Abstract
Various modifications of the reconstruction following pancreaticoduodenectomy (PD) have been described. Pancreaticogastrostomy (PG) was first described clinically by Waugh and Clagett from the Mayo Clinic in 1946. Despite recent randomized trials and meta-analysis, the literature is still ambiguous as to which is a safer procedure. We hereby describe our experience of more than 400 pancreaticogastrostomies. The legacy of performing only pancreaticogastrostomy (PG) started by the senior author (BMLK) continued from 1977 to date in this surgical unit of a tertiary care hospital. We present the results of this case series analysis of a total of 467 Whipple’s pancreaticoduodenectomy in whom PG was performed. The mean operative time was 260.8 ± 50.3 min (180–390 min) with an average blood loss of 1068 ± 606.19 ml (400–2600 ml). None of the patients had clinically significant POPF. Thirty-five patients had postoperative bleeding out of which 12 were early and 23 had delayed hemorrhage. The most common postoperative complication was delayed gastric emptying which was seen in 96 patients (20.5%). Transient bile leak was seen in 84 patients (18%). Wound infection was seen in 70 (15%) patients. The overall 30-day mortality was 2% (10 out of 400). PG as a reconstructive technique is a safe option following PD with minimal incidence of clinically significant postoperative pancreatic fistula (POPF) as shown in our series of more than 400 patients. This is the largest series to date of pancreaticogastrostomy following PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreaticoduodenectomy remains the treatment of choice for periampullary malignancies. Advances in pancreatic surgery techniques and perioperative care have led to reduced mortality rates for pancreaticoduodenectomy (PD) in high-volume centers. However, morbidity after pancreatic resection remains high, with 30–60% of patients experiencing complications following surgery, mainly as a result of leak and subsequent fistula from the pancreatic anastomosis.
Uncontrolled leak from the pancreatic anastomosis is associated with substantial complications that can start a downward spiral of sepsis, multiorgan failure, and even death. Consequently, multiple strategies have been implemented in order to decrease the leak from pancreatic anastomosis. These include different suturing techniques; options for external and internal drainage; topical sealants; and pharmacologic prophylaxis, including octreotide. Another factor evaluated is the luminal organ to which the pancreas is anastomosed. The two main options are pancreaticojejunostomy (PJ) and pancreaticogastrostomy (PG). The abundance of literature on this issue reflects the ongoing controversy regarding the optimal method of pancreatic anastomosis. This discussion has produced 10 randomized clinically trials (RCTs) (from 1990 to 2016) and at least 14 systematic reviews with meta-analysis data (from 2007 to 2016) however with conflicting results. In fact, this has generated more confusion than answers, and the question remains open: is pancreaticogastrostomy (PG) better than pancreaticojejunostomy (PJ) in avoiding postoperative pancreatic fistula (POPF)? Nevertheless, a position statement of the International Study Group of Pancreatic Fistula (ISGPF) has recently noted that the dilemma “PG versus PJ” cannot be resolved due to the “high heterogeneity” found in the studies. Though there are case series on pancreaticojejunostomy but the data on pancreaticogastrostomy is limited. Most of the studies have reported small number of patients and limited follow-up. We hereby describe our experience of 467patients who underwent PD with PG as a reconstructive technique which is the largest single center experience of PG reported to date.
Patients and Methods
The legacy of performing only pancreaticogastrostomy (PG) started by the senior author (BMLK) continued from 1977 to date in this surgical unit of a tertiary care hospital. The demographic profile, clinical profile, preoperative imaging findings, and preoperative biochemical profile were recorded in a prestructured pro forma. Preoperative histopathological diagnosis if available was also included. Preoperative biliary stenting was done in patients with cholangitis, severe malnutrition, and serum bilirubin > 15 mg/dl.
Procedure of PD
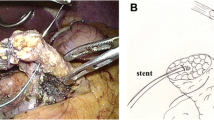
All patients were kept on liquid diet for 24 h prior to surgery and nil per mouth overnight. Pharmacological bowel preparation was done. Prophylactic broad spectrum antibiotic was given at the time of induction. From the year 2001 onwards, staging laparoscopy was performed in all patients to look for any ascites, peritoneal, or liver deposits. In absence of any metastatic disease, laparotomy was done via either a Chevron incision or a midline laparotomy. The tumor was assessed for resectability and if resectable, a standard pancreaticoduodenectomy was done. The pancreatic stump was managed by a pancreaticogastrostomy in all patients. The pancreatic stump was mobilized along the splenic vein for 3–4 cm and the pancreatic duct was identified and cannulated. Hemostatic sutures with 3-0 polypropylene were placed on the cut end of the pancreatic stump. This step was done in the latter half of our experience resulting in few patients with bleeding from the pancreatic stump in the postoperative period. PG was done in 4 layers. The first layer was made with non-absorbable sutures between the seromuscular layer of stomach and the anterior pancreatic capsule. A transverse gastrotomy was made in the posterior wall of the stomach and the pancreatic stump was telescoped into the stomach taking care that the pancreas end fitted snugly into the stomach. The second and third layers were intragastric using full thickness 2-0 polyglactin suture. The fourth layer was between the seromuscular layer of the stomach and posterior capsule of pancreas (Fig. 1–3). The hepaticojejunostomy and antecolic gastrojejunostomy were made either as a single loop (earlier until 2008) or as an isolated loop as described in our previous publication [1]. Feeding jejunostomy was made and a single subhepatic drain was placed.
Intraoperative parameters including operative time, blood loss, and intraoperative complications were recorded. Drain was left for 4–5 days after surgery. Both nature and volume of drain were recorded and drain fluid was sent for amylase determination on postoperative day 3 depending on the patient’s clinical condition. Octreotide was given subcutaneously for 5 days at 100 μg thrice daily. Jejunostomy feeding was started on 3rd day and oral feeding was resumed on postoperative days 5 to 7. A gastrografin study was done on day 5 to look for delayed gastric emptying and hepatic scintigraphy (HIDA) scan was done on day 7 to look for any leak and patency of bilio-enteric pathway.
Clinical postoperative pancreatic fistula (POPF) was defined as amylase level in drainage fluid > 3 times that in serum as per the International Study Group on Pancreatic Surgery (ISGPF) [2]. Grade A POPF is transient and needs no special management. Grade B fistula is a fistula with clinical impact that requires a change in the therapeutic management and grade C is a fistula with severe clinical effect and requires a major change in management.
Total hospital stay and postoperative complications were recorded. Patients were followed-up at 1 month, 3 months, 6 months, and half yearly thereafter.
Results
We present the results of this case series analysis of a total of 467 Whipple’s pancreaticoduodenectomy in whom PG was performed. The median age of the patients was 53.2 years (range 38–78 years). The most common presenting symptom was surgical obstructive jaundice (which was seen in almost all the patients (463 out of 467)) followed by pain abdomen (70%) and weight loss. Preoperative endoscopic retrograde cholangiopancreatography (ERCP) stenting was done in 133 patients (28.5%) and open cholecystostomy in 9 patients prior to 2001. (Table 1). The most common tumor was ampullary adenocarcinoma (57.6%) followed by carcinoma head of pancreas (15.3%) (Table 1). On final histopathology, neuroendocrine tumor was seen in 6 patients and dysplasia in 16 patients. The remaining were adenocarcinoma (Table 1).
Operative Details
Mean operative time was 260.8 ± 50.3 mm (180–390 min) with an average blood loss of 1068 ± 606.19 ml (400–2600 ml). The average number of transfusions recorded was 2.12 packed cells for surgery. Classical Whipple’s with pancreaticogastrostomy was performed in 366 patients (78.4%) and isolated loop technique was used in 101 patients (22%). Vascular reconstruction was performed in 5 patients (5 portal vein reconstructions) due to tumor involvement. One patient required a right nephrectomy in view of renal hilar infiltration by the tumor. The texture of the pancreas was soft in majority of the patients (81%) (Table 2).
Complications
Thirty-five patients had postoperative bleeding out of which 12 were early and 23 had delayed hemorrhage. The most common source of bleeding was gastrojejunostomy site ulcer (16 patients), gastroduodenal artery pseudoaneurysm in 10 patients, and 9 patients had bleeding from the pancreatic stump (none required reexploration and all were managed with endoscopic argon beam coagulation of the bleeder) (Table 3).
The most common postoperative complication was delayed gastric emptying which was seen in 96 patients (20.5%). However, this percentage was much lower in patient with isolated loop technique (5 out of 101 (5.2%)) when compared with those with standard Whipple’s with pancreaticogastrostomy (91 (24.8%)) (Table 3).
Transient bile leak was seen in 84 patients (18%) and all of them stopped spontaneously without any intervention and no long-term biliary fistula formed in any of the patients. Three patients had bile leak because of the leak from the biliary enteric anastomosis out of which one had associated gastroduodenal artery (GDA) bleeding. This patient was reexplored and reanastomosis and GDA bleed was controlled. Patient however had sepsis and eventually succumbed after 45 days. The remaining two patients were managed conservatively and did not require any surgical intervention. HIDA scan done after 4 weeks showed patent bilio-enteric clearance.
Wound infection was seen in 70(15%) patients, out of which 40 patients had undergone preoperative biliary drainage. Out of the 70 patients, 50 had superficial surgical site infection (SSSI), 14 had deep SSI, and only 6 patients had deep organ space infection. Subacute intestinal obstruction was seen in 15 patients and majority were managed conservatively. The most common non-surgical morbidity was lower respiratory tract infection (LRTI) and pleural effusion which was seen in 12% patients.
The median hospital stay was 15.2 days (8–42 days). The overall 30-day mortality was 2% (10 out of 467). Seven out of them died due to massive gastrointestinal bleed and one patient died due to septic shock following gastrojejunostomy leak. One patient died following HJ leak with GDA bleed. One patient had an aberrant origin of common hepatic artery (CHA) from superior mesenteric artery (SMA) with an intrapancreatic course. This artery was inadvertently transected during the pancreatic neck division. The CHA was reconstructed. However, on postoperative day 9, the patient has a disruption of the anastomosis with hepaticojejunostomy leak and succumbed to hemorrhagic shock with liver failure despite reexploration and ligation of CHA (Table 4).
Postoperative Pancreatic Fistula
Transient hyperamylasemia was seen in 2% patients (grade A POPF). This hyperamylasemia resolved by postoperative day 5 or 7. None of the patients had a grade B or grade C pancreatic fistula requiring intervention or redo surgery (Table 3).
Reoperation
The reexploration rate in our series was 4.7% (22 out of 467). The most common reason for reexploration was bleeding (18 patients), internal herniation (1 patient), and gastrojejunostomy leak in two patient and HJ leak in one patient.
Readmissions
There were a total of 71 (15.2%) readmissions due to various problems. The most common cause of readmission was inability to tolerate oral feeds due to delayed gastric emptying (60%) and wound infection (33%). Seven percent patients were readmitted with subacute intestinal obstruction. Other reason for readmission included cholangitis, fever.
Of the 467 patients, 101 were performed using isolated loop technique. This technique has brought down the rate of delayed gastric emptying from 21.6 to 5.2%.
Discussion
Pancreaticoduodenectomy (PD) is the only accepted curative treatment of malignant diseases of the periampullary region. Since Allen O Whipple [3] performed the procedure in two stages in 1935, PD has evolved in terms of technical refinement. Although the operative mortality after PD has reduced to around 5% [4] [also Howard J. History of pancreatic head resection—the evaluation of surgical technique] the incidence of postoperative morbidity is still around 50% even at high-volume centers. Major reasons for this reduction in mortality are improvement in preoperative imaging, surgical technique, and most importantly, anesthesia and postoperative critical care. The overall mortality rate in our series has been similar to that of literature.
In spite of the marked reduction in mortality, PD is still associated with high postoperative complication rates, which are in the range of 50% [4] in some large recent series. The major complications are delayed gastric emptying (DGE), pancreatic leak, intraabdominal sepsis, bile leak, and gastrointestinal or intraabdominal hemorrhage.
POPF is the most dreaded complication following PD, with a reported incidence of around 2–20% [5]. It prolongs hospital stay and can lead to intraabdominal sepsis or hemorrhage and even death. There is a multitude of diverse approaches in use today aiming to reduce the incidence of POPF. Prophylactic octreotide, use of fibrin glue to occlude the main pancreatic duct, suture ligation of the pancreatic duct, pancreatic duct stenting, modification of the jejunal anastomosis (end-to-end versus end-to-side, invagination versus duct-to-mucosa), pancreaticogastrostomy (PG), use of an isolated Roux-en-Y limb to drain the pancreas, and total pancreatectomy have all been suggested. There is, however, ongoing debate as to which is the most effective strategy.
Pancreatic stump reconstruction has been considered “the Achilles heel of PD” [6]. Various modifications have been tried and PJ has commonly been performed at major centers. The incidence of POPF following PJ has been found to remain in the range of 10–18% [2]. This high rate of fistula formation has been attributed to the fact that pancreatic juice entering the jejunum becomes activated with enterokinase. Any leakage at the anastomosis, therefore, results in peritoneal contamination with succus entericus and bile. Obstruction or edema of the jejunal limb can result in positive pressure on the pancreaticojejunal anastomosis, increasing the chance of leakage.
PG was first described by Waugh and Clagget [7] in 1946. Since then, many authors have found it to be a safer procedure than PJ. The purported advantages of PG over PJ are many the low pH of the gastric lumen and a lack of enterokinase inactivate pancreatic enzymes, thus rendering pancreatic juice less damaging to the anastomosis itself and to surrounding structures in case of leakage. The alkaline pancreatic secretions may help protect the pancreaticogastric anastomosis against marginal ulceration. The thick gastric wall with its excellent blood supply as well as anatomical proximity to the pancreatic remnant allow for a very secure anastomosis without tension. Postoperative gastric decompression is easily performed and provides constant removal of pancreatic and gastric secretions thereby causing less tension on the pancreaticogastric anastomosis. The anastomosis can be accessed endoscopically and intraluminal bleeding around the anastomosis can be easily controlled endoscopically. Also, the anastomosis is located away from major vessels that are skeletonized during PD; thus, the risk of extraluminal bleeding due to proteolytic digestion of vascular structures is less in case of a leak.
In our previous report [6] of 125 pancreaticogastrotomies, we have shown a fistula rate of 0% and shown the efficacy of PG as a reconstructive technique following Whipple’s pancreaticoduodenectomy.
Literature has been inconsistent in comparing POPF rates between PG and PJ. Three RCTs [8,9,10] have shown similar POPF rates between PG and PJ anastomosis. Wente et al. [11] have done separate meta-analyses of 3 RCTs [8,9,10] and 13 non-randomized observational studies. While the meta-analysis of RCTs revealed no difference in outcome in terms of POPF and mortality, 12 of the 13 non-randomized studies showed a lower incidence of POPF in patients undergoing PG. However, 6 of these 12 studies also reported higher hemorrhagic complications after PG. The authors concluded that non-randomized studies are subject to bias and can be misleading. One drawback of the meta-analysis of the 3 RCTs is that the definition of pancreatic fistula was not consistent.
A recent meta-analysis of seven RCTs (including the 3 RCTs of the previous meta-analysis) [12], however, has revealed a significant benefit of PG reconstruction compared with PJ with regard to POPF, intraabdominal fluid collection and biliary fistula. Subgroup analysis looking specifically at trials using ISGPF definition also favored PG reconstruction. However, overall morbidity was comparable between the two procedures, which may be attributed to the different definitions of included complications.
Although another meta-analysis of 10 RCTs with 1629 patients found significant less POPF after PG compared with PJ, a Cochrane review [10] of the same RCTs concluded that the risk of bias was high in all but one trial and thus, superiority of one technique over the other cannot be demonstrated.
The largest RCT so far by Keck et al. [13] comprising 440 patients also failed to show any difference in incidence of clinically significant pancreatic fistula (ISGPF grade B/C). However, risk of bleeding (ISGPF grade A/B but not C) was found to be more after PG. In multivariate analysis, the single most important factor influencing pancreatic fistula rate was the texture of the pancreas.
The most significant observation in the current series is that no pancreatic fistula developed in 467patients. This is in keeping with the published reports of PG following PD. In most randomized trials published to date, the incidence of pancreatic fistula following PG is 0 to 11% [8,9,10, 14, 15]. The incidence of pancreatic fistula in pooled data from all published randomized trials is 10.4% (59 of 553). However, when ISGPF criteria are applied, clinically significant fistula rate is only 0.9% (5 out of 562). In contrast, the incidence of pancreatic fistula after PJ ranges from 0 to 35%, being commonly in the range of 10 to 20%. In addition, the mortality of a pancreatic fistula related to a PJ is more than that following PG.
The POPF rates following PJ have been found to be higher in patients with ampullary carcinoma as the pancreas is softer. The results of the current study are, thus, all the more significant in that majority of the PDs were performed for ampullary cancer with relatively soft pancreas. Therefore, the advantage of PG over PJ is all the more pronounced in patients with soft pancreas.
The most common technique used for pancreaticogastrostomy is a two-layer anastomosis between the pancreatic stump and the posterior wall of stomach midway between the lesser and greater curvature, allowing sufficient pancreas to project into the lumen of stomach. Duct-to-mucosa anastomosis has been described by some authors with equally good results. Takao et al. [16] have described a modification where a stent is placed in the pancreatic duct and passed through the posterior and anterior walls of stomach and drained to the exterior through the anterior abdominal wall. With this modification, they were able to achieve duct-to-mucosa approximation in patients with PPPD without the need for an anterior gastrotomy. They reported no pancreatic leaks in a series of 46 patients. Thus, all variations of pancreaticogastrostomy have yielded equally good results.
Topalet al [17] showed that PG performed by invagination method has a higher incidence of intragastric bleed. Similar findings were reported by Figueras et al. [18]. According to these reports, bleeding occurs from the cut edge of pancreatic stump. We have been performing only the invaginated PG and to date, we have not had a bleeding from the pancreatic stump. This can be explained by the fact that we place hemostatic 3-0 polypropylene sutures on the pancreatic stump after identification and cannulation of the pancreatic duct.
Conclusions
Pancreaticogastrostomy as a reconstructive technique is a safe option following PD with complication rate similar to that of PJ with almost nil incidence of clinically significant POPF as shown in our series of 467 patients. The present series presents the largest series to date of pancreaticogastrostomy following PD.
References
Krishna A et al (2015) Preventing delayed gastric emptying after Whipple’s procedure—isolated roux loop reconstruction with pancreaticogastrostomy. Indian J Surg 77(2):703–707
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, International Study Group on Pancreatic Fistula Definition et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Whipple AO, Parsons WB, Mullins CR (1935) Treatment of carcinoma of the ampulla of Vater. Ann Surg 102(4):763–779
Xiong JJ et al (2014) Meta-analysis of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Br J Surg 101.10:1196–1208
Liang TB, Bai XL, Zheng SS (2007) Pancreatic fistula after pancreaticoduodenectomy: diagnosed according to International Study Group Pancreatic Fistula (ISGPF) definition. Pancreatology 7:325–331
Kapur BML, Misra MC, Seenu V, Goel AK (1998) Pancreaticogastrostomy for reconstruction of pancreatic stump after pancreaticoduodenectomy for ampullary carcinoma. Am J Surg 176(3):274–278
Waugh JM, Clagett OT (1946) Resection of the duodenum and head of the pancreas for carcinoma; an analysis of thirty cases. Surgery 20:224–232
Bassi C, Falconi M, Molinari E, Salvia R, Butturini G, Sartori N, Mantovani W, Pederzoli P (2005) Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann Surg 242:767–771
Yeo CJ, Cameron JL, Maher MM, Sauter PK, Zahurak ML, Talamini MA, Lillemoe KD, Pitt HA (1995) A prospective randomized trial of pancreaticogastrostomy versus pancreaticojejunostomy after pancreaticoduodenectomy. Ann Surg 222:580–588
Duffas JP, Suc B, Msika S, Fourtanier G, Muscari F, Hay JM, French Associations for Research in Surgery et al (2005) A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg 189:720–729
Wente MN, Shrikhande SV, Müller MW, Diener MK, Seiler CM, Friess H, Büchler MW (2007) Pancreaticojejunostomy versus pancreaticogastrostomy: systematic review and meta-analysis. Am J Surg 193:171–183
Xiong JJ, Altaf K, Mukherjee R, Huang W, Hu WM, Li A, Ke NW, Liu XB (2012) Systematic review and meta-analysis of outcomes after intraoperative pancreatic duct stent placement during pancreaticoduodenectomy. Br J Surg 99:1050–1061
Keck T, Wellner UF, Bahra M, Klein F, Sick O, Niedergethmann M, Wilhelm TJ, Farkas SA, Börner T, Bruns C, Kleespies A (2016) Pancreatogastrostomy versus pancreatojejunostomy for RECOnstruction after PANCreatoduodenectomy (RECOPANC, DRKS 00000767): perioperative and long-term results of a multicenter randomized controlled trial. Ann Surg 263(3):440–449
Wellner UF, Sick O, Olschewski M, Adam U, Hopt UT, Keck T (2012) Randomized controlled single-center trial comparing pancreatogastrostomy versus pancreaticojejunostomy after partial pancreatoduodenectomy. J Gastrointest Surg 16:1686–1695
Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, Belgian Section of Hepatobiliary and Pancreatic Surgery et al (2013) Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol 14:655–662
Takao S et al (1993) Modified pancreaticogastrostomy following pancreaticoduodenectomy. Am J Surg 165(3):317–321
Topal B, Fieuws S, Aerts R, Weerts J, Feryn T, Roeyen G, Belgian Section of Hepatobiliary and Pancreatic Surgery et al (2013) Pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy for pancreatic or periampullary tumours: a multicentre randomised trial. Lancet Oncol 14:655–662
Figueras J, Sabater L, Planellas P, Muñoz-Forner E, Lopez-Ben S, Falgueras L, Sala-Palau C, Albiol M, Ortega-Serrano J, Castro-Gutierrez E (2013) Randomized clinical trial of pancreaticogastrostomy versus pancreaticojejunostomy on the rate and severity of pancreatic fistula after pancreaticoduodenectomy. Br J Surg 100:1597–1605
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krishna, A., Bansal, V.K., Kumar, S. et al. Pancreaticogastrostomy After Whipple’s Surgery Avoids Pancreatic Fistula—a Large Case Series Analysis. Indian J Surg 82, 415–420 (2020). https://doi.org/10.1007/s12262-019-01991-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-019-01991-4