Abstract
Background
Patients with multiple myeloma (MM) have increased risks of venous thromboembolism (VTE) and arterial thromboembolism (ATE). The risk of thrombosis differs among different treatment regimens. It is unknown if daratumumab could affect thrombosis risk.
Methods
A comprehensive search was conducted until April 2020. Events of VTE, including pulmonary embolism and deep venous thrombosis, as well as events of ATE, including acute ischemic stroke and myocardial infarction, were extracted from trials. In addition, events of thrombocytopenia and gastrointestinal (GI) bleeding were also extracted.
Results
Six trials were included in the meta-analysis. Daratumumab was associated with a lower risk of VTE compared with non-daratumumab regimen (Risk ratio [RR], 0.60; 95% confidence interval [CI], 0.40–0.91). The risk of ATE had no significant difference (RR, 0.80; 95% CI, 0.48–1.33). Daratumumab was also associated with a trend of higher risk of Grade 3/4 thrombocytopenia (RR, 1.14; 95% CI, 0.94–1.38), while the risk of GI bleeding was not significantly different (RR, 1.32; 95% CI, 0.38–4.65).
Conclusion
Daratumumab is associated with lower risk of VTE in clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cancer patients are known to have a higher incidence of thromboembolism than the general population. Patients with malignant hematologic diseases, in particular those with multiple myeloma (MM), are among the highest risk group [1, 2]. In a population study, the hazard ratio was 7.5 for venous thromboembolism (VTE) and 1.7 for arterial thromboembolism (ATE) in patients with MM, compared with their matched controls [3]. Studies have shown that the risk of thromboembolism in MM is modified by patient factors, disease status, as well as treatment regimen [4]. Indeed, in patients receiving immunomodulatory drugs (IMiDs) containing regimen, the incidence of VTE could be as high as 20% [5]. Therefore, routine VTE prophylaxis is recommended for patients receiving IMiD-containing regimen [6].
Daratumumab, an anti-CD38 monoclonal antibody, is becoming the first-line treatment for relapsed/refractory MM, as well as newly diagnosed MM with high risk features. However, its association with thromboembolism has not been well studied. Given that CD38 plays a critical role in the procoagulant activity of platelets and hemostasis [7], concerns have been raised whether its inhibition could affect the risk of thromboembolism. In this meta-analysis, we aim to investigate the risks of ATE and VTE in patients receiving daratumumab.
Materials and methods
Literature search
This study was performed in accordance with the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) guideline. In April 2020, the following data sources were searched: The Cochrane Controlled Trial Register, EMBASE, PubMed, ClinicalTrials.gov, as well as conference proceedings of the American Society of Hematology and the American Society of Clinical Oncology. The following medical terms were used in the search: (1) daratumumab, (2) darzalex, (3) 1 OR 2, (4) myeloma, (5) 3 AND 4. Furthermore, a validated search strategy to identify controlled trials were used in PubMed [8] and the “controlled trials” filter was used in EMBASE. The search was limited to publications in English.
Study selection
The inclusion criteria were specified in advance. Studies were eligible for inclusion if they are randomized-controlled trials comparing daratumumab-containing and non-daratumumab regimen. We included both trials using daratumumab in newly diagnosed MM as well as relapsed/refractory MM. For cases in which several reports were available for the same trial, the most recent data were included. Two of the authors (J.W. and Y.K.) reviewed the relevant reports and applied inclusion criteria independently.
Data extraction
Two of the authors (J.W. and Y.K.) independently extracted the data from included trials. The data were obtained from published reports, study results from ClinicalTrials.gov, or directly from investigators of the trial. For VTE, incidences of pulmonary embolism (PE) and deep venous thrombosis (DVT) were extracted. For ATE, incidences of acute ischemic stroke (AIS) and myocardial infarction (MI) were extracted. Other information, such as characteristics of trial participants, type of intervention, and incidence of all and any grade 3 or 4 thrombocytopenia, were also extracted. Disagreements were resolved by discussion between the two review authors; if no agreement could be reached, a third investigator would be consulted.
Statistical analysis
When specific data were not available, requests for the information were sent to the corresponding authors of the trial. Risk ratio (RR) of thromboembolism events was the primary measure of interest. Given the heterogeneity of the population, the random-effects model was used throughout the analysis. The Paule-Mandel method for random-effects model was used due to small number of studies and rarity of events, which is supposed to lead to more conservative results [9]. The heterogeneity was assessed by the Paule-Mandel tau square, I2 index, and Cochran’s Q test. Publication bias was assessed using funnel plots. Meta-regression with a mixed-effects model was used to assess the association between the response rate or thrombocytopenia and thromboembolism events; the restricted maximum likelihood method was used to estimate variance. All tests were two sided, and p < 0.05 was considered statistically significant. Statistical calculations were made using R statistical software version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study selection and characteristics of included trials
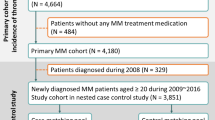
The search yielded 630 potentially relevant reports, of which 56 were considered for further investigation. Of these, 50 reports were excluded for various reasons (Fig. 1). The final meta-analysis consisted of 6 trials [10,11,12,13,14,15], randomizing 3,802 patients, from 2016 to 2020. The characteristics of the included trials were shown in Table 1. All trials are open labeled, parallelly assigned, and demonstrate adequate concealment of allocation (Supplemental Table 1).
Different strategies for VTE prophylaxis were applied in different trials. In the PULLOX trial [10], patient either received aspirin or low-molecular-weight heparin (LMWH) per physicians’ preference. In the MAIA trial [13], patients received aspirin, LMWH, or warfarin, based on the VTE risk factors, according to the International Myeloma Working Group (IMWG) recommendations [6]. In the GRIFFIN trial [15], all patients received aspirin; the addition of a second prophylactic medication, LMWH, was optional. However, in the ALCYONE trial [12], where no IMiD was administered, no VTE prophylaxis was required per trial protocol. Details for VTE prophylaxis were not available for the CASTOR trial [11] and the CASSIOPEIA trial [14].
Daratumumab use and the risk of VTE
All trials reported relevant data for the analysis of VTE. The funnel-plot (Supplemental Fig. 1), followed by the Egger regression test, did not find significant publication bias (p = 0.44). Treatment with daratumumab was associated with a statistically significant lower rate of VTE compared with non-daratumumab regimens (RR, 0.60; 95% confidence interval [CI], 0.40–0.91; Fig. 2). For subtypes of VTE, there was a significantly lower risk of PE associated with daratumumab (RR, 0.60; 95% CI, 0.38–0.95; Fig. 2). There was a trend of lower risk for DVT but this was not statistically significant (RR, 0.67; 95% CI, 0.26–1.67; Fig. 2).
The subgroup analysis of specific therapeutic regimens showed a significantly lower risk of VTE among trials with IMiD-containing regimens (RR, 0.61; 95% CI, 0.40–0.94; 4 trials, 2,568 patients; Supplemental Fig. 2). There was no significant difference for non-IMiD regimens (RR, 0.44; 95% CI, 0.06–3.37; 2 trials, 1,180 patients; Supplemental Fig. 2).
Daratumumab use and the risk of ATE
Five trials [10,11,12,13, 15] reported relevant data for the analysis of ATE. The funnel-plot (Supplemental Fig. 3), followed by the Egger regression test, did not find significant publication bias (p = 0.46). No significant difference was found regarding the risk of overall ATE (RR, 0.80; 95% CI, 0.48–1.33), acute ischemic stroke (RR, 0.89; 95% CI, 0.42–1.87), or myocardial infarction (RR, 0.68; 95% CI, 0.33–1.39). (Fig. 3).
The subgroup analysis showed no significant difference of risk of ATE among trials with IMiD-containing regimen (RR, 0.61; 95% CI, 0.34–1.12; 3 trials, 1494 patients; Supplemental Fig. 3) or with non-IMiD regimen (RR, 1.55; 95% CI, 0.60–3.99; 2 trials, 1,180 patients; Supplemental Fig. 4).
Daratumumab use and the incidence of thrombocytopenia
Compared with non-daratumumab regimens, the use of daratumumab was associated with a trend of higher incidence of all-grade thrombocytopenia (RR, 1.09; 95% CI, 0.96–1.24; Fig. 4), as well as Grade 3/4 thrombocytopenia (RR, 1.14; 95% CI, 0.94–1.38; Fig. 4). No significant difference of the incidence of gastrointestinal bleeding was observed (RR, 1.32; 95% CI, 0.38–4.65; Fig. 4).
Meta-regression analysis of risk of VTE
Given that significant heterogenicity of thrombocytopenia incidence and treatment response rate exist between the treatment arms and the control arms, meta-regression analysis was performed to assess their impact on the VTE. The outcome is the RR of VTE and the modifier is the incidence of all-grades thrombocytopenia in the daratumumab arm, or the odds ratio (ORs) of achieving complete response (CR) or better (including CR and stringent CR) after treatment. No significant association was identified (p = 0.84 and 0.97, as shown in Fig. 5a and b, respectively).
Meta-regression analysis of the risk ratio of VTE in relation to the incidence of thrombocytopenia and treatment response rate. a No significant association was observed between the risk of VTE and the incidence of all-grades thrombocytopenia (p = 0.84). b No significant association was observed between the risk of VTE and the odds ratio of achieving CR or better (including CR and stringent CR) (p = 0.97). The linear model is shown in the solid line with corresponding 95% confidence interval bounds shown in dashed lines. OR odds ratio, CR complete response
Discussion
In this meta-analysis, we showed that in randomized-controlled trials (RCTs), the use of daratumumab was associated with a lower risk of VTE comparing with non-daratumumab regimen. The risk of ATE, however, was not significantly different between daratumumab and non-daratumumab regimens. Furthermore, daratumumab was associated with higher incidences of thrombocytopenia.
Six trials were identified directly comparing daratumumab and non-daratumumab regimen. Heterogeneity was noticed among the studies, with the incidence of VTE ranging from 0 to 4.4% in the daratumumab arm, and 0.9–6.0% in the non-daratumumab arm. This could be explained by differences in disease status among various trials. Past studies have shown that the risk of VTE is higher at the time of diagnosis than after relapse [3]. We also found a higher incidence of VTE for newly diagnosed MM than relapsed/refractory MM (2.6% vs 1.7%, respectively) in patients receiving daratumumab. Moreover, the heterogeneity could also be caused by different treatment regimens. When IMiDs were given in combination with other agents, the risk of VTE significantly increased and remained higher despite VTE prophylaxis [16]. In the daratumumab arm of our study, the incidence of VTE was 2.6% for patients on IMiD-containing regimen, compared with only 0.3% for patients on non-IMiD regimen. Other treatment related factors, such as the use of erythropoietin, could not be explored due to limited information. Given heterogeneities of included studies, the random-effects model was used, despite small I2, which is notoriously imprecise in meta-analysis with small number of studies [17].
Our study showed that daratumumab was associated a lower risk of VTE in clinical trials. The mechanisms are unclear; however, a possible explanation could be the “on-target, off tumor” effect of CD38 inhibition. CD38, a surface glycoprotein, acting as a receptor and an ectoenzyme, is involved in intracellular Ca2+ signaling. It is widely expressed on immune cells, as well as red blood cells and platelets [18]. In vitro studies showed that thrombin-induced platelet activation was compromised by CD38 deficit; animal models showed that CD38-deficient mice had longer bleeding times and unstable formations of thrombus [7]. Therefore, platelet dysfunction might contribute to lower incidences of VTE. In addition, patients on daratumumab had improved health-related quality of life [19], which would further reduce VTE risk factors such as immobility. Finally, we found severe thrombocytopenia, a protective factor for VTE [20], was more common in the daratumumab arm. Of note, although it is still unclear if treatment response rate in MM is associated with risk of VTE, patients in the daratumumab arm have significantly improved response rate. Nonetheless, meta-regression did not find the risk of VTE was significantly associated with improved response rate (indicated by the odds ratio of complete response or better).
Looking into subtypes of VTE, daratumumab was associated with a trend of lower risk of DVT, but not statistically significant. In addition, in the subgroup analysis, trials with non-IMiD regimen had a trend of lower risk of VTE, but not statistically significant. These results could be due to insufficient statistical power due to small numbers of studies and rarity of events. However, true insignificance could not be excluded.
In terms of ATE, we did not find significant risk differences between daratumumab and its comparators (RR, 0.80; 95% CI, 0.48–1.33). However, a lower trend was seen in the subgroup analysis of IMiD-containing regimens (RR, 0.61; 95% CI, 0.34–1.12). CD38 has been found on cardiomyocytes [21] and preclinical studies have shown that CD38 deficiency is cardio-protective. For example, Guan et al. [22] showed that CD38 deficiency protected mice heart from ischemia/perfusion injury through the anti-oxidative stress pathway. Unlike VTE, for which the risk peaks within the first few months after initiation of therapy and decreases dramatically thereafter [23], the risk curve for ATE is more flat and elevated for a prolonged period. In a large registry study, MM was associated with increased risk of ATE of 1.9-, 1.5-, and 1.5-fold at 1-, 5-, and 10-year follow up [3]. Therefore, given limited follow up time in clinical trials, a risk difference might not become obvious. Future studies using registries are needed to further identify the association between daratumumab use and the risk of ATE.
Myeloma treatment regimens are associated with high rates of bone marrow suppression, which is more common with multi-drug combination [24]. A recent study [25] found patients on daratumumab had higher rates of neutropenia, anemia, and thrombocytopenia, indicating that daratumumab-containing regimen have considerable bone marrow suppression effects. In our meta-analysis, we also found a trend of higher incidences of all grades and severe thrombocytopenia in patients receiving daratumumab. However, we found the risk of GI bleeding was low in both arms and had no significant difference.
Conclusion
In patients with MM, daratumumab in combination with other anti-myeloma medications is associated with a lower risk of VTE in clinical trials. The risk reduction should be confirmed by prospective controlled studies.
Funding source
None.
References
Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293:715–22.
Cesarman-Maus G, Braggio E, Fonseca R. Thrombosis in multiple myeloma (MM). Hematology. 2012;17(Suppl 1):S177–S180180.
Kristinsson SY, Pfeiffer RM, Bjorkholm M, Goldin LR, Schulman S, Blimark C, et al. Arterial and venous thrombosis in monoclonal gammopathy of undetermined significance and multiple myeloma: a population-based study. Blood. 2010;115:4991–8.
Leebeek FW. Update of thrombosis in multiple myeloma. Thromb Res. 2016;140(Suppl 1):S76–80.
Carrier M, Le Gal G, Tay J, Wu C, Lee AY. Rates of venous thromboembolism in multiple myeloma patients undergoing immunomodulatory therapy with thalidomide or lenalidomide: a systematic review and meta-analysis. J Thromb Haemost. 2011;9:653–63.
Palumbo A, Rajkumar SV, Dimopoulos MA, Richardson PG, San Miguel J, Barlogie B, et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia. 2008;22:414–23.
Mushtaq M, Nam TS, Kim UH. Critical role for CD38-mediated Ca2+ signaling in thrombin-induced procoagulant activity of mouse platelets and hemostasis. J Biol Chem. 2011;286:12952–8.
Robinson KA, Dickersin K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. Int J Epidemiol. 2002;31:150–3.
Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods. 2016;7:55–79.
Dimopoulos MA, Oriol A, Nahi H, San-Miguel J, Bahlis NJ, Usmani SZ, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:1319–31.
Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375:754–66.
Mateos MV, Dimopoulos MA, Cavo M, Suzuki K, Jakubowiak A, Knop S, et al. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378:518–28.
Facon T, Kumar S, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med. 2019;380:2104–15.
Moreau P, Attal M, Hulin C, Arnulf B, Belhadj K, Benboubker L, et al. Bortezomib, thalidomide, and dexamethasone with or without daratumumab before and after autologous stem-cell transplantation for newly diagnosed multiple myeloma (CASSIOPEIA): a randomised, open-label, phase 3 study. The Lancet. 2019;394:29–38.
Voorhees PM, Kaufman JL, Laubach JP, Sborov DW, Reeves B, Rodriguez C, et al. Daratumumab, lenalidomide, bortezomib, & dexamethasone for transplant-eligible newly diagnosed multiple myeloma: GRIFFIN. Blood. 2020. https://doi.org/10.1182/blood.2020005288.
Al-Ani F, Bermejo JM, Mateos MV, Louzada M. Thromboprophylaxis in multiple myeloma patients treated with lenalidomide - A systematic review. Thromb Res. 2016;141:84–90.
Ioannidis JP, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–6.
van de Donk N, Richardson PG, Malavasi F. CD38 antibodies in multiple myeloma: back to the future. Blood. 2018;131:13–29.
Perrot A, Facon T, Plesner T, Usmani SZ, Kumar S, Bahlis NJ, et al. Faster and sustained improvement in health-related quality of life (HRQoL) for newly diagnosed multiple myeloma (NDMM) patients ineligible for transplant treated with daratumumab, lenalidomide, and dexamethasone (D-Rd) versus Rd alone: MAIA. J Clin Oncol. 2019;37:8016.
Baelum JK, Moe EE, Nybo M, Vinholt PJ. Venous Thromboembolism in Patients With Thrombocytopenia: Risk Factors, Treatment, and Outcome. Clin Appl Thromb Hemost. 2017;23:345–50.
Plummer C, Driessen C, Szabo Z, Mateos MV. Management of cardiovascular risk in patients with multiple myeloma. Blood Cancer J. 2019;9:26.
Guan XH, Liu XH, Hong X, Zhao N, Xiao YF, Wang LF, et al. CD38 Deficiency protects the heart from ischemia/reperfusion injury through activating SIRT1/FOXOs-mediated antioxidative stress pathway. Oxid Med Cell Longev. 2016;2016:7410257.
Ishak J, Dimopoulos MA, Weber D, Knight RD, Shearer A, Caro JJ. Declining Rates of Adverse Events and Dose Modifications with Lenalidomide in Combination with Dexamethasone. Blood. 2008;112:3708.
Leleu X, Gay F, Flament A, Allcott K, Delforge M. Incidence of neutropenia and use of granulocyte colony-stimulating factors in multiple myeloma: is current clinical practice adequate? Ann Hematol. 2018;97:387–400.
Al Hadidi S, Miller-Chism CN, Kamble R, Mims M. Safety analysis of five randomized controlled studies of daratumumab in patients with multiple myeloma. Clin Lymphoma Myeloma Leukemia. 2020. https://doi.org/10.1016/j.clml.2020.04.004.
Acknowledgements
None
Author information
Authors and Affiliations
Contributions
Concept and design: JW. Data collection, assembly, and analysis: JW, YK. Manuscript writing: All authors. Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Wang, J., Kim, Y. Risk of thromboembolism in patients with multiple myeloma treated with daratumumab: a systemic review and meta-analysis. Int J Hematol 112, 650–657 (2020). https://doi.org/10.1007/s12185-020-02954-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-020-02954-2