Abstract
We aimed to demonstrate the role of SPECT/CT in preoperative localization of parathyroid lesions in patients with hyperparathyroidism who had technetium-99m (Tc-99m) methoxyisobutylisonitrile (MIBI) dual-phase parathyroid scintigraphy. We evaluated retrospectively the scintigraphic data of 103 patients who had parathyroidectomy after Tc-99m MIBI dual-phase parathyroid scintigraphy with SPECT/CT. The planar and SPECT/CT images were evaluated separately to determine their efficacy in localizing parathyroid lesions. These results were then compared with surgical data. There were 84 female and 19 male patients whose mean age was 54 ± 12 years. A total of 115 parathyroid lesions in 103 patients were resected during operations. In 87 patients, with both planar and SPECT/CT images, a total of 100 lesions could be detected correctly. In 11 patients, only SPECT/CT images could show 13 subcentimetric lesions. In three patients, three lesions were evaluated as parathyroid lesions both with planar and SPECT/CT images, but according to histopathologic evaluation, they came out to be nonparathyroidal lesions. In two patients, two parathyroid lesions could not be detected preoperatively neither with planar nor with SPECT/CT images. The lesion-based sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 87 %, 99 %, 97.1 %, 95.3 %, and 95.8 % for planar images and 98.3 %, 99 %, 97.4 %, 99.4 %, and 98.8 % for SPECT/CT images, respectively. Tc-99m MIBI parathyroid scintigraphy should be a diagnostic modality of choice in preoperative evaluation of patients with hyperparathyroidism. SPECT/CT has an incremental value both in demonstrating subcentimetric lesions and in accurately localizing lesions anatomically.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of technetium-99m (Tc-99m) methoxyisobutylisonitrile (MIBI) for parathyroid imaging was first reported in 1989 [1]. As the surgery evolves to minimally invasive techniques, parathyroid scintigraphy has become a routine imaging technique in the preoperative localization of parathyroid pathologies.
Concomitant nodular thyroid disease with hyperparathyroidism is common, ranging from 20 to 75 % in endemic regions like Turkey [2]. A major limitation related to parathyroid imaging using either ultrasonography (USG) or Tc-99m MIBI parathyroid scintigraphy is the presence of concomitant thyroid nodules mimicking parathyroid lesions or other metabolically active tissues such as lymph node or thyroid cancer which cause false positive results on Tc-99m MIBI scans [3]. Recently, single photon emission computed tomography (SPECT) is used to increase the sensitivity which seems to show certain advantages compared to planar imaging [4, 5]. SPECT also has more success in the detection of small parathyroid adenomas and has a higher performance in determining the topographic localization of deeply located lesions in the neck or in ectopic sites and in differentiating these from concomitant thyroid nodules [6]. However, SPECT does not provide anatomical detail. Imaging with SPECT/computed tomography (SPECT/CT) improves the success of minimally invasive surgery by accurate anatomical localization of parathyroid lesions.
The purpose of this study was to evaluate the role of preoperative Tc-99m MIBI parathyroid SPECT/CT in the detection of parathyroid lesions in patients with hyperparathyroidism who were candidates for minimally invasive surgery.
Material and Method
Between November 2010 and March 2014, 550 patients have been referred to our nuclear medicine department for Tc-99m MIBI parathyroid scintigraphy for preoperative evaluation. Endocrinologists have confirmed hyperparathyroidism in these patients in accordance with their history and laboratory test values like parathyroid hormone (PTH), serum calcium (Ca), phosphorus (P), creatinine (Cr), and 25-hydroxy vitamin D levels. Patients with laboratory test results consistent with primary hyperparathyroidism were considered for surgical treatment when there was a worsening condition resistant to medical therapy like nephrolithiasis, low glomerular filtration rate, or bone/neuromuscular disorder. Asymptomatic patients whose serum Ca levels were above 1 mg/dl than the upper limit of normal range and kidney clearance less than 60 ml/min or who had osteoporosis or age less than 50 years were also considered for surgery [7]. Patients with laboratory test results consistent with secondary hyperparathyroidism due to a chronic renal disorder were considered for surgical treatment when Ca levels were above 11.5–12 mg/dl under treatment, in the presence of extraskeletal calcification, severe bone pain, fracture, or calciphylaxis in phosphate restriction or in the presence of pruritus resistant to treatment [7]. Patients with suspicion of malignancy were also operated. One hundred and three patients (84 females and 19 males; mean age 54 ± 12) who had parathyroidectomy constituted our patient group. The scintigraphic and surgical data of these patients were compared retrospectively.
Image Acquisition Protocol
All patients had double-phase parathyroid scintigraphy with Tc-99m MIBI, early SPECT/CT study, and thyroid scintigraphy.
Tc-99m MIBI Dual-Phase Planar Scintigraphy
Patients were injected intravenously of 740 MBq Tc-99m MIBI. Images were acquired on a Siemens ECAM gamma camera equipped with a low-energy, high-resolution, parallel-hole collimator. Both neck and chest planar images in anterior position were acquired with 128 × 128 matrix size at 15 min (early phase) and at 2 h (delayed phase).
Early Tc-99m MIBI SPECT/CT Fusion Images
Immediately after the early planar images, the early SPECT study was acquired on a Siemens ECAM gamma camera, using 60 projections with 30 s each, over a 180° anterior arc from right lateral to left lateral position at 3° angular steps. After SPECT acquisitions, CT acquisitions of the appropriate regions were performed on spiral four-slice CT (CT component of Biograph™ TruePoint™ PET-CT) with slice thickness of 2 mm, current of 60 mA, and voltage of 130 kV. No contrast medium was injected during the procedure. Then, the CT images and reconstructed SPECT images were evaluated after SPECT/CT fusion images were rendered using Siemens syngo™ software.
Thyroid Scintigraphy
After 24 h from the injection of Tc-99m MIBI, 185 MBq Tc-99m pertechnetate was injected to the patients. The images were acquired 10 min later, with 128 × 128 matrix, in anterior position with a 20 % window centered at around 140 keV photopeak using a low-energy, high-resolution, parallel-hole collimator. Tc-99m thyroid scintigraphy was performed for the evaluation of possible thyroid nodules.
Image Interpretation
The interpretation of Tc-99m MIBI images was performed in consensus by two experienced nuclear medicine physicians who were blinded to the results of other diagnostic modalities. Tc-99m MIBI double-phase planar parathyroid images and thyroid images were evaluated together. Tc-99m MIBI SPECT/CT fusion images were analyzed separately.
Planar parathyroid images were considered positive for parathyroid pathology in the presence of focal area of increased uptake in the neck or mediastinum showing either a progressive increase or a prolonged retention at delayed phase. The presence of focal uptake in early images even if not seen on delayed phase (rapid washout) was also accepted as positive for parathyroid pathology. In the presence of thyroid nodule on thyroid planar images, corresponding early and delayed parathyroid scintigraphy images were evaluated accordingly.
SPECT/CT fusion study interpretation was performed by using transaxial, coronal, and sagittal slices and also three-dimensional images created from the SPECT data. A SPECT/CT fusion study was considered positive in the presence of a focal area of increased uptake of Tc-99m MIBI. The anatomic localization was done with the aid of CT data.
A scan was considered true positive when it correctly identified the presence of abnormal gland which was operated afterwards. A scan was considered false positive when no pathological gland was found at operation, although the scan had suggested the presence of hyperactive parathyroid tissue. A scan was considered false negative when a pathological parathyroid gland was removed at surgery, although the scan had not demonstrated the presence of hyperactive parathyroid tissue at the resection site. Normal parathyroid glands were considered as true negative for the statistical analysis.
Statistical Analysis
Sensitivity, specificity, positive and negative predictive values, and accuracy of planar and SPECT/CT images of Tc-99m MIBI parathyroid scintigraphy were calculated on per-lesion basis.
Results
The study included a total of 103 patients (84 females and 19 males; mean age 54 ± 12; range 21–78 years) who were operated because of hyperparathyroidism with or without concomitant thyroid nodules.
The mean PTH level of patients was 441 pg/ml (60–5000 pg/ml; normal range of the laboratory was 15–65 pg/ml), and the mean Ca level was 11.4 mg/dl (8.1–17.8 mg/dl; normal range of the laboratory was 8.5–10.5 mg/dl).
Eighty-eight patients were in follow-up due to primary hyperparathyroidism, seven patients had chronic renal failure and thought to have secondary or tertiary hyperparathyroidism, five patients were suspected to have parathyroid carcinoma, and three patients were thought to have parathyroid hyperplasia (two patients had multiple endocrine neoplasia (MEN) 1 syndrome and the other patient had MEN 2 syndrome).
Forty-four patients had concomitant multinodular goiter. In 11 patients, USG revealed thyroid nodules in different localizations other than parathyroid lesions. Tc-99m pertechnetate thyroid scintigraphy showed nodular lesions in these areas.
After the injections of Tc-99m MIBI or Tc-99m pertechnetate, no adverse reaction occurred.
Surgical Data
All of the patients had parathyroidectomy with/without thyroidectomy. The decision of parathyroidectomy has been established according to the criteria mentioned in the “Material and Method” section. After surgery, 115 parathyroid lesions were excised in 103 patients in whom 12 glands were located in ectopic localizations.
Ninety-one patients had one parathyroid lesion, and nine patients had multiglandular parathyroid pathology, with a total of 24 glands. Four patients had two adenomas. One of these patients had MEN 1 syndrome who had parathyroid adenomas located in the left upper and lower poles. The other patient had an adenoma located in left lobe and also another adenoma located in an ectopic location in the mediastinum. The two patients with chronic renal failure had three hyperplastic parathyroid lesions each. The other patient with MEN 1 syndrome had four parathyroid pathologies (two adenomas and two hyperplastic glands). The patient with MEN 2 syndrome had also four parathyroid pathologies (one adenoma and three hyperplastic glands).
There were five parathyroid carcinoma patients. Two of these patients had PTH levels above 3000 pg/ml, and lesions were bigger than 4 cm. In the other two patients, the lesions were nearly 1.5 cm in diameter and one had invasion to the trachea. The last patient had a lesion which had cystic and calcific parts.
Lesion localizations in surgical notes were as follows: 43 lesions were located in the left lower pole, 45 lesions in the right lower pole, 9 lesions in the left upper pole, 6 lesions in right upper lobe, and 12 lesions in the ectopic locations. Ectopic adenomas were excised from the anterior mediastinum in three patients, tracheoesophageal groove in two patients, high mediastinal region in three patients, retrotracheal region in one patient, right upper paratracheal region in one patient, prevascular region in one patient, and intrathymic in one patient. Especially lesions in tracheoesophageal groove, retrotracheal, and intrathymic regions were beyond the normal operation area of the surgeons.
Scintigraphic Data
When the localization of parathyroid pathologies as evaluated on planar and SPECT/CT findings was compared with surgical data, it was determined that in 87/103 patients, both planar and SPECT/CT images were true positive (84.5 %). Although planar scans were positive in these 87 patients, accurate anatomic localization could be defined with CT findings in 75 of 87 patients. In these 87 patients, 100 parathyroid lesions were detected.
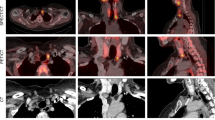
In 11/103 (10.7 %) patients, while planar images were false negative, SPECT/CT images were true positive. There were a total of 13 parathyroid lesions. When CT data was inspected, we saw that the dimensions of these lesions were subcentimetric and localized in posterior regions. One lesion was located in the thymus, ectopically (Figs. 1 and 2).
Planar Tc-99m MIBI dual-phase parathyroid (a–c) and Tc-99m pertechnetate thyroid (d) images of a female patient who is 43 years old. Her parathyroid hormone level is 5000 pg/ml, and serum calcium level is 10.8 mg/dl. There is no abnormal Tc-99m MIBI uptake in early (a) and late (c) planar images taken from the neck and from the chest (b)
Tc-99m MIBI SPECT/CT images of the same patient in Fig. 1. Focal Tc-99m MIBI uptake (arrow) can be clearly seen in the anterior region of the thorax in SPECT images (first row). In CT images, there is a nodular lesion (arrow), 8 mm in diameter, located anteriorly to the aortic arch (middle row). This lesion is reported as parathyroid pathology, located in the anterior mediastinum (arrow) with the aid of SPECT/CT images (bottom row). After the resection of this lesion, histopathologic evaluation revealed a parathyroid adenoma, located in thymic tissue
In 2/103 (1.9 %) patients, planar and SPECT/CT images were false negative. One of these patients had concomitant multiple thyroid nodules in both lobes. The dimensions of the largest thyroid nodule were 7 × 4 × 5 cm, and it was located in the right lobe. The patient had thyroidectomy with parathyroidectomy. The resected parathyroid adenoma was located in the right lobe, just below the largest thyroid nodule. The weight of the resected parathyroid adenoma was 81 gr, and its dimensions were 1.2 × 1 × 0.8 cm. In the same patient, a thyroid papillary microcarcinoma was defined in the left lobe. The other patient had subtotal thyroidectomy before. The patient had residual thyroid tissue in the right lobe. The parathyroid adenoma was found in the lower pole of the right lobe. Its diameter was 1.1 cm. These two adenomas did not show any abnormal Tc-99m MIBI uptake to allow detection or differentiation from thyroid uptake.
In 3/103 (2.9 %) patients, although planar and SPECT/CT images were positive, after the histopathological evaluation, one lesion came out to be a thyroid nodule and the other two lesions were thyroid carcinomas. They were accepted as false positive.
Twelve patients had parathyroid adenomas located in ectopic locations. Planar and SPECT/CT images showed the existence of ectopic parathyroid tissues in 11 of these patients, but exact anatomical localization could only be done with CT data. Dual planar images were falsely negative in one patient who had an intrathymic parathyroid adenoma. SPECT/CT images of this patient could localize the lesion (Figs. 1 and 2).
The lesion-based sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were 87 %, 99 %, 97.1 %, 95.3 %, and 95.8 % for planar images and 98.3 %, 99 %, 97.4 %, 99.4 %, and 98.8 % for SPECT/CT images, respectively. A summary of these values is given in Table 1. The comparison of lesion characterizations against the reference (histopathologic evaluation) for planar and SPECT/CT images is also shown in Tables 2 and 3, respectively.
Discussion
Contemporary modalities that help endocrine surgeons to localize abnormal parathyroid glands in patients with hyperparathyroidism should provide high-resolution anatomical and functional images of pathology. Parathyroid scintigraphy is considered almost the best preoperative localization method in patients with hyperparathyroidism [8]. The dual-phase planar Tc-99m MIBI parathyroid scintigraphy has been widely used and has also been shown to provide high sensitivity, ranged between 74–87 % [9]. The sensitivity of planar Tc-99m MIBI images is also 87 % in our study.
SPECT/CT, as an alternative approach to planar imaging, has the benefit of combining anatomy and function. A hybrid SPECT/CT device which has a CT unit, incorporated to the gamma camera (SPECT unit), is more expensive than a plain gamma camera, and therefore, it is not as widespread as the latter. Fortunately, most gamma cameras have software programs that produce fusion SPECT/CT images with CT data of exterior source, like in our department. Therefore, it is possible to have planar, SPECT, and SPECT/CT images with a gamma camera equipped with an appropriate software program.
Our present study suggests that the SPECT/CT is more sensitive (98.3 %) than planar imaging (87 %) for parathyroid lesion localization, although the specificities (99 %) are not different. In our study, the diameters of parathyroid glands which could not be found by dual-phase planar scintigraphy were smaller than 1 cm. The average diameter of these 13 lesions that could only be detected with SPECT/CT was 7 mm which proved better resolution characteristic of SPECT imaging than planar imaging. Additionally, although SPECT allows evaluation of depth, SPECT/CT shows more accurate localization of the activity demonstrated on SPECT imaging which often provides an incremental value to the operating surgeon [10–12]. The precise localization which is provided by SPECT/CT can outline the relationship of the adenoma with adjacent organs such as the thyroid, trachea, esophagus, and great vessels which can be damaged during the operation.
USG has been shown to have a sensitivity of 56–100 % and a specificity of 40–99 % in accurate localization of the parathyroid lesions [13]. Although USG allows anatomical detection of enlarged parathyroid glands, co-existing nodular thyroid tissue reduces the sensitivity and specificity. Also, deeply localized adenomas in the neck or ectopic adenomas are poorly visualized with USG. The use of preoperative scintigraphic imaging has also been most advantageous in identifying parathyroid lesions that are located in ectopic locations. In this study, 12 patients had adenomas with ectopic locations whose anatomical localization could only be done with CT data. Especially, lesions located in tracheoesophageal groove, retrotracheal, and intrathymic regions were beyond the normal operation area of the surgeons. With the detection of these lesions, the most curative surgery could be planned.
SPECT/CT is able to validate the inconclusive findings of SPECT or planar images. In some cases, this leads to proper categorization of SPECT findings as Tc-99m MIBI-avid nonparathyroid lesions, diminishing false positive findings. False positive scans will occur only when structures other than a parathyroid adenoma take up and concentrate Tc-99m MIBI to a higher degree than the surrounding tissues. In this regard, false positive Tc-99m MIBI scans have been attributed to thyroid adenomas, lymph nodes, diffuse thyroid hyperplasia, and thyroid cancers [14]. There were three false positive cases in our study. In the first patient while Tc-99m MIBI images revealed foci, consistent with parathyroid pathology, the histopathology was thyroid nodule. The other two patients had thyroid carcinoma. It is known that Tc-99m MIBI-positive thyroid nodules have an increased risk of malignancy [15, 16].
In our study, false negative cases occurred in patients with primary hyperparathyroidism with histopathologically proven small parathyroid adenomas. Qiu et al. stated the optimal threshold for localization of parathyroid lesions in Tc-99m MIBI scintigraphy by ROC analysis as 1.03 cm [17]. Tc-99m MIBI is a nonspecific tracer that is taken up by mitochondria-rich cells. The degree of Tc-99m MIBI uptake in parathyroid adenoma has been reported to correlate with not just the size of the gland but also the cytologic composition [18]. Greater uptake can be seen in adenomas with a predominance of oxyphilic cells compared with chief cells [19–22]. Although SPECT/CT has a better resolution than planar imaging, leading to better visualization of small lesions, cytologic composition still hampers Tc-99m MIBI uptake, leading to a false negative result. High washout from the parathyroid tissue can also result in false negative findings in dual-phase Tc-99m MIBI scans [23]. Although delayed neck and thorax SPECT/CT was stated not to be able to show additional lesions than planar scintigraphy [17], we think that early SPECT/CT imaging may overcome this problem.
In our study, the sensitivity of planar dual-phase Tc-99m MIBI scintigraphy was 87 % and the accuracy was 95.8 %. However, the sensitivity and accuracy of the SPECT/CT was 98.3 % and 98.8 %, respectively. In a retrospective study of 63 consecutive patients with primary hyperparathyroidism, the sensitivity and accuracy of SPECT/CT were found to be 90 % and 91 %, respectively [24]. In a series of 48 patients with concomitant thyroid nodules, the sensitivity and specificity of SPECT/CT were 77.5 % and 96.77 %, respectively [22]. Several studies reported higher sensitivities of parathyroid SPECT/CT ranging from 88 % to 100 % [25]. Recently, a meta-analysis showed that the sensitivities of SPECT/CT and planar scintigraphy were 84 % and 63 %, respectively [26]. Although with the aid of thyroid scintigraphy, the thyroid nodules can be differentiated from parathyroid pathologies in the planar Tc-99m MIBI images, the better sensitivity and accuracy values of SPECT/CT both in our study and in other studies prove that there is an obvious incremental value of SPECT/CT to Tc-99m MIBI dual-phase parathyroid scintigraphy.
The main limitation of our study arises from our inclusion criterion. We constituted our patient group with patients who had surgery after parathyroid scintigraphy. This criterion probably resulted in inclusion of patients with mostly positive scans because a negative scan probably would not lead to surgery. Although this situation may cause a higher detectability rate of parathyroid scintigraphy in our study, the main outcome which is the incremental value of SPECT/CT is still valid.
Conclusion
Although the dual-phase Tc-99m MIBI parathyroid scintigraphy, with the aid of Tc-99m pertechnetate thyroid scintigraphy, can show parathyroid pathologies with high sensitivity and accuracy, there is an incremental value of SPECT/CT both in lesions smaller than 1 cm and in accurate anatomical localization. Tc-99m MIBI parathyroid scintigraphy with SPECT/CT must not be omitted during preoperative preparations of patients with hyperparathyroidism.
References
Coakley AJ, Kettle AG, Wells CP, O’Doherty MJ, Collins RE (1989) 99Tcm sestamibi: a new agent for parathyroid imaging. Nucl Med Commun 10:791–794
Hurley DL, Gharib H (1996) Evaluation and management of multinodular goiter. Otolaryngol Clin N Am 29:527–540
Taillefer R, Boucher Y, Potvin C, Lambert R (1992) Detection and localization of parathyroid adenomas in patients with hyperparathyroidism using a single radionuclide imaging procedure with technetium-99m-sestamibi (double-phase study). J Nucl Med 33:1801–1807
Rubello D, Casara D, Fiore D, Muzzio P, Zonzin G, Shapiro B (2002) An ectopic mediastinal parathyroid adenoma accurately located by a single-day imaging protocol of Tc-99m pertechnetate-MIBI subtraction scintigraphy and MIBI-SPECT-computed tomographic image fusion. Clin Nucl Med 27:186–190
Lorberboym M, Minski I, Macadziob S, Nikolov G, Schachter P (2003) Incremental diagnostic value of preoperative 99mTc-MIBI SPECT in patients with a parathyroid adenoma. J Nucl Med 44:904–908
Billotey C, Sarfati E, Aurengo A, Duet M, Mündler O, Toubert ME et al (1996) Advantages of SPECT in technetium-99m-sestamibi parathyroid scintigraphy. J Nucl Med 37:1773–1778
Turkish Endocrinology and Metabolism Association Guideline for Diagnosis and Treatment of Metabolic Bone Diseases (2015) Ankara, Turkey.
Taubman M, Goldfarb M, Lew J (2011) Role of SPECT and SPECT/CT in the surgical treatment of primary hyperparathyroidism. Int J Mol Imaging. Article ID: 141593, 7 pages.
Mariani G, Gulec SA, Rubello D, Boni G, Puccini M, Pelizzo MR et al (2003) Preoperative localization and radioguided parathyroid surgery. J Nucl Med 44:1443–1458
Zhen L, Li H, Liu X, Ge BH, Yan J, Yang J (2013) The application of SPECT/CT for preoperative planning in patients with secondary hyperparathyroidism. Nucl Med Commun 34:439–444
Dasgupta D, Navalkissoor S, Ganatra R, Buscombe J (2013) The role of single photon computed tomography/computed tomography in localizing parathyroid adenoma. Nucl Med Commun 34:621–626
Lavely W, Goetze S, Friedman K, Leal JP, Zhang Z, Garret-Mayer E et al (2007) Comparison of SPECT/CT, SPECT, and planar imaging with single- and dual-phase (99m)Tc-sestamibi parathyroid scintigraphy. J Nucl Med 48:1084–1089
Noda S, Onoda N, Kashiwagi H, Kawajiri H, Takashima T, Ishikawa T et al (2014) Strategy of operative treatment of hyperparathyroidism using US scan and Tc-99m-MIBI SPECT/CT. Endocr J 61:225–230
Mahajan A, Starker L, Ghita M, Udelsman R, Brink JA, Carling T (2012) Parathyroid four-dimensional computed tomography: evaluation of radiation dose exposure during preoperative localisation of parathyroid tumors in primary hyperparathyroidism. World J Surg 36:1335–1339
Saggiorato E, Angusti T, Rosas R, Martinese M, Finessi M, Arecco F et al (2009) 99mTc-MIBI imaging in the presurgical characterization of thyroid follicular neoplasms: relationship to multidrug resistance protein expression. J Nucl Med 50:1785–1793
Leidig-Bruckner G, Cichorowski G, Sattler P, Bruckner T, Sattler B (2012) Evaluation of thyroid nodules—combined use of 99mTc-methylisobutylnitrile scintigraphy and aspiration cytology to assess risk of malignancy and stratify patients for surgical or nonsurgical therapy—a retrospective cohort study. Clin Endocrinol 76:749–758
Qiu ZL, Wu B, Shen CT, Zhu RS, Luo QY (2014) Dual-phase (99m)Tc-MIBI scintigraphy with delayed neck and thorax SPECT/CT and bone scintigraphy in patients with primary hyperparathyroidism: correlation with clinical or pathological variables. Ann Nucl Med 28:725–735
Mihai R, Gleeson F, Buley ID, Roskell DE, Sadler GP (2006) Negative imaging studies for primary hyperparathyroidism are unavoidable: correlation of sestamibi and high resolution ultrasound scanning with histological analysis in 150 patients. World J Surg 30:697–704
Taieb D, Urena-Torres P, Zanotti-Fregonara P, Rubello D, Ferretti A, Henter I et al (2013) Parathyroid scintigraphy in renal hyperparathyroidism. Clin Nucl Med 38:630–635
Witteveen JE, Kievit J, Stokkel MPM, Morreau H, Romijn JA, Hamdy NAT (2011) Limitations of Tc99m-MIBI SPECT imaging scans in persistent primary hyperparathyroidism. World J Surg 35:128–139
Öksüz MÖ, Dittman H, Wicke C, Müssig K, Bares R, Pfannenberg C et al (2011) Accuracy of parathyroid imaging: a comparison of planar scintigraphy, SPECT, SPECT-CT and C-11 methionine PET for the detection of parathyroid adenomas and glandular hyperplasia. Diagn Interv Radiol 17:297–307
Shafiei B, Hoseinzadeh S, Fotouhi F, Malek H, Azizi F, Jahed A et al (2012) Preoperative Tc-99m-sestamibi scintigraphy in patients with primary hyperparathyroidism and concomitant nodular goiter: comparison of SPECT-CT, SPECT, and planar imaging. Nucl Med Commun 33:1070–1076
Ciappuccini R, Morera J, Pascal P, Rame JP, Heutte N, Aide N et al (2012) Dual-phase Tc-99m sestamibi scintigraphy with neck and thorax SPECT/CT in primary hyperparathyroidism. Clin Nucl Med 37:223–228
Patel C, Salahudeen HM, Lansdown M, Scarsbrook A (2010) Clinical utility of ultrasound and 99mTc sestamibi SPECT/CT for preoperative localisation of parathyroid adenoma in patients with primary hyperparathyroidism. Clin Radiol 65:278–287
Im HJ, Lee IK, Paeng JC, Lee KE, Cheon GJ, Kang KW et al (2014) Functional evaluation of parathyroid adenoma using Tc-99m-MIBI parathyroid SPECT/CT: correlation with functional markers and disease severity. Nucl Med Commun 35:649–654
Wei WJ, Shen CT, Song HJ, Qiu ZL, Luo QY (2015) Comparison of SPECT/CT, SPECT and planar imaging using (99m)Tc-MIBI as independent techniques to support minimally invasive parathyroidectomy in primary hyperparathyroidism: a meta-analysis. Hell J Nucl Med 18:127–135
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Funding
Our research has not been funded by any organization.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
Our study is retrospectively designed. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Ozkan, Z.G., Unal, S.N., Kuyumcu, S. et al. Clinical Utility of Tc-99m MIBI SPECT/CT for Preoperative Localization of Parathyroid Lesions. Indian J Surg 79, 312–318 (2017). https://doi.org/10.1007/s12262-016-1489-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-016-1489-7