Abstract
It is uncertain if different immunomodulatory drugs (IMID) pose distinct thrombotic risk in patients with newly diagnosed multiple myeloma (MM). Among 2397 MM patients from the SEER-Medicare database from 2007 to 2013, 78% received lenalidomide, and 22% received thalidomide. After inverse probability weighting to balance confounders, the 12-month incidences of venous thromboembolism (VTE 10%) and arterial thromboembolism (ATE 5%) were similarly high in both groups. Lenalidomide versus thalidomide had a subdistribution hazard ratio of 1.11 (0.59–2.02) for VTE and a subdistribution hazard ratio of 0.96 (0.45–1.98) for ATE. Overall survival was not significantly different with a hazard ratio of 0.88 (0.60–1.18) for lenalidomide versus thalidomide. Concurrent anticoagulant prophylaxis was infrequently prescribed in < 20% of both groups. Our study demonstrates that despite improvement in myeloma-directed therapy and supportive care, thrombosis remains an important consideration for all IMID-treated MM patients. Appropriate risk stratification and vigilant thromboprophylaxis remain essential to prevent this complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy backbones with immunomodulatory drugs (IMID) have become the standard of care for the treatment of multiple myeloma (MM) [1]. Despite improved survival outcomes, thrombotic complications remain a concern especially in older patients with comorbidities. A meta-analysis showed that lenalidomide-based regimen may be associated with a lower rate of thromboembolism than thalidomide-containing regimen in patients with newly diagnosed MM with (0.7 versus 2.6 per 100-patient-cycle) or without prophylaxis (0.8 versus 4.1 per 100-patient-cycle) [2]. Since thalidomide is still commonly used outside of the USA, it is important to understand if current thromboprophylaxis guidelines are generalizable to all immunomodulatory drugs. However, no prior population studies directly compared the incidence of thrombotic events between the two IMID-based regimens while accounting for important confounders. In the current study, we used propensity score weighting to compare the incidence of venous thromboembolism (VTE) and arterial thromboembolism (ATE) and survival in patients with newly diagnosed MM who are treated with lenalidomide- versus thalidomide-containing regimens.
Methods
We performed a retrospective cohort study using the SEER-Medicare database in the USA and included all patients 66 years or older with newly diagnosed MM from 2007 to 2013. The study was reviewed and considered exempt by the University of Washington Institutional Review Board. Patients were included if they had a prescription for an IMID within 12 months of diagnosis and complete enrollment for fee-for-service and prescription drug coverage for at least 12 months prior to treatment. Patients were followed from the IMID index date until first VTE occurrence or death. They were censored for disenrollment from Medicare A/B/D, enrollment in health maintenance organization, or end of available claims data on December 31, 2014. We defined first VTE (including pulmonary embolism (PE) and deep vein thrombosis (DVT)) and first ATE (including cerebrovascular accident (CVA) and myocardial infarction (MI)) using previously validated ICD-9-CM codes with positive predictive value of 75–95% [3,4,5]. Specifically, we defined VTE outcome as having either one inpatient claim or two outpatient claims at least 30 days apart in combination with an anticoagulant prescription within 90 days [6]. As stroke and myocardial infarction treatments require admissions, only inpatient discharge claims were used to identify ATE.
Demographic information was obtained from the Patient Entitlement and Diagnosis Summary File (PEDSF). Thrombotic risk factors including ischemic heart disease, congestive heart failure, peripheral vascular disease, cerebral vascular disease, atrial fibrillation, hypertension, obstructive pulmonary disease, diabetes, renal disease, liver disease, peptic ulcers, anemia, coagulopathy (congenital or acquired factor deficiencies, qualitative platelet defects, purpura and other hemorrhagic conditions, and unspecified thrombocytopenia), central venous catheter (CVC), recent sepsis, recent surgery, recent bleeding history, and remote (> 6 months) VTE history were ascertained from Medicare files using a look-back window of up to 12 months [7,8,9]. Concurrent chemotherapy, dexamethasone, and erythropoietin were defined using a −30 to +30-day window from when IMID prescriptions were initiated [10]. Concurrent anticoagulants were defined using a −30 to +7-day window from initiation of IMID prescriptions. Dexamethasone dose per cycle was calculated from the average monthly dexamethasone dose.
We used inverse probability of treatment weighting (IPTW) to balance potential confounders including demographics, comorbidities, concurrent medications, and year of diagnosis, where a standardized difference of < 0.1 was considered adequately balanced. We included the year of diagnosis as a proxy for other unobserved confounders in cancer therapeutic changes over time. Hazard ratios (HR) based on weighted Kaplan-Meier curves and Cox models (HR) were used to compare overall survival [11]. Subdistribution hazard ratios (SHR) based on weighted cumulative incidence curves and Fine-Gray were used to compare the incidence of VTE and ATE where death was treated as a competing risk. Variance was estimated via 200 bootstraps to preserve the correct sample size [12].
Results
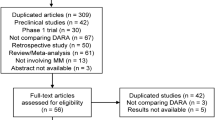
The SEER-Medicare registry contained 30,757 patients with newly diagnosed MM from 2007 to 2013. From this initial cohort, 394 patients were excluded for having an incorrect diagnosis, 23,710 patients were excluded from either not having Medicare Part D prescription drug coverage or not receiving an IMID within 12 months of diagnosis, 4053 patients were excluded for having an enrollment period shorter than 12 months prior to treatment, and 203 patients were excluded for having a recent thrombotic event within 6 months prior to IMID index date. Among the 2397 patients who met the eligibility criteria for the study, 78% received lenalidomide (n = 1863), and 22% received thalidomide (n = 534).
In the native cohort, there was a strong temporal trend of increasing lenalidomide use after its initial approval among the US Medicare patients (Table 1). Compared to the thalidomide group, patients who were treated with lenalidomide-based regimen were more likely to receive bortezomib and lower dose of dexamethasone. Although approximately 43% of the total patients would have been classified as “high thrombotic risk” according to the existing NCCN/IMWG consensus [13], concurrent anticoagulant including low-molecular-weight heparin (LMWH), warfarin, or direct oral anticoagulants (DOAC) was prescribed in only 10.7% of lenalidomide group and 18.6% of thalidomide group.
The unadjusted 12-month incidence rate (IR) and onset of various thromboembolic outcomes are shown in Table 2. Specifically, the lenalidomide cohort had a rate of 2.1 per 100-person-year for PE, 6.3 per 100-person-year for DVT, 2.4 per 100-person-year for MI, and 0.8 per 100-person-year for CVA. The thalidomide cohort had a similar rate of 1.9 per 100-person-year for PE, 6.0 per 100-person-year for DVT, 2.8 per 100-person-year for MI, and 2.1 per 100-person-year for CVA. PE and MI occurred very early during the treatment with a median onset of 47 days (IQR 26–126) and 53 days (IQR 22–126), respectively. DVT and CVA occurred within the first 3–6 months of treatment with a median onset of 83 days (IQR 38–133) and 135 days (IQR 88–192).
All observed confounders, including demographics, concurrent treatments, and comorbidities, were balanced between the two groups after IPTW adjustment with standardized differences < 0.1 (Table 1). The 12-month incidences of VTE (10%) and ATE (5%) were similarly high in both groups (Fig. 1). Lenalidomide versus thalidomide had a SHR of 1.11 (0.59–2.02) for VTE and a SHR 0.96 (0.45–1.98) for ATE. Overall survival was not significantly different with a HR of 0.88 (0.60–1.18) for lenalidomide versus thalidomide.
Discussion
In this propensity score weighted cohort study of older patients with newly diagnosed MM, concurrent anticoagulant prophylaxis was infrequently prescribed (< 20%), while the 12-month cumulative incidences of VTE (10%) and ATE (5%) were similarly high in both lenalidomide and thalidomide treatment groups. Overall, our results suggest that appropriate risk stratification and vigilant thromboprophylaxis remain essential for MM patients receiving any immunomodulatory drugs.
The relative rates of thrombotic complication in lenalidomide- versus thalidomide-containing regimens have not been studied in detail previously. One retrospective cohort study from Mayo Clinic evaluated patients receiving lenalidomide/dexamethasone versus thalidomide/dexamethasone matched on age, sex, transplant status, and dose of dexamethasone. Thromboembolism occurred in 9.2% in lenalidomide group versus 15.3% in the thalidomide group [14]. The result seems to echo the findings from a prior meta-analysis of pooled prospective trials that showed lower thrombotic complications for lenalidomide versus thalidomide [2]. Since thalidomide is an older IMID, commonly given in the era of high-dose dexamethasone and cytotoxic treatment, it is challenging to distinguish the effect of the specific IMID on the risk of thrombosis without adjustment for other patient- and treatment-specific risk factors for VTE. Unlike the previous studies, our current IPTW analysis suggests that the venous and arterial thrombotic risks remain similarly high in lenalidomide and thalidomide. The infrequent use of anticoagulant prophylaxis may be related to perceived lower risk of thrombosis associated with newer drugs or the difficulty to appropriately risk stratify patients without a validated risk prediction tool.
The effect of different IMIDs on survival is also a debated topic. The beforementioned matched cohort analysis showed an improved overall survival with lenalidomide versus thalidomide containing regimen (HR 0.60, 95% CI 0.40–0.92); however, the study did not account for disease-specific confounders [14]. Another retrospective cohort study using the UnitedHealth database showed no difference in overall survival among different IMIDs (HR 1.00, 95% CI 0.71–1.41) after accounting for baseline confounders [15]. While our findings agree with the latter report, the lack of difference in survival between the two IMID containing regimens should be interpreted with caution as unobserved confounders such as disease severity could have influenced this outcome. The maturing results from the induction phase of the Myeloma XI randomized trial will hopefully address the impact of different IMIDs on survival [16].
There are inherent limitations associated with our retrospective study. Despite using previously validated algorithms, the use of administrative codes could have introduced non-differential misclassification that diminished the detectable difference between the treatment arms. Medicare database only enrolled patients after age 65 so this analysis was limited to old patients in the USA. The database did not contain laboratory values for initial staging or capture nonprescription drugs such as aspirin, and these might be important factors as discussed above. Finally, among the 12% of patients that were exposed to anticoagulant at the time of IMID initiation, we did not distinguish whether they received chronic anticoagulant for prior atrial fibrillation or remote VTE or whether they received new anticoagulant for VTE prevention.
In conclusion, the incidences of venous and arterial thromboses are similarly high in older patients with newly diagnosed MM receiving lenalidomide- and thalidomide-containing regimens. Our study shows that anticoagulant prophylaxis is underutilized in real-world practice. Future studies should focus on validating new clinical risk stratification tools to provide guidance on appropriate thromboprophylaxis for MM patients receiving IMID containing regimens.
References
Moreau P (2017) How I treat myeloma with new agents. Blood 130:1507–1513. https://doi.org/10.1182/blood-2017-05-743203
Carrier M, Le Gal G, Tay J et al (2011) Rates of venous thromboembolism in multiple myeloma patients undergoing immunomodulatory therapy with thalidomide or lenalidomide: a systematic review and meta-analysis. J Thromb Haemost 9:653–663. https://doi.org/10.1111/j.1538-7836.2011.04215.x
White RH, Garcia M, Sadeghi B, Tancredi DJ, Zrelak P, Cuny J, Sama P, Gammon H, Schmaltz S, Romano PS (2010) Evaluation of the predictive value of ICD-9-CM coded administrative data for venous thromboembolism in the United States. Thromb Res 126:61–67. https://doi.org/10.1016/j.thromres.2010.03.009
Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH (2004) Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: estimating positive predictive value on the basis of review of hospital records. Am Heart J 148:99–104. https://doi.org/10.1016/j.ahj.2004.02.013
Jones SA, Gottesman RF, Shahar E, Wruck L, Rosamond WD (2014) Validity of hospital discharge diagnosis codes for stroke: the atherosclerosis risk in communities study. Stroke 45:3219–3225. https://doi.org/10.1161/STROKEAHA.114.006316
Lyman GH, Eckert L, Wang Y, Wang H, Cohen A (2013) Venous thromboembolism risk in patients with cancer receiving chemotherapy: a real-world analysis. Oncologist 18:1321–1329. https://doi.org/10.1634/theoncologist.2013-0226
National Cancer Institute NCI Comorbidity Index. https://healthcaredelivery.cancer.gov/seermedicare/considerations/comorbidity.html
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27. https://doi.org/10.1097/00005650-199801000-00004
Chrischilles EA, Winiecki SK, Carnahan RM, et al. Mini-sentinel assessment protocol thromboembolic events after immunoglobulin administration. https://www.sentinelinitiative.org/vaccines-blood-biologics/assessments/thromboembolic-events-after-immunoglobulin-administration
Cancer Research Network Cancer Therapy Look-up Tables. https://crn.cancer.gov/resources/codes.html
Austin PC (2014) The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 33:1242–1258. https://doi.org/10.1002/sim.5984
Austin PC (2016) Variance estimation when using inverse probability of treatment weighting (IPTW) with survival analysis. Stat Med 35:5642–5655. https://doi.org/10.1002/sim.7084
National Comprehensive Cancer Network (2018) Cancer-associated venous thromboembolic disease. VTE-A2
Gay F, Hayman SR, Lacy MQ, Buadi F, Gertz MA, Kumar S, Dispenzieri A, Mikhael JR, Bergsagel PL, Dingli D, Reeder CB, Lust JA, Russell SJ, Roy V, Zeldenrust SR, Witzig TE, Fonseca R, Kyle RA, Greipp PR, Stewart AK, Rajkumar SV (2010) Lenalidomide plus dexamethasone versus thalidomide plus dexamethasone in newly diagnosed multiple myeloma: a comparative analysis of 411 patients. Blood 115:1343–1350. https://doi.org/10.1182/blood-2009-08-239046
Luo J, Gagne JJ, Landon J, Avorn J, Kesselheim AS (2017) Comparative effectiveness and safety of thalidomide and lenalidomide in patients with multiple myeloma in the United States of America: a population-based cohort study. Eur J Cancer 70:22–33. https://doi.org/10.1016/j.ejca.2016.10.018
Jackson GH, Davies FE, Pawlyn C, Cairns DA, Striha A, Collett C, Hockaday A, Jones JR, Kishore B, Garg M, Williams CD, Karunanithi K, Lindsay J, Jenner MW, Cook G, Russell NH, Kaiser MF, Drayson MT, Owen RG, Gregory WM, Morgan GJ, UK NCRI Haemato-oncology Clinical Studies Group (2019) Lenalidomide maintenance versus observation for patients with newly diagnosed multiple myeloma (Myeloma XI): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 20:57–73. https://doi.org/10.1016/S1470-2045(18)30687-9
Acknowledgments
AL performed the research, designed the study, analyzed the data, and wrote the paper. DAG and GHL performed the research, designed the study, and wrote the paper. QW and GW analyzed the data. SL and ENL contributed essential tools and wrote the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The current study itself was conducted without funding from industry. AL reports grant funding from the Conquer Cancer Foundation Young Investigator Award, Hemostasis and Thrombosis Research Society Mentored Research Award supported by an independent medical educational grant from Shire, and National Hemophilia Foundation Shire Clinical Fellowship Award. Other authors report no relevant financial interests, activities, relationships, or affiliations.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Statement of informed consent
Informed consent was not obtained because this was a de-identified aggregate national claims database study where individual patient could not be identified and informed consent could not be obtained. The study was reviewed and considered exempt by the University of Washington Institutional Review Board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, A., Wu, Q., Warnick, G. et al. The incidence of thromboembolism for lenalidomide versus thalidomide in older patients with newly diagnosed multiple myeloma. Ann Hematol 99, 121–126 (2020). https://doi.org/10.1007/s00277-019-03860-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-019-03860-2