Abstract
Purpose
To improve the solubility of carvedilol by preparing cocrystals utilizing solvent-free, continuous technology hot melt extrusion.
Methods
Cocrystals of carvedilol and nicotinamide were formed in 1:2 ratio using hot melt extrusion (HME) by altering the parameters associated with the temperature of barrels and screw speed of the shaft. The product was characterized by DSC, PXRD, and FTIR, while the morphology was determined by SEM. Saturation solubility studies and dissolution rate were compared with carvedilol.
Results
The processing parameters in HME significantly affected the cocrystallization which improved on changing the temperature and screw speed (cocrystals were formed when the temperature was set above the eutectic melting point). The obtained carvedilol cocrystals showed a distinct difference in morphological characteristics as compared to pure drug. The cocrystals showed the presence of additional peaks in DSC thermograph as well as band shifts in infrared spectrum. The powder XRD of cocrystals showed the difference in the 2θ values as compared with carvedilol indicating an interaction between carvedilol and nicotinamide. The saturation solubility studies and in vitro dissolution studies showed of cocrystals showed an increase in solubility and drug release, respectively, in 0.1N HCl.
Conclusion
Hence, cocrystallization utilizing HME marks an important advantage over other conventional techniques. A single step, continuous process, scalable, and solvent-free HME process proved to be the best method to produce cocrystals on a larger scale with maximum yield. However, to further decrease the number of manufacturing steps, efforts are being made to combine crystallization and formulation in a single step.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cocrystallization is a promising approach to increase the solubility and bioavailability of active pharmaceutical ingredients, their thermodynamic stability, and a wide range of mechanical properties. Any active pharmaceutical ingredient (API) irrespective of acidic, basic, or ionizable groups could potentially be cocrystallized. Cocrystals can be defined as crystalline materials composed of two or more molecules within the same crystal lattice held together by non-covalent bonds [1,2,3].
Advantages of cocrystals [4]:
- a.
Cocrystals are highly stable in comparison with amorphous solids and anhydrous crystals since they do not get converted to crystalline hydrate at higher relative humidity (RH).
- b.
All the API molecules whether ionizable or non-ionizable can be made into cocrystals.
- c.
Coformers used can be an inactive excipient, different API, and food additives or preservative, i.e., any biologically accepted product.
- d.
Cocrystals can be produced using solid-state synthesis green technologies without any by-products or use of solvents, i.e., they are environment-friendly.
Therefore, cocrystals are convenient for improving the bioavailability, solubility, stability, and dissolution rate of the drug. Different methods to prepare cocrystals include solvent evaporation, solvent crystallization, solid state grinding, solvent drop grinding, hot melt extrusion (HME), and sonocrystallization [1, 5,6,7]. Solvent evaporation and grinding are most common techniques used for preparing cocrystals. However, these techniques are more suitable for small-scale screening operations only. HME technology can be used to produce cocrystals feasible on manufacturing scale by controlled heat and shear deformation. HME technology is a widely used processing technology in rubber, food, and plastic industries and in the year 1970, it demonstrated its application in pharma sector to manufacture medical devices, implants, and inserts and has recently been used in formulation development of various dosage forms and drug delivery systems. Due to its advantages like solvent-free process, single step, and readily scalable process, HME technology is growing steadily in pharmaceutical field [7,8,9,10].
Carvedilol belongs to biopharmaceutical classification system (BCS) class II; thus, it behaves as a low soluble and a high permeable drug, so once it is available in the form of a solution, it rapidly gets absorbed. Due to hepatic first-pass metabolism, the oral bioavailability of carvedilol is low, i.e., around 25% [11, 12]. For a formulation scientist, the major hurdle to overcome is aqueous solubility of the drug. The drug gets absorbed only if present in the form of a solution at the site of absorption. Various techniques developed to enhance the solubility of a drug include physical and chemical modification of drug for, e.g., solid dispersions, cyclodextrin inclusion complexes, micronization, hydrotropy, and utilizing nanotechnology like nanosuspensions, nanoemulsions, nanocrystals, cocrystals, and co-amorphous technology. To select an appropriate solubility enhancement method for a drug, it primarily depends on the properties of the drug, site of absorption, and required characteristics of final dosage form [13,14,15]. Hence, the main objective of this present research work was to formulate carvedilol cocrystals using nicotinamide as coformer and hot melt extrusion as the technique of cocrystallization. These cocrystals can later be formulated into an appropriate drug delivery system.
Material and Method
Materials
Carvedilol USP was gifted by Mylan Laboratories Ltd., Hyderabad, India. Nicotinamide was purchased from Suvidhinath Laboratories, Gujarat, India. Hydrochloric acid was purchased from Qualigens, Mumbai, India. All other chemicals used in the research work were of analytical grade.
Selection of Coformers
Cocrystals are basically formed by hydrogen bonding between drug and coformer. Nicotinamide can donate 1 hydrogen atom and accept a pair of hydrogen atoms, while carvedilol can accept 5 hydrogen atoms and donate 3 hydrogen atoms, therefore, having high chances of cocrystal formation. Citric acid, succinic acid, tartaric acid, and benzoic acid were tried as coformers, but DSC and FTIR results showed that only nicotinamide formed good cocrystals.
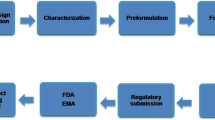
Cocrystallization in Hot Melt Extruder
Carvedilol (10 g) and nicotinamide (20 g) were taken in 1:2 ratio and blended for 15 mins using a mortar and pestle. Cocrystallization was carried out using co-rotating twin screw hot melt extruder (Omicron 10P, STEER, India) having diameter ratio (Do/Di) of 1.71. The powdered blend was fed into the extruder at a rate of 20 rpm using a gravimetric screw feeder. The four heating zones in the barrel were set at 32 °C (B1), 85 °C (B2), 92 °C (B3), and 90 °C (B4) at a screw speed of 175 rpm. The screw configurations and barrel heating zones are shown in Fig. 1. The product obtained was dried in the oven at 40 °C for 10 mins to remove any residual moisture (if present).
Evaluation of Cocrystals
Visual Morphology
The visual appearance of plain carvedilol, nicotinamide, and obtained cocrystals was studied using cannon EOS 700D [16].
Differential Scanning Calorimeter [17]
Shimadzu TA-60 WS thermal analyzer was used to obtain differential scanning calorimeter (DSC) measurements. The instrument comprises a calorimeter (DSC 60), a flow controller (FCL 60), a thermal analyzer (TA 60), and operating software TA 60 by Shimadzu Corporation, Japan. The required amount of sample (2 mg) was placed in aluminum pans and sealed with aluminum lid. The samples were placed in a sample holder and allowed to heat from 25 to 350 °C at a fixed scanning rate of 10 °C/min under a nitrogen flow of 30 ml/min. The reference used was the empty aluminum pan. The basic principle of heat flow as a function of temperature was measured for cocrystals.
Fourier Transform Infrared Spectroscopy [17]
Shimadzu FTIR-8300 system (Kyoto, Japan) was used to obtain spectra of the prepared samples. The spectrum was recorded over a range of 4000–500 cm−1. The procedure consisted of dispersing the cocrystals in KBr and then compressing into a disc with an applied pressure of 5 tons for 5 mins using a hydraulic press. The pellet formed was placed in the path of light and spectrum was obtained. Unwanted bands were discarded from the respective spectrum.
Powder X-Ray Diffraction [18]
The powder XRD pattern of optimized cocrystal, drug, and nicotinamide was collected using Rigakuminiflex 600 X-ray diffractometer (Rigaku Co., Tokyo, Japan), operated at 600 W, with a fixed tube current (15 mA) and a fixed voltage(40 kV). The X-ray-diffracted beam was monochromated by a graphite monochromator and detected by a standard scintillation counter. Diffraction intensities were measured over a range of 5–800 (2θ).
Scanning Electron Microscopy [19]
Scanning electron microscope (SEM) was used to study the morphology of cocrystals, drug, and nicotinamide. The instrument used was EVO MA18 with Oxford EDS(X-act) (Zeiss, Germany). The samples were pelletized and mounted on aluminum stub using double-sided adhesive type of gold tape. The samples were placed in a vacuum at 10 Torr to increase the conductivity of the samples. The samples were scanned by an electronic beam at an acceleration potential of 20 kV. The images obtained were collected.
Saturation Solubility Studies [20]
Equilibrium dynamic solubility of cocrystals was measured by shake flask method. 0.1N HCl was used as the solvent (as carvedilol showed maximum solubility in acidic pH). Samples were prepared by adding excess quantities of cocrystals in 2 ml of 0.1N HCl. All the samples were placed in an orbital shaker. The temperature was maintained at 37 °C and samples were shaken at 150 rpm. Samples were collected after 48 h and centrifuged at 5000 rpm for 10 min. The clear supernatant was separated, filtered, diluted, and analyzed using a UV-visible spectrophotometer.
In Vitro Dissolution Studies [16]
Cocrystals containing 100 mg equivalent of the drug was weighed and filled in a hard gelatin capsule (size 0). The in vitro dissolution studies were carried out using USP apparatus I (Basket) at 75 rpm in 900 ml of 0.1N HCl for 1 h. Five milliliters of samples were withdrawn at intervals of 5, 10, 15, 20, 30, 45, and 60 mins and replenished with the same amount of dissolution medium. Test samples were then filtered using Whatman filter paper and diluted if necessary. These samples were analyzed using UV-visible spectrophotometer.
Flow Property Evaluation [16]
Flow properties of the optimized ratio were carried out where tapped density (TD), bulk density (BD), compressibility index (CI), Hausner’s ratio (HR), and angle of repose were compared with the pure drug.
Drug Content [20]
Ten milligrams of cocrystals were weighed and dissolved in 10 ml methanol. The volume was made up using 0.1N HCl. Required dilutions were carried out using 0.1N HCl and were analyzed spectrophotometrically using a UV-visible spectrophotometer to determine the amount of carvedilol present in 10 mg of cocrystals.
Percentage Practical Yield [21]
The percentage practical yield of the prepared cocrystals was calculated to know the efficiency of the method. Cocrystals were collected and practical yield was determined using the equation
Results and Discussions
Visual Morphological Studies
Certain differences were observed in the morphological features of carvedilol cocrystals as compared with pure carvedilol and nicotinamide. Pure carvedilol appeared white odorless crystalline in nature, while nicotinamide appeared as fine and bright white powder, and cocrystals prepared appeared to be a fine white crystalline flaky powder as shown in Fig. 2. Hence, this indicates that carvedilol and nicotinamide have reacted to form a product with morphological characteristics different from drug and conformer.
DSC
Carvedilol, nicotinamide, and cocrystals were subjected to thermal screening by DSC. Carvedilol exhibited a single endothermic peak at 117 °C, and nicotinamide also yielded a sharp endothermic peak at 134 °C. The cocrystals showed an endothermic peak at 100.93 °C and an additional melting endotherm at 126.60 °C as shown in Figs. 3 and 4. The first peak (minor) may be due to eutectic temperature of the mixture, while the second peak indicates the melting point of cocrystals as the shift in melting point was observed as compared to pure drug and coformer indicating the formation of a new compound. However, the intensity has decreased which may be due to partial amorphization.
FTIR
In carvedilol, spectra absorption peaks were observed at 3344.57 cm−1, 2926.01 cm−1, 1597.06 cm−1, and 1253.73 cm−1 that correspond to N–H and O–H stretching vibration peak merged, C–H stretching vibration, N–H bending vibration, and O–H bending and C–O stretching vibrations. The IR spectrum for nicotinamide shows the characteristic peak at 3363.86 cm−1, 3159.40 cm−1, and 1685.79 cm−1 due to N–H stretch, O–H stretch, and C=O stretching vibration peaks. From the spectral study, it was observed that the characteristic band for N–H at 3344.57 cm−1 was shifted to 3350.35 cm−1 with broadening and decrease in intensity. Carvedilol drug spectrum as a band at 1597 cm−1 and 2843.07 cm−1 was found absent in spectrum of cocrystal. The shift in peaks with a decrease in intensity and absence of some peaks suggests the possibility of cocrystal formation (Figs. 5 and 6).
XRD
Powder XRD patterns of carvedilol, nicotinamide, and optimized carvedilol nicotinamide cocrystals 1:2 are shown in Figs. 7 and 8. The details of diffraction peaks are shown in Table 1. The cocrystals prepared showed sharp diffraction patterns that confirmed their crystalline nature. The difference in the 2θ values of carvedilol and cocrystal indicates an interaction between carvedilol and nicotinamide. The cocrystals exhibited powder XRD patterns with different peak position as compared to carvedilol with reduced peaks and intensity. Hence, from the above results, it can be said that cocrystals possessed different internal structure compared to pure carvedilol, i.e., some interaction has taken place.
SEM
The SEM images of carvedilol, nicotinamide, and optimized cocrystals are shown in Figs. 9 and 10. The SEM analyses revealed the differences of crystal habit in cocrystal as compared with the drug. Carvedilol exhibited irregular shape with a smooth surface, while cocrystals exhibited slight needle-shape crystals.
Saturation Solubility Studies
The solubility of pure carvedilol in 0.1N HCl (pH 1.2) at 37 °C was found to be 0.093 mg/ml after 48 h. Whereas, carvedilol nicotinamide cocrystals prepared by HME showed dynamic solubility of 1.41 mg/ml in 0.1N HCl after 48 h as shown in Fig. 11. Cocrystals (1:2) showed approximately 15-fold increase in solubility as compared to pure carvedilol. The 15-fold increase in solubility may be due to several reasons like cocrystals formation or due to the additive effect of carvedilol and nicotinamide since both have nitrogen in their parent ring that can get protonated at an acidic pH.
In Vitro Drug Release
The in vitro drug release studies demonstrated a 4.79-fold increase in solubility for the prepared cocrystals as compared to pure carvedilol as shown in Fig. 12 and Table 2. Pure carvedilol showed release profile maximum of 18.35% in 60 mins. The percent drug release at end of 60 mins for cocrystals was 88% in 60 mins. The increase in drug release may be due to the formation of hydrogen bonding between amide functional group and a carboxyl group of nicotinamide. Due to nicotinamide in association with carvedilol, it increases the polarity of hydrophobic carvedilol thus increasing its solubility.
Flow Property Evaluation Studies
On the basis of the data shown in Table 3, cocrystals considerably improved the flow properties from very poor to good in comparison with the pure drug.
Drug Content
The amount of drug present in cocrystals was found to be 99.09%.
Percent Practical Yield
The percentage practical yield of HME technology for preparation of cocrystals of carvedilol using nicotinamide as coformer was found to be 86.26%. The high percentage yield of HME technology can have benefits in producing cocrystals on manufacturing scale.
Discussion
Pharmaceutical cocrystals offer a way to improve solubility of BCS class II drugs without a change in their thermodynamic stability of the crystalline form of the drug. Pharmaceutical cocrystals are being developed with an increase in the number of patents; however, there are few marketed examples of products involving cocrystals due to several drawbacks (time consumption, residual solvent) related to conventional synthesis of cocrystals. An advanced technique like hot melt extrusion has been used to overcome its drawbacks and also suggests the possibility to combine the synthesis and formulation in order to reduce the steps in the manufacturing of the drug product.
In this work, we considered that carvedilol and nicotinamide would form cocrystals in a given stoichiometric ratio. This formation could be due to major interaction of amide group in nicotinamide and nitrogen in pyridine ring of carvedilol. The processing parameters in HME, i.e., temperature, screw speed, and feeding rate, have significant effect on the output of cocrystals. It was necessary to maintain a specific set of temperatures in three different zones (B1 is always set to 30 °C; hence, only the temperature of the three zones, i.e., B2, B3, and B4, are changed). It was seen in DSC that setting the temperature above the eutectic melting point is a requirement for the formation of cocrystals. However, when the temperature was set above the eutectic melting point, the product obtained had begun to melt with change in color (ash colored). Therefore, it was necessary to subsequently increase the screw speed to form cocrystals. As temperature was set to 85 °C, 92 °C, and 90 °C at 175 rpm, the product was formed with good crystalline appearance. Once the temperature was set, the screw speed was altered to decrease the residence time. At screw speed of 100 rpm, the product obtained was sticky in nature and, on drying, formed very large and hard crystals. As the revolutions per minute was set to 175, good crystalline with uniform size was obtained. The ratio of drug and coformer and its physicochemical properties plays a major role in formation of cocrystals. Initially, the ratio of 1:6 of drug and coformer, respectively, was taken and cocrystals formed using HME at a lower temperature (60 °C, 65 °C, and 65 °C at 75 rpm). However, this ratio had very low amount of drug thus increasing the dose size when formulated into suitable drug delivery system. Hence, various ratios of drug and coformer were selected, i.e., 1:1, 1:2, 2:1, 1:3, and 3:1. From the above ratios, 1:2 ratio showed highest solubility and dissolution rate. The cocrystals of carvedilol nicotinamide (1:2) produced via HME showed a high practical yield, thereby indicating a good technique for scale up.
Conclusion
The work demonstrated that forming cocrystals of carvedilol with nicotinamide utilizing a viable HME process, the simultaneous enhancement in solubility, dissolution rate, and improved flow properties of carvedilol could be achieved. Many techniques have been used to improve the solubility of carvedilol like micronization, nanoformulation (dendrimers, nanocrystals, polymeric nanoparticles), solid dispersions, and inclusion complexes; however, all these techniques suffer from one major drawback, i.e., industrial applicability. This study focusses on preparing carvedilol cocrystal with improved characteristics and further demonstrates that the use of cocrystals prepared by HME can be a feasible and valuable approach to deliver neutral compounds with low solubility. However, to further decrease the number of manufacturing steps, efforts are being made to combine crystallization and formulation in HME.
References
Sanjay AN, Manohar SD, Bhanudas SR. Pharmaceutical cocrystallization: a review. J Adv Pharma Educ Res. 2014;4(4).
Patole T, Deshpande A. Co-crystallization-a technique for solubility enhancement. Int J Pharm Sci Res. 2014;5(9):3566.
Jampílek J, Dohnal J. Investigation of carbohydrates and their derivatives as crystallization modifiers. In Carbohydrates-comprehensive studies on glycobiology and glycotechnology 2012. InTech.
Yadav AV, Shete AS, Dabke AP, Kulkarni PV, Sakhare SS. Co-crystals: a novel approach to modify physicochemical properties of active pharmaceutical ingredients. Indian J Pharm Sci. 2009;71(4):359–70.
Kotak U, Prajapati V, Solanki H, Jani G, Jha P. Co-crystallization technique its rationale and recent progress. World J Pharm Pharm Sci. 2015;4(4):1484–508.
Yamamoto K, Tsutsumi S, Ikeda Y. Establishment of cocrystal cocktail grinding method for rational screening of pharmaceutical cocrystals. Int J Pharm. 2012;437(1):162–71.
Li S, Yu T, Tian Y, McCoy CP, Jones DS, Andrews GP. Mechanochemical synthesis of pharmaceutical cocrystal suspensions via hot melt extrusion: feasibility studies and physicochemical characterization. Mol Pharm. 2016;13(9):3054–68.
Jagtap PS, Jain SS, Dand N, Jadhav KR, Kadam VJ. Hot melt extrusion technology, approach of solubility enhancement: a brief review. Der Pharm Lett. 2012;4:42e53.
Patil H, Tiwari RV, Repka MA. Hot-melt extrusion: from theory to application in pharmaceutical formulation. AAPS PharmSciTech. 2016;17(1):20–42.
Hot Melt Extrusion - Drug Manufacturing | Twin Screw Extruders [Internet]. Particlesciences.com. 2018 [cited 19 February 2018]. Available from: http://www.particlesciences.com/news/technical-briefs/2011/hot-melt-extrusion.html.
Kalimuthu S, Yadav AV. Formulation and evaluation of carvedilol loaded Eudragit E100 nanoparticles. Int J PharmTech Res. 2009;1:179–83.
Jamakandi VG. Formulation and evaluation of immediate release tablet of carvedilol using liquisolid compacts technique for solubility enhancement. AJP. 2016;10(03):10.
Zoghbi A, Wang B. Carvedilol solubility enhancement by inclusion complexation and solid dispersion. JDDT. 2015;5(2):1–8.
Nollenberger, T. (2017). Using polymers to enhance solubility of poorly soluble drugs. [online] Pharmtech.com. Available at: http://www.pharmtech.com/using-polymers-enhance-solubility-poorly-soluble-drugs [Accessed 25 Jul. 2017].
Fernandes GJ, Kumar L, Sharma K, Tunge R, Rathnanand M. A review on solubility enhancement of carvedilol—a BCS class II drug. J Pharmaceut Innov. 2018:1–6.
Desai H, Rao L, Amin P. Carbamazepine cocrystals by solvent evaporation technique: formulation and characterisation studies. Am J of Pharm Tech Res. 2014;2:4.
Shayanfar A, Asadpour-Zeynali K, Jouyban A. Solubility and dissolution rate of a carbamazepine–cinnamic acid cocrystal. J Mol Liq. 2013;187:171–6.
Manin A, Voronin A, Drozd K, Manin N, Bauer-Brandl A, Perlovich G. Cocrystal screening of hydroxybenzamides with benzoic acid derivatives: a comparative study of thermal and solution-based methods. Eur J Pharm Sci. 2014;65:56–64.
Sanphui P, Bolla G, Nangia A, Chernyshev V. Acemetacin cocrystals and salts: structure solution from powder X-ray data and form selection of the piperazine salt. IUCrJ. 2014;1(2):136–50.
Mounika P, Raj V, Divya G. Preparation and characterization of novel co-crystal forms of fexofenadine. IJIPR. 2015;6(1):458–63.
Chandel N, Gupta V, Pandey A, Saxena S. Co-crystalization of aceclofenac and paracetamol and their characterization. Int J Pharma Life Sci. 2011;2(8).
Acknowledgements
The authors are grateful to STEER Engineering, Bengaluru, India, for providing an opportunity to work on hot melt extruder (OMICRON 10) and Manipal College of Pharmaceutical Sciences, Manipal Academy of Higher Education for providing the facilities to carry out the research work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fernandes, G.J., Rathnanand, M. & Kulkarni, V. Mechanochemical Synthesis of Carvedilol Cocrystals Utilizing Hot Melt Extrusion Technology. J Pharm Innov 14, 373–381 (2019). https://doi.org/10.1007/s12247-018-9360-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-018-9360-y