Abstract
Haploidentical donors have emerged as an alternative donor source for salvage stem cell transplantation (SCT) after graft failure; however, data regarding salvage haploidentical SCT using posttransplant cyclophosphamide (PTCy) are limited. Using nationwide data (2011–2019), we retrospectively investigated transplant outcomes after salvage haploidentical SCT using PTCy for graft failure (n = 33, median age 34 years). The total dose of PTCy was 75–100 mg/kg (standard dose) in 26 patients (78.8%) and 40–50 mg/kg (lower dose) in 5 patients (15.2%). The neutrophil engraftment rate at 30 days was 81.8%. One-year overall survival (OS) and non-relapse mortality (NRM) rates were 47.4% and 46.0%, respectively. The standard-dose group exhibited better OS (61.1% vs. 0.0% at 1 year, P = 0.022) and NRM (35.1% vs. 80.0% at 1 year, P = 0.052) than the lower-dose group. Moreover, the standard-dose group was less prone to both grades II–IV (11.5% vs. 40.0%) and III–IV (0.0% vs. 40.0%) acute graft-versus-host disease (GVHD). Use of cyclophosphamide in previous SCT and conditioning did not affect OS or NRM. In conclusion, haploidentical salvage SCT using PTCy offers promising survival outcomes. Prospective studies are required to validate the efficacy of salvage haploidentical SCT using PTCy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Graft failure (GF) is a life-threatening complication following allogeneic stem cell transplantation (SCT) [1,2,3,4]. Between 4.0 and 7.3% of all allogeneic SCT cases exhibit GF [1,2,3,4,5]; a higher incidence is observed in cord blood transplantations [5]. Although salvage SCT is the only curative therapy for GF, the long-term survival rate after salvage SCT is still modest, reaching only 11–58% [1,2,3,4,5,6,7].
In the past decade, haploidentical donors emerged as alternative donors in salvage SCT because of rapid availability and fast neutrophil engraftment [8,9,10,11,12,13,14,15,16]; however, acute graft-versus-host disease (GVHD) commonly occurs after salvage SCT, occasionally hampering the success of salvage haploidentical SCT [9]. Most patients who underwent salvage haploidentical SCT received calcineurin inhibitor–based standard GVHD prophylaxis with or without antithymocyte globulin [8,9,10, 12,13,14,15], and data regarding the outcomes after salvage haploidentical SCT using posttransplant cyclophosphamide (PTCy) are still limited [8, 11, 12]. Currently, optimal strategies for salvage haploidentical SCT remain unestablished.
Therefore, on behalf of the Transplant Complications Working Group of the Japan Society for Transplantation and Cellular Therapy, this nationwide retrospective study aimed to evaluate the transplant outcomes and risk factors for survival after salvage haploidentical SCT using PTCy.
Materials and methods
The Transplant Registry Unified Management Program 2 of the Japanese Data Center for Hematopoietic Cell Transplantation provided the clinical data [17, 18]. Patients who were diagnosed with GF and underwent a second or higher allogeneic SCT from the haploidentical related donor (≥ 2 antigen-mismatch), using PTCy as GVHD prophylaxis, between 2011 and 2019 were included. GF diagnosis was made at the respective transplant center. Our retrospective study protocol adhered to the principles of the Declaration of Helsinki, with the approval of the institutional review board of the Tokai University School of Medicine.
In this study, overall survival (OS) was defined as the time between salvage SCT and death or the time of the last visit. Death without relapse or disease progression indicated non-relapse mortality (NRM). An absolute neutrophil count of at least 0.5 × 109/L for three consecutive times defined neutrophil engraftment. Regarding the total dose of PTCy, patients who received 75–100 mg/kg of PTCy were classified as the standard-dose group, whereas those who received 40–50 mg/kg of PTCy were classified as the lower-dose group. The dose of PTCy was at the discretion of each attending physician. The modified disease risk index was classified according to the previously reported criteria [19,20,21]. Acute and chronic GVHD were diagnosed and graded at each center according to the published criteria [22, 23]. Furthermore, we defined severe organ dysfunction as either ejection fraction ≤ 50%, serum creatinine ≥ 2 mg/dL, bilirubin ≥ 1.5 × upper limit of normal, or aspartate aminotransferase/alanine aminotransferase ≥ 2.5 × upper limit of normal [21, 24].
The distribution of patient characteristics was compared using Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables. We also used the Kaplan–Meier method to estimate OS probabilities, and the log-rank test to analyze differences among groups. The incidences of NRM, engraftment, acute and chronic GVHD, and Gray’s test were determined using a cumulative incidence method. The competing risks included relapse in the NRM analysis; NRM in the relapse analysis; relapse and NRM in the engraftment analysis; and relapse, NRM, and recurrent GF in the acute and chronic GVHD analysis. The OS was examined by multivariate analysis using the Cox proportional hazard regression model. Factors from the univariate analysis with P values < 0.1 were included in the multivariate analysis. Covariates included in the univariate models for each analysis are the total dose of PTCy, patient age, patient sex, performance status (PS) at salvage SCT, modified disease risk index, continuation of antimicrobial treatment at salvage SCT day, severe organ dysfunction, GVHD prophylaxis other than PTCy, conditioning regimen, donor source at salvage SCT, cyclophosphamide (Cy) use at previous SCT, transplantation year, and days from SCT to salvage SCT. All P values were two-sided, and all statistical data were analyzed using EZR, a graphical user interface for R software (the R Foundation for Statistical Computing, version 2.13.0, Vienna, Austria) [25].
Results
Patient and transplant characteristics
Table 1 shows the patient and transplant characteristics, and Table S1 describes them in detail. This study included 33 patients, with a median age of 34 (range: 2–67) years. Among them, 21 (63.6%) had a PS of 0–1. At salvage transplantation, 12 (36.4%) received treatment for active infection, and 5 (15.2%) had severe organ dysfunction. The median interval from previous SCT to salvage SCT was 49 (26–1468) days, and 22 patients (66.7%) underwent salvage SCT within 100 days from previous SCT. The total dose of PTCy was 75–100 mg/kg in 26 patients (78.8%, standard-dose group) and 40–50 mg/kg in 5 patients (15.2%, lower-dose group); however, that in 2 patients (6.1%) was unknown. Regarding previous SCT, 22 patients (67.7%) underwent cord blood transplantation and 6 patients (18.2%) had haploidentical transplantation. In the previous SCT, 17 patients (51.5%) received Cy as a conditioning regimen (n = 14) or GVHD prophylaxis (n = 4) (Table S1).
Outcomes after salvage SCT using PTCy
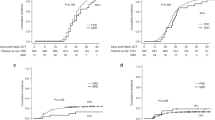
The median time for neutrophil engraftment after salvage SCT was 18 days, and the cumulative incidence of neutrophil engraftment at 30 days and platelet engraftment at 60 days was 81.8% (Fig. 1a) and 30.3% (Fig. 1b), respectively. Remarkably, neutrophil engraftment was successfully achieved at 22 days after salvage SCT in a patient who had donor-specific anti-HLA antibody (Table S1, case 32). The median OS was 359 days, and the OS at 1 year was 47.4% (Fig. 1c); in addition, the NRM at 1 year was 46.0% (Fig. 1d). At 100 days after salvage SCT, 15.2% and 6.1% of the patients experienced grade II–IV and III–IV acute GVHD (Fig. 1e, f), respectively.
Transplant outcomes after salvage haploidentical SCT using PTCy. The neutrophil (a) and platelet recovery rates (b), overall survival (c), non-relapse mortality (d), and the incidence of grade II–IV (e) and III–IV (f) acute GVHD. SCT stem cell transplantation, PTCy posttransplant cyclophosphamide, Cy cyclophosphamide, GVHD graft-versus-host disease
Prognostic effects of the total dose of PTCy
We investigated the prognostic effects of the total dose of PTCy for transplant outcomes after salvage SCT. No significant differences in patient characteristics were found between the standard-dose and lower-dose groups (Table S2). In the univariate analysis, the neutrophil engraftment was similar between the standard-dose and lower-dose groups (80.8% and 80.0%, respectively, at 30 days; P = 0.52; Fig. 2a), as was the case with platelet engraftment (34.6% and 20.0%, respectively, at 60 days; P = 0.28; Fig. 2b). Notably, the standard-dose group had a significantly better OS than the lower-dose group (61.1% vs. 0.0% at 1 year; P = 0.022; Table 2; Fig. 2c). In the multivariate analysis for OS adjusting for PS, lower-dose PTCy was significantly associated with a worse OS (hazard ratio, 3.03; 95% CI, 1.00–9.15; P = 0.049; Table 2). The standard-dose group had a lower NRM than the lower-dose group, but the difference was not significant (35.1% vs. 80.0% at 1 year; P = 0.052; Fig. 2d). Moreover, the standard group was less likely to experience both grades II–IV (11.5% vs. 40.0% at 100 days; P = 0.010; Fig. 2e) and III–IV of acute GVHD (0.0% vs. 40.0% at 100 days; P < 0.001; Fig. 2f) than the lower-dose group. Figure S1 shows the forest plot for OS stratified by patient characteristics. The beneficial effects of standard-dose PTCy was more evident in younger patients or those with good PS (Figure S1).
Transplant outcomes after salvage haploidentical SCT using PTCy stratified by the total dose of Cy. The neutrophil (a) and platelet recovery rates (b), overall survival (c), non-relapse mortality (d), and incidence of grade II–IV (e) and III–IV (f) acute GVHD. SCT stem cell transplantation, PTCy posttransplant cyclophosphamidem, Cy cyclophosphamide, GVHD graft-versus-host disease
Effects of Cy use in previous SCT and conditioning regimen
To elucidate the safety of successive Cy administration in a short period, we focused on patients who received Cy in previous SCT (n = 17) and those who received Cy-based conditioning regimen in salvage SCT (n = 10). The median total dose of Cy was 120 (50–130) and 30 (30–50) mg/kg in previous SCT and in the Cy-based conditioning regimen, respectively. Remarkably, the OS was comparable between patients with and without Cy administration in previous SCT (52.3% in patients with Cy in previous SCT vs. 43.8% in those without at 1 year; P = 0.83; Fig. 3a); the NRM was also comparable between these patients (47.8% in patients without Cy in previous SCT vs. 43.8% in those without at 1 year; P = 0.89; Fig. 3b). Regarding the conditioning regimen in the salvage SCT, fludarabine plus cyclophosphamide (FluCy)-based conditioning did not affect the OS (40.0% in patients with FluCy-based conditioning vs. 52.9% in those without at 1 year; P = 0.98; Fig. 3c). Although patients with FluCy-based conditioning had higher NRM than those without, the difference was still not significant (60.0% vs. 36.8% at 1 year; P = 0.51; Fig. 3d).
Subgroup analyses for transplant outcomes after salvage haploidentical SCT using PTCy stratified by Cy use in previous SCT and as the conditioning regimen. Overall survival (a) and non-relapse mortality (b) according to Cy use in previous SCT. Overall survival (c) and non-relapse mortality (d) according to the conditioning regimen. SCT stem cell transplantation, PTCy posttransplant cyclophosphamide, Cy cyclophosphamide
Discussion
This study demonstrated that salvage SCT using PTCy can lead to promising transplant outcomes and that administering the standard dose of PTCy can prevent severe acute GVHD and ensure long-term survival.
The feasibility of salvage haploidentical SCT has already been extensively studied [8,9,10,11,12,13,14,15,16]. However, reports about salvage haploidentical SCT using PTCy remain limited [8, 9, 11, 12]. Thus, this nationwide retrospective study investigated the transplant outcomes of salvage haploidentical SCT using PTCy. Salvage cord blood transplantation for GF entails the risks of recurrent GF and early mortality caused by the delayed neutrophil engraftment [4, 9, 16, 26], whereas salvage haploidentical SCT using antithymocyte globulin is associated with severe acute GVHD [9]. These problems can substantially hinder long-term survival after salvage SCT. Nevertheless, our study showed that haploidentical salvage SCT using PTCy offered fast neutrophil engraftment (81.8% at 30 days) and effectively prevented severe acute GVHD after salvage SCT (Grade III–IV; 6.1% at 100 days), leading to promising survival outcomes (47.4% at 1 year). Our results are similar to those of a French study, which reported an OS rate of 56% at 1 year and a neutrophil engraftment rate of 79% [11]. Given that 1-year OS after salvage cord blood transplantation reported so far was only 16.7–34.6% [9, 12, 16], our study further supports the idea that the strategy of salvage haploidentical SCT using PTCy can be a promising option for GF after allogeneic SCT. However, prospective studies are still required to investigate the efficacy and safety of salvage haploidentical SCT using PTCy.
Considering Cy toxicity, haploidentical SCT using lower-dose PTCy has been examined for years [27, 28]. A multicenter prospective study revealed that the 80 mg/kg of PTCy is feasible [27]. The incidence of acute and chronic GVHD in patients receiving 80 mg/kg of PTCy seemed comparable to the historical data using 100 mg/kg of PTCy (grade III–IV acute GVHD, 1–5%; chronic GVHD, 28–35%) [27, 29, 30]. However, patients receiving 25–50 mg/kg concentration of PTCy have a nonnegligible risk of developing severe acute GVHD (grade III–IV; 9.1–33%) [28]. Patients who developed GF are likely to suffer from concomitant infection [16] and severe organ dysfunction [5, 31] caused by the predisposed conditioning regimen, leading to a poor PS [21]. Therefore, the administration of lower-dose PTCy has been attempted. Our study included the largest number of patients who underwent salvage haploidentical SCT using PTCy for GF, enabling us to examine the prognostic factors for survival. We, for the first time, examined the prognostic impact of Cy dose in salvage SCT using PTCy. Unfortunately, lower-dose PTCy was significantly associated with worse OS. Patients who received lower-dose PTCy demonstrated similar neutrophil engraftment rate after salvage SCT. Nevertheless, lower-dose PTCy resulted in a significantly poor OS, which would be attributed to the higher incidence of severe acute GVHD after salvage SCT. Although frail patients could also be included in the lower-dose PTCy group, poor OS was also found in a multivariate analysis adjusting for PS. Given that three out of five patients in the lower-dose group succumbed to acute GVHD, standard-dose PTCy might be indispensable to effectively prevent the development of acute GVHD after salvage SCT.
Another clinical concern for salvage SCT using PTCy is whether patients who had received Cy as a conditioning regimen or GVHD prophylaxis in previous SCT can tolerate the successive Cy administration in a short period. The original method of haploidentical SCT using PTCy reported in 2008 included the Cy-containing conditioning regimen [32]; however, the incidence of Cy-induced cardiomyopathy reached 8.5% in patients who received a conditioning regimen with 200 mg/kg of Cy [33]. Even in patients who received 100–120 mg/kg of Cy, 1.4% experienced Cy-induced cardiomyopathy [33, 34]. Moreover, Cy-induced cardiomyopathy occurred after haploidentical SCT using PTCy was also reported.[34]. Thus, we evaluated the prognostic risk of Cy use in previous SCT and in the conditioning regimen. In previous SCT, 13 patients received Cy-based conditioning regimen, 3 received PTCy, and 1 received both Cy-based conditioning regimen and PTCy (Table S1). As for the conditioning regimen in salvage SCT, 10 patients used FluCy-based conditioning. Notably, OS and NRM were not significantly different with respect to the Cy use in previous SCT and in the conditioning regimen. One possible explanation for these results is that the duration from the previous SCT to salvage SCT (median 49 days) could mitigate toxicity associated with successive Cy administration. In fact, only one patient succumbed to organ failure after salvage SCT in our study (Table S1). Considering the low incidence of Cy-induced cardiomyopathy, the study’s small sample size precludes the definitive conclusion for the safety of successive Cy administration. Hence, our results should be carefully validated in larger cohorts.
This study has some limitations. First, this study is a retrospective study based on the registry database in Japan. Thus, the dose of PTCy was at the discretion of each attending physician or institution, possibly resulting in some biases. Moreover, our database does not include data on whether the GF was primary or secondary. Although the univariate analysis showed that the number of days from SCT to salvage SCT (cut-off points of 100 or 60 days) was not a significant prognostic factor, our results should still be carefully interpreted. Furthermore, the prognostic impact of PTCy dose focusing on the primary graft failure should be evaluated in a larger study. Second, the sample size is small for detecting the significant association between PTCy total dose and NRM. However, this study still demonstrated that the incidence of severe acute GVHD was significantly higher in the lower-dose PTCy group. Considering the dismal outcomes of patients who developed severe acute GVHD [35], the higher incidence of severe acute GVHD in the lower-dose PTCy group seemed unacceptable. Third, some data regarding patient characteristics were lacking, particularly the detailed information on anti-HLA antibody titers [36], suggesting the possibility of some biases. Despite these limitations, our study further supports the efficacy and safety of salvage SCT using PTCy for GF after allogeneic SCT. We believe that our results provide useful information for the prevention and treatment strategies for GF.
In conclusion, salvage haploidentical SCT using PTCy offers promising survival outcomes and could be a crucial option for GF after allogeneic SCT. An adequate dose of PTCy (i.e., 75–100 mg/kg) might be indispensable to achieve long-term survival. We plan to conduct a prospective study to further clarify the efficacy of salvage SCT using PTCy for GF after allogeneic SCT.
Data availability
Clinical data were provided by the Transplant Registry Unified Management Program 2 of the Japanese Data Center for Hematopoietic Cell Transplantation. Restrictions are applicable to the availability of the data, which were used under license for this study.
References
Olsson R, Remberger M, Schaffer M, Berggren DM, Svahn B-M, Mattsson J, et al. Graft failure in the modern era of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2013;48:537–43.
Olsson RF, Logan BR, Chaudhury S, Zhu X, Akpek G, Bolwell BJ, et al. Primary graft failure after myeloablative allogeneic hematopoietic cell transplantation for hematologic malignancies. Leukemia. 2015;29:1754–62.
Schriber J, Agovi M-A, Ho V, Ballen KK, Bacigalupo A, Lazarus HM, et al. Second unrelated donor hematopoietic cell transplantation for primary graft failure. Biol Blood Marrow Transplant. 2010;16:1099–106.
Fuji S, Nakamura F, Hatanaka K, Taniguchi S, Sato M, Mori S-I, et al. Peripheral blood as a preferable source of stem cells for salvage transplantation in patients with graft failure after cord blood transplantation: a retrospective analysis of the registry data of the japanese society for hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18:1407–14.
Waki F, Masuoka K, Fukuda T, Kanda Y, Nakamae M, Yakushijin K, et al. Feasibility of reduced-intensity cord blood transplantation as salvage therapy for graft failure: results of a nationwide survey of adult patients. Biol Blood Marrow Transplant. 2011;17:841–51.
Onishi Y, Mori T, Kako S, Koh H, Uchida N, Kondo T, et al. Outcome of second transplantation using umbilical cord blood for graft failure after allogeneic hematopoietic stem cell transplantation for aplastic anemia. Biol Blood Marrow Transplant. 2017;23:2137–42.
Lund TC, Liegel J, Bejanyan N, Orchard PJ, Cao Q, Tolar J, et al. Second allogeneic hematopoietic cell transplantation for graft failure: poor outcomes for neutropenic graft failure. Am J Hematol. 2015;90:892–6.
Kliman D, Bilmon I, Kwan J, Blyth E, Micklethwaite K, Panicker S, et al. Rescue haploidentical peripheral blood stem cell transplantation for engraftment failure: a single-centre case series. Intern Med J. 2018;48:988–91.
Harada K, Fuji S, Seo S, Kanda J, Ueki T, Kimura F, et al. Comparison of the outcomes after haploidentical and cord blood salvage transplantations for graft failure following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020;55:1784–95.
Tang BL, Zhu XY, Zheng CC, Liu HL, Geng LQ, Wang XB, et al. Successful early unmanipulated haploidentical transplantation with reduced-intensity conditioning for primary graft failure after cord blood transplantation in hematologic malignancy patients. Bone Marrow Transplant. 2015;50:248–52.
Prata PH, Resche-Rigon M, Blaise D, Socié G, Rohrlich P-S, Milpied N, et al. Outcomes of salvage haploidentical transplant with post-transplant cyclophosphamide for rescuing graft failure patients: a report on behalf of the francophone society of bone marrow transplantation and cellular therapy. Biol Blood Marrow Transplant. 2019;25:1798–802.
Singh H, Nikiforow S, Li S, Ballen KK, Spitzer TR, Soiffer R, et al. Outcomes and management strategies for graft failure after umbilical cord blood transplantation. Am J Hematol. 2014;89:1097–101.
Park JA, Koh KN, Choi ES, Jang S, Kwon SW, Park C-J, et al. Successful rescue of early graft failure in pediatric patients using T-cell-depleted haploidentical hematopoietic SCT. Bone Marrow Transplant. 2014;49:270–5.
Kato M, Matsumoto K, Suzuki R, Yabe H, Inoue M, Kigasawa H, et al. Salvage allogeneic hematopoietic SCT for primary graft failure in children. Bone Marrow Transplant. 2013;48:1173–8.
Moscardó F, Romero S, Sanz J, Sanz MA, Montesinos P, Lorenzo I, et al. T cell-depleted related HLA-mismatched peripheral blood stem cell transplantation as salvage therapy for graft failure after single unit unrelated donor umbilical cord blood transplantation. Biol Blood Marrow Transplant. 2014;20:1060–3.
Alcazer V, Conrad A, Valour F, Bachy E, Salles G, Huynh A, et al. Early-onset severe infections in allogeneic hematopoietic stem cell transplantation recipients with graft failure. Am J Hematol. 2019;94:E109–11.
Kanda J. Scripts for TRUMP data analyses. Part II (HLA-related data): statistical analyses specific for hematopoietic stem cell transplantation. Int J Hematol. 2016;103:11–9.
Atsuta Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10.
Armand P, Kim HT, Logan BR, Wang Z, Alyea EP, Kalaycio ME, et al. Validation and refinement of the Disease Risk Index for allogeneic stem cell transplantation. Blood. 2014;123:3664–71.
Armand P, Gibson CJ, Cutler C, Ho VT, Koreth J, Alyea EP, et al. A disease risk index for patients undergoing allogeneic stem cell transplantation. Blood. 2012;120:905–13.
Harada K, Kimura S-I, Fuji S, Najima Y, Yakushijin K, Uchida N, et al. Prognostic factors in salvage transplantation for graft failure following allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2021. https://doi.org/10.1038/s41409-021-01310-0.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant. 1995;15:825–8.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S, et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol. 1991;28:250–9.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Harada K, Fuji S, Seo S, Uchida N, Kawakita T, Yano S, et al. Comparison of immunosuppressant regimens in salvage cord blood transplantation for graft failure after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2021;56:400–10.
Sugita J, Kamimura T, Ishikawa T, Ota S, Eto T, Kuroha T, et al. Reduced dose of posttransplant cyclophosphamide in HLA-haploidentical peripheral blood stem cell transplantation. Bone Marrow Transplant. 2021;56:596–604.
Nakamae H, Koh H, Katayama T, Nishimoto M, Hayashi Y, Nakashima Y, et al. HLA haploidentical peripheral blood stem cell transplantation using reduced dose of posttransplantation cyclophosphamide for poor-prognosis or refractory leukemia and myelodysplastic syndrome. Exp Hematol. 2015;43:921-929.e1.
Sugita J, Kawashima N, Fujisaki T, Kakihana K, Ota S, Matsuo K, et al. HLA-haploidentical peripheral blood stem cell transplantation with post-transplant cyclophosphamide after busulfan-containing reduced-intensity conditioning. Biol Blood Marrow Transplant. 2015;21:1646–52.
Sugita J, Kagaya Y, Miyamoto T, Shibasaki Y, Nagafuji K, Ota S, et al. Myeloablative and reduced-intensity conditioning in HLA-haploidentical peripheral blood stem cell transplantation using post-transplant cyclophosphamide. Bone Marrow Transplant. 2019;54:432–41.
Shimada K, Narimatsu H, Morishita Y, Kohno A, Saito S, Kato Y. Severe regimen-related toxicity of second transplantation for graft failure following reduced-intensity cord blood transplantation in an adult patient. Bone Marrow Transplant. 2006;37:787–8.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14:641–50.
Ishida S, Doki N, Shingai N, Yoshioka K, Kakihana K, Sakamaki H, et al. The clinical features of fatal cyclophosphamide-induced cardiotoxicity in a conditioning regimen for allogeneic hematopoietic stem cell transplantation (allo-HSCT). Ann Hematol. 2016;95:1145–50.
Marumo A, Omori I, Tara S, Otsuka Y, Konuma R, Adachi H, et al. Cyclophosphamide-induced cardiotoxicity at conditioning for allogeneic hematopoietic stem cell transplantation would occur among the patients treated with 120 mg/kg or less. Asia Pac J Clin Oncol. 2022. https://doi.org/10.1111/ajco.13674.
Zeiser R, Blazar BR. Acute graft-versus-host disease - biologic process, prevention, and therapy. N Engl J Med. 2017;377:2167–79.
Fuji S, Oshima K, Ohashi K, Sawa M, Saito T, Eto T, et al. Impact of pretransplant donor-specific anti-HLA antibodies on cord blood transplantation on behalf of the transplant complications working group of Japan society for hematopoietic cell transplantation. Bone Marrow Transplant. 2020;55:722–8.
Acknowledgements
The authors thank all the physicians and staff at the transplant centers who provided the clinical data to the Transplant Registry Unified Management Program of the Japan Society of Hematopoietic Cell Transplantation. The authors also thank Enago (www.enago.jp) for the English language review. KH, YN, MK, AS, SF and Hideki N designed this study on behalf of the transplant complication working group in the Japan Society for Hematopoietic Cell Transplantation. KH performed all analyses and wrote the first draft. Hirohisa N, MT, MA, MO, YH, TI, and YA contributed to data interpretation and correction of the draft. All authors approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Ethics approval
Our study protocol was approved by the institutional review board of the Tokai University School of Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Harada, K., Najima, Y., Kato, M. et al. Outcomes of salvage haploidentical transplantation using posttransplant cyclophosphamide for graft failure following allogeneic hematopoietic stem cell transplantation. Int J Hematol 116, 744–753 (2022). https://doi.org/10.1007/s12185-022-03405-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-022-03405-w