3]. The entire procedure is implemented using a plasmakinetic resectoscope, without the requirement for standard laparoscopic instruments, instrument exchange, or insufflation with CO2 gas.
-
5.
We regain the luminal continuity by cutting at the center of the circular staple line using a plasmakinetic resectoscope under direct visualization without guidance of fluoroscopy. The position of the proximal lumen must be accurately confirmed. We share our experience associated with precise identification of the luminal position under direct visualization. However, it must be emphasized that this technique should be implemented by highly experienced surgeons.
There have been 10 studies about successful minimally invasive treatment of completely obstructed colorectal anastomosis in the literature [3,4,5,6,7,8,9,10,11,12]. Characteristics of these case reports are listed in Table 1. The reason for complete obstruction is unclear. Complete obstruction of colorectal anastomosis is rare, so treatment consensus is unavailable, and the treatment depends on each individual’s situation.
Artifon Catheter Puncture and Blunt Penetration Technique Before Balloon Dilation
In the two cases, specialized devices for other particular purposes are utilized to reestablish the luminal continuity. Curcio et al. insert a suprapapillary biliary puncture catheter (Artifon catheter) into the center of the circular staple line at the level of the anastomosis to restore the continuity under endoscope, and then they used this Artifon catheter to inject dye to identify the proximal bowel; then a guide wire on which to implement balloon dilation is inserted through the Artifon catheter [4]. Yazawa et al implement the similar technique with a device designed as a transanal drainage system for obstructing colorectal cancer [5]. This commercially available device has a blunt tip, so it is impossible to injure organs outside the bowel even if misdirected thrust occurs. But if the membranous web composed in the anastomotic ring is too thick or firm to be inserted through by this blunt tip device, this technique is not effective. These two techniques are thought to be superior to other methods using electrocision in avoiding thermal injuries.
Endoscopic Incision Before Balloon Dilation
Yuan et al claim. that the combination of endoscopic small incision and balloon dilation is an effective and safe technique for completely obstructed colorectal anastomosis. They use a needle knife to make a small incision at the expected position of the lumen to restore the luminal continuity under direct visualization; then the stenosis is dilated utilizing a wire-guided balloon dilator [6]. Single electrocautery incision is associated with high risk of perforation or bleeding and may result in scar contraction [17, 18]. Nonsurgical treatment for complete obstruction of colorectal anastomosis is almost always conducted under fluoroscopic guidance. This method of accurate identification of the luminal position under direct visualization is similar with ours.
Endoscopic Rendezvous Technique
The endoscopic rendezvous technique has been reported for dilating complex esophageal stenosis [19, 20]. Kaushik et al. successfully apply this technique in the treatment of a complete obstruction of colorectal anastomosis [7]. One colonoscope is advanced to the anastomosis through the loop ileostomy. The other endoscope is advanced to the anastomosis transanally in a retrograde fashion. Under fluoroscopic and transilluminated guidance, a 19-gauge EUS needle is pushed through the membranous web and is visualized by the opposing colonoscope. A guide wire is advanced through the needle and captured proximally by the opposing colonoscope, allowing for subsequent wire-guided dilation. This endoscopic rendezvous technique requires two endoscopists and two colonoscopes.
The similar techniques named CT-guided endoscopic rendezvous technique and ultrasonography-guided endoscopic rendezvous recanalization have been also reported [8,9,10,11]. Identification of the obstructed anastomosis is occasionally unlikely under conventional fluoroscopy in complex situations. CT fluoroscopy or endoscopic ultrasonography guidance allows the endoscopist to visualize the obstructed anastomosis and the position of the endoscopes three-dimensionally. In three cases, after endoscopic dilation, a lumen-apposing metal stent is deployed across the fistula [9,10,11]. Limitations of this rendezvous technique include instrument exchange, a second endoscopy unit, and a pre-existing ostomy.
Guidance with Prototype Front-View Echoendoscope
Minimally invasive recanalization of complete obstruction of colorectal anastomosis is implemented almost always under fluoroscopic guidance [3,4,5, 7,8,9,10,11]. Lusong et al. present a case of successful recanalization of a complete obstruction of colorectal anastomosis with a prototype front-view and forward-array echoendoscope [12]. Real-time EUS imaging guides penetration through the stricture. SpyGlass fiberoptic probe visualization is used to confirm the access into the proximal obstructed segment. Subsequent wire-guided balloon dilator is implemented through the instrument channel of the prototype echoendoscope to dilate the stricture. The entire procedure is implemented with a single endoscope, without instrument exchange or the risk of losing wire access. The limitation of this technique is that the prototype front-view and forward-array echoendoscope is not a ubiquitous device.
Transanal Minimally Invasive Surgery
As a relatively new method, transanal minimally invasive surgery (TAMIS) is designed on a platform which is readily available in most operating suites, bringing access for more proximal rectal lesions [21]. Bong et al. have described their experience utilizing TAMIS to successfully treat a complete obstruction of colorectal anastomosis after LAR [3]. The proximal lumen position is identified with contrast medium, and then the occluded lumen is incised by electrocautery. After adequate excision of fibrotic tissue at the stricture, the continuity of the bowel is established. The entire procedure requires standard laparoscopic instruments, instrument exchange, and insufflation with CO2 gas. There is no sign of bleeding or perforation after surgery.
TAMIS has a wide application besides local excision, including repair of rectovaginal/rectourethral fistula, ligation of hemorrhage in distal rectum, removal of colorectal foreign body, total mesorectal excision for rectal cancer, and suture closure of an anastomotic leakage [22,23,24,25]. Therefore, if perforation occurs, it can be repaired in time by TAMIS. This report shows that TAMIS is safe and feasible for the treatment of complete anastomotic occlusion.
Transanal plasmakinetic resection is a valid and safe technique for treatment of a complete obstruction of colorectal anastomosis after low anterior resection. With the development of minimally invasive procedures, many boundaries have been pushed to set up less invasive techniques which have minimal surgical trauma, equivalent clinical results, and improved patient satisfaction. However, the luminal position must be accurately confirmed, and these procedures must be performed carefully in selected patients by skilled surgeons or endoscopists. During the procedure, the surgeon or endoscopist should always be prepared for bleeding or perforation, and conventional surgery should be available whenever necessary.
References
Luchtefeld MA, Milsom JW, Senagore A, Surrell JA, Mazier WP (1989) Colorectal anastomotic stenosis. Results of a survey of the ASCRS membership. Dis Colon Rectum 32:733–736
Lefevre JH, Bretagnol F, Maggioni L et al (2011) Redo surgery for failed colorectal or coloanal anastomosis: a valuable surgical challenge. Surgery 149:65–71
Bong JW, Lim SB (2019) Transanal minimally invasive surgery as a treatment option for a completely occluded anastomosis after low anterior resection: a new approach to severe anastomotic stenosis. Asian J Endosc Surg 12:175–177
Curcio G, Spada M, di Francesco F, Tarantino I, Barresi L, Burgio G, Traina M (2010) Completely obstructed colorectal anastomosis: a new nonelectrosurgical endoscopic approach before balloon dilatation. World J Gastroenterol 16:4751–4754
Yazawa K, Morioka D, Matsumoto C et al (2014) Blunt penetration technique for treatment of a completely obstructed anastomosis after rectal resection: a case report. J Med Case Rep 8:236
Yuan X, Liu W, Ye L, Wu M, Hu B (2019) Combination of endoscopic incision and balloon dilation for treatment of a completely obstructed anastomotic stenosis following colorectal resection: a case report. Medicine (Baltimore) 98:e16292
Kaushik N, Rubin J, McGrath K (2006) Treatment of benign complete colonic anastomotic obstruction by using an endoscopic rendezvous technique. Gastrointest Endosc 63:727–730
Albertsmeier M, Rittler P, Hoffmann RT, Spelsberg F (2011) Treatment of a completely obstructed colonic anastomotic stricture using a CT-guided endoscopic rendezvous technique. Endoscopy 43(Suppl 2 UCTN):E5–E6
Poincloux L, Pezet D, Rouquette O (2016) Successful recanalization of complete anastomotic stricture using colorectal endoscopic ultrasound-guided rendezvous thus allowing stoma reversal: two cases. Endoscopy 48(S 01):E353–E354
Sanaei O, Ngamruengphong S, Chen YI, Bukhari M, Brewer Gutierrez O, Kumbhari V, Khashab MA (2017) Endoscopic ultrasonography-guided freestyle rendezvous recanalization of a complete postoperative rectosigmoid anastomotic obstruction with a lumen-apposing metal stent. Endoscopy 49:E206–E207
Gornals JB, Albines G, Trenti L, Mast R, Frago R (2015) EUS-guided recanalization of a complete rectal anastomotic stenosis by use of a lumen-apposing metal stent. Gastrointest Endosc 82(4):752
De Lusong MA, Shah JN, Soetikno R et al (2008) Treatment of a completely obstructed colonic anastomotic stricture by using a prototype forward-array echoendoscope and facilitated by SpyGlass. Gastrointest Endosc 68:988–992
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kawada K, Sakai Y (2016) Preoperative, intraoperative and postoperative risk factors for anastomotic leakage after laparoscopic low anterior resection with double stapling technique anastomosis. World J Gastroenterol 22:5718–5727
Oz MC, Forde KA (1990) Endoscopic alternatives in the management of colonic strictures. Surgery 108:513–519
Ravo B (1988) Colorectal anastomotic healing and intracolonic bypass procedure. Surg Clin North Am 68:1267–1294
Kwon YH, Jeon SW, Lee YK (2013) Endoscopic management of refractory benign colorectal strictures. Clin Endosc 46:472–475
Hagiwara A, Sakakura C, Shirasu M, Torii T, Hirata Y, Yamagishi H (1999) Sigmoidofiberscopic incision plus balloon dilatation for anastomotic cicatricial stricture after anterior resection of the rectum. World J Surg 23:717–720
McGrath K, Brazer S (2002) Combined antegrade and retrograde dilation: a new endoscopic technique in the management of complex esophageal stricture [comment]. Gastrointest Endosc 56:163
Baumgart DC, Veltzke-Schlieker W, Wiedenmann B, Hintze RE (2005) Successful recanalization of a completely obliterated esophageal stricture by using an endoscopic rendezvous maneuver. Gastrointest Endosc 61:473–475
Lee BC, Oh S, Lim SB, Yu CS, Kim JC (2017) Transanal minimally-invasive surgery for treating patients with regressed rectal cancer after preoperative chemoradiotherapy. Ann Coloproctol 33:52–56
Nepal P, Mori S, Kita Y, Tanabe K, Baba K, Uchikado Y, Kurahara H, Arigami T, Sakoda M, Maemura K, Natsugoe S (2019) Radial incision and cutting method using a transanal approach for treatment of anastomotic strictures following rectal cancer surgery: a case report. World J Surg Oncol 17:48
Nepal P, Mori S, Kita Y, Tanabe K, Baba K, Sasaki F, Nasu Y, Ido A, Uchikado Y, Kurahara H, Arigami T, Sakoda M, Maemura K, Natsugoe S (2019) Combined endoscopic submucosal dissection and transanal minimally invasive surgery for the management of lower rectal adenoma extending above the dentate line: a case report. Medicine (Baltimore) 98:e15289
Caycedo-Marulanda A, Jiang HY, Kohtakangas EL (2017) Transanal minimally invasive surgery for benign large rectal polyps and early malignant rectal cancers: experience and outcomes from the first Canadian centre to adopt the technique. Can J Surg 60:416–423
Atallah S, Albert M, Debeche-Adams T, Larach S (2013) Transanal minimally invasive surgery (TAMIS): applications beyond local excision. Tech Coloproctol 17:239–243
Funding
This study was supported by the First Hospital of Jilin University.
Author information
Authors and Affiliations
Contributions
Jinguo Wang was the lead investigator, drafted the article, and performed the surgery and revised the manuscript; Na Wang drafted the article, reviewed the literature, and revised the manuscript; Daguang Wang reviewed the literature, drafted the article, and made critical revisions to the manuscript; Weihua Tong was the assistant surgeon, drafted the article, collected the patient’s information, and gave the final approval of the manuscript.
Corresponding author
Ethics declarations
We have obtained Institutional Ethics approval and written informed consent to participate this study and to publish this paper from the patient.
Conflict of Interest
The authors declare that they have no conflict of interest.
There is no part of this article presented in conference proceedings. I hereby certify that this paper consists of original, unpublished work which is not under consideration for publication elsewhere.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(MP4 34463 kb).
Rights and permissions
About this article
Cite this article
Wang, N., Wang, D., Tong, W. et al. Minimally Invasive Treatment of a Completely Obstructed Rectal Anastomosis by Using a Transanal Plasmakinetic Resectoscope: a Case Report and Review of Literature. Indian J Surg 83, 1127–1133 (2021). https://doi.org/10.1007/s12262-020-02674-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02674-1