Abstract
Our aim was to show whether sensitivity for detecting volume changes in regional gray matter in default mode network (DMN) at converted [from mild cognitive impairment to Alzheimer’s disease (from MCI to AD)] phase was improved by use of a standardized volume with global gray-matter volume. T1-weighted MR images (T1WI) of seven normal subjects and seven converted (from MCI to AD) patients were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database. Gray-matter images segmented with Statistical Parametric Mapping 5 were measured by the atlas-based method. We focused on five nodes of the DMN. For each phase, region of interest (ROI) volumes in the five nodes were standardized by two methods: (1) the ratio to the screening phase (S_volume) and (2) the ratio to the screening phase after both volumes were standardized by the global gray-matter volume (S_N_volume). Significant group differences between longitudinal gray-matter volume change of the converted (from MCI to AD) group and that of the normal group were found in lateral temporal cortex by S_N_volume, and precuneus by S_N_volume. These findings are useful for improving the understanding of DMN volume changes at the converted (from MCI to AD) phase.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Resting-state functional magnetic resonance imaging (RfMRI) has rapidly become the target of advanced research in brain function studies [1]. RfMRI is a noninvasive technique used for investigating and characterizing in vivo the spontaneous correlations of blood-oxygen-level-dependent (BOLD) signals within and between different regions of the brain. RfMRI is an important diagnostic tool for evaluating brain function and neuronal connectivity. Previous reports of resting-state functional connectivity suggest the existence of at least three canonical networks [2–5]. The first, termed the central executive network, comprises the dorsolateral prefrontal cortex and posterior-parietal cortex and is also considered crucial for maintenance and processing of information in the working memory. The second, termed the salience network, includes the anterior cingulate cortex and fronto-insular cortex, which are combined as the ventrolateral prefrontal cortex and anterior insula. The third system, termed the default mode network (DMN), combines the posterior cingulate cortex, precuneus, lateral temporal cortex (LTC), medial prefrontal cortex (MPFC), and inferior parietal lobule (IPL). Analysis of low-frequency spontaneous BOLD fluctuations enables RfMRI to detect resting-state synchronization in the functional network of these regions [2, 6–9]. Because this network is typically deactivated during external stimulation, it has been termed the DMN.
Many studies have investigated the behavioral function of the DMN. The role of the DMN is to optimize performance by allocating resources to task-related regions and away from task-irrelevant structures [10]. It has been suggested that the DMN is involved in the processes of self-referential mental activity and introspectively oriented mode [11] and that it plays a role in attending to environmental stimuli as well as mediating processes such as reviewing past knowledge and preparing future actions. It may also be involved in episodic memory [12].
Interestingly, the DMN regions comprise the typical predilection sites of Alzheimer’s disease (AD) [13], the most frequent cause of dementia in the elderly and the most common neurodegenerative disorder in humans. Early symptomatology for AD has been linked to changes in the DMN, based on glucose metabolism and blood flow positron emission tomography and single photon emission computed tomography measurements [14]. RfMRI has identified significant disruptions in DMN co-activation in patients with AD [12, 15]. In addition, RfMRI is a non-invasive and radiation-exposure-free biomarker of early AD [12]. As a result, the DMN has rapidly become the target of extensive research in the AD field [14, 16–20].
However, to the best of our knowledge, estimation of subdivided DMN volume in normal and converted [from mild cognitive impairment to Alzheimer’s disease (from MCI to AD)] groups has not been reported in previous studies. We can estimate the gray-matter volume of the DMN by the atlas-based method using segmented gray-matter images from magnetic resonance (MR) T1-weighted images (T1WI) [21]. Therefore, our aim in the present study was to show whether the sensitivity for detecting volume changes of regional gray matter in DMN at the converted (from MCI to AD) phase was improved by use of standardized volume with global gray-matter volume compared with another method in the atlas-based method.
2 Materials and methods
2.1 Subjects
Data used in the preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.ucla.edu). The ADNI was launched in 2003 by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, the Food and Drug Administration, private pharmaceutical companies, and non-profit organizations, as a $60 million, 5-year public–private partnership. The primary goal of the ADNI has been to test whether serial MRI, positron emission tomography (PET), other biological markers, and clinical and neuropsychological assessment can be combined for measurement of the progression of MCI and early AD. Determination of sensitive and specific markers of very early AD progression is intended to aid researchers and clinicians to develop new treatments and monitor their effectiveness, as well as lessen the time and cost of clinical trials.
ADNI is the result of efforts of many co-investigators from a broad range of academic institutions and private corporations, and subjects have been recruited from more than 50 sites across the US and Canada. The initial goal of ADNI was to recruit 800 adults, ages 55–90 years, to participate in the research, with approximately 200 cognitively normal older individuals to be followed for 3 years, 400 people with MCI to be followed for 3 years, and 200 people with early AD to be followed for 2 years. (For up-to-date information, see http://www.adni-info.org.)
We downloaded data on two groups: a normal group and a converted (from MCI to AD) group, from the ADNI database. The ADNI database includes several hundred subjects in each group (i.e., normal, MCI, and AD). However, public data in the converted (from MCI to AD) group in the ADNI includes only 16 subjects. In addition, subjects with deficit data (i.e., deficit on 3D-T1WI or deficit on cognitive function tests) were excluded from this study. As a result, used data as converted (from MCI to AD) group were 7 subjects. We then set up these two groups of subjects in whom three factors (gender, age, and education period) were matched between the normal and the converted (from MCI to AD) group. The characteristics of these groups are summarized in Tables 1 and 2. Table 1 shows individual information (converted phase, gender, age, and education period) on the matched participants in our study (from the ADNI database). The converted phase means phase at conversion from MCI to AD. Table 2 shows cognitive test scores of the matched groups in our study (from the ADNI database). The 3D-T1WIs for all subjects in the present study were obtained by a 1.5 Tesla scanner at each visit phase (at screening and at 6, 12, 24, 36, and 48 months). Subjects with MCI visited at 18 months additionally. Details on the MRI scanning protocol are indicated in the ADNI database. The MRI scanning protocols are identical for each subject.
2.2 Image processing for brain tissue segmentation
We used Statistical Parametric Mapping 5 (SPM5) [22] software (Wellcome Department of Imaging Neuroscience Group, London, UK; http://www.fil.ion.ucl.ac.uk/spm). The 3D-T1WIs in native space were bias-corrected, spatially normalized, and segmented into gray matter, white matter, and cerebrospinal fluid images. The voxel size was set to 2 × 2 × 2 mm3 for the spatially normalized images and was set as the default on SPM5 for other images. The parameters of SPM5 were identical in analyses for all T1WIs.
2.3 Atlas-based volume measurement method and statistical analysis
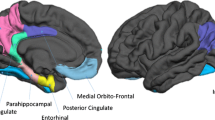
Regions of interest (ROI) for gray-matter volume measurement of the DMN were obtained by WFU PickAtlas [21]. This program automatically generates segmented atlas ROI templates in Montreal Neurological Institute (MNI) space [23]. The ROIs defined in the atlas were originally based on manual drawing of the borders of brain regions according to the Talairach atlas [21]. Figure 1 shows the placement of ROIs in the following five DMN regions: posterior cingulate, precuneus, LTC, MPFC, and IPL [14, 16–18, 20]. ROI volume measurements were performed on spatially normalized gray-matter images for each of the five regions. ROI volumes were calculated by ‘number of voxel in the ROI’ × ‘tissue existence probability’. Brain shapes were normalized to MNI space, and intensity modulation step was included in this normalization process. Then, the spatially normalized gray-matter images have information of tissue existence probability. The gray-matter volumes can be calculated from tissue existence probability. ROI volumes were measured bilaterally in all subjects. ROI volumes for the five regions were standardized in each phase by two methods: 1) the ratio to the screening phase (S_volume) and 2) the ratio to the screening phase after both volumes were standardized by the global gray-matter volume (S_N_volume). S_volume and S_N_volume were defined by the following formulae:
The global gray-matter volume was measured by SPM5.
Two-way repeated measure analysis of variance (two-way repeated ANOVA) was used to test for group differences (the independent variable is group, and the dependent variable is visit phase) in S_volume and S_N_volume in each of the five ROIs between the normal group and the converted (from MCI to AD) group. Significant difference was defined as p < 0.1.
3 Results
Two-way repeated ANOVA revealed significant group differences in the LTC for S_N_volume (more progressive value reduction of S_N_volume in the converted (from MCI to AD) group compared with the normal group) and in the precuneus for S_N_volume (more progressive value increase of S_N_volume the converted (from MCI to AD) group compared with the normal group). No significant group differences in other ROIs for S_N_volume and in all ROIs for S_volume were found. The trend of visit-phase-related volume change is shown in Fig. 2.
Scatterplots of S_N_volume (left side) and S_volume (right side) according to visit phase. Two-way repeated ANOVA revealed significant group differences between the normal and converted (from MCI to AD) groups in the LTC for S_N_volume and in the precuneus for S_N_volume. S_volume is defined as the ratio to the screening phase; S_N_volume is defined as the ratio to the screening phase after both volumes were standardized by global gray-matter volume (see formulae in the Sect. 2). Visit phase is shown on the horizontal axes [at screening and at 6, 12, 24, 36, and 48 months (m)]. The ROI names are indicated on the respective plot areas. The mean of the standardized value in the normal (red) and converted (from MCI to AD) groups (blue) is shown with the respective standard deviation
4 Discussion
In the present study, significant group differences were observed in regional volumes for S_N_volume, but not for S_volume. For example, the LTC of the converted (from MCI to AD) group showed progressive value reduction of S_N_volume (see the left-side panel of the LTC in Fig. 2), while there appeared to be more progressive value increase of S_N_volume in the precuneus of the converted (from MCI to AD) group (see the left-side panel of the precuneus in Fig. 2) than in the normal group. Therefore, our results suggest that S_N_volume is more sensitive than S_volume for detecting atrophy. S_N_volume is corrected for individual differences in the speed of global brain atrophy (i.e., a high S_N_volume value indicates that the reduction in ROI volume is less rapid than that in global gray matter, while a low S_N_volume value indicates that the reduction in ROI volume is more rapid than that in global gray matter). In other words, more progressive value increase of S_N_volume in the precuneus of the converted (from MCI to AD) group than in the normal group does not mean volume increase of the precuneus; it means that the reduction in the volume of precuneus in the converted (from MCI to AD) group is less rapid than that in the global gray matter compared with the normal group. In contrast, S_volume is not corrected for individual differences in the speed of global brain atrophy. That is, S_N_volume is influenced by ‘cortex atrophy in AD effect’, and S_volume is influenced by ‘cortex atrophy in AD effect’ and ‘cortex atrophy in aging effect’ [24–27]. Standard deviations were generally larger in S_volume than in S_N_volume, probably because S_volume includes individual differences in aging effect (see Fig. 2). This difference in the variation of data points between S_volume and S_N_volume may explain why S_N_volume is more sensitive than S_volume for detecting brain atrophy in the DMN.
In many previous reports, a significantly reduced gray-matter volume was observed in the LTC of AD patients (compared with controls) [26–29]. In addition, in comparing AD patients with controls, Frisoni et al. [30] reported that the largest atrophic regions (i.e., largest significant cluster size) corresponded to the hippocampal cortex while smaller atrophic regions (i.e., smaller significant cluster size) were found in the temporal and cingulate gyri. Based on these lines of evidence, it is widely accepted that atrophy is more progressive in the LTC of patients with AD and MCI compared with that in normal subjects.
In the present study, volume reduction in the LTC of the converted (from MCI to AD) group was more progressive compared with that of the normal group in terms of S_N_volume.
It appears to be an error of brain volume analysis that the atrophy speed of the precuneus in the converted (from MCI to AD) group was slower than that of the normal group. However, two previous studies showed increased cortical thickness in the precuneus of an asymptomatic MCI group compared with a control subject group and suggested that this increment in cortical thickness could be related to reactive neuronal hypertrophy and/or inflammation driven by amyloid in the very early stages of the disease [31, 32]. Therefore, we hypothesize that the less rapid volume loss in the precuneus of the converted (from MCI to AD) group in the present study could be related to reactive neuronal hypertrophy and/or to inflammation driven by amyloid.
Group differences between the normal group and the converted (from MCI to AD) group were not observed in the other three regions (posterior cingulate, medial prefrontal cortex, and inferior parietal lobule). However, the results must be interpreted with caution. Volume changes may not have been observed because of two factors: a small sample size and a small gray-matter volume change in the regions. We expect that volume changes would also have been observed in these three regions if we had used a large sample, because gray-matter volume reduction was observed in these three regions in previous studies [26–30]. In other words, in the present study, group differences between the normal group and the converted (from MCI to AD) group were larger in the LTC and precuneus than in the other three regions.
Early pathology observations have revealed that AD affects a subset of neurons in regional and laminar specific neuronal systems [33]. A disconnection syndrome occurs in AD, beginning with the entorhinal cortex, after which the disease gradually progresses in a stepwise fashion along cortico-cortical connections [34]. Large cross-sectional studies have revealed that cortical neurofibrillary tangle densities and amyloid deposition are associated with the severity of dementia, neuronal loss, and atrophy [35]. These pathology observations support the hypothesis that the DMN and its subsystems are affected early in AD and MCI. In fact, other previous studies have demonstrated a loss of functional connectivity in the DMN in AD and MCI [36, 37].
Petrella et al. [38] showed highest integrity in controls and lowest integrity in subjects with AD for fMRI-measured DMN connectivity using goodness-of-fit indices. Although an association between AD and the DMN is of great interest, there are few reports on DMN gray-matter volume in AD patients. One previous report [38] found a significant difference in gray-matter probability in the DMN among four groups. When individual brain shapes were transformed to MNI space by the spatial normalization process with intensity modulation, signals of voxel in the spatially normalized gray-matter images mean the gray-matter probability. The four groups were normal controls, MCI nonconverters, MCI converters, and AD patients, and the gray-matter probabilities were 0.453 ± 0.024, 0.441 ± 0.036, 0.415 ± 0.028, and 0.422 ± 0.047, respectively. However, this previous report did not discuss the gray-matter volumes of the subdivided DMN. To the best of our knowledge, subdivided DMN volume changes in normal and AD groups are reported for the first time in the present report.
The hippocampus is integral to episodic memory processing [39]. Episodic memory loss is one of the cardinal features of AD [40] and the medial temporal lobe is among the first areas affected by pathology in AD [41]. The hippocampus has a key role in cognitive function. However, the hippocampus is relatively small, resulting in ROI placement being error prone. In addition, the bilateral hippocampus had the lowest associations with other regions of the DMN in both young and old cohorts [42], and numerous studies regarding hippocampal volume change in normal and AD subjects are reported. Therefore, we did not use a hippocampal ROI in the present study.
When gray-matter volume is measured in areas of the DMN defined by RfMRI, care must be taken regarding the following three factors:
-
1.
Previous studies showed that control by the gray-matter volume in each voxel is important in RfMRI because the signal is influenced by aging [43–45]. Activity expressed in resting-state networks was decreased (that is, a lower BOLD signal change was observed) in older compared with younger subjects. These results were influenced by correction with the gray-matter volume index within the areas of these resting-state networks. In addition, age effects are reported in several other brain regions with normal aging by RfMRI (increased parietal and decreased hippocampal activation [46, 47], increased [48] and also decreased [49] anterior cingulate cortex activation, decreased deactivation of the medial parietal/posterior cingulate region [50], and decreased activation of a large part of the frontal and/or parietal brain areas [51] ). Accelerated atrophy is also reported in the posterior cingulate gyrus, one of the core regions of the DMN [52] and an area with the earliest decline in glucose utilization in the preclinical stages of AD [53].
-
2.
The defined area of the DMN varies between RfMRI methods because of differences in analytical procedure among the various methods. Koch et al. [42] reported that effects of normal aging such as loss of the posterior cingulate cortex co-activity could be detected by independent component analyses, but not by signal time course correlation analyses of DMN inter-connectivity.
-
3.
Marek et al. [54] reported diurnal changes in the neuronal activity level of resting-state networks.
When reports regarding the gray-matter volume of the DMN are compared the influence of factors 1–3 may confuse our understanding of the phenomenon, whereas in contrast, DMN areas defined by use of the atlas-based method are generally consistent between reports. Therefore, when reports regarding gray-matter volume of the DMN are compared, the confusion factor is reduced in the atlas-based method compared with when RfMRI is used. However, we must be mindful that the DMN defined by the atlas-based method is not the true area of the DMN in the individual.
We used the voxel size as 2 × 2 × 2 mm3. If image with 2 × 2 × 2 mm3 was used as structural image, partial volume effect is an important problem. In addition, using smaller voxel size may improve the accuracy for brain volumetry with the spatial normalized gray-matter image. However, previous studies commonly used approximately 2 × 2 × 2 mm3. In our other study, we showed that variation of spatial resolution changed a result of brain volumetry. Therefore, if we want to compare the present report with previous reports, we need to use same voxel size between the present study and previous study.
A main limitation of the present study is that the DMN regions were defined by the atlas-based method rather than the RfMRI method. Unfortunately, because fMRI was not performed by ADNI on the participants in the present study, we are unable to infer individual DMN regions. A common definition of the DMN area was used, based on many reports [14, 16–18, 20]. We employed five nodes of the DMN based on the definitions provided in these reports. When gray-matter volume is measured in areas of the DMN defined by RfMRI, care must be taken regarding the three factors mentioned. Therefore, we think that estimates of gray-matter volume change with regions defined by RfMRI are complicatedness compared with atlas-based method as present study.
Another limitation is the small sample size (we used all public data of the converted (from MCI to AD) group in the ADNI (see the MATERIALS AND METHODS in the present report). The result of brain volumetry with MRI was influenced by many factors (i.e., image distortion, signal intensity non-uniformity of image, and signal-to-noise ratio) [55–58]. Further studies with a large sample size are required for validation of the present result. We expect that the ADNI data base provide more many data as converted (from MCI to AD) group.
The last limitation is the possibility of mis-registration in spatial normalization process and mis-segmentation in the gray-matter image. Volumetry with the normalized gray-matter image has this limitation. Therefore, we checked spatially normalized T1WIs and the gray-matter images, and we found not clearly mis-registration (i.e., mainly inversion of image-orientation) and mis-segmentation (i.e., mainly interfusion of the white matter). Group comparison method for volumetry with the spatially normalized gray-matter images was used many previous reports about brain atrophy, but we must be cautious with the possibility that the registration errors may have an undefined contribution to the result of the comparison between the groups.
5 Conclusion
To the best of our knowledge, this is the first study to show that sensitivity for regional gray-matter volume change in the DMN is improved by the use of standardized analysis with global gray-matter volume, and to report longitudinal change for gray-matter volumes of the subdivided DMN (posterior cingulate, precuneus, LTC, MPFC, and IPL) in normal and converted (from MCI to AD) groups. The results are useful for improving our understanding of the features of regional gray-matter volume indication methods and for improving our understanding of DMN volume changes in the converted (from MCI to AD) phase.
References
Biswal BB, Van Kylen J, Hyde JS. Simultaneous assessment of flow and bold signals in resting-state functional connectivity maps. NMR Biomed. 1997;10:165–70.
Greicius MD, Krasnow B, Reiss AL, Menon V. Functional connectivity in the resting brain: a network analysis of the default mode hypothesis. Proc Natl Acad Sci USA. 2003;100:253–8.
Fox MD, Corbetta M, Snyder AZ, Vincent JL, Raichle ME. Spontaneous neuronal activity distinguishes human dorsal and ventral attention systems. Proc Natl Acad Sci USA. 2006;103:10046–51.
Golland Y, Bentin S, Gelbard H, Benjamini Y, Heller R, Nir Y, et al. Extrinsic and intrinsic systems in the posterior cortex of the human brain revealed during natural sensory stimulation. Cereb Cortex. 2007;17:766–77.
Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56.
Gusnard DA, Raichle ME. Searching for a baseline: functional imaging and the resting human brain. Nat Rev Neurosci. 2001;2:685–94.
Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL. A default mode of brain function. Proc Natl Acad Sci USA. 2001;98:676–82.
Binder JR, Frost JA, Hammeke TA, Bellgowan PS, Rao SM, Cox RW. Conceptual processing during the conscious resting state. A functional MRI study. J Cogn Neurosci. 1999;11:80–95.
Shulman GL, Corbetta M, Buckner RL, Raichle ME, Fiez JA, Miezin FM, et al. Top-down modulation of early sensory cortex. Cereb Cortex. 1997;7:193–206.
Polli FE, Barton JJ, Cain MS, Thakkar KN, Rauch SL, Manoach DS. Rostral and dorsal anterior cingulate cortex make dissociable contributions during antisaccade error commission. Proc Natl Acad Sci USA. 2005;102:15700–5.
Fransson P. Spontaneous low-frequency bold signal fluctuations: an fMRI investigation of the resting-state default mode of brain function hypothesis. Hum Brain Mapp. 2005;26:15–29.
Greicius MD, Srivastava G, Reiss AL, Menon V. Default-mode network activity distinguishes alzheimer’s disease from healthy aging: evidence from functional MRI. Proc Natl Acad Sci USA. 2004;101:4637–42.
Mosconi L. Brain glucose metabolism in the early and specific diagnosis of Alzheimer’s disease. FDG-pet studies in mci and ad. Eur J Nucl Med Mol Imaging. 2005;32:486–510.
Buckner RL, Andrews-Hanna JR, Schacter DL. The brain’s default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38.
Rombouts SA, Damoiseaux JS, Goekoop R, Barkhof F, Scheltens P, Smith SM, et al. Model-free group analysis shows altered bold fMRI networks in dementia. Hum Brain Mapp. 2009;30:256–66.
Wermke M, Sorg C, Wohlschlager AM, Drzezga A. A new integrative model of cerebral activation, deactivation and default mode function in Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2008;35(Suppl 1):S12–24.
Fleisher AS, Sherzai A, Taylor C, Langbaum JB, Chen K, Buxton RB. Resting-state bold networks versus task-associated functional MRI for distinguishing Alzheimer’s disease risk groups. Neuroimage. 2009;47:1678–90.
McCaffrey P, Fagan T, Landhuis E. Alzheimer research series on the default network. J Alzheimers Dis. 2010;19:747–58.
Zhang D, Raichle ME. Disease and the brain’s dark energy. Nat Rev Neurol. 2010;6:15–28.
Shin J, Kepe V, Small GW, Phelps ME, Barrio JR. Multimodal imaging of Alzheimer pathophysiology in the brain’s default mode network. Int: J Alzheimers Dis; 2011. p. 687945.
Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage. 2003;19:1233–9.
Ashburner J, Friston KJ. Unified segmentation. Neuroimage. 2005;26:839–51.
Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89.
Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–42.
Goto M, Abe O, Aoki S, Takao H, Hayashi N, Miyati T, et al. Database of normal Japanese gray matter volumes in the default mode network. J Magn Reson Imaging. 2014;39:132–42.
Baron JC, Chetelat G, Desgranges B, Perchey G, Landeau B, de la Sayette V, et al. In vivo mapping of gray-matter loss with voxel-based morphometry in mild Alzheimer’s disease. Neuroimage. 2001;14:298–309.
Matsuda H, Kitayama N, Ohnishi T, Asada T, Nakano S, Sakamoto S, et al. Longitudinal evaluation of both morphologic and functional changes in the same individuals with Alzheimer’s disease. J Nucl Med. 2002;43:304–11.
Busatto GF, Garrido GE, Almeida OP, Castro CC, Camargo CH, Cid CG, et al. A voxel-based morphometry study of temporal lobe gray-matter reductions in Alzheimer’s disease. Neurobiol Aging. 2003;24:221–31.
Chetelat G, Desgranges B, De La Sayette V, Viader F, Eustache F, Baron JC. Mapping gray-matter loss with voxel-based morphometry in mild cognitive impairment. NeuroReport. 2002;13:1939–43.
Frisoni GB, Testa C, Zorzan A, Sabattoli F, Beltramello A, Soininen H, et al. Detection of grey matter loss in mild Alzheimer’s disease with voxel based morphometry. J Neurol Neurosurg Psychiatry. 2002;73:657–64.
Fortea J, Sala-Llonch R, Bartres-Faz D, Bosch B, Llado A, Bargallo N, et al. Increased cortical thickness and caudate volume precede atrophy in psen1 mutation carriers. J Alzheimers Dis. 2010;22:909–22.
Fortea J, Sala-Llonch R, Bartres-Faz D, Llado A, Sole-Padulles C, Bosch B, et al. Cognitively preserved subjects with transitional cerebrospinal fluid SS-amyloid 1–42 values have thicker cortex in Alzheimer’s disease vulnerable areas. Biol Psychiatry. 2011;70:183–90.
Hyman BT, Gomez-Isla T. Alzheimer’s disease is a laminar, regional, and neural system specific disease, not a global brain disease. Neurobiol Aging. 1994;15:353–4.
De Lacoste MC, White CL 3rd. The role of cortical connectivity in Alzheimer’s disease pathogenesis: a review and model system. Neurobiol Aging. 1993;14:1–16.
Berg L, McKeel DW Jr, Miller JP, Storandt M, Rubin EH, Morris JC, et al. Clinicopathologic studies in cognitively healthy aging and Alzheimer’s disease: relation of histologic markers to dementia severity, age, sex, and apolipoprotein e genotype. Arch Neurol. 1998;55:326–35.
Hedden T, Van Dijk KR, Becker JA, Mehta A, Sperling RA, Johnson KA, et al. Disruption of functional connectivity in clinically normal older adults harboring amyloid burden. J Neurosci. 2009;29:12686–94.
Sheline YI, Raichle ME, Snyder AZ, Morris JC, Head D, Wang S, et al. Amyloid plaques disrupt resting state default mode network connectivity in cognitively normal elderly. Biol Psychiatry. 2010;67:584–7.
Petrella JR, Sheldon FC, Prince SE, Calhoun VD, Doraiswamy PM. Default mode network connectivity in stable versus progressive mild cognitive impairment. Neurology. 2011;76:511–7.
Eichenbaum H. The hippocampus and declarative memory: cognitive mechanisms and neural codes. Behav Brain Res. 2001;127:199–207.
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology. 1984;34:939–44.
Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–59.
Koch W, Teipel S, Mueller S, Buerger K, Bokde AL, Hampel H, et al. Effects of aging on default mode network activity in resting state fMRI: does the method of analysis matter? Neuroimage. 2010;51:280–7.
Johnson SC, Saykin AJ, Baxter LC, Flashman LA, Santulli RB, McAllister TW, et al. The relationship between fMRI activation and cerebral atrophy: comparison of normal aging and Alzheimer disease. Neuroimage. 2000;11:179–87.
Prvulovic D, Hubl D, Sack AT, Melillo L, Maurer K, Frolich L, et al. Functional imaging of visuospatial processing in Alzheimer’s disease. Neuroimage. 2002;17:1403–14.
He Y, Wang L, Zang Y, Tian L, Zhang X, Li K, et al. Regional coherence changes in the early stages of Alzheimer’s disease: a combined structural and resting-state functional MRI study. Neuroimage. 2007;35:488–500.
Cabeza R, Daselaar SM, Dolcos F, Prince SE, Budde M, Nyberg L. Task-independent and task-specific age effects on brain activity during working memory, visual attention and episodic retrieval. Cereb Cortex. 2004;14:364–75.
Daselaar SM, Fleck MS, Dobbins IG, Madden DJ, Cabeza R. Effects of healthy aging on hippocampal and rhinal memory functions: an event-related fMRI study. Cereb Cortex. 2006;16:1771–82.
Sharp DJ, Scott SK, Mehta MA, Wise RJ. The neural correlates of declining performance with age: evidence for age-related changes in cognitive control. Cereb Cortex. 2006;16:1739–49.
Otsuka Y, Osaka N, Morishita M, Kondo H, Osaka M. Decreased activation of anterior cingulate cortex in the working memory of the elderly. NeuroReport. 2006;17:1479–82.
Lustig C, Snyder AZ, Bhakta M, O’Brien KC, McAvoy M, Raichle ME, et al. Functional deactivations: change with age and dementia of the Alzheimer type. Proc Natl Acad Sci USA. 2003;100:14504–9.
Damoiseaux JS, Beckmann CF, Arigita EJ, Barkhof F, Scheltens P, Stam CJ, et al. Reduced resting-state brain activity in the ‘‘Default network’’ In normal aging. Cereb Cortex. 2008;18:1856–64.
Andrews-Hanna JR, Reidler JS, Sepulcre J, Poulin R, Buckner RL. Functional–anatomic fractionation of the brain’s default network. Neuron. 2010;65:550–62.
Minoshima S, Giordani B, Berent S, Frey KA, Foster NL, Kuhl DE. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer’s disease. Ann Neurol. 1997;42:85–94.
Marek T, Fafrowicz M, Golonka K, Mojsa-Kaja J, Oginska H, Tucholska K, et al. Diurnal patterns of activity of the orienting and executive attention neuronal networks in subjects performing a stroop-like task: a functional magnetic resonance imaging study. Chronobiol Int. 2010;27:945–58.
Shuter B, Yeh IB, Graham S, Au C, Wang SC. Reproducibility of brain tissue volumes in longitudinal studies: effects of changes in signal-to-noise ratio and scanner software. Neuroimage. 2008;41:371–9.
Ewers M, Teipel SJ, Dietrich O, Schonberg SO, Jessen F, Heun R, et al. Multicenter assessment of reliability of cranial MRI. Neurobiol Aging. 2006;27:1051–9.
Goto M, Abe O, Kabasawa H, Takao H, Miyati T, Hayashi N, et al. Effects of image distortion correction on voxel-based morphometry. Magn Reson Med Sci. 2012;11:27–34.
Goto M, Abe O, Miyati T, Kabasawa H, Takao H, Hayashi N, et al. Influence of signal intensity non-uniformity on brain volumetry using an atlas-based method. Korean J Radiol. 2012;13:391–402.
Acknowledgments
This study was supported by a Grant-in-Aid for Scientific Research on Innovative Areas (Comprehensive Brain Science Network) from the Ministry of Education, Science, Sports and Culture of Japan.
Conflict of interest
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Alzheimer’s Disease Neuroimaging Initiative.
Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.ucla.edu). As such, the investigators within the ADNI contributed to the design and implementation of the ADNI and/or provided data but did not participate in the analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.ucla.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
About this article
Cite this article
Goto, M., Abe, O., Aoki, S. et al. Longitudinal gray-matter volume change in the default-mode network: utility of volume standardized with global gray-matter volume for Alzheimer’s disease: a preliminary study. Radiol Phys Technol 8, 64–72 (2015). https://doi.org/10.1007/s12194-014-0295-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12194-014-0295-9