Abstract
MicroRNAs (miRNAs) are small non-coding RNAs composed of 18–25 nucleotides that can post-transcriptionally regulate gene expression and have key regulatory roles in cancer, acting as both oncogenes and tumor suppressors. About 1000 genes in humans encode miRNAs, which account for approximately 3% of the human genome, and up to 30% of human protein coding genes may be regulated by miRNAs. The objective of this article is to evaluate the expression profile of four miRNAs previously implicated in triple negative breast cancer: miR-10b, miR-26a, miR-146a and miR-153, and to determine their possible interaction in triple negative and non triple negative breast cancer based on clinical outcome and the expression of BRCA1. 24 triple-negative and 13 non triple negative breast cancer cases, were studied by q-RT-PCR and immunohistochemistry to determine the expression of the four studied miRNAs and the BRCA1 protein, respectively. We observed that the BRCA1 protein was absent in 62.5% of the triple negative cases. Besides, the miR-146a and miR-26a were over expressed in triple negative breast cancer. These two miRNAs, miR-10b and miR-153 were significantly associated to lymph node metastases occurrence in triple negative breast carcinoma. All the analyzed microRNAs were not associated with the expression of BRCA1 in our conditions. Our work provides evidence that miR-146a, miR-26a, miR-10b and miR-153 could be defined as biomarkers in triple negative breast cancer to predict lymph node metastases (LNM).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequent carcinoma affecting females and the second leading cause of cancer-related deaths in women [1–3]. It is a heterogeneous disease that is functionnally classified based on molecular profiles into different subtypes including luminal A, luminal B, human epidermal growth factor receptor 2 (HER2)-enriched, basal-like, normal breast-like group and claudin-low subtype.
Basal-like breast cancers contribute to 80% of triple negative breast cancer (TNBC) [4], one of the most aggressive subtypes, that lacks estrogen receptor, progesterone receptor and human epidermal growth factor receptor 2 (HER2) overexpression. TNBC represents 15%–20% of all breast cancers [4, 5]. It is often characterized as young age, high proliferation, high histological grade, big tumor size, high clinical stage at diagnosis, high rate of positive lymph node, high risk of recurrence and distant metastases and it is associated with lack or low expression of BRCA1 protein [6, 7]. Lacking of effective treatment method, it is essential that new, alternative therapeutic targets for TNBC are identified. Several studies have identified microRNAs (miRNAs) playing a key role in all cellular processes and they are promising targets for many types of cancer [2, 7, 8].
MiRNAs are a family of 21–25 nucleotide non-coding RNAs molecules that regulate the expression of various genes involved in the cell signaling pathways [2, 8–10]. In the present study, we explored the expression levels of four microRNAs: miR-10b, miR-26a, miR-146a and miR-153 in both triple negative and non triple negative mammary tumors. These miRNAs were previously identified by Fkih M’hamed et al. as potentiel triple negative breast cancer biomarkers based on expression profiling results in 10 cell lines using PCR Array and qRT-PCR [11]. Moreover, we investigated their possible interactions with the clinical outcome and the expression of BRCA1.
Materials and Methods
Patients
Two groups of patients are tested in this study, the first with a triple negative breast cancer profile and the second with a non triple negative breast cancer profile (Luminal A, Luminal B). Formalin-fixed, paraffin-embedded (FFPE) tissue files were drawn from the department of pathology of Farhat Hached Hospital of Sousse. 25 FFPE tissues were recovered for each group of patients.
Three 6 mm cores were obtained from each tumor tissue. All samples were from Tunisian women who lived in the central region of Tunisia.
Clinico-pathological data including age at diagnosis, histological grade, tumor size, lymph node status and ER, PR and HER-2 tumor expression of patients were collected from the Farhat Hached Hospital data base. We selected 37 samples after extraction and quality control of RNA. These cases were divided into two groups and are summarized in Table 1: 24 patients with triple negative breast carcinoma and 13 patients with non triple negative breast cancer profile. The study was approved by the institutional review board of the Farhat-Hached Hospital (Comité d’éthique et de Recherche du CHU Farhat-Hached).
Quantitative Real-Time PCR
Total RNA was extracted using miRNeasy FFPE kit (Qiagen, France) according to the manufacturer’s instructions. The RNA quality and concentrations were assessed using an Agilent Bioanalyzer 2100 (Kit Agilent RNA 6000 nano) and a spectrophotometer and then converted to cDNA using the miScript II RT Kit (Qiagen, France). Expression of miRNAs was measured using the miScript SYBR Green PCR Kit (Qiagen, France) on an ABI7900HT system (TaqMan, Applied Biosystem) and miScript Primer Assays (Qiagen, France, Table S1) according to the manufacturer’s protocol. All amplification reactions were performed in triplicates. U6 (Hs-RNU6–2-1 miscript Primer Assay) was used as internal control. All samples were normalized to the internal control and fold changes were calculated using the ∆∆CT method.
Immunohistochemistry
Immunohistochemical staining for the detection of BRCA1 expression was assessed on formalin-fixed paraffin embedded (FFPE) tissues using the EnVision Kit (EnVision ™ FLEX, High pH (Dako Autostainer / Autostainer Plus)) according to the manufacturer’s instructions and the primary antibody anti-BRCA1 (Anti-BRCA1 antibody [MS110] (ab16780) by Abcam ). Briefly, 5 um thick sections of paraffin embedded tissues were cut and dried overnight at 37 °C, deparaffinized and rehydrated. Antigen retrieval was done with the citrate buffer at pH 6 by boiling sections in water bath for 40 min until temperature reaches 98 °C. The activity of endogenous peroxidases was neutralized using reagent EnVision Peroxidase-Blocking Reagent FLEXTM for 5 min. Slides were subsequently washed in a washing buffer EnVision FLEXTM Wash buffer diluted in distilled water at room temperature. The sections were then incubated overnight with the appropriate primary antibody. We used monoclonal antibodies anti-BRCA1 with dilution 1/80. Then incubation of the slides was performed for 15 min in the presence of FLEXTM EnVision and Mouse linker.
The revelation of primary antibodies bound to their antigens is carried out by incubation for 20 min with the blade kit FLEXTM EnVision / HRP followed by washing. Then, the chromogenic substrate (diamino benzidine) is added to reveal the peroxidase activity. It is applied for 5 to 15 min followed by rinsing the sections in distilled water. Finally, the sections were counterstained with hematoxylin, dehydrated and mounted. All slides were coded and were evaluated under a light microscope by two experienced pathologists.
Statistical Analysis
A p-value <0.05 was considered as statistically significant. All statistical analyses were performed with SPSS 20 (SPSS, IBM) software and SEM (Statistics Epidemiology Medicine, developed by Kwiatkowski et al. [12]) software.
Results
Clinical Outcome
Clinical data including age at diagnosis, SBR grade, tumor size and lymph node metastases were compared between triple negative and non triple negative breast cancer patients (Table 2).
We observed that young women aged 49 years or under at diagnosis represent 50% in the triple negative breast cancer group while they are 61.54% in the non triple negative breast cancer group, p = 1.23E-7. We noticed that grade 3 concerns 50% of the patients with triple negative breast cancer; however, it is presented in only 15,38% of the patients with non triple negative breast cancer; p = 1.26E-12. We also observed that tumor size upper 3 cm presented in 37.5% of the patients with triple negative breast cancer and in 30,77% of the patients with non triple negative breast cancer, p = 3.07E-7. No significant difference was obtained for lymph node metastases.
Immunohistochemistry Study of BRCA1 Protein
BRCA1 protein expression among triple negative and non triple negative breast cancer patients was assessed according to the presence or the absence of BRCA1 protein within mammary tissues by routine immuno-histochemistry.
The positive staining was marked 1 and negative staining was marked 0. The BRCA1 protein was absent in 62.5% of the triple negative cases compared to 30.77% of non triple negative ones with p = 0.068 (Table 3).
miRNA Expression Levels in Triple Negative and Non Triple Negative Mammary Tumors
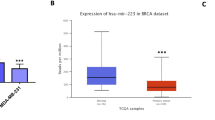
We analyzed the expression of four microRNAs (miR-10b; miR-26a; miR-146a and miR-153) among triple negative and non triple negative mammary tumors. The expression levels were normalized with the corresponding mean value of the reference gene U6. The difference of the expression levels of miR-10b, miR-26a; miR-146a and miR-153 between the two analyzed groups was not significant (p > 0.05), probably because of the small number of subjects in each group of patients (Table 4, Fig.1).
However we could observe that miR-146a and miR-26a were over-expressed 3 times and 1.5 times respectively in triple negative compared to non triple negative mammary tumors (Table 4).
For miR-153 and miR-10b, the expression levels were similar between triple negative and non triple negative groups.
Relationship between miRNAs Expression and BRCA1 Protein Expression
We assessed the relationship between miRNAs expression and BRCA1 protein expression among triple negative and non triple negative breast cancer patients using a non-parametrical statistical Mann-Whitney U test.
We found no significant difference between the expression of miRNAs and the expression of BRCA1 protein in our conditions (Table 5).
Relationship between miRNAs Expression and Clinico-Pathological Features
We analyzed the relationship between clinico-pathological features among triple negative and non triple negative of patients and miRNAs expression in triple negative and non triple negative mammary tumors.
We did not record any significant difference in the analyzed data (mean ± SD) between the two groups of mammary tumors for the age at diagnosis, tumor size and grade of the tumor (Fig.2).
However, using a non-parametrical statistical Mann-Whitney U test, miR-146a and miR-26a expression levels, are higher in triple negative breast cancer patients without lymph node metastases than in triple negative breast cancer patients with lymph node metastases, p (two tailed test) = 0,043 (Fig.3), p(two tailed test) = 0,011 (Fig.4) respectively. miR-10b has tendency to be associated with lymph node metastases among triple negative breast cancer patients p(two tailed test) = 0.082 , p (one tailed test) = 0.045 (Fig.5).
Moreover, we assessed the correlation between clinico-pathological features and miRNAs associations among triple negative and non triple negative patients using SEM software. The normalized expression data of the analyzed miRNAs were log2 transformed in order to display confidence intervals at 95% of average. We found some significant associations.
The multiple linear regression showed that the co-expression of miR-10b and miR-26a is correlated with the parameter triple negative tumor (r = 0.367, p = 0.022). The covariables miR-10b and miR-26a thus explain 13.4% of changes in tumor TN parameter (Table 6).
The logistic regression explained that the expression of miR-153 and miR-146 is inversely correlated with lymph node metastases (attached overall probability model p = 0.043) (Table 7).
Correlations between the Analyzed miRNAs
In order to better understand the interaction between microRNAs expression in triple negative and non triple negative breast cancer, we assessed the correlation between them using the Spearman’s Rho method.
In triple negative breast cancer, we observed two groups of correlating miRs. The first group was constituted by miR-146a, miR-10b and miR-26a. The highest correlation was found between miR-10b and miR-26a (Spearman’s rho: 0.805, p < 0.01), then the correlation between miR-146a and miR-26a (Spearman’s rho: 0.668, p < 0, 01) and between miR-146a and miR-10b (Spearman’s rho: 0.462, p < 0.05).
The second group formed by two miRNAs: miR-153 and miR-10b (Spearman Rho: 0.523, p < 0.01).
Considering the non triple negative breast cancer, we recorded a significant correlation (p < 0.05) between 3 miRNAs : miR-146a, miR-10b and miR-26a (Spearman’s Rho: 0.654; 0.610; 0.615) (Table 8).
The Signaling Pathways and Target Genes for the 4 miRNAs Involved in Triple Negative Breast Cancer
To determine the signaling pathways and target genes of the analyzed miRNAs, we used the DIANA-TarBase v.7 available online at http://www.microrna.gr/tarbase. This database allowed us to reveal the target genes of each miRNA and to study in which signaling pathway and pathologies they are implicated.
As shown in Fig. 6, different signaling pathways and pathologies modulated by the 4 analyzed miRNAs.
We extracted the different signaling pathways that might be involved in breast cancer triple negative based on literature:
-
Transcriptional misregulation in cancer (hsa05202)
-
Pathways in cancer (hsa05200)
-
PI3K-Akt signaling pathway (hsa04151)
-
Apoptosis (hsa04210)
-
NF-kappa B signaling pathway (hsa04064)
-
TGF-beta signaling pathway (hsa04350)
-
p53 signaling pathway (hsa04115)
For each signaling pathway, we determined the miRNA and their corresponding target genes involved in breast cancer triple negative (Table 9).
Discussion
Due to the absence of well-defined treatment method, Triple Negative Breast Cancer (TNBC) has attracted more attention [7]. MiRNAs are potential alternative therapeutic targets for cancer. They are also candidate diagnostic and prognostic indicators of breast cancer and have become an area of intense research focus in recent years [1].
Here, we explored the expression levels of BRCA1 protein and four miRNAs in triple negative and non triple negative mammary tumors. The studied miRNAs were selected since they were potentially overexpressed in TNBC, according to our first work in human triple negative breast cancer cells [11].
First, we compared the clinico-pathological features between triple negative and non triple negative mammary tumors, and we showed that our results are in agreement with the literature. TNBC tumors had younger age at diagnosis, were larger in tumor size and were of higher histological grade.
Also, TNBC are often linked to inactivation of the BRCA1 tumor suppressor gene, which leads to impaired homologous recombination-mediated DNA repair [13, 14]. These data are consistent with our immuno-histochemistry results. The BRCA1 protein was absent in 62.5% of the triple negative cases.
Second, we compared the expression levels of the four miRNAs (miR-10b, miR-26a, miR-146a and miR-153) between the two groups of TNBC and non TNBC, and noted that only miR-146a and miR-26a were over-expressed in triple negative compared to non triple negative mammary tumors. Concerning miR-146a, our finding were consistent with other studies [15, 16].
Since BRCA1 may also be regulated at the post-transcriptional level by microRNAs [17], we assessed the correlation between miRNAs expression and BRCA1 protein expression among triple negative and non triple negative breast cancer patients. By doing so, we found no significant difference in our conditions, indicating that the BRCA1 functional loss in triple negative mammary tumors may be regulated by other mechanism. Yamashita et al. reported that epigenetic inactivation of BRCA1 through promoter hypermethylation is an important mechanism that leads to functional loss of BRCA1 in TNBC [14]. Moreover, Zhang and Long demonstrated that BRCA1 methylation was statistically associated with lymph node metastasis, histological grade 3, triple-negative phenotype, and low levels of BRCA1 protein expression [18]. The other reason could be the low number of cases (especially in non TNBC group) that may not be enough for that kind of analysis.
The relationship between clinico-pathological features and miRNAs expression in triple negative and non triple negative mammary tumors demonstrated that miR-146a, miR-26, miR-10b and miR-153 expression levels were associated with lymph node metastasis among triple negative breast cancer patients. These results of miR-26a and miR-146a are in agreement with other studies of Liu et al. and Stückrath et al. [19, 20].
Moreover, Chen et al. demontrated that circulating miR-10b and miRNA-373 are potential biomarkers for detecting the lymph node status of breast cancer [22].
In this way and according to lymph node status, Rask et al. reported that differential expression levels of miR-139, miR-486 and miR-21 in breast cancer patients may represent a useful signature for the identification of high-risk breast cancer patients [21].
Regarding miR-153, Chen et al. showed that this miRNA was positively correlated with the lymph node status and distant metastasis in non-small cell lung cancer patients [24].
Then, we found a significant correlation between the analyzed miRNAs, as between miR-146a and miR-26a (Spearman’s rho: 0.668, p < 0, 01) in TNBC group.
These correlations are involved in various biological processes, including proliferation, migration, invasion, angiogenesis, and metabolism by targeting multiple mRNAs [11, 23, 25, 26].
Last, in the present study, we used the DIANA-TarBase v.7 data to determine the signaling pathways and target genes of the analyzed miRNAs that might be involved in TNBC (Table 7).
Among the target signaling pathways, we found the PI3K-Akt signaling pathway. Three miRNAs are involved in this pathway: miR-146a-5p targets the BRCA1 gene, miR-26a-5p target genes include GSK3B, CCND2, IFNB1, CCNE2, MYC, and PTEN and miR-153 targets MCL1 and BCL2.
Activation of the PI3K-AKT pathway by mutations of PIK3CA and PTEN inhibition are molecular characteristics already described in TNBC [26–28]. Other studies reported the carcinogenesis-related processes in TNBC via the PI3K/AKT signaling pathway [29–32].
Recently, Phua et al. reported that gene expression studies uncovered multi-factorial regulation of genes in the PI3K/AKT/mTOR pathway by miR-184 in breast cancer [33]. Besides, miR-214 acts as a potential oncogene in breast cancer by targeting the PTEN-PI3K/Akt signaling pathway [34].
Concerning our analyzed miRNA, Xu et al. indicated that the differential miRNA signatures include miR-146a in synovial fluid from osteoarthritis patients demonstrated primarily upregulation of the PI3K-Akt signaling pathway and other biologic cellular processes [35].
Chai et al. reported that miR-26a expression reduced macrophage colony-stimulating factor expression and recruitment of macrophages in hepatocellular carcinoma through the PI3K/Akt pathway [36]. Furthermore, the overexpression of miR-153 inhibited stretch stress-enhanced vascular smooth muscle cells proliferation and the activity of PI3K-AKT signaling [37].
Another pathway that is involved in TNBC is the NF-κB signaling pathway. Our results showed two miRNAs that are involved in this pathway: miR-146a-5p target genes include NFKB1, CXCL8, CD40Ig, TRAF6, BCL2A1 and IRAK1 and miR-153 target BCL2.
The nuclear factor NF-κB pathway has been suggested to be an important regulator of triple negative breast cancer. This pathway is responsible for controlling cellular processes [2]. Chen et al. demonstrated that the activation of G-protein coupled estrogen receptor (GPER) suppresses epithelial mesenchymal transition of triple negative breast cancer cells via NF-κB signaling [38].
Bhaumik et al. reported that miR-146a/b is a negative regulator of constitutive NF-κB activity in a breast cancer setting with reduction of metastases [39]. Moreover, other study showed that the expression of validated miRNAs (miR-146a, miR-99b and miR-205) induced by BRCA1 that commonly regulate TRAF2, were sufficient to modulate NF-κB activity [40].
Beyond the two signaling pathways cited, we have identified in the Table 7 other pathways : Transcriptional misregulation in cancer (hsa05202), Pathways in cancer (hsa05200), Apoptosis (hsa04210), TGF-beta signaling pathway (hsa04350) and p53 signaling pathway (hsa04115). Future studies should try to identify how our analyzed miRNA and these pathways are involved in the developpement of carcinogenesis-related processes in TNBC.
To conclude, our findings have important implications on TNBC. We identified miR-146a miR-26a, miR-10b and miR-153 as potential biomarkers in TNBC to predict lymph node metastases.
Furthermore, when discussing TNBC, we should keep in mind that it is a heterogeneous disease. Lehmann et al. classified triple negative tumors into six subtypes including 2 basal-like (BL1 and BL2), an immunomodulatory (IM), a mesenchymal (M), a mesenchymal stem-like (MSL), and a luminal androgen receptor (LAR) subtype [41]. This Classification may partly explain the contradictory results reported in the literature.
Further studies are warranted to understand the biological role of these miRNAs, their targets and the signaling pathways involved in TNBC. Molecular tools, such as gene expression, DNA sequencing, methylation profiles and protein expression can help to identify new biomarkers and treatment options of TNBC.
BRCA1, Breast Cancer 1; ER, estrogen receptor; HER2, human epidermal growth factor receptor 2; LNM, lymph node metastases; miRNAs, miR, microRNAs; PR, progesteron receptor; qRT-PCR, quantitative reverse transcription polymerase chain reaction; RNA, Ribonucleic acid; TNBC, Triple Negative Breast Cancer.
References
Kwan JYY, Psarianos P, Bruce JP, Yip KW, Liu F-F (2016) The complexity of microRNAs in human cancer. J Radiat Res. doi:10.1093/jrr/rrw009
Gyparaki M-T, Basdra EK, Papavassiliou AG (2014) MicroRNAs as regulatory elements in triple negative breast cancer. Cancer Lett 354:1–4
van Schooneveld E, Wildiers H, Vergote I, Vermeulen PB, Dirix LY, Van Laere SJ (2015) Dysregulation of microRNAs in breast cancer and their potential role as prognostic and predictive biomarkers in patient management. Breast Cancer Res 17:21
Arnedos M, Bihan C, Delaloge S, Andre F (2012) Triple-negative breast cancer: are we making headway at least? Ther Adv Med Oncol 4:195–210
Yadav BS, Chanana P, Jhamb S (2015) Biomarkers in triple negative breast cancer: a review. World J Clin Oncol 6:252–263
Andrés R, Pajares I, Balmaña J, Llort G, Ramón Y, Cajal T, Chirivella I et al (2014) Association of BRCA1 germline mutations in young onset triple-negative breast cancer (TNBC). Clin Transl Oncol 16:280–284
Qiu J, Xue X, Hu C, Xu H, Kou D, Li R et al (2016) Comparison of clinicopathological features and prognosis in triple-negative and non-triple negative breast cancer. J Cancer 7:167–173
Zaleska K (2015) miRNA - therapeutic tool in breast cancer? Where are we now? Rep Pract Oncol Radiother 20:79–86
D’Ippolito E, Iorio MV (2013) MicroRNAs and triple negative breast cancer. Int J Mol Sci 14:22202–22220
Popovska-Jankovic K, Noveski P, Chakalova L, Petrusevska G, Kubelka K, Plaseska-Karanfilska D (2012) MicroRNAs in breast cancer -our initial results. Balkan J Med Genet 15:87–89
Fkih M’hamed I, Privat M, Ponelle F, Penault-Llorca F, Kenani A, Bignon Y-J (2015) Identification of miR-10b, miR-26a, miR-146a and miR-153 as potential triple-negative breast cancer biomarkers. Cell Oncol (Dordr) 38:433–442
Kwiatkowski F, Girard M, Hacene K, Berlie J. 2000. [Sem: A suitable statistical software adaptated for research in oncology]. Bull Cancer.;87:715–21
Turner NC, Reis-Filho JS, Russell AM, Springall RJ, Ryder K, Steele D et al (2007) BRCA1 dysfunction in sporadic basal-like breast cancer. Oncogene 26:2126–2132
Yamashita N, Tokunaga E, Kitao H, Hitchins M, Inoue Y, Tanaka K et al (2015) Epigenetic inactivation of BRCA1 through promoter hypermethylation and its clinical importance in triple-negative breast cancer. Clin Breast Cancer 15:498–504
Garcia AI, Buisson M, Bertrand P, Rimokh R, Rouleau E, Lopez BS et al (2011) Down-regulation of BRCA1 expression by miR-146a and miR-146b-5p in triple negative sporadic breast cancers. EMBO Mol Med 3:279–290
Kumaraswamy E, Wendt KL, Augustine LA, Stecklein SR, Sibala EC, Li D et al (2015) BRCA1 regulation of epidermal growth factor receptor (EGFR) expression in human breast cancer cells involves microRNA-146a and is critical for its tumor suppressor function. Oncogene 34:4333–4346
Iorio MV, Ferracin M, Liu C-G, Veronese A, Spizzo R, Sabbioni S et al (2005) MicroRNA gene expression deregulation in human breast cancer. Cancer Res 65:7065–7070
Zhang L, Long X (2015) Association of BRCA1 promoter methylation with sporadic breast cancers: evidence from 40 studies. Sci Rep 5:17869
Liu P, Tang H, Chen B, He Z, Deng M, Wu M et al (2015) miR-26a suppresses tumour proliferation and metastasis by targeting metadherin in triple negative breast cancer. Cancer Lett 357:384–392
Stückrath I, Rack B, Janni W, Jäger B, Pantel K, Schwarzenbach H (2015) Aberrant plasma levels of circulating miR-16, miR-107, miR-130a and miR-146a are associated with lymph node metastasis and receptor status of breast cancer patients. Oncotarget 6:13387–13401
Rask L, Balslev E, Søkilde R, Høgdall E, Flyger H, Eriksen J, et al.. 2014. Differential expression of miR-139, miR-486 and miR-21 in breast cancer patients sub-classified according to lymph node status. Cell Oncol (Dordr); 37:215–27
Chen W, Cai F, Zhang B, Barekati Z, Zhong XY (2013) The level of circulating miRNA-10b and miRNA-373 in detecting lymph node metastasis of breast cancer: potential biomarkers. Tumour Biol 34:455–462
Nakata K, Ohuchida K, Mizumoto K, Kayashima T, Ikenaga N, Sakai H et al (2011) MicroRNA-10b is overexpressed in pancreatic cancer, promotes its invasiveness, and correlates with a poor prognosis. Surgery 150:916–922
Chen W-J, Zhang E-N, Zhong Z-K, Jiang M-Z, Yang X-F, Zhou D-M et al (2015) MicroRNA-153 expression and prognosis in non-small cell lung cancer. Int J Clin Exp Pathol 8:8671–8675
Bao B, Ali S, Banerjee S, Wang Z, Logna F, Azmi AS et al (2012) Curcumin analogue CDF inhibits pancreatic tumor growth by switching on suppressor microRNAs and attenuating EZH2 expression. Cancer Res 72:335–345
Visani M, de Biase D, Marucci G, Cerasoli S, Nigrisoli E, Bacchi Reggiani ML, et al.. 2014. Expression of 19 microRNAs in glioblastoma and comparison with other brain neoplasia of grades I-III. Mol Oncol. 8:417–30
Gonçalves A, Sabatier R, Charafe-Jauffret E, Gilabert M, Provansal M, Tarpin C et al (2013) Triple-negative breast cancer: histoclinical and molecular features, therapeutic management and perspectives. Bull Cancer 100:453–464
Cossu-Rocca P, Orrù S, Muroni MR, Sanges F, Sotgiu G, Ena S et al (2015) Analysis of PIK3CA mutations and activation pathways in triple negative breast cancer. PLoS One 10:e0141763
Wang J, Zhang C, Chen K, Tang H, Tang J, Song C et al (2015) ERβ1 inversely correlates with PTEN/PI3K/AKT pathway and predicts a favorable prognosis in triple-negative breast cancer. Breast Cancer Res Treat 152:255–269
Park YH, Jung HH, Ahn JS, Im Y-H (2013) Statin induces inhibition of triple negative breast cancer (TNBC) cells via PI3K pathway. Biochem Biophys Res Commun 439:275–279
De P, Sun Y, Carlson JH, Friedman LS, Leyland-Jones BR, Dey N (2014) Doubling down on the PI3K-AKT-mTOR pathway enhances the antitumor efficacy of PARP inhibitor in triple negative breast cancer model beyond BRCA-ness. Neoplasia 16:43–72
Li J, Song Z, Wang Y, Yin Y, Liu Y, Yuan R et al (2016) Overexpression of SphK1 enhances cell proliferation and invasion in triple-negative breast cancer via the PI3K/AKT signaling pathway. Tumour Biol. doi:10.1007/s13277-016-4954-9
Phua YW, Nguyen A, Roden DL, Elsworth B, Deng N, Nikolic I et al (2015) MicroRNA profiling of the pubertal mouse mammary gland identifies miR-184 as a candidate breast tumour suppressor gene. Breast Cancer Res 17:83
Wang F, Li L, Chen Z, Zhu M, Gu Y (2016) MicroRNA-214 acts as a potential oncogene in breast cancer by targeting the PTEN-PI3K/Akt signaling pathway. Int J Mol Med 37:1421–1428
Xu J-F, Zhang S-J, Zhao C, Qiu B-S, Gu H-F, Hong J-F et al (2015) Altered microRNA expression profile in synovial fluid from patients with knee osteoarthritis with treatment of hyaluronic acid. Mol Diagn Ther 19:299–308
Chai Z-T, Zhu X-D, Ao J-Y, Wang W-Q, Gao D-M, Kong J, et al.. 2015. microRNA-26a suppresses recruitment of macrophages by down-regulating macrophage colony-stimulating factor expression through the PI3K/Akt pathway in hepatocellular carcinoma. J Hematol Oncol; 8:56
Song L, Duan P, Guo P, Li D, Li S, Xu Y et al (2012) Downregulation of miR-223 and miR-153 mediates mechanical stretch-stimulated proliferation of venous smooth muscle cells via activation of the insulin-like growth factor-1 receptor. Arch Biochem Biophys 528:204–211
Chen Z-J, Wei W, Jiang G-M, Liu H, Wei W-D, Yang X et al (2016) Activation of GPER suppresses epithelial mesenchymal transition of triple negative breast cancer cells via NF-κB signals. Mol Oncol. doi:10.1016/j.molonc.2016.01.002
Bhaumik D, Scott GK, Schokrpur S, Patil CK, Campisi J, Benz CC (2008) Expression of microRNA-146 suppresses NF-kappaB activity with reduction of metastatic potential in breast cancer cells. Oncogene 27:5643–5647
Tanic M, Zajac M, Gómez-López G, Benítez J, Martínez-Delgado B (2012) Integration of BRCA1-mediated miRNA and mRNA profiles reveals microRNA regulation of TRAF2 and NFκB pathway. Breast Cancer Res Treat 134:41–51
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y et al (2011) Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121:2750–2767
Acknowledgements
We would like to thank Fabrice Kwiatkowski for his help in analysis data by SEM software.
This research was funded by grants from the Laboratory of Biochemistry Research unit UR 12ES08 Cell Signaling and Disease of Faculty of Medicine of Monastir, the department of Pathology of Farhat Hached Hospital, the Molecular Oncology Laboratory of Center Jean Perrin in Clermont-Ferrand and the Fuda (Founding of the University of Auvergne).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome. The manuscript has been read and approved by all named authors.
Competing Interests
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
Ethics approval and consent was waived by the institutional review board of the Farhat-Hached Hospital of Sousse (Comité d’éthique et de Recherche du CHU Farhat-Hached).
Electronic supplementary material
ESM 1
(DOCX 10 kb)
Rights and permissions
About this article
Cite this article
Fkih M’hamed, I., Privat, M., Trimeche, M. et al. miR-10b, miR-26a, miR-146a And miR-153 Expression in Triple Negative Vs Non Triple Negative Breast Cancer: Potential Biomarkers. Pathol. Oncol. Res. 23, 815–827 (2017). https://doi.org/10.1007/s12253-017-0188-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12253-017-0188-4