Abstract
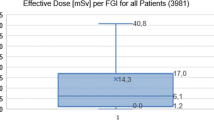
Interventional radiology is based on minimally invasive procedures that allow diagnosis and percutaneous treatment of diseases in almost all organ systems. Such procedures have many benefits, but they also contribute significantly to collective radiation dose. In this regard, effective dose (E) is a convenient quantity to estimate patients’ stochastic radiation risk. However, E cannot be accurately evaluated immediately. In the present study, we aimed to estimate the E value in 15 selected interventional procedures. The estimation was based on dose area product (DAP) measurements and used case-specific conversion coefficients. The E values ranged from 3.3 to 69.9 mSv, depending on the kind of procedure. This wide range was mainly due to the broad variation in DAP values, which in turn depend on the details of how the procedures are performed. This suggests that to ensure valid comparative studies and universal reference levels, all interventional procedures should be well classified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Interventional radiology is based on minimally invasive procedures that allow diagnosis and percutaneous treatment of diseases in almost all organ systems. Recently, it has been used with growing frequency, and increasingly complicated radiological procedures are becoming technically possible. These techniques bring immense benefits to patients, but they also represent a significant proportion of patients’ collective radiation doses from all medical exposures. In this regard, to minimize public radiation exposure, the ALARA principle (as low as reasonably achievable) is commonly applied [1,2,3,4,5].
However, when complex procedures are performed or repeated on the same patient, high-radiation dose levels can occur owing to long fluoroscopy times or requirements for high-quality images. For this reason, the evaluation of X-ray doses in patients undergoing interventional radiology is gaining interest. Moreover, the Euratom European Council Directive (2013/59) [6] emphasizes that medical exposure must be justified, suggests that doses connected to medical procedures be recorded, and advocates the use of diagnostic reference levels and dose-indicating devices.
Effective dose (E) is an estimation of health risk due to the stochastic effects of radiation exposure. However, E is usually difficult to determine accurately. Indeed, the new Recommendations of the International Commission on Radiological Protection (ICRP) [7] set severe limitations on the use of E for assessing patients’ radiation exposure. Conversely, interventional procedures deliver higher doses than standard radiological examinations. Therefore, a relatively simple parameter that measures risk of patients would be extremely useful. In this context, E could be considered a good candidate for comparing risk between different types of procedures, technologies, irradiation geometries, and radiation qualities.
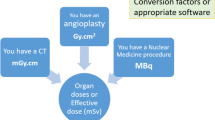
Different approaches to the determination of E have been proposed in the literature. Some authors [8,9,10,11] have used case-specific conversion coefficients to derive E from directly measurable parameters such as the dose area product (DAP) or entrance surface dose. Others have used commercial software or dosimeters to estimate absorbed doses in critical organs exposed to X-ray beams and then estimated E by applying the tissue-weighting factors published by ICRP 103 [7, 12,13,14,15]. The aim of this work was to estimate E in several interventional procedures. The estimation was based on DAP data and used conversion coefficients published in the literature [16] and properly adapted to fit the procedures under investigation.
2 Materials and methods
The interventional radiological procedures were performed at the Tor Vergata University Hospital using two Philips AlluraXperFD20/20® biplane systems (Philips Healthcare, Best, The Netherlands). Both systems were equipped with continuous and pulsed fluoroscopy (1–15 frames per second[fps]) and variable frame-digital subtraction angiography (1 or 2 fps).Two external filtration settings were available, namely 0.4 mm of copper or 0.1 mm of copper with an additional millimeter of aluminum. The half-value layer of each tube was 5.07 and 5.21 mm of aluminum at 80 kVp for 0.1 mm Cu + 1 mm Al additional filtration setting, and 7.37 and 7.31 mm of aluminum at 80 kVp for 0.4 mm Cu + 1 mm Al additional filtration setting.
The source-to-image receptor distance ranged from 90 to 120 cm. Tube voltage and current settings were controlled by an automatic exposure control (AEC).Both angiographic systems were installed with a DAP meter consisting of a transmission ionization chamber. These were calibrated according to protocols available in the literature [17,18,19,20,21,22] that consider both beam quality and patient-table attenuation. Calibrations were performed using a reference dosimeter (solid-state detector; UNFORS XI, RaySafe™, Billdal, Sweden) for dose measurements and reflective-type XR-RV3 Gafchromic® films (International Specialty Products, Wayne, USA) for field-size measurements, respectively. The calibration procedure was performed for the two filtration conditions, as was the attenuation effect due to the patient table. Two calibration curves (with and without patient-table attenuation) were produced for each system and for tube voltages ranging from 60 to 120 kVp. To create the calibration curve with patient-table attenuation, the reference dosimeter was placed on the top of the mattress and patient table, with the X-ray tube under the couch. To construct the calibration curve without patient-table attenuation, the dosimeter was placed in the air, with the X-ray tube parallel to the floor. To measure the field size, films were cut in pieces of 15×15 cm, with the white side facing the source. Three pieces were considered and individually positioned in place of the reference dosimeter and exposed to the primary X-ray beam with negligible backscatter. To do this, they were placed on a 10-cm-thick polystyrene support at 100 cm from the focal spot. We used 80kVp, 10 mAs, no filtration, and a nominal field size of 10 × 10 cm. The impressed area was then measured using a scanner (EPSON Expression 10000 XL) 2 days later. The scan parameters used were reflective mode, no color corrections, and resolution of 72 dpi. The Picodose X 8.0 PRO software (Tecnologie Avanzate, Torino, Italy) was used to extract default grayscale profiles on the central axis. From these profiles, we calculated the field dimension as the distance between the points corresponding to gray value of 50% relative to that on central axis, using Microsoft Office Excel 2007. Dose measurements were multiplied by the field size to obtain the DAP measured (DAPmeas). Finally, we obtained DAP calibration factors by dividing DAPmeas by DAP reading from the DAP meter installed (DAPnom).The DAP readings in the procedures under investigation were then corrected using the calibration factors determined.
The procedures under investigation were as follows: cerebral artery angiography, hepatic chemoembolization, percutaneous disc decompression, embolization of cerebral artery aneurysm, abdominal aortic endoprosthesis, facet joint injections, periradicular infiltration, nephrostomy, biliary drainage, limb salvage, varicocele embolization, carotid artery stenting, facet medial branch neurolysis, vertebroplasty, and ischemic stroke.
This randomized prospective study was approved by the ethical committee of our institute. Before enrollment, each patient provided formal informed consent. The study lasted 1 year, and 150 patients were enrolled, 10 for each procedure. At the end of each intervention, a dedicated staff filled out a form containing the patients’ personal information (extracted from medical record), technical and dosimetric data (from print patient report), and some other information by visual inspection of procedures performed in the operating room (e.g., region of the body irradiated). Specifically, the form gathered the following information: name, age, weight and height, procedure type, angiographic system used, average voltage and current of the tube, cumulative fluoroscopy time, number of radiographic and fluorographic images, position of the X-ray tube (both rotation and tilt), partial DAP values for each position of the X-ray tube, cumulative DAP, cumulative air kinetic energy released in matter, both in fluoroscopy and radiographic modality and body region. Data regarding height and weight were collected to calculate the corresponding body mass index (BMI) using the following formula:
To obtain the relationship between DAP and E values, tabulated conversion coefficients (CCp), which have been published in terms of E/DAP [16], were used. These CCp values were evaluated using a Monte Carlo code simulating an average adult patient; they were tabulated for each region of the body at a given fixed tube projections. That is, for each region and projection, the CCp values depended on tube voltage and total tube filtration. Tabulated values of tube potential ranged from 50 to 120 kVp, while those for total filtration ranged between 2 and 5 mm Al. These CCp values were used with some approximations. As not all projections and body regions involved in these procedures were considered in the present report, those missing were approximated to those of the closest-tabulated data [16]. In addition, the published CCp values allowed for a maximum total beam filtration of 5 mm Al, even though some of the investigated procedures were performed using an equivalent Al filtration of > 5 mm. To extrapolate for these, the tube voltages and best fit projections of the tabulated CCp values were estimated, using an exponential function, as a function of the filter equivalent thickness. In this way, we calculated the CCp value of each single examination.
In all the procedures involving > 1 projection or body region, the corresponding partial effective dose (\( E_{i,j} = {\text{CC}}_{i,j} \cdot {\text{DAP}}_{i,j} \)) was calculated for each irradiation condition (i) and patient (j). On the basis of all i projections, the total effective dose for patient j(\( E_{\text{j}} \)) was then calculated as \( E_{j} \; = \;\sum\nolimits_{i} {E_{i,j} } \).
Finally, in each p procedure, the total E was obtained as the average of all \( E_{\text{j}} \) values. The average CCp value of each p procedure was also measured, as was its corresponding ranges.
3 Results
The calibration factors of the DAP meters ranged from 0.44 to 0.75 when the patient table and mattress were included, and from 0.87 to 1.4 in air (i.e., without the patient table and mattress). These factors depended on the tube voltage and filtration conditions used. For example, Tables 1 and 2 show calibration factors for one of the two Philips units under one filtration condition (0.1 mm Cu + 1 mm Al additional filtration setting) in fluoroscopic modality, with and without a patient table and mattress included, respectively. Table 3 reports for each procedure the BMI, cumulative fluoroscopy time, number of radiographic images, and tube voltage, along with the corresponding ranges. The following procedures involved a longer fluoroscopy time and higher number of radiographic images: embolization of cerebral artery aneurysm, abdominal aortic endoprosthesis, and limb salvage. The measured DAPs, together with the CC p conversion coefficients and calculated E values, are shown in Table 4. The values represent the overall average of patients who underwent the same p procedure. The average estimated CC p values ranged from 0.07 to 0.25 mSvGy−1 cm−2 in all procedures involving the head, as well as in periradicular infiltration. By comparing Tables 3 and 4, we can see that higher DAP values correspond to higher cumulative fluoroscopy times and/or higher radiographic images, except in the case of the limb salvage procedure. The reasons for this occurrence have been already discussed in a previous study [4]. The E values ranged from 5.4 to 166.3 mSv for both facet joint injection and abdominal aortic endoprosthesis. These procedures had the shortest and longest fluoroscopy times, as well as the lowest and highest numbers of required radiographic images, respectively. Thus, they also had the lowest and highest DAP values.
4 Discussion
In interventional radiology, it is difficult to manage radiation risk. First, there is no agreement on appropriate indicators suitable to characterize the radiation risk. Moreover, not all procedures are standardized, and the reference levels suggested in the literature refer only to certain specific interventional radiological procedures [17, 23,24,25,26]. In this regard, E can be used to compare the risks among different technologies or radiological procedures, as well as to compare exposure among patients subjected to the same procedure, but in different hospitals.
In the literature, several strategies have been proposed to determine E [27]. Such approaches use both direct and indirect methods [12,13,14,15, 28]. In the present study, E was determined on the basis of DAP values. The values were properly corrected for the calibration factors, and the conversion coefficients from Ref. [16] were revised to take into account the technical specifications of the procedures under investigation. E values ranging from 5.4 to 166.3 mSv—for facet joint injections and abdominal aortic endoprosthesis, respectively—were obtained.
As a rule, it is not possible to guarantee a monotonically increasing relationship between E and DAP. However, in the present study, higher DAPs corresponded to higher E values, and vice versa. The DAP and E values obtained in the present study were not always in agreement with those reported in the literature, although the data available in the literature are not even in agreement with each other [1, 9,10,11,12,13,14, 29, 30]. As there are many factors that can affect dosimetric data within the same type of procedure, a reliable comparison was difficult to obtain. In fact, each specific procedure depends on the specific protocol used by radiologists, which can differ in terms of (1) the characteristics of the fluoroscopy and cine views (orientations and number of radiographic images), (2) the geometry of the fields being used (distances, field sizes), (3) technical parameters (filtration and tube voltage), (4) changes of physicians and medical staff, and (5) experience and variation in patients’ anatomy and pathology. In addition, the comparison was further complicated because interventional procedures were not classified in the same way.
Specifically, procedures involving the chest and abdominal regions had, on average, conversion factors similar to each other (ranging from 0.19 to 0.25 mSv/Gy cm2). These values are consistent with data reported in the literature [1, 8,9,10, 13, 31, 32]. For example, both hepatic chemoembolization and nephrostomy yielded a CCp value of 0.20 mSv/Gy cm2, which falls within the range of values reported in the literature (from 0.13 to 0.16 and from 0.16 to 0.26, respectively) [1, 9, 10]. A unique coefficient of 0.07 mSv/Gy cm2 was found in the case of procedures that affected the head region; this figure is also quite consistent with that reported in the literature [1, 8].
In the case of the lower limb procedure, values ranging from 0.02 to 0.26 mSv/Gy cm2 are reported in the literature [1, 10, 13, 32]. Such a wide range is unsurprising considering that these values refer to generic peripheral or lower extremity procedures and no other information is available. The CCp we found in the present study (0.11 mSv/Gy cm2) is well within this range.
Regarding percutaneous disk decompression, abdominal aortic endoprosthesis, facet joint injections, periradicular infiltration, ischemic stroke, and facet medial branch neurolysis, to our knowledge, no dosimetric data are available in the literature. However, although these procedures do not involve patient exposure to high-radiation doses, we believe estimation of their associated radiation risk is important, as these procedures are common in hospitals and are often repeated in adjacent body regions. In addition, the availability of information in the literature may help physicians in standardizing the various techniques, which will in turn allow reliable comparison among the different operating methods.
The uncertainty for the dose values proposed in this work has two major components. First were uncertainties associated with the calculation of corrective factors. Specifically, in certain cases, the angle projections or tube potentials did not coincide exactly with the reported data [16]. For this reason, some approximations were performed, whereby we performed a projection and chose the potential value closest to the actual value. That is, the value reported in the literature was adopted (approximately 12%) [10], as the same method was applied to determine the CC p values but in different types of procedures. The uncertainty in the fitting procedure of the tabulated CC p values was considered negligible with regard to the filter equivalent thickness. That is, the R2 value associated to the fit was close to 1. The second component of uncertainty was related to the procedure used to calibrate the DAP. A global estimation of 12% was made. However, using the propagation error theory, a combined uncertainty of approximately 17% was calculated and adopted.
Another concern is regarding the dependence of conversion factors on BMI. As reported in [33], the NPRB coefficients were published for patients with standard dimension and tend to overestimate the effective dose for obese patients. As reported in Table 3, our average BMI values for all procedures are close to 25 kg/m2, which is the limit accepted in the literature for overweight patients and would not be considered as obese (> 30 kg/m2). Hence, we are confident that the effective dose values reported in this study are reliable and maybe used as a preliminary guidance for other centers that perform similar procedure.
5 Conclusion
In the present study, we estimated the E values of some interventional radiological procedures. Our estimation was based on DAP measurement and used tabulated conversion coefficients that have been published in terms of E/DAP. For some procedures, the DAP and E values were different from those reported in the literature. By contrast, the CC p values were fairly in agreement with those proposed in the literature for a large set of procedures. Therefore, we can conclude that these discrepancies were mainly due to DAP values, which in turn depend on how the procedures are performed. This suggests that all interventional procedures should be univocally classified, optimized, and standardized to allow valid comparative studies and universal reference levels. Importantly, the E values found in this study are the first to appear in the literature, although some of the procedures analyzed do not expose patients to high-radiation doses. A larger number of procedures will have to be investigated to confirm our data. Nonetheless, this study could be used as a preliminary guidance for other centers that perform similar procedures.
References
McParland BJ. A study of patient radiation doses in interventional radiological procedures. Br J Radiol. 1998;71:175–85.
Miller DL, Balter S, Wagner LK, Cardella J, Clark TWI, Neithamer CD, Schwartzberg MS, Swan TL, Towbin RB, Rholl KS, Sacks D. Quality improvement guidelines for recording patient radiation dose in the medical record. J VascIntervRadiol. 2004;15:423–9.
Balter S, Hopewell JW, Miller DL, Wagner LK, Zelefsky MJ. Fluoroscopically guided interventional procedures: a review of radiation effects on patients’ skin and hair. Radiology. 2010;254(2):326–41.
Falco MD, Masala S, Stefanini M, Fiori R, Gandini R, Bagalà P, Morosetti D, Calabria E, Tonnetti A, Verona-Rinati G, Santoni R, Simonetti G. Patient skin dose measurements using a cable free system MOSFETs based in fluoroscopically guided percutaneous vertebroplasty, percutaneous disc decompression, radiofrequency medial branch neurolysis, and endovascular critical limb ischemia. J. Appl. Clin. Med Phys. 2015;16(1):298–310.
Söderman M, Mauti M, Boon S, Omar A, Marteinsdóttir M, Andersson T, Holmin S, Hoornaert B. Radiation dose in neuroangiography using image noise reduction technology: a population study based on 614 patients. Neuroradiology. 2013;55:1365–72.
Euratom BSS. Council Directive 2013/59 EURATOM of 5 December 2013 Laying Down the Basic Safety Standards for the Protection of the Health of Workers and the General Public against the Dangers Arising from Ionizing Radiation, and Repealing Directives 89/618/Euratom. 2013.
International Commission on Radiological Protection. Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann. ICRP. 2007;37:1–332.
Schultz FW, Zoetelief J. Dose conversion coefficients for interventional procedures. RadiatProtDosim. 2005;117:225–30.
Bor D, Sancak T, Olgar T, Elcim Y, Adanali A, Sanlidilek U, Akyar S. Comparison of effective doses obtained from dose-area product and air kerma measurements in interventional radiology. Br J Radiol. 2004;77:315–22.
Compagnone G, Giampalma E, Domenichelli S, Renzulli M, Golfieri R. Calculation of conversion factors for effective dose for various interventional radiology procedures. Med Phys. 2012;39(5):2491–8.
Fitousi NT, Efstathopoulos EP, Delis HB, Kottou S, Kelekis AD, Panayiotakis GS. Patient and staff dosimetry in vertebroplasty. Spine. 2006;31(23):E884–9.
Von Wrangel A, Cederblad A, Rodriguez-Catarino M. Fluoroscopically guided percutaneous vertebroplasty: assessment of radiation doses and implementation of procedural routines to reduce operator exposure. Acta Radiol. 2009;50:490–6.
Molyvda-Athanasopoulou E, Karlatira M, Gotzamani-Psarrakou A, Koulouris C, Siountas A. Radiation exposure to patients and radiologists during interventional procedures. RadiatProtDosim. 2011;147(1–2):86–9.
Tappero C, Barbero S, Costantino S, Bergui M, Ropolo R, Bradac G, Gandini G. Patient and operator exposure during percutaneous vertebroplasty. Radiol Med. 2009;114:595–607.
Smans K, Struelens L, Hoornaert MT, Bleeser F, Buls N, Bosmans H. A study of the correlation between dose area product and effective dose in vascular radiology. RadiatProtDosim. 2008;130:300–8.
Hart D, Jones DG, Wall BF. Estimation of effective dose in diagnostic radiology from entrance surface dose and dose-area product measurements. National Radiological Protection Board, Chilton. Technical Report NRPB-R262. (1994).
Balter S, Miller DL, Vano E, Ortiz Lopez P, Bernardi G, Cotelo E, Faulkner K, Nowotny R, Padovani R, Ramirez AA. pilot study exploring the possibility of establishing guidance levels inx-ray directed interventional procedures. Med Phys. 2008;35:673–80.
Faulkner K, Busch HP, Cooney P, Malone JF, Marshall NW, Rawlings DJ. An international intercomparison of dose-area product meters. RadiatProtDosim. 1002;43:131–4.
International Commission on Radiation Units and Measurements. Patient dosimetry for X rays used in medical imaging. ICRU Report 74. J. ICRU. 2005;5(2):1–113.
International Electrotechnical Commission. Area exposure product meter. IEC Report 580, Geneva (1977).
Wall BF. Quality control of dose-area product meters. Technical and Physical Parameters for Quality Assurance in Medical Radiology, BIR Report 18, 140-142. Moores BM, Stieve FE, Eriskat H, Schibilla H (BIR, London, 1989).
International Atomic Energy Agency. Dosimetry in diagnostic radiology: An international code of practice. Technical Reports Series 457. IAEA, Vienna (2007).
Vano E, Sanchez R, Fernandez JM, Gallego JJ, Verdu JF, Gonzalez de Garay M, Azpiazu A, Segarra A, Hernandez MT, Canis M, et al. Patient dose reference levels for interventional radiology: a national approach. CardiovascInterventRadiol. 2009;32:19–24.
Miller DL, Kwon D, Bonavia GH. reference levels for patient radiation dose in interventional radiology: proposed initial values for U.S. practice. Radiology. 2009;253(3):753–64.
Topaltzikis T, Rountas C, Moisidou R, Fezoulidis I, Kappas C, Theodorou K. Radiation dose to patients and staff during angiography of the lower limbs. Derivation of local dose reference levels. Phys. Medica. 2009;25:25–30.
Miller DL, Balter S, Cole PE, Lu HT, Schueler BA, Geisinger M, Berenstein A, Albert R, Georgia JD, Noonan PT, et al. Radiation doses in interventional radiology procedures: the RAD-IR study part i: overall measures of dose. J VascIntervRadiol. 2003;14:711–27.
Padovani R, Quai E. Patient Dosimetry approaches in interventional Cardiology and literature dose data review. RadiatProtDosim. 2005;117(1–3):217–21.
Perisinakis K, Damilakis J, Theocharopoulos N, Papadokostakis G, Hadjipavlou A, Gourtsoyiannis N. Patient exposure and associated radiation risks from fluoroscopically guided vertebroplasty or kyphoplasty. Radiology. 2004;232(3):701–7.
Sapiin B, Ng KH, Abdullah BJJ. Radiation Dose to Patients Undergoing Interventional Radiological Procedures in Selected Hospitals in Malaysia: Retrospective Study. J.H.K. CollRadiol. 2004; 7:129–136.
Struelens L, Vanhavere F, Bosmans H, Van Loon R. Effective doses in angiography and interventional radiology: calculation of conversion coefficients for angiography of the lower limbs. Br J Radiol. 2005;78:135–42.
Hidajat N, Wust P, Felix R, Schroder RJ. Radiation exposure to patient and staff in epatic chemoembolization: risk estimation of cancer and deterministic effects. CardiovascInterventRadiol. 2006;29:791–6.
Hart, D. and Wall, B. F. Radiation Exposure of the UK Population from Medical and Dental X-ray Examinations. National Radiological Protection Board, Chilton. NRPB –W4. (2002).
Ector J, Dragusin O, Adriaenssens B, Huybrechts W, Willems R, Ector H, et al. Obesity is a major determinant of radiation dose in patients undergoing pulmonary vein isolation for atrial fibrillation. J Am Coll Card. 2007;50(3):234–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they had no conflict of interest in this study.
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of the Institutional Review Board (IRB) and with the 1964 Helsinki Declaration and its later amendments. This article does not contain any studies with animals.
Informed consent
Informed consent was obtained from all individual participants in the study.
About this article
Cite this article
Falco, M.D., Masala, S., Stefanini, M. et al. Effective-dose estimation in interventional radiological procedures. Radiol Phys Technol 11, 149–155 (2018). https://doi.org/10.1007/s12194-018-0446-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-018-0446-5