Abstract
Twin-screw extruder (TSE), originally built and developed for plastic and rubber industries approximately 100 years ago, is now slowly but steadily gaining popularity in the pharmaceutical industry for manufacturing various dosage forms. TSE has proven to be a robust, multi-purpose, and environment-friendly instrument that has displayed the potential to revolutionize the manufacturing processes in the pharmaceutical industry. Having the facility to arrange process analytical tools at various segments, TSE has given an opportunity to the manufacturers for monitoring the quality of the product at critical stages of the manufacturing process and thus helped in shifting the focus of the pharmaceutical industry from “end product testing” to “building the quality at each stage.” The broad applicability of TSE in formulating ranges of dosage forms is been evident from the large numbers of research papers (more than 100) that have been published and marketed formulations that have entered the market in the last 10 years. The published research papers have demonstrated the applicability of TSE in preparing a variety of dosage forms and intermediates such as pharmaceutical salts, co-crystals, solid dispersions, transdermal gels, solid lipid nanoparticles, and ready to compressed granules.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 1871, Sturges secured one of the earliest patents on single-screw extruders which was designed for pumping soap as a spirally arranged flanges/screws on a shaft [1]. The wide-spread usage of single-screw extruders began in early 1930 for the extrusion of thermoplastic material in the polymer industry and around 1935, they started to get used in the continuous extrusion of pasta products in the food industry [2]. While the initial development of single-screw and twin-screw extruders started relatively simultaneously, the acceptance and widespread implementation of single-screw extruders was smoother and quicker compared to twin-screw extruders due to mechanical simplicity and cost-effectiveness [3]. The major differences between single- and twin-screw extruders lie in the mechanism they use to transport the material (how material moves forward in the barrel) and their mixing intensity [4]. The transport mechanism in single-screw extruders depends on frictional forces between particles and viscous forces in the conveying zone of the melt [5]. In the single-screw extruder, the material creates a static layer on the surface of the screw, and thus the material starts to rotate in the direction of the screw rotation. If the material spends excess time within the barrel, it possibly starts to degrade inside it. Another limitation of the single-screw extruder is its limited processability, which is generally required to be compensated by having long equipment length [6].
Twin-screw extruder was initially developed to integrate several unit operations (such as mixing, melting, and reaction between materials) into a single one. The practical advantage of merging various unit operations into a single one leads to significant improvements in the efficiency of the manufacturing process [7]. Twin-screw extruder creates a specific temperature and pressure inside the barrel, needed for the material to be processed in a specific way. It has the ability to maintain the specific temperature in individual barrel/zone by regulating the flow of heat in that area, while the pressure is regulated by configuring specific screw design and rotation speed [8]. Most of the twin-screw extruders have three distinct zones: a feeding zone, a conveying zone, and an intense mixing zone. Twin-screw extruder gives the flexibility for arranging the screws in different configurations as per requirement and thus makes it a multipurpose instrument [9].
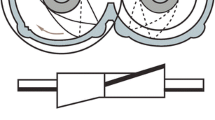
The screws in the twin-screw extruder either rotate in the same direction (co-rotation) or the opposite direction (counter-rotation). The counter-rotating extruders generate very intense pressure and the material is compressed between the gap of the two screws.
Counter-rotating extruders are mainly used in plastics industries where high pressure is required to process materials. The counter-rotating twin-screw extruders are usually operated at a lower speed than the co-rotating twin-screw extruders since they can produce high pressure due to the rotation of the screws in opposite directions. The key drawbacks associated with counter-rotating twin-screw include the possibility of air entrapment, product deterioration due to high pressure, and low material output due to low screw speed [10].
The commonly used extruders in the pharmaceutical industry are of co-rotating type as the intense pressure produced by counter-rotating extruders can degrade the materials used in the pharmaceutical industry. Co-rotating twin-screw extruders used in the pharmaceutical industry are generally of intermeshing type with self-wiping/cleaning ability. The rotation of the screws in the same direction cannot generate as much pressure as being produced in the counter-rotating extruders. To compensate the deficiency in pressure, the screws in co-rotating extruders generally rotate at the high speed compared to counter-rotating screws. The high rotation speed of the screws in the co-rotating extruders also results in the high material output. Another advantage of the co-rotating extruder is the low wear/tear of screws and barrel as they do not experience the pushing action of the material generated due to the rotation of the screws in the opposite directions. In co-rotating twin-screw extruder, it is possible to arrange different types of screw (conveying, kneading, and distributive) elements in a verity of ways to generate unique screw design every time [11].
In the single-screw extruder, the movement of the material depends on the rotational speed of the screws, contrary to that in the twin-screw extruder it depends on the configuration of the screws which makes the material movement in the twin-screw extruders very efficient and fast compared to a single-screw extruder [12]. The two primary-type twin-screw extruders (co-rotating and counter-rotating) can be further classified into non-intermeshing and fully intermeshing type extruders. The non-intermeshing twin-screw extruders have a very limited positive conveying capacity as it cannot form closed/semi-closed compartments.
In the fully intermeshing screw design–type extruders, the backflow of the material is minimum so it works with maximum positive conveying (forward movement) efficiency [13]. Another significant advantage of the intermeshing screw design is that no continuous bed of material exists through the entire length of the extruder as the material length constantly gets broken by the flight of screws [14]. The classification of various types of extruders used in the pharmaceutical industry is given in Fig. 1.
Basic Components of Twin-Screw Extruder
A typical TSE—laboratory scale with its various parts is shown in Fig. 2.
Screw Elements
Various types of screw with different configurations can be arranged on the shaft according to the requirements. The main function of the screw element is to determine the extent of torque (force) transmitted to material due to the rotation of the shaft. The OD/ID ratio (outside screw diameter/inside screw diameter) and channel depth are significant screw parameters that determine the volume available for material to get a transfer and extension of torque transmitted on the materials [15]. As the inner diameter decreases, so do the channel depth and ultimately the volume available for the material to get transferred. An increase in the channel depth decreases the torque transmitted to the material being processed. Screw elements can be broadly classified into three categories: conveying (forwarding), mixing, and zoning elements (screws) [16].
Forwarding elements are positioned at the entry point from where the material enters in the barrel from the feeder, at the vent opening, and the discharge end of the extruder. The main function of forwarding elements is to move the material in the forward direction. Forwarding elements are always flighted in a forward position that is why they have very limited mixing capacity and exert very limited pressure on the material. The forwarding elements with larger pitch have a higher conveying capacity (Fig. 3) [17].
The mixing element/kneading elements exert considerable torque on the material and have a high mixing ability (Fig. 4). Based on the material required to be processed, different numbers of kneading zones can be strategically arranged on the shaft. Kneading elements can be of the dispersive type or distributive type [18]. Distributive elements have very narrow widths which repeatedly divide and recombine the melt streams of the material whereas dispersive elements have very broad width which generally squeeze, and lengthen the material.
Another parameter that regulates the intensity of mixing and pressure exerted on the material is the offset angle of kneaders [19]. As the offset angle between the successive kneading screws increases, the pressure exerted on the moving material also increases. Depending on the offset angle of the kneading elements, they can be classified as forwarding, neutral, or reversing type kneading elements. For the kneading element, screws with offset angles of 30° and 60° are known as forwarding screws, while 90° is considered neutral and more than 90° is considered reverse screws [20].
Zoning elements separate various unit operations that are going along the length of the shaft. For example, the zoning element downstream of the kneading section ensures that the material is uniformly mixed and processed before leaving the kneading section (Fig. 5). Another type of zoning element arranged near the vent restricts the vacuum from getting spread upstream or downstream within the barrel. The reverse flighted screw elements are used as zoning elements in cases where intense pressure is required to process the material [21].
Barrel
The shaft containing screws are arranged on the barrel that withstands the pressure. The barrel opening of the twin-screw extruder is of the shape “8.” The outer part of the barrel is made up of high strength steel whereas the liner is made up of sturdy and corrosion-resistant material as per requirement. Conventionally, the heat is generated inside the barrel either by placing electronic external heater bands or by internal electrical cartridges. The entire barrel length can also be divided into different zones and the specific temperature of each zone can be maintained according to requirements. The length of the processing section in TSE is described in terms of the length to diameter (L/D) ratio which is the ratio of the overall length of the processing section to the outer diameter of the screws. For example, if the OD is 20 mm and the length of the processing section is 400 mm, then L/D ratio would be 20/1 [22]. Depending on the scale of the production and material handling capacity, different extruders have different L/D ratio.
Feeder
The material is added to TSE by using vibratory trays and single-screw/twin-screw augers. The most widely used, loss-in-weight type of feeder maintains a constant flow of the material (mass bases) by adjusting the feed rate from the hopper. The piston or gear pump is used to feed the liquid material into the barrel. The piston/gear maintains the specific injection rate of the liquid materials into the barrel based on the viscosity of the liquid. Generally, the extruder is kept in starve-fed position—the amount of material added to the barrel is less than it can accommodate. The feed rate of the material in the barrel can have a very significant effect on the critical characteristics of the end product [23].
Being a multi-purpose instrument, TSE has been used to prepare a wide range of formulations. The following section explains the advantages and procedures to prepare various dosage forms prepared by using TSE. Table 1 summarizes the list of marketed product which are developed or manufactured by using TSE [3, 24,25,26,27].
Film
Traditionally, transdermal and/or transmucosal films for drug delivery are produced by film-casting techniques. The drug, polymer, and other required excipients are dissolved in a common solvent. The prepared solution is spread on the plain surface for the evaporation of the solvent and the resultant dry film is subsequently scrapped and cut in an appropriate size for the application. Production of the mucoadhesive film by TSE offers many advantages over this traditional technique such as: (1) being a green technique, no solvent is required; (2) it is a continuous process; (3) low production cost; and (4) efficient mixing of drugs with polymer (Fig. 6) [28, 29].
Palem et al. have prepared the domperidone (DOM) buccal film by using TSE and evaluated its in vitro and in vivo performance. The films with three different compositions were prepared by using Prism 16 mm Euro Lab co-rotating TSE, rotating at 50 rpm with the barrel temperature ranging from 120 to 160 °C. The extruded films confirmed no drug excipient interaction and had excellent content uniformity. The optimized HME film formulation exhibited a tensile strength of 0.72 kg/mm2, elongation at break of 28.4%/mm2, the in vivo residence time of 120 min, peak detachment force of 1.55 N, work of adhesion of 1.49 mJ, swelling index of 210.2%, erosion of 10.5%, and 84.8% in vitro drug release in 2 h. The results of the bioavailability study in healthy human male volunteers displayed improvement in drug permeation from the buccal formulation prepared by TSE compared with the marketed tablet. The bioavailability of the drug released from the buccal film was statistically significant (1.5-fold higher) than oral formulation [30].
Mididoddi et al. have prepared transdermal films of ketoconazole for onychomycosis by using hydroxypropyl cellulose (HPC) and poly(ethylene oxide) (PEO) as polymers. The six batches were prepared by using Killion extruder-KLB-100, co-rotating screw extruder at temperature ranging between 150 and 160 °C. Bioadhesion studies proved that the HPC films tested on “etched” nails had significantly higher peak adhesion force (PAF) and area under the curve (AUC) than that of non-treated “control” nails. The result of DSC, SEM, and XRD studies confirmed the amorphous nature of the drug in the films prepared by TSE. The prepared films were stable for 12 months at 25 °C/60% RH in an unpackaged condition [31].
Regev et al. have prepared dapivirine vaginal film by film casting method and by using TSE. The polymeric thin films were manufactured by utilizing Nano-16 mm Leistritz Extruder Twin Screw at 105–145 °C and 150–210 rpm. The prepared films were compared for physicochemical, biological, and safety characteristics including in vitro drug release, mechanical strength, tissue permeability, compatibility with vaginal Lactobacilli, and in vitro bioactivity. The results showed that the films prepared by TSE was not only thicker and had higher weight compared to film prepared by casting method but also had lower water content and had faster disintegration time. The puncture strength (normalized to film thickness) of the films prepared by TSE was found to be similar to that of the film prepared by the solvent casting method, suggesting similar mechanical properties required for user acceptability. The films prepared by TSE disintegrated much rapidly (0.78 min) compared to the film prepared by the solvent casting method (6.33 min). The microscopic study indicated the presence of no particulate matter (crystalline drug) in the extruded DPV film. The in vitro assay exhibited no cellular toxicity of the film prepared by TSE proving its non-toxic nature [32].
Repka et al. have prepared muco-adhesive matrix film of 10% (w/w) clotrimazole (CT) for local applications in the oral cavity. The CT film was prepared at a temperature range of 125–130 °C utilizing a Killion-KLB-100 extruder equipped with a 6-in. flex-lip die at 70 rpm. The film was prepared by using HPC and poly(ethylene oxide) as polymeric carriers and the polycarbophil as a bioadhesive material. The extruded films demonstrated excellent content uniformity and a post-processing drug content of 93.3%. The result of the DSC and XRD study proved molecular level dispersion of drug within the extruded films. The films had desirable and consistent release properties along with acceptable bioadhesive strength (PAF = 3.63 N, work of adhesion = 0.61 N/mm). The drug release from the film was 100% in less than 8 h with the erosion-controlled mechanism [33].
Chen et al. have prepared bioadhesive films of miconazole by using PolyOx—poly(ethylene oxide) and Klucel as polymers. The films were prepared by using Prism 16 mm, Euro Lab extruder equipped with a 6-in. flex-lip die. The influence of different processing parameters such as temperatures (160, 175, 190, and 205 °C), extruder screw speeds (30, 50, and 70 rpm), and formulation composition on the critical film properties such as bioadhesiveness, temperature stability, and drug release properties were examined. The XRD studies proved that the films were stable for 8 months. All the films prepared by TSE were able to sustain the release of miconazole for approximately 10 h [34].
Wet Granulation
Tablets account for more than 80% of all commercially available dosage forms [35]. However, for most drugs, it is practically impossible to directly compress API into tablets as most APIs lack flowability and compressibility required for direct compression. Among wet granulation, dry granulation, and direct compression—three prominent methods used for tablet manufacturing, wet granulation is the most predominant and competent granulation process. In the wet granulation process, mixture of API and other suitable excipients, such as diluents and disintegrating agents, is granulated using a granulating liquid (water or a hydroalcoholic solution containing suitable binder) [36]. One of the critical limitations of the wet granulation technique is low drug loading efficiency. This meant the large quantity of excipients is often required to improve tableting properties and thus limiting drug load of less than 50% [37]. Since the inception of basic principles related to tablet manufacturing around 1950 to 1960, there have been no substantial changes in the manufacturing principles [38, 39]. Much of the changes that were implemented in the tablet manufacturing process were related to the scale of the equipment but the fundamental principles virtually remained the same. Janet Woodcock, head of Center for Drug Evaluation and Research at the Food and Drug Administration had reflected this stalemate in the 2011 annual meeting of American Association of Pharmaceutical Scientists in the following words “the manufacturing will change in the next 25 years as current manufacturing practices are abandoned in favour of cleaner, flexible, more efficient continuous manufacturing.”
Continuous wet granulation by twin-screw extruder combines mixing, granulation, and drying in a single step and can produce directly compressible granules that do not require further processing step (Fig. 7) [40,41,42]. It also allows automation, facilitates the incorporation of process analytical technology tools, provides real-time quality information, reduces manufacturing cost, and needs less space for installation compared to the conventional wet granulation method [40, 43,44,45].
Maniruzzaman et al. have used a continuous wet granulation process by using TSE for the manufacturing of ibuprofen (IBU) granules. The dry blends of the drug, polymer, inorganic carrier, and the binder (PEG) were fed into the EuroLab-16 twin-screw extruder with a L/D ratio of 40. Three kneading zones were used for all the granulation trials and granulating fluid—ethanol was supplied at a constant rate. The extruded granules were dried in an oven at 30 °C for 2 h and micronized through a cutter milled. The extruded granules showed uniform particle size distribution and excellent flowability. The results of dissolution studies indicated that the dissolution rates varied between 65 and 80% after 120 min for the extruded granules while it was only 10% for bulk IBU. The X-ray analysis indicated that a small fraction of pure drug was converted to amorphous form within the granules. The increased dissolution rate was attributed to the adsorption of the drug in the inorganic porous network and reduced particle size due to intense mixing in the barrel [46].
Meena et al. have performed wet granulation using a twin-screw extruder for improving the tablet ability of poorly compactible drug—acetaminophen. Acetaminophen (95%) was mixed with binders (5% povidone or partially pregelatinized starch) and wet granulated by using Process-11 (Thermo Fisher Scientific), a co-rotating twin-screw extruder without using the die plate at 70 °C with 7% (w/w) water (200 rpm and 40 to 90 °C). The L/D ratio of the extruder was 40:1 with a barrel diameter (D) of 11 mm. The optimized process was able to give > 90% granules of the total weight of the powder material added to the extruder in the size range of 125 to 1000 μm without any milling step. The tablets produced by compressing prepared granules had high drug loading capacity (93.6% drug load) and superior mechanical strength (hardness > 1.7 MPa), compared to the tablets prepared by conventional high shear wet granulation [47].
Melt Granulation
Melt granulation is an agglomeration technique where granules are prepared due to the softening or melting of binders that are heated to near or above their melting point. Melt granulation is commonly performed in high shear mixers by using hydrophobic binders such as microcrystalline waxes, paraffin, and glycerol monostearate which can give sustained-release formulations whereas hydrophilic binders such as polyethylene glycols are used for preparing immediate-release formulations [48]. In high shear mixers, the melting or softening of the binder is triggered by the external heating element and/or heat generated due to friction between particles. The heat generated because of the friction between the particles makes it difficult to regulate the temperature during the granulation process which could result in uncontrolled granule growth and thermal decomposition of materials [49].
The melt granulation by twin-screw extruder allows intimate mixing between the drug substance and the binder inside the barrel. The upper limit of temperature in a high shear granulator is usually 100 °C, compared to that much higher temperature and uniform distribution of heat can be achieved in a twin-screw extruder. Another critical advantage of using twin-screw extruder is that being a continuous process, the end product output can be easily increased by extending the time of usage [50].
Thiam Tan et al. have developed a melt granulation process by using a combination of hydrophilic binder (HPMC K4M, PEO 1 M) and hydrophobic binder (Compritol® ATO 888, Precirol® ATO 5) to produce directly compressible granules of verapamil. 60% verapamil, 1% colloidal silicon dioxide, and binders in the specific ratio were blended. The pre-mix was extruded through Nano-16 (Leistritz) Co-rotating Twin-Screw Extruder. The barrel temperature was kept below the melting point of verapamil (140 °C). The co-rotating screw configuration consisted of kneading blocks and conveying elements to have required level of mixing. The extrudes were cooled to room temperature and milled to granules using a conical mill. The result of in vitro dissolution studies indicated a significant impact of process parameters such as drug/binder ratio and hydrophilic polymer/binder ratio on the key characteristic of prepared granules. The prepared granules were directly compressed using 10 mm diameter single-punch-tableting hydraulic press. The drug release from HPMC K4M–and PEO 1-M–based formulations fit both diffusion and erosion mechanism. However, only CP35-D (Compritol® ATO 888:PEO 1 M = 35:5—direct molded) and CP35-M (Compritol® ATO 888:PEO 1 M = 35:5—milled) were observed to follow the diffusion release mechanism [51].
Keen et al. have developed a continuous granulating process with the help of TSE for preparing directly compressible granules of tramadol HCl. Tramadol HCl and glyceryl behenate were added to 16 mm Nano-16 Twin-Screw Extruder with (20:1) L:D ratio, operating at 200 rpm and 80 °C. The screw design had two kneading block sections for all experiments. The first kneading block section (30° offset) extended from 11 to 13 diameters of the screw length. The second kneading block section (60° offset) extended from 16.5 to 18.5 diameters of the screw length. The release profile of continuous twin-screw granules had minimal burst, yet were able to release complete drug within 16 h. The formulation was also able to resist alcohol-induced dose dumping of the drug [52].
Batra et al. have screened different polymeric binders for their suitability to improve the compactibility of two poorly compressible drugs—metformin hydrochloride and acetaminophen by using the twin-screw melt granulation process. The processing temperatures for the drugs were set at 180 °C and 130 °C for metformin hydrochloride and acetaminophen, respectively. Screw configuration, screw speed, and feed rate were optimized in such a way that all polymeric binders were able to produce directly compressible granules. The granules produced using only 10% (w/w) concentration of hydroxypropyl cellulose, hydroxypropyl methylcellulose, polyvinylpyrrolidone, Klucel® EXF, Eudragit® EPO, and Soluplus®, demonstrated good tablet tensile strength (> 2 MPa) [53].
Taste Masking
In the pharmaceutical industry, the number of APIs stimulating unpleasant taste (e.g., salty, acidic, or metallic) is steadily increasing, making taste masking a pre-requisite for improving the palatability and compliance of orally administrated products, especially for pediatric/geriatric patients [54]. The most commonly used methods for taste masking are film coating and the addition of sugars, flavors, or sweeteners in the formulation [55]. The latter method has a restriction in terms of maximum allowed concentration in the formulation due to regulatory requirements. Freeze drying, microencapsulation, fluidized bed coating, high shear mixing, supercritical fluids, and spray drying have successfully been used to mask the taste of various bitter active substances [56]. Taste masking by twin-screw extruder offers several additional advantages such as: it is a continuous process, easy to scale up, applicable to moisture-sensitive APIs, provides enhanced API stability within the carrier matrix, and also being rapid as well [57].
Alshehri et al. have used twin-screw extruder for masking the bitter taste of mefenamic acid (MA) by using Eudragit® E PO as a polymer. Mefenamic acid was blended with Eudragit® E PO at drug loadings of 20%, 25%, 30%, and 40% using a V-shell blender. The binary mixtures of drug and polymer were added to 16 mm Prism, Euro Lab (Thermo Fisher Scientific) co-rotating twin-screw extruder at 110 °C temperature with a screw speed of 100 rpm. The extrudates were milled and sieved by USP mesh (#35). The result of DSC and XRD studies revealed that MA was present in the amorphous phase in all the formulations. Two optimized formulations (with 20% and 25% drug loads) were selected to formulate the orally disintegrating tablets (ODTs). The drug release (in acetate buffer) from the 20% and 25% drug-loaded extrudates reached more than 85% within 40 min, whereas it was less than 1% for the pure drug and less than 15% for the physical mixture (20% of drug load). The prepared tablets had acceptable friability and disintegration time in addition to having the desired taste-masking effect [58].
Pimparade et al. have developed an orally disintegrating tablet (ODT) of caffeine citrate using TSE by adding ethyl cellulose as a polymer and other suitable plasticizers. The blends of the drug, polymer, pore former, and plasticizer were melt extruded using 11 mm Process-11 (Thermo Fisher Scientific), a co-rotating twin-screw extruder with a modified screw design at 50 rpm over a temperature range of 125–130 °C. The extrudates were milled and sieved through #40/35. An Astree e-tongue system equipped with an Alpha M.O.S sensor set #2 was used to assess the extent of taste masking of API. The test-masking studies performed on 9 healthy volunteers proved that the optimized formulation was statistically significant in masking the taste of drug compared to other tested formulations [59].
Juluri et al. have investigated the potential of Kleptose Linecaps DE17 (KLD), a spray-dried amylose pea maltodextrin, for masking the unpleasant/bitter taste of griseofulvin (GRI) and caffeine anhydrous (CA). Amylose pea maltodextrin is obtained by partial hydrolysis of pea starch. GRI and CA at 15% (w/w) and 70% (w/w) KLD and xylitol as plasticizers at a concentration of 15% (w/w) were blended in a V-shell blender. The pre-mix was extruded using co-rotating twin-screw extruder at 100 rpm and a temperature range of 150/155 °C (first zone/later zones). The melt extrudates were milled and screened through USP mesh (#40 pass and #50 retains) to prepare particle/granules. Dissolution studies of HME extrudates using simulated salivary medium displayed three times less drug release from the formulation compared to the physical mixture at the end of 5 min (the lesser drug release, the better the taste-masking efficiency). Furthermore, the results from the sensory evaluation in the human panel demonstrated that there is a statistically significant difference (P < 0.05) in the bitterness score between formulation prepared by TSE and physical mixture [60].
Delay-Released Tablet
Delay-released/sustained-release dosage forms have made it possible to achieve optimum utilization of a substantial number of drugs in specific disease conditions such as rheumatoid arthritis, gout, angina pectoris, etc. Conventionally, these kinds of dosage forms are prepared by entrapping the drug molecules within the slow-dissolving/eroding polymers (matrix type) or coating the drug layer with a suitable semi-permeable/selectively dissolving membrane (reservoir type) [61]. These conventional approaches suffer from some of the critical process or formulation-related limitations such as the following: (1) inability to accommodate high doses, (2) inefficient distribution of drug within the polymeric matrix, and (3) additional processing steps required for making a reservoir-type system that led to costing and complexity. The preparation of delay releases/sustained-release formulations by TSW not only provides an opportunity to overcome the above-mentioned limitations but also provides other unique advantages such as the following: (1) avoidance of organic solvent, (2) single-step operation, and (3) minimum burst effect due to the intimate mixing of drugs with polymers [62, 63].
Dumpa et al. have prepared a chronotherapeutic drug delivery system of ketoprofen (KTP) and IBU by using TSE. Eudragit S100 (ES100) and ethyl cellulose (EC) (2.5 and 5%) were used as the matrix-forming agent and release-retarding agent, respectively. The extrudates were prepared by using Prism Euro Lab (Thermo Fisher Scientific) 16-mm Co-rotating Twin-Screw Extruder and were subsequently filled in the capsule for chronotherapeutic delivery. KTP with 40% drug loading with EC (2.5 and 5%) and ES100 was extruded at a temperature of 120 °C, 100 rpm screw speed, and feed rate of 5 g/min. The IBU at 40% drug loading with EC (2.5 and 5%) and ES100 was extruded at 100 °C, 100 rpm screw speed, and 5 g/min feed rate. The results of DSC and XRD studies verified that drugs were homogeneously dispersed within the matrix in amorphous form. The prepared formulation had the desired lag time of 6 h, tested in three-stage in vitro dissolution drug-release study. The percentage drug release from 1, 2, and 3 mm pellets with 40% drug load showed < 20% release from all formulations at 6 h. The results of accelerated stability (40 °C/75% RH, 100%) proved that both KTP and IBU formulations were stable for 4 months [64].
Almeida et al. have prepared mini-matrices of metoprolol tartrate—model drug by using different grades of ethylene-vinyl acetate (EVA9, EVA15, EVA28, and EVA4) with vinyl acetate (VA) content of 9%, 15%, 28%, and 40%, respectively. The mini-matrices were prepared by extruding the material through Haake MiniLab II Micro Compounder (Thermo Electron) Co-rotating Twin-Screw Extruder operating at different screw speeds (40, 60, and 90 rpm) and processing temperatures (60, 80, 90, 100, 110, 120, 130, and 140 °C). The study proved that while EVA40 and EVA28 could only be processed at a temperature of 60 °C, EVA15 and EVA9 required temperature of 100 and 110 °C, respectively. The results of the DSC analysis also proved that the extrusion process did not change the polymorphic structure of the drug (remained in crystalline form only). It was also observed that there was a significant effect of various grades of EVA on the drug release from EVA/MPT matrices (50/50, w/w) [65].
Tiwari et al. have prepared sustained-release multiple unit dosage form of venlafaxine hydrochloride (VH) by using cellulosic polymer (ethylcellulose) and acrylic polymers (Eudragit RS PO). The effect of various formulation factors such as type of polymers, polymer concentration, type of plasticizers (dibutyl sebacate, triethyl citrate, acetyl tributyl citrate, PEG 6000), and concentration of plasticizers on the drug release was evaluated. The extrudates were prepared by laboratory-scale Pharma-11 (Thermo Fisher Scientific, Germany) Co-rotating Twin-Screw Extruder with a length-to-diameter ratio of (40 L/D) at a 50-rpm screw speed and a powder feed rate of 300 g/h (45–150 °C). The results of DSC and XRD studies proved that the VH was present in the crystalline form within ethyl cellulose and Eudragit RSPO matrix. Plasticizer concentration did not have a significant impact on the percentage of drug release at 8 h contrary to the type of plasticizer had significant effect. In vivo evaluations in the rabbit indicated a significant increase in the time to reach maximum concentration (tmax) and extent of absorption (AUC (0-∞)) from the extended-release pellets compared to the VH immediate release blends [66].
Yang et al. have prepared sustained-release pellets of metoprolol tartrate (MT) by using ethyl cellulose (EC) as a sustained-release carrier, and stearic acid (SA) as an erosive coating material. The cores containing EC were prepared by using TSE, and the prepared cores were coated with SA by using hot-melt method. MT (30%, w/w, based on the formulation weight), EC, and plasticizers were fed into a Haake TM Mini CTW (Thermo Fisher Scientific) Twin-Screw Extruder. The screw speed was 10 rpm, and the residence time was kept at 10 min. The obtained extrudates were cooled at room temperature, cut into mini-matrices, and spheronized at about 100 °C. The spheronized particles were coated with a mixture of SA and PEG 6000 (96:4, w/w). The result of the in vivo study in rats proved the plasma concentration of coated pellets increased slowly in the first 2 h, was maintained steady state for about 4 h, and decreased gradually after 6 h. The prolonged Tmax and reduced Cmax proved sustained release of MT from the coated pellets compared with the immediate release solution [67].
Vithani et al. have developed sustained-release tablet formulations of diclofenac sodium by using lipid matrices made up of Compritol 888 ATO. Diclofenac sodium/Compritol 888 ATO dry powders were mixed properly and extruded by using Eurolab 16 Twin-Screw (Thermo Fisher Scientific) Extruder at 25 rpm screw speed, 0.7 kg/h feed rate, and the temperature below 80 °C. The extruded pellets were milled and passed through a 500-mm mesh sieve. The extruded granules were blended with lubricants and mixed for 10 min and compressed at 10 kN compression forces using a Flexitab trilayer tablet press. Results of in vitro dissolution studies proved that the tablets were able to sustain the release for more than 12 h [68].
Ma et al. have developed hydroxypropyl methylcellulose (HPMC)–based controlled release formulations of theophylline by using TSE. The drug, propylene glycol, and various grades of HPMC were mixed and were placed in a K-tron KT-20 feeder (Pitman, NJ) for extrusion; 16 mm Prism PharmaLab-16 (Thermo Fisher Scientific) twin-screw extruder with a 6 mm strand die was used for the extrusion process (150–170 °C, 100–300 rpm, and 10–40 g/min feed rate). The dissolution results displayed sustained release of the drug for more than 8 h without burst release from the formulations [69].
Vasanthavada et al. have developed a modified-release formulation of imatinib mesylate, with a drug load of approximately 90% by using a twin-screw extruder. The imatinib mesylate was mixed with release-controlling polymers and extruded through 16 mm co-rotating twin-screw extruder with a length-to-diameter ratio of 40:1 at 185 °C. The extruder barrel was divided into six temperature zones. Each of the zones was maintained at a fixed processing temperature as follows: 50 °C (zone 1), 110 °C (zone 2), 130 °C (zone 3), 170 °C (zone 4), and 185 °C (zone 5), and zone 6 was for the die, which was not used. The formulations were able to release 100% drug from 2 to > 8 h based on the type and quantity of the polymer used. Tablets containing the water-insoluble polymer-EC retarded drug release to a greater extent than those containing water-soluble polymer—HPC. Compared to tablets produced by wet granulation technology with similar compositions, the tablets produced by TSE had better hardness and crushing strength. Further, the tablets met acceptable friability testing criteria of less than 0.8% weight loss at a mean compression force of 15–20 kN. The result of in vivo bioavailability study in humans demonstrated that the administration of a single dose of imatinib 800 mg containing HPC resulted in a peak concentration approximately twofold that of the first peak and 1.5-fold of the second peak compared to Gleevec®400 mg IR formulation [70].
Patil et al. have prepared sustained-release matrix tablets of ondansetron HCl with the help of TSE by using stearic acid as a binding agent. Ondansetron HCl (20% w/w) was blended with other excipients such as hydroxypropyl cellulose, ethyl cellulose, fumaric acid, and stearic acid. The premix was passed through a fully intermeshing co-rotating twin-screw extruder (11 mm, Process 11, Thermo Fisher Scientific) with a modified screw design. Among eight zones, zone 2 and zone 3 were set at 110 °C, zone 4 was set at 70 °C and the remaining zones (zones 5–8) were heated to 50 °C. All the formulations had content uniformity of (> 98%) after the melt granulation. The in vitro release study demonstrated 90% of drug release in 24 h from the formulations containing stearic acid + ethyl cellulose and 100% drug release in 8 h from the formulation containing stearic acid + hydroxypropyl cellulose [71].
Solid Dispersion
The term solid dispersion was coined in the early 1970s by Chiou and Riegelman for describing the dispersion of an API in an inert carrier by using solvent, melting, or other methods. However, nowadays, the term solid dispersion is modified as amorphous solid dispersion—a glass solution where the amorphous form of poorly soluble drug is entrapped within inert amorphous polymeric carrier [72]. A glass solution in the true sense is a one-phase system in which all molecules of the API are intimately mixed with the carrier molecules. Such situation is more favorable for improving the dissolution properties of the poorly soluble drug as the drug is entrapped in molecularly dispersed state or in amorphous form within polymeric matrix [73]. Co-milling, melting method, solvent evaporation, and co-precipitation are some of the popular methods for preparing amorphous solid dispersions [74]. The formulation of amorphous solid dispersion by using a twin-screw extruder is a continuous process where the drug, polymer, and optional excipients such as plasticizers are mixed intimately under controlled conditions of temperature and shear pressure [75]. The processing temperature is usually kept adequately higher than the glass transition temperature of the polymer to induce sufficient plasticity to have uniform distribution of polymer throughout powder material [76]. The processing temperature is usually kept 15–30 °C above the glass transition temperature of the polymer but below the melting point of the drug to ensure the uniform molecular dispersion of the drug within the polymer matrix [77]. Other advantages of using twin-screw extruders are as follows: continuous process, green process, allows automation, facilitates the incorporation of process analytical tools that can provide real-time information regarding the quality of the product, reduces manufacturing cost, and requires less manufacturing space as it performs many unit operations simultaneously (Fig. 8) [78].
Zi et al. have developed solid dispersions (SD) of lopinavir (LPV) to improve its bioavailability and other physicochemical properties. Kollidon VA 64® (VA64)—a hydrophilic polymer and Soluplus®—a polymeric surfactant were used to prepare the polymeric matrix for the dispersion of the drug. The dissolution profiles of extrudates prepared by TSE were significantly better than those solid dispersions prepared by the solvent evaporation method. The optimized formulations containing LPV-polymer-sorbitan monolaurate (SBM)-CLSF (Kollidon® CL-SF) in the ratio of 1:4:0.4:0.6 (w/w), respectively were prepared by using process 11 (Haake, Thermo Fisher) co-rotating twin-screw extruder with 11 mm diameter screws and the length/diameter ratio of 40:1. The bioavailability of LPV in soluplus-matrixed extrudates was 1.70-fold higher than the extrudates with VA64 and 3.70-fold higher than LPV crystal. In situ permeability and Caco-2 cell transport studies revealed that soluplus significantly enhanced the permeability of LPV through rat intestine and Caco-2 cell monolayer. The soluplus-matrixed extrudates showed a statistically significant enhancement in the absorption of LPV through the jejunum segment of the rat while extrudates composed of VA64 showed no such trends. After 6 months of storage at 25 °C/60% RH, the LPV-polymer-SBM-CLSF extrudates show no sign of drug crystallization. Contrary to that the drug presence in that solid dispersion prepared by solvent evaporation indicated recrystallization of the drug [79].
He et al. have prepared a solid dispersion of fenofibrate by using Eudragit E100 and PVP-VA as a carrier in TSE. The results of the DSC and XRD studies proved that the fenofibrate existed in the noncrystalline state in both kinds of solid dispersions. The solid dispersion prepared with Eudragit E100 polymer (1:2) has the dissolution of 84% and 65% at 60 min in 0.1 M HCl and water, respectively, whereas the solid dispersion prepared with the ratio 1:4 has 73.6% and 87.3% drug release, respectively. The solid dispersion prepared with PVP-VA (1:2) has the dissolution of 60% and 65% at 60 min in 0.1 M HCl and water, respectively, whereas for the ratio of 1:4, it was 64% and 53%, respectively, in the same dissolution media. The solid dispersion containing Eudragit E100 (1:4) had 177.1% times higher bioavailability compared to the micronization Lipanthyl® capsule [80].
Jijun et al. have prepared nimodipine solid dispersion by using a mixture of Eudragit® EPO and Kollidon VA-64 as carriers. Solid dispersion was prepared by using Coperion KEYATE-20 (Nanjing, China) Twin-Screw Extruder. The feed rate and screw rate were set at 3.5 Hz. The temperatures of the extruder barrel zone and die were set between 80 and 130 °C. The results of the DSC and XRD studies proved the amorphous nature of drugs within the extrudates. The 90% drug released was observed in 1 h in 900 mL 0.1 M HCl. The extruded material was collected, milled, passed through an #80 sieve, and compressed to tablets using the wet granulation method and dry granulation method. Recrystallization was observed to some degree in the tablet prepared by the wet granulation method after the storage period, contrary to that the tablets prepared by the direct compression method were able to maintain the amorphous nature of the drug [81].
McFall et al. have formulated aripiprazole (ARI)-loaded pH-modulated solid dispersions to enhance the solubility, dissolution, and bioavailability of the drug. Kollidon® 12 PF (PVP) and succinic acid were used as polymers and acidifiers, respectively. A mixture of ARI (20–40%, w/w), PVP (60–80%, w/w), and succinic acid (0–10%, w/w) was extruded at 120 °C using a Process-11 (Thermo Fisher Scientific) Twin-Screw Extruder with the screw speed varied between 80 and 120 rpm. The extrudates were milled into a fine powder to subsequently compressed into tablets by using a direct compression method. The results of the dissolution studies proved that the formulation batches containing acidifier had the highest levels of drug solubility (> 15,000 μg/mL) and better drug release profiles (>90%) compared to the pure drug and other formulations. Results of in vivo studies proved that the optimized batch had significantly better oral bioavailability (Cmax and AUC0–12) than the pure ARI [82].
Kate et al. have prepared atovaquone solid dispersion by using various hydrophilic polymers such as PVP K-30, PVP-VA 64, and HPMC E5 and plasticizer such as Tween 80, docusate sodium, polyethylene glycol (PEG) 400, Gelucire® 44/14, soluplus®, Poloxamer 188, PEG 6000, and VBP-1. Solid dispersions were prepared by using Haake MiniLab Conical Co-rotating Screws Twin-Screw Extruder (Thermo Scientific) at a maximum temperature of 350 °C and the maximum pressure of 200 bars. The optimized formulation containing PVP VA 64 as polymer and soluplus as plasticizer had a better release profile compared to Malarone® tablets. The result of in vivo studies proved 3.2-fold and 4.6-fold higher bioavailability for the optimized formulation compared to Malarone® tablets and atovaquone pure drug, respectively. The enhanced bioavailability of the optimized formulation also resulted in 100% anti-malarial activity in murine infection model at 1/8th of the therapeutic dose [83].
Yang et al. have prepared solid dispersions of nimodipine by using HPMC, Eudragit® EPO, ethyl acrylate, Plasdone S630® as a polymeric carrier in TE-20 32:1 (Coperion Keya Co., China) Co-Rotating Twin-Screw Extruder. The feed rate was fixed at 60 rpm, and the screw rate was set at 40 rpm. The five temperature zones were set at 100, 130, 130, 140, and 145 °C from feeder to die for both Eudragit® EPO and PVP/VA and 100, 140, 170, 170, and 175 °C for HPMC. The results of in vitro dissolution studies indicated that Nimotop® tablets and the capsules containing PVP/VA extrudates exhibited rapid drug dissolutions—more than 70% drug released within 15 min. The drug release from HPMC-containing extrudates were intermediate, while extrudates containing Eudragit® EPO were able to release only 40% of the drug after 1 h. All solid dispersions had a faster dissolution rate compared to their physical mixtures. The mean bioavailability of nimodipine solid dispersion prepared with Eudragit® EPO and Nimotop® were comparable, but the solid dispersions prepared with HPMC and PVP/VA exhibited much lower bioavailability. However, the AUC0–12 h values for all three solid dispersions were significantly higher than physical mixtures made up of the same compositions [84].
Fule et al. have developed solid dispersion containing two antimalarial drugs—artemether (ARTM) and lumefantrine (LUMF). Soluplus® (polyethyleneglycol–polyvinyl caprolactam–polyvinyl acetate grafted copolymer) was used as a primary carrier to prepare matrices and PEG 400, Lutrol F127, and Lutrol F68 were used as surfactants. Drugs, soluplus (1:1), and calculated quantity of selected plasticizers were mixed and extruded through Pharma-11 (Thermo Scientific) Twin-Screw Extruder. The solubility and in vitro dissolution performance of both drugs in solid dispersion formulations were improved significantly compared with pure drugs and marketed products. The pharmacokinetic studies in rats revealed that the solid dispersion had 44.12–65.24-fold increase in the AUC(0–72) and 42.87–172.61-fold improvement in Cmax compared to that of pure drugs and commercial product [85].
Co-crystals
Co-crystals are multi-component molecular crystals in which chemically different molecules are present at fixed stoichiometric ratio [86]. Co-crystallization offers a convenient way to modify the physicochemical properties of APIs such as dissolution rate, intrinsic solubility, melting point, hygroscopicity, compressibility, bulk density, and friability. Using twin-screw extruder to prepare co-crystals offers several advantages such as highly intensive mixing, close material packing that improves surface contact between drug and co-former leading to the formation of co-crystals without using any organic solvents (Fig. 9) [87].
Shaikh et al. have prepared co-crystal of theophylline and 4-aminobenzoic acid (1:1 mol ratio) by using polyethylene glycol as a binder. Melt granulation was carried out in a co-rotating 12 mm hybrid mini-extruder (Three-Tec GmbH) with two kneading zones separated by conveying elements. The result of DSC and XRD studies proved that melt granules containing 5% of PEG 8000 have higher purity and crystallinity compared to other concentrations used (10%, 20%, and 30%). The melt-granulated co-crystals have better tensile strength compared to pure drug and co-crystals prepared by other methods. Moreover, the prepared THP-4ABA melt-granulated co-crystals were stable for 14 days at 50 °C and 75% RH [88].
Moradiya et al. have prepared carbamazepine (CBZ)–trans-cinnamic acid (TCA) co-crystals (equimolar) by using Eurolab 16 Twin-Screw Extruders (Thermo Fisher, Germany) at temperature below 135 °C at a screw speed of 10 rpm. The results of the DSC study and XRD proved that the prepared co-crystal was of high purity. The extruded co-crystals showed faster dissolution rates compared to bulk CBZ and the prototype co-crystals [89].
Daurio et al. have prepared AMG 517–sorbic acid co-crystal using a twin-screw extruder. A Prism Pharma Lab 16 mm Twin-Screw Extruder (25: 1 L/D) with four kneading zone was used at a maximum temperature of 135 °C. The quantitative HPLC analysis proved that the conversion of AMG 517 free base to the AMG 517–sorbic acid co-crystal in the TSE was higher than 99%. In addition to improving the surface area, the co-crystals produced by the twin-screw extruder also improved bulk density and flow function coefficient [90].
Fernandes et al. have prepared co-crystals of carvedilol and nicotinamide in a 1:2 ratio using TSE to improve the solubility of the drug. The co-crystals were prepared by using Omicron 10P (STEER, India) Co-rotating Twin-Screw Extruder with a diameter ratio (Do/Di) of 1.71. Four heating zones in the barrel were set as 32 °C (B1), 85 °C (B2), 92 °C (B3), and 90 °C (B4) at a screw speed of 175 rpm. The obtained carvedilol co-crystals had a distinct difference in morphological characteristics compared to pure drug. The result of DSC and XRD indicated the formation of co-crystals with high purity. Co-crystals (1:2) showed approximately 15-fold improvement in solubility compared to pure carvedilol. Pure carvedilol showed a release profile of a maximum of 18.35% in 60 min whereas it was 88% for co-crystals [91].
Moradiya et al. have prepared high-quality carbamazepine−saccharin (1:1 M ratio) co-crystals by using Eurolab-16 (Thermo Fisher, Germany) Co-rotating Twin-Screw Extruder with two different screw speeds of 5 and 10 rpm. The temperature was varied between 120 and 140 °C to optimize the co-crystal quality. The single peak was obtained at 174 °C in the DSC thermogram proved the formation of high-quality co-crystal by TSE. The in vitro dissolution test resulted in a high dissolution rate of co-crystal (66% in 60 min) prepared by TSE compared to the bulk drug [92].
Gel
Gels are defined as a semi-solid system consists of either dispersion containing small inorganic particles or large organic molecules interpenetrated by a liquid [93]. Depending on the gelling agent used, gels can be prepared by titration method (Carbopol-934P), by changing temperature (cellulose derivative and Poloxamers), or by adding specific ions (sodium alginate) [94].
All of the above-mentioned methods require more than one costly equipment such as large refrigeration units, steam heating units, and de-aeration equipment to prepare it. It also consume a great deal of energy to maintain the temperature throughout the duration of the mixing [95]. Another disadvantage associated with these methods is the difficulty in the scale-up process. One of the challenging parts in scaling up the conventional gel formulation methods is to have an equal distribution of all the components in the formulation to maintain the product consistency [96].
TSE provides several advantages over conventional manufacturing methods such as the least processing time, one-step continuous manufacturing process, and the requirement of no scrappers or mixing equipment as all mixing is performed by the screw elements of the TSE (Fig. 10) [97].
Pawar et al. have developed and evaluated a Kolliphor® P407– and Kollisolv® PEG400–based transdermal gel formulation of diclofenac sodium by using TSE. Diclofenac sodium was dissolved in sufficient amount of Kollisolv® PEG400 and Milli-Q water. To this solution, about 1% of propylene glycol was added, and the final volume was adjusted with an equivalent amount of Milli-Q water. On the other hand, Kolliphor® P407, menthol (as a counterirritant), and citric acid (as a chelating agent) were passed through a #30 sieve and mixed using a sigma cone blender. Kolliphor® P407–containing phase was fed into 11 mm Process-11 (Thermo Fisher Scientific) Co-rotating Twin-Screw Extruder by using a volumetric feeder at a rate of 2 g/min. The phase-containing drug was introduced from zone 4 at a feed rate of 4 mL/min while the temperature was set at 100 °C. The optimized gel formulation made a homogeneous and transparent film when applied on a glass slide. The prepared gel had a pH of 7.02 and uniform drug content of 100.04 ± 2.74%. The DSC and XRD analyses of the gel formulation prepared by TSE had the complete melting of the crystalline drug into an amorphous form. The result of the texture analysis study proved that the Kolliphor® P407 and Kollisolv® PEG400 formed excellent gel with consistent viscoelastic properties. Gel prepared by TSE displayed significant improvement in drug release—nearly 100% release at the end of 12 h. The flux value of the gel prepared by TSE was 106, compared to the flux value of 60 that the marketed formulation had, inferring a significant difference (P < 0.05) at the end of 1 h [98].
Mendonsa et al. have developed poloxamer (30% and 40%) gels of model drug ketoprofen by using TSE. The first mixing zone consisted of 60° elements and was situated at zone 3 to break down the agglomerates of the physical blend. The second mixing zone consisted of 90° elements and was situated at zone 6 to ensure that water and the binary mixture were uniformly mixed. The temperature was set around 97 °C to ensure that the drug and polymer were completely melted. The absence of a drug peak in the DSC thermogram for the prepared formulations indicated that the crystalline drug was either converted to an amorphous form or was present in the soluble form in the polymer matrix. The low shear value obtained as the result of the rheological study indicated that the viscosity of the products was high. The result of ex vivo permeability study in porcine epidermis indicated that the amount of drug permeated from the extruded gel was 4.082 ± 1.1 μg/cm2 from 30% poloxamer gels whereas from the control gel it was 3.979 ± 1.2 μg/cm2 [99].
SMEDDS
The liquid form of self-microemulsifying drug delivery system (SMEDDS) is usually filled with soft gelatin capsules which are very expensive. In addition, liquid SMEDDS (L-SMEDDS) has the possibility of getting leached out of the capsules or drug precipitation [100]. In light of the above-mentioned facts, the conversion of L-SMEDDS to solid SMEDDS (S-SMEDDS) can be a more suitable approach as it offers various advantages such as reducing production costs, improved stability, better patient compliance, and improvements in dosing accuracy [101]. S-SMEDDS are conventionally prepared by incorporating L-SMEDDS into powders using different techniques, such as adsorption on solid carriers, wet granulation by high-shear mixer, spray drying, extrusion spheronization, and melt granulation method [102]. Compared to all of these methods, TSE offers additional advantages such as easy to scale up, being a solvent-free method, and less processing time (Fig. 11) [103].
Silva et al. have developed S-SMEDDS and evaluated the effects of the process and formulation variables on S-SMEDDS properties. First, L-SMEDDS were developed for the model drug—carvedilol and the solid extrudates were prepared by extruding the lipid mixture and HPMCAS through a twin-screw extruder. The optimized L-SMEDDS formulation containing 20% (w/w) of the total mass of the solid formulation was accurately weighed and mixed with carvedilol to homogenize for 2 min. Next, colloidal silicon dioxide (2%, w/w), MCC (30 to 33%, w/w), HPMCAS/HPC (41%, 8:1 ratio, w/w), and talc (2%) were sequentially added to the mixture and again mixed. The resulting mixture (7.5 g) was then fed into 16-mm EHM 5 (Labmaq do Brasil Ltd.,) a lab-scale vertical (L/D = 16) twin-screw extruder using a manual feed hopper. The extruded material was collected, cooled to room temperature, and manually cut into small pieces (1000–2000 μm). S-SMEDDS diffractograms displayed no peaks related to crystalline carvedilol; % carvedilol released in the HCl medium at 120 min was in the range of 12.97 ± 0.52 to 25.54 ± 0.77%, and all the S-SMEDDS structures remained intact after the dissolution period of 120 min. In pH 6.8 dissolution medium, % carvedilol released ranged between 43.62 ± 1.31 to 85.54 ± 1.79% after 300 min. The mean globule size and PDI values of the reconstituted microemulsions ranged between 145.63 ± 2.00 and 164.72 ± 2.29 nm and from 0.209 ± 0.006 to 0.262 ± 0.004, respectively, after 300 min [104].
Solid Lipid Nanoparticles
The conventionally used methods for preparing the solid lipid nanoparticle (SLNs) are solvent diffusion method, emulsification, and solvent evaporation followed by size reduction using high-pressure homogenization or ultra-sonication [105]. All these methods are a batch process that required careful monitoring of each processing step to prevent batch to batch variations in the final product. Comparing all of these conventional methods, the preparation of solid lipid nanoparticles by twin-screw extruder offers several extra advantages such as rapid processing time, elimination of environmentally harmful solvents used in conventional methods, and continuous production (Fig. 12) [106].
Bagde et al. have prepared topical SLNs of IBU using TSE and evaluated in vitro and in vivo characteristics. The lipid and IBU were triturated in a mortar to have a uniform mixture. On the other hand, the surfactant was added into the water and the solution was continuously stirred at 70 °C. The lipid–drug mixture was fed into the feeder in the Omicron 10P Co-rotating Twin-Screw Extruder. The aqueous solution of the surfactant was injected into the mixing zone of the extruder barrel. The barrel temperature for all the zones was maintained at 110 °C. The formulation was first processed at 50 rpm screw speed once and subsequently reprocessed at 800 rpm. The emulsion with reduced size was cooled at room temperature to obtain SLNs. The prepared SLNs were entrapped in Carbopol 934 gel by using the titration method. The drug release study, skin deposition study, and in vivo anti-inflammatory activity studies exhibited 84.37 ± 4.65% drug release, 12.05 ± 0.81% drug deposition, and 40.17 ± 2.41% edema inhibition, respectively, for the SLN entrapped gel which was significantly higher (P < 0.05) than the controlled gel [107].
Patil et al. have demonstrated continuous production of SLNs by combining two processes: melt emulsification and high-pressure homogenization (HPH) for size reduction. Fenofibrate SLNs were prepared by mixing a lipid (Compritol® 888 ATO/Precirol® ATO 5) and an aqueous phase containing surfactant (Cremophor EL/Pluronic® F-68) inside the 11-mm Process 11 (Thermo Fisher Scientific) Co-rotating Twin-Screw Extruder at temperatures 10–15 °C above than the melting point of the lipid. The barrel temperature for zone 2 was maintained at either 150 or 120 °C and the rest of the zones including the die temperature were kept at 90 °C. Screw speed for all the formulations was either 160 or 240 rpm. The hot pre-emulsion resulted from hot-melt extrusion passing through an insulated tube connecting to HPH and was homogenized twice at 85 °C and 1000 bar pressure to reduce the particle size of pre-emulsion. The developed novel platform demonstrated better process control and size-reduction compared to the conventional process of hot homogenization (batch process). The dissolution profile of the fenofibrate SLNs prepared by the TSE and HPH was faster than that of the crude fenofibrate and a micronized marketed fenofibrate formulation. At the end of a 5-h in vitro dissolution study, SLN formulation released 92–93% of the drug, whereas drug release was approximately 65 and 45% for the marketed micronized formulation and crude drug, respectively. The results of the pharmacokinetic study demonstrated a statistically significant improvement in Cmax, Tmax, and AUC0–24 h from SLN formulations compared to the crude drug and marketed micronized formulation [108]
Salt Formation
The most widely used method in the pharmaceutical industry for enhancing the dissolution profile of a poorly soluble substance is the salt formation of acidic and basic drugs but the processing of salts on a very large scale still remains a complex process [109]. In majority of cases, very large volumes of organic solvents and high temperatures are required to dissolve drugs and salt-forming agents to prepare salt of poorly soluble drugs. One of the major limitations of currently used method used in industry for preparing pharmaceutical salt is that it is still a batch process which is time consuming and tedious [110]. The preparation of salt by TSE would provide the following advantages compared to the solution crystallization method: (a) exclusion of large volumes of organic solvents required to dissolve the drug, (b) continuous production of the salt, (c) easy scale-up since a twin-screw extruder can be operated continuously and operation duration can be extended in order to increase the output, and (d) the process is compatible to Quality by Design (QbD) approach as various process analytical technologies (PAT) can be used with TSE (Fig. 13) [111].
Lee et al. have reported a solvent-free continuous method for preparing a salt of weakly basic drug haloperidone with maleic acid by using a twin-screw extruder. Extrusion of a 1:1 mixture of haloperidol and maleic acid at the extruder barrel temperature of 60 °C resulted in the formation of highly crystalline salt. Haloperidol (37.5 g, 100 mmol) and maleic acid (11.6 g, 100 mmol) were blended by using a Turbula mixer for 10 min and then fed into a 16-mm co-rotating twin-screw extruder at a mass flow rate of 0.75 g/min and 100 rpm screw speed. The salt prepared by twin-screw extruder was highly crystalline and non-hygroscopic. The haloperidol-maleic acid salt prepared by twin-screw extruder had a high solubility (4.7 mg/mL) compared to pure drug and was found to be stable for 90 days at least at 25 °C and 75% RH [112].
Abuse Deterrent Formulations
Pharmaceutical manufacturers have started to develop dosage forms that are resilient to various forms of tampering techniques—best known as abuse-deterrent formulations (ADFs) to prevent the abuse and misuse of prescription drugs. The overall goal of an ADF is to produce a product less favorable to abuse and misuse. This can be extended to the products that have the ability to prevent, discourage, or decrease the feeling of euphoria, high or rush sought after the misuse [113]. Primary approaches for making abuse-deterrent formulation are by preventing the drug from being used in other ways than as intended. The types of primary approaches found in the literature were subcategorized into four areas, as follows: (i) physical barriers; (ii) viscosity management; (iii) sorption processes; and (iv) solubility modification [114].
Maddineni et al. have prepared abuse-deterrent pellets of model drug lidocaine hydrochloride by using a twin-screw extruder. PolyOx® WSR301, Benecel® K15M, and Carbopol 71G were used as polymers and 10% (w/w) vitamin E succinate as a processing aid to prepare tamper-resistant melt-extruded pellets. The blends of polymers were extruded in 16 mm Prism EuroLab (Thermo Fisher Scientific) a lab-scale twin-screw extruder with 3 mm diameter circular die with 20% (w/w) drug. The barrel temperature varied between 110 and 130 °C and screw speed were kept at 50 rpm. The obtained extrudates were cut to a length of 3 mm using a bench-top pelletizer. All formulations demonstrated sufficient hardness and elasticity and could not be reduced into fine particles (< 150 μm) by gridding which proved that the formulation cannot be snorted. In addition, all the formulations exhibited good gelling tendency in water and had minimum minimal extraction of the drug in the aqueous medium [115].
Nukala et al. have developed an egg-shaped tablet (egglet) using fused deposition modeling (FDM)—a 3D printing technology to prepare abuse-deterrent formulation for the model drug metformin hydrochloride. Drug-loaded polymeric filaments (1.5 mm) were prepared using TSE which were subsequently printed as egglets of different sizes and in-fill densities. Accurately weighed individual polymer (polyvinyl alcohol) and sorbitol were mixed in a weight ratio of 9:1. The premix was extruded using Process 11 (Thermo Fisher Scientific) 11-mm Twin-Screw Extruder with an L/D ratio of 40 at a temperature ranging between 140 and 170 °C. The extrudes were printed by MakerBot® Replicator 2 desktop single-nozzle 3D printer (MakerBot Inc., USA) with a 0.4-mm nozzle into egglets. Extreme hardness (> 500 N) and very large particle size (> 1 mm) confirmed the formulation was snorting deterrent. The ability of the formulation to release less than 15% of drugs in 5 min demonstrated the deterrence through injectable route. Quality target product profile D85 < 30 min and % Sext < 15 was achieved with egglets of 6 mm diameter, 45% infill density, and 15% w/w drug loading capacity [116].
Jedinger et al. have developed an abuse- and alcohol-resistant formulation by using TSE and film-coating technique for the drug antipyrine and codeine phosphate. Deformable pellets prepared by TSE were coated with a flexible Aquacoat® ARC film to ensure the prolonged release and to circumvent alcohol-induced dose dumping. The matrix material (cornstarch, xanthan, and gum Arabic) in powder form was placed into a ZSK 18, Coperion GmbH Co-rotating Twin-Screw Extruder with a L/D ratio of 40, screw speed of 200 rpm, and with 10 individually controllable heating sections. The model drugs (codeine phosphate hemihydrates and antipyrine) were dissolved in purified water, and the solutions were fed from the side into the extruder containing the matrix melt. All formulations were abuse deterrent: they had a high compression strength and conversion to powder by was impossible. The pellets comprising gum Arabic and xanthan as a matrix former did not remain intact and gave a very fast drug release compared to cornstarch-based pellets. The cornstarch-based pellets had a prolonged release over 8 h and were also resisted the dose dumping in 20 and 40% ethanol [117].
Table 2 summarizes various process parameters, drugs, and excipients described in examples mentioned in the manuscript.
Overall Summary and Future Prospect
Until a few years ago, the pharmaceutical industry was considered quite conservative in adopting the new manufacturing technology as it was seemed to offer a considerable challenge in maintaining product quality and thus obtaining regulatory approval. The advent of the concept of integrated continuous manufacturing practices led by the instruments such as twin-screw extruders that integrates all the unit operations in single step has enticed the pharmaceutical industry to change the traditional manufacturing methods. Ability to accelerate product development, shorten the time required for a drug molecule to reach the market, improve the cost-benefit ratio, and better control over the quality of the drug product are some of the unique advantages offered of continuous manufacturing practices that have pushed the pharmaceutical industry to explore the full potential of tools like twin-screw extruder. The steady increase in numbers of research papers and patents related to the application of twin-screw extruder that had come out from academia and industry had also given confidence to various regulatory agencies such as US-FDA, MHRA, and EMA to encourage the manufacturer to use and adopt tools such as twin-screw extruder so that decade-old manufacturing practices becomes more efficient, clean, and economical.
Twin-screw extruder has emerged as an attractive tool that can combine many unit operations in a single-line operation. The ability to exert the required shear force through the heat energy from the barrel and due to rotation of the screws has made twin-screw extruder a very efficient tool for manufacturing ranges of dosage forms. The more recent introduction of pharmaceutical-grade twin-screw extruder where different screw designs can be arranged on the shaft according to requirement has given it a unique advantage among all other contemporary instruments/tools used in the pharmaceutical industry.
Preparation of amorphous solid dispersion using the twin-screw extruder to improve the solubility of steadily increasing poor drug molecules has emerged as a method of choice as it enables molecular level mixing between drugs and polymer without solubilizing them in any organic solvent. Melt granulation by twin-screw extruder has provided a viable, efficient, and economical alternative to conventional tablet manufacturing methods such as wet granulation and dry granulation. Successful application of twin-screw extruder in preparing advance dosages such as solid SMEDDS, lipid/polymeric particles, pharmaceutical salt, and co-crystal has proven its ability to play a multi-faceted role in the manufacturing industry.
Twin-screw extruder also supports the efforts of the pharmaceutical industry and the various regulatory agencies to shift the quality control approach from “testing the product at last stage” to “building the quality of the product at each processing step” by integrating PAT tools. Accommodation of modern process analytical tools (PAT) such as near IR spectroscopy and Raman spectroscopy on the twin-screw extruder has also made it possible to constantly analyze the quality of the product throughout the processing period. The real-time monitoring of the product throughout the process by the PAT tool has aided the pharmaceutical industry to move towards the integration QbD approach in product development and manufacturing which can generate a plethora of information regarding process efficiency and also ensures real-time control on the quality of the product.
Inherent automation, reduction of capital cost due to compact structure, highly efficient energy transmission, and ability to perform multiple operations simultaneously have made twin-screw extruder a very promising tool for the small-scale start-up as well.
The interest of researchers, academia, and industry in the twin-screw extruder is constantly growing. The constant impetus from the regulatory agencies and rising numbers of successful market formulations clearly indicates the era of twin-screw extruder has not passed but just arrived on the horizon of the pharmaceutical industry.
Conclusion
The advent of TSE in the pharmaceutical industry has started to change the basic principle and concept of manufacturing processes for the various dosage forms. Efficient, clean, compact, and environment-friendly manufacturing operations offered by TSE have enticed industry and academicians equally to develop manufacturing methods for a variety of dosage forms. The option of configuring TSE with different screw designs, depending on the requirement and nature of the dosage form has made TSE a multi-purpose instrument in real sense.
References
Bouvier J-M, Campanella OH. Extrusion processing technology: food and non-food biomaterials. New Jersey: John Wiley & Sons; 2014.
Bruin S, Van Zuilichem D, Stolp W. A review of fundamental and engineering aspects of extrusion of biopolymers in a single-screw extruder. J Food Process Eng. 1978;2(1):1–37.
Martin C. Twin screw extruders as continuous mixers for thermal processing: a technical and historical perspective. AAPS PharmSciTech. 2016;17(1):3–19.
Lawal A, Kalyon DM. Mechanisms of mixing in single and co-rotating twin screw extruders. Polym Eng Sci. 1995;35(17):1325–38.
Meijer H, Elemans P. The modeling of continuous mixers. Part I: the corotating twin-screw extruder. Polym Eng Sci. 1988;28(5):275–90.
Wilczyński K, Lewandowski A, Wilczyński KJ. Experimental study for starve-fed single screw extrusion of thermoplastics. Polym Eng Sci. 2012;52(6):1258–70.
Mollan M. Historical overview. Drugs Pharma Sci. 2003;133:1–18.
Frame N. Operational characteristics of the co-rotating twin-screw extruder. The technology of extrusion cooking. Berlin: Springer; 1994. p. 1–51.
Padmanabhan B. Understanding the extruder processing zone: the heart of a twin screw extruder. Plastic Addit Comp. 2008;10(2):30–5.
Erol M, Kalyon D. Assessment of the degree of mixedness of filled polymers: effects of processing histories in batch mixer and co-rotating and counter-rotating twin screw extruders. Int Polym Process. 2005;20(3):228–37.
Poulesquen A, Vergnes B, Cassagnau P, Michel A, Carneiro OS, Covas JA. A study of residence time distribution in co-rotating twin-screw extruders. Part II: experimental validation. Polym Eng Sci. 2003;43(12):1849–62.
Goffart D, Van Der Wal D, Klomp E, Hoogstraten H, Janssen L, Breysse L, et al. Three-dimensional flow modeling of a self-wiping corotating twin-screw extruder. Part I: the transporting section. Polym Eng Sci. 1996;36(7):901–11.
Bravo V, Hrymak A, Wright J. Numerical simulation of pressure and velocity profiles in kneading elements of a co-rotating twin screw extruder. Polym Eng Sci. 2000;40(2):525–41.
Huber GR. Twin-screw extruders. Extrud Food Appl. 2000:81–114.
Kajiwara T, Nagashima Y, Nakano Y, Funatsu K. Numerical study of twin-screw extruders by three-dimensional flow analysis—development of analysis technique and evaluation of mixing performance for full flight screws. Polym Eng Sci. 1996;36(16):2142–52.
Bhattacharya S, Choudhury GS. Twin-screw extrusion of rice flour: effect of extruder length-to-diameter ratio and barrel temperature on extrusion parameters and product characteristics. J Food Process Preserv. 1994;18(5):389–406.
Thompson M, Sun J. Wet granulation in a twin-screw extruder: implications of screw design. J Pharm Sci. 2010;99(4):2090–103.
Nakayama Y, Takemitsu H, Kajiwara T, Kimura K, Takeuchi T, Tomiyama H. Improving mixing characteristics with a pitched tip in kneading elements in twin-screw extrusion. AICHE J. 2018;64(4):1424–34.
Shearer G, Tzoganakis C. Distributive mixing profiles for co-rotating twin-screw extruders. Adv Polymer Technol. 2001;20(3):169–90.
Li H, Thompson M, O’donnell K. Understanding wet granulation in the kneading block of twin screw extruders. Chem Eng Sci. 2014;113:11–21.
Martin C, Haight B. Devolatilization via twin-screw extrusion. In: Pharmaceutical extrusion technology, vol. 325. Boca Raton: CRC Press; 2018.
Steiner R, Haight B. Extruder design. In: Pharmaceutical extrusion technology. Boca Raton: CRC Press; 2018. p. 37–52.
Chen B, Zhu L, Zhang F, Qiu Y. Process development and scale-up: twin-screw extrusion. Developing solid oral dosage forms. Amsterdam: Elsevier; 2017. p. 821–68.
Shah S, Maddineni S, Lu J, Repka MA. Melt extrusion with poorly soluble drugs. Int J Pharm. 2013;453(1):233–52.
Tiwari RV, Patil H, Repka MA. Contribution of hot-melt extrusion technology to advance drug delivery in the 21st century. Expert Opin Drug Deliv. 2016;13(3):451–64.
Stanković M, Frijlink HW, Hinrichs WL. Polymeric formulations for drug release prepared by hot melt extrusion: application and characterization. Drug Discov Today. 2015;20(7):812–23.
Jermain SV, Brough C, Williams RO III. Amorphous solid dispersions and nanocrystal technologies for poorly water-soluble drug delivery–an update. Int J Pharm. 2018;535(1–2):379–92.
Morales JO, McConville JT. Manufacture and characterization of mucoadhesive buccal films. Eur J Pharm Biopharm. 2011;77(2):187–99.
Jani R, Patel D. Hot melt extrusion: an industrially feasible approach for casting orodispersible film. Asian J Pharma Sci. 2015;10(4):292–305.
Palem CR, Kumar Battu S, Maddineni S, Gannu R, Repka MA, Yamsani MR. Oral transmucosal delivery of domperidone from immediate release films produced via hot-melt extrusion technology. Pharm Dev Technol. 2013;18(1):186–95.
Mididoddi PK, Repka MA. Characterization of hot-melt extruded drug delivery systems for onychomycosis. Eur J Pharm Biopharm. 2007;66(1):95–105.
Regev G, Patel SK, Moncla BJ, Twist J, Devlin B, Rohan LC. Novel application of hot melt extrusion for the manufacturing of vaginal films containing microbicide candidate dapivirine. AAPS PharmSciTech. 2019;20(6):239.
Repka MA, Prodduturi S, Stodghill SP. Production and characterization of hot-melt extruded films containing clotrimazole. Drug Dev Ind Pharm. 2003;29(7):757–65.
Chen M, Lu J, Deng W, Singh A, Mohammed NN, Repka MA, et al. Influence of processing parameters and formulation factors on the bioadhesive, temperature stability and drug release properties of hot-melt extruded films containing miconazole. AAPS PharmSciTech. 2014;15(3):522–9.
Jivraj M, Martini LG, Thomson CM. An overview of the different excipients useful for the direct compression of tablets. Pharma Sci Technol Today. 2000;3(2):58–63.
Gokhale R, Trivedi NR. Wet granulation in low- and high-shear mixers. In: Handbook of pharmaceutical granulation technology. Boca Raton: CRC Press; 2016. p. 199–219.
Sheth BB, Bandelin FJ, Shangraw RF. Compressed tablets. In: Pharmaceutical dosage forms: tablets, vol. 1. New York: Marcel-Dekker, Inc.; 1980. p. 109–85.
Lute SV, Dhenge RM, Salman AD. Twin screw granulation: effects of properties of primary powders. Pharmaceutics. 2018;10(2):68.
Lute SV, Dhenge RM, Salman AD. Twin screw granulation: an investigation of the effect of barrel fill level. Pharmaceutics. 2018;10(2):67.
Keleb EI, Vermeire A, Vervaet C, Remon JP. Twin screw granulation as a simple and efficient tool for continuous wet granulation. Int J Pharm. 2004;273(1):183–94. https://doi.org/10.1016/j.ijpharm.2004.01.001.
Fonteyne M, Vercruysse J, Díaz DC, Gildemyn D, Vervaet C, Remon JP, et al. Real-time assessment of critical quality attributes of a continuous granulation process. Pharm Dev Technol. 2013;18(1):85–97. https://doi.org/10.3109/10837450.2011.627869.
Keleb EI, Vermeire A, Vervaet C, Remon JP. Continuous twin screw extrusion for the wet granulation of lactose. Int J Pharm. 2002;239(1):69–80. https://doi.org/10.1016/S0378-5173(02)00052-2.
Leuenberger H. New trends in the production of pharmaceutical granules: batch versus continuous processing. Eur J Pharm Biopharm. 2001;52(3):289–96. https://doi.org/10.1016/S0939-6411(01)00199-0.
Keleb EI, Vermeire A, Vervaet C, Remon JP. Extrusion granulation and high shear granulation of different grades of lactose and highly dosed drugs: a comparative study. Drug Dev Ind Pharm. 2004;30(6):679–91. https://doi.org/10.1081/ddc-120039338.
Kumar A, Vercruysse J, Toiviainen M, Panouillot P-E, Juuti M, Vanhoorne V, et al. Mixing and transport during pharmaceutical twin-screw wet granulation: experimental analysis via chemical imaging. Eur J Pharm Biopharm. 2014;87(2):279–89. https://doi.org/10.1016/j.ejpb.2014.04.004.
Maniruzzaman M, Ross SA, Dey T, Nair A, Snowden MJ, Douroumis D. A quality by design (QbD) twin—screw extrusion wet granulation approach for processing water insoluble drugs. Int J Pharm. 2017;526(1):496–505. https://doi.org/10.1016/j.ijpharm.2017.05.020.
Meena AK, Desai D, Serajuddin ATM. Development and optimization of a wet granulation process at elevated temperature for a poorly compactible drug using twin screw extruder for continuous manufacturing. J Pharm Sci. 2017;106(2):589–600. https://doi.org/10.1016/j.xphs.2016.10.020.
Schæfer T, Mathiesen C. Melt pelletization in a high shear mixer. VIII. Effects of binder viscosity. Int J Pharm. 1996;139(1–2):125–38.
Schæfer T, Mathiesen C. Melt pelletization in a high shear mixer. VII. Effects of product temperature. Int J Pharm. 1996;134(1–2):105–17.
Van Melkebeke B, Vermeulen B, Vervaet C, Remon JP. Melt granulation using a twin-screw extruder: a case study. Int J Pharm. 2006;326(1–2):89–93.
Thiam Tan DC, Lim Chin WW, Tan EH, Hong S, Gu W, Gokhale R. Effect of binders on the release rates of direct molded verapamil tablets using twin-screw extruder in melt granulation. Int J Pharm. 2014;463(1):89–97. https://doi.org/10.1016/j.ijpharm.2013.12.053.
Keen JM, Foley CJ, Hughey JR, Bennett RC, Jannin V, Rosiaux Y, et al. Continuous twin screw melt granulation of glyceryl behenate: development of controlled release tramadol hydrochloride tablets for improved safety. Int J Pharm. 2015;487(1):72–80. https://doi.org/10.1016/j.ijpharm.2015.03.058.
Batra A, Desai D, Serajuddin AT. Investigating the use of polymeric binders in twin screw melt granulation process for improving compactibility of drugs. J Pharm Sci. 2017;106(1):140–50.
Douroumis D. Practical approaches of taste masking technologies in oral solid forms. Expert Opin Drug Deliv. 2007;4(4):417–26.
Ayenew Z, Puri V, Kumar L, Bansal AK. Trends in pharmaceutical taste masking technologies: a patent review. Rec Patent Drug Deliv Formul. 2009;3(1):26–39.
Maniruzzaman M, Boateng JS, Chowdhry BZ, Snowden MJ, Douroumis D. A review on the taste masking of bitter APIs: hot-melt extrusion (HME) evaluation. Drug Dev Ind Pharm. 2014;40(2):145–56.
Maniruzzaman M, Boateng JS, Snowden MJ, Douroumis D. A review of hot-melt extrusion: process technology to pharmaceutical products. ISRN Pharma. 2012;2012:1–9.
Alshehri SM, Park J-B, Alsulays BB, Tiwari RV, Almutairy B, Alshetaili AS, et al. Mefenamic acid taste-masked oral disintegrating tablets with enhanced solubility via molecular interaction produced by hot melt extrusion technology. J Drug Deliv Sci Technol. 2015;27:18–27.
Pimparade MB, Morott JT, Park J-B, Kulkarni VI, Majumdar S, Murthy S, et al. Development of taste masked caffeine citrate formulations utilizing hot melt extrusion technology and in vitro–in vivo evaluations. Int J Pharm. 2015;487(1–2):167–76.
Juluri A, Popescu C, Zhou L, Murthy RN, Gowda VK, Kumar C, et al. Taste masking of griseofulvin and caffeine anhydrous using Kleptose Linecaps DE17 by hot melt extrusion. AAPS PharmSciTech. 2016;17(1):99–105.
Wen H, Park K. Oral controlled release formulation design and drug delivery: theory to practice. New Jersey: John Wiley & Sons; 2011.
Claeys B, Vervaeck A, Hillewaere XK, Possemiers S, Hansen L, De Beer T, et al. Thermoplastic polyurethanes for the manufacturing of highly dosed oral sustained release matrices via hot melt extrusion and injection molding. Eur J Pharm Biopharm. 2015;90:44–52.
Verstraete G, Van Renterghem J, Van Bockstal P-J, Kasmi S, De Geest B, De Beer T, et al. Hydrophilic thermoplastic polyurethanes for the manufacturing of highly dosed oral sustained release matrices via hot melt extrusion and injection molding. Int J Pharm. 2016;506(1–2):214–21.
Dumpa NR, Sarabu S, Bandari S, Zhang F, Repka MA. Chronotherapeutic drug delivery of ketoprofen and ibuprofen for improved treatment of early morning stiffness in arthritis using hot-melt extrusion technology. AAPS PharmSciTech. 2018;19(6):2700–9.
Almeida A, Possemiers S, Boone M, De Beer T, Quinten T, Van Hoorebeke L, et al. Ethylene vinyl acetate as matrix for oral sustained release dosage forms produced via hot-melt extrusion. Eur J Pharm Biopharm. 2011;77(2):297–305.
Tiwari R, Agarwal SK, Murthy R, Tiwari S. Formulation and evaluation of sustained release extrudes prepared via novel hot melt extrusion technique. J Pharm Innov. 2014;9(3):246–58.
Yang Y, Shen L, Li J, Shan W-G. Preparation and evaluation of metoprolol tartrate sustained-release pellets using hot melt extrusion combined with hot melt coating. Drug Dev Ind Pharm. 2017;43(6):939–46.
Vithani K, Cuppok Y, Mostafa S, Slipper I, Snowden M, Douroumis D. Diclofenac sodium sustained release hot melt extruded lipid matrices. Pharm Dev Technol. 2014;19(5):531–8.
Ma D, Djemai A, Gendron CM, Xi H, Smith M, Kogan J, et al. Development of a HPMC-based controlled release formulation with hot melt extrusion (HME). Drug Dev Ind Pharm. 2013;39(7):1070–83.
Vasanthavada M, Wang Y, Haefele T, Lakshman JP, Mone M, Tong W, et al. Application of melt granulation technology using twin-screw extruder in development of high-dose modified-release tablet formulation. J Pharm Sci. 2011;100(5):1923–34.
Patil H, Tiwari RV, Upadhye SB, Vladyka RS, Repka MA. Formulation and development of pH-independent/dependent sustained release matrix tablets of ondansetron HCl by a continuous twin-screw melt granulation process. Int J Pharm. 2015;496(1):33–41. https://doi.org/10.1016/j.ijpharm.2015.04.009.
Chiou WL, Riegelman S. Pharmaceutical applications of solid dispersion systems. J Pharm Sci. 1971;60(9):1281–302.
Shi X, Fan N, Zhang G, Sun J, He Z, Li J. Quercetin amorphous solid dispersions prepared by hot melt extrusion with enhanced solubility and intestinal absorption. Pharm Dev Technol. 2020;25(4):472–81. https://doi.org/10.1080/10837450.2019.1709502.
Meng F, Gala U, Chauhan H. Classification of solid dispersions: correlation to (i) stability and solubility (ii) preparation and characterization techniques. Drug Dev Ind Pharm. 2015;41(9):1401–15.
Zhang P, Shadambikar G, Almutairi M, Bandari S, Repka MA. Approaches for developing acyclovir gastro-retentive formulations using hot melt extrusion technology. J Drug Deliv Sci Technol. 2020;60:102002. https://doi.org/10.1016/j.jddst.2020.102002.
Muvva A, Lakshman D, Dwibhashyam VSNM, Dengale S, Lewis SA. In vitro-in silico evaluation of Apremilast solid dispersions prepared via corotating twin screw extruder. J Drug Deliv Sci Technol. 2020;59:101844. https://doi.org/10.1016/j.jddst.2020.101844.
Leuner C, Dressman J. Improving drug solubility for oral delivery using solid dispersions. Eur J Pharm Biopharm. 2000;50(1):47–60.
Serajuddin AT. Solid dispersion of poorly water-soluble drugs: early promises, subsequent problems, and recent breakthroughs. J Pharm Sci. 1999;88(10):1058–66.
Zi P, Zhang C, Ju C, Su Z, Bao Y, Gao J, et al. Solubility and bioavailability enhancement study of lopinavir solid dispersion matrixed with a polymeric surfactant-Soluplus. Eur J Pharm Sci. 2019;134:233–45.
He H, Yang R, Tang X. In vitro and in vivo evaluation of fenofibrate solid dispersion prepared by hot-melt extrusion. Drug Dev Ind Pharm. 2010;36(6):681–7.
Jijun F, Lishuang X, Xiaoli W, Shu Z, Xiaoguang T, Xingna Z, et al. Nimodipine (NM) tablets with high dissolution containing NM solid dispersions prepared by hot-melt extrusion. Drug Dev Ind Pharm. 2011;37(8):934–44.
McFall H, Sarabu S, Shankar V, Bandari S, Murthy SN, Kolter K, et al. Formulation of aripiprazole-loaded pH-modulated solid dispersions via hot-melt extrusion technology: in vitro and in vivo studies. Int J Pharm. 2019;554:302–11.
Kate L, Gokarna V, Borhade V, Prabhu P, Deshpande V, Pathak S, et al. Bioavailability enhancement of atovaquone using hot melt extrusion technology. Eur J Pharm Sci. 2016;86:103–14. https://doi.org/10.1016/j.ejps.2016.03.005.
Zheng X, Yang R, Zhang Y, Wang Z, Tang X, Zheng L. Part II: bioavailability in beagle dogs of nimodipine solid dispersions prepared by hot-melt extrusion. Drug Dev Ind Pharm. 2007;33(7):783–9.
Fule R, Dhamecha D, Maniruzzaman M, Khale A, Amin P. Development of hot melt co-formulated antimalarial solid dispersion system in fixed dose form (ARLUMELT): evaluating amorphous state and in vivo performance. Int J Pharm. 2015;496(1):137–56. https://doi.org/10.1016/j.ijpharm.2015.09.069.
Steed JW. The role of co-crystals in pharmaceutical design. Trends Pharmacol Sci. 2013;34(3):185–93. https://doi.org/10.1016/j.tips.2012.12.003.
Douroumis D, Ross SA, Nokhodchi A. Advanced methodologies for cocrystal synthesis. Adv Drug Deliv Rev. 2017;117:178–95.
Shaikh R, Walker GM, Croker DM. Continuous, simultaneous cocrystallization and formulation of theophylline and 4-aminobenzoic acid pharmaceutical cocrystals using twin screw melt granulation. Eur J Pharm Sci. 2019;137:104981.
Moradiya HG, Islam MT, Halsey S, Maniruzzaman M, Chowdhry BZ, Snowden MJ, et al. Continuous cocrystallisation of carbamazepine and trans-cinnamic acid via melt extrusion processing. CrystEngComm. 2014;16(17):3573–83.
Daurio D, Nagapudi K, Li L, Quan P, Nunez F-A. Application of twin screw extrusion to the manufacture of cocrystals: scale-up of AMG 517–sorbic acid cocrystal production. Faraday Discuss. 2014;170:235–49.
Fernandes GJ, Rathnanand M, Kulkarni V. Mechanochemical synthesis of carvedilol cocrystals utilizing hot melt extrusion technology. J Pharm Innov. 2019;14(4):373–81. https://doi.org/10.1007/s12247-018-9360-y.
Moradiya H, Islam MT, Woollam GR, Slipper IJ, Halsey S, Snowden MJ, et al. Continuous cocrystallization for dissolution rate optimization of a poorly water-soluble drug. Cryst Growth Des. 2014;14(1):189–98. https://doi.org/10.1021/cg401375a.
Lu Z, Fassihi R. Influence of colloidal silicon dioxide on gel strength, robustness, and adhesive properties of diclofenac gel formulation for topical application. AAPS PharmSciTech. 2015;16(3):636–44.
Akhtar MF, Hanif M, Ranjha NM. Methods of synthesis of hydrogels… a review. Saudi Pharma J. 2016;24(5):554–9.
Chang R-K, Raw A, Lionberger R, Yu L. Generic development of topical dermatologic products: formulation development, process development, and testing of topical dermatologic products. AAPS J. 2013;15(1):41–52.
Garg S, Goldman D, Krumme M, Rohan LC, Smoot S, Friend DR. Advances in development, scale-up and manufacturing of microbicide gels, films, and tablets. Antivir Res. 2010;88:S19–29.
Bhagurkar AM, Angamuthu M, Patil H, Tiwari RV, Maurya A, Hashemnejad SM, et al. Development of an ointment formulation using hot-melt extrusion technology. AAPS PharmSciTech. 2016;17(1):158–66.
Pawar J, Narkhede R, Amin P, Tawde V. Design and evaluation of topical diclofenac sodium gel using hot melt extrusion technology as a continuous manufacturing process with Kolliphor® P407. AAPS PharmSciTech. 2017;18(6):2303–15.
Mendonsa NS, Murthy SN, Hashemnejad SM, Kundu S, Zhang F, Repka MA. Development of poloxamer gel formulations via hot-melt extrusion technology. Int J Pharm. 2018;537(1–2):122–31.
Singh B, Beg S, Khurana RK, Sandhu PS, Kaur R, Katare OP. Recent advances in self-emulsifying drug delivery systems (SEDDS). Crit Rev Ther Drug Carrier Syst. 2014;31(2):121–85.
Tang B, Cheng G, Gu J-C, Xu C-H. Development of solid self-emulsifying drug delivery systems: preparation techniques and dosage forms. Drug Discov Today. 2008;13(13–14):606–12.
Dokania S, Joshi AK. Self-microemulsifying drug delivery system (SMEDDS)–challenges and road ahead. Drug Deliv. 2015;22(6):675–90.
Crowley MM, Zhang F, Repka MA, Thumma S, Upadhye SB, Kumar Battu S, et al. Pharmaceutical applications of hot-melt extrusion: part I. Drug Dev Ind Pharm. 2007;33(9):909–26.
Silva LAD, Almeida SL, Alonso EC, Rocha PB, Martins FT, Freitas LA, et al. Preparation of a solid self-microemulsifying drug delivery system by hot-melt extrusion. Int J Pharm. 2018;541(1–2):1–10.
Müller RH, MaÈder K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery–a review of the state of the art. Eur J Pharm Biopharm. 2000;50(1):161–77.
Breitenbach J. Melt extrusion: from process to drug delivery technology. Eur J Pharm Biopharm. 2002;54(2):107–17.
Bagde A, Patel K, Kutlehria S, Chowdhury N, Singh M. Formulation of topical ibuprofen solid lipid nanoparticle (SLN) gel using hot melt extrusion technique (HME) and determining its anti-inflammatory strength. Drug Deliv Translat Res. 2019;9(4):816–27.
Patil H, Feng X, Ye X, Majumdar S, Repka MA. Continuous production of fenofibrate solid lipid nanoparticles by hot-melt extrusion technology: a systematic study based on a quality by design approach. AAPS J. 2015;17(1):194–205.
Berge SM, Bighley LD, Monkhouse DC. Pharmaceutical salts. J Pharm Sci. 1977;66(1):1–19.
Wermuth CG, Stahl PH. Selected procedures for the preparation of pharmaceutically acceptable salts. In: Handbook of pharmaceutical salts: properties, selection, and use; 2002. p. 249–63.
Daurio D, Medina C, Saw R, Nagapudi K, Alvarez-Núñez F. Application of twin screw extrusion in the manufacture of cocrystals, part I: four case studies. Pharmaceutics. 2011;3(3):582–600.
Lee HL, Vasoya JM, MDL C, Yeh KL, Lee T, Serajuddin AT. Continuous preparation of 1: 1 haloperidol–maleic acid salt by a novel solvent-free method using a twin screw melt extruder. Mol Pharm. 2017;14(4):1278–91.
Mastropietro DJ, Omidian H. Current approaches in tamper-resistant and abuse-deterrent formulations. Drug Dev Ind Pharm. 2013;39(5):611–24. https://doi.org/10.3109/03639045.2012.680468.
Mastropietro DJ, Omidian H. Abuse-deterrent formulations: part 1 – development of a formulation-based classification system. Expert Opin Drug Metab Toxicol. 2015;11(2):193–204. https://doi.org/10.1517/17425255.2015.979786.
Maddineni S, Battu SK, Morott J, Soumyajit M, Repka MA. Formulation optimization of hot-melt extruded abuse deterrent pellet dosage form utilizing design of experiments. J Pharm Pharmacol. 2014;66(2):309–22.
Nukala PK, Palekar S, Patki M, Patel K. Abuse deterrent immediate release egg-shaped tablet (egglets) using 3D printing technology: quality by design to optimize drug release and extraction. AAPS PharmSciTech. 2019;20(2):80.
Jedinger N, Schrank S, Fischer JM, Breinhälter K, Khinast J, Roblegg E. Development of an abuse-and alcohol-resistant formulation based on hot-melt extrusion and film coating. AAPS PharmSciTech. 2016;17(1):68–77.
Acknowledgments
The authors are sincerely thankful to Dr. Vijay Kulkarni, DGM, Business Development and Collaborations, STEERLife India Pvt. Ltd. and Mr. Amit Singh, Deputy Manager, Business Development and Sales Pharmaceutical—STEERLife India Pvt. Ltd. for their constant support, encouragement, and materials they have provided throughout the writing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Clearance
The authors declare that no animal or human was used during the course of the review article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dhaval, M., Sharma, S., Dudhat, K. et al. Twin-Screw Extruder in Pharmaceutical Industry: History, Working Principle, Applications, and Marketed Products: an In-depth Review. J Pharm Innov 17, 294–318 (2022). https://doi.org/10.1007/s12247-020-09520-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-020-09520-7